Summary Guidelines - The Castle Practice
advertisement

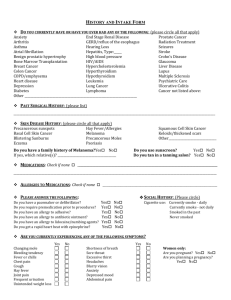
Summary Guidelines The notes are date stamped when they arrive in the practice. All new records must be sorted into date order and tagged within 2 weeks of arriving at the practice. All new notes must be summerised within 8 weeks of arriving at the practice. Check that the patient is currently registered and that you have all the relevant medical notes (including any from the oversized records filing system these records are clearly marked with: other records in administration room Double check the date of birth of the patient matches the date on the records and that it is defiantly the same patient Search all notes including summary cards, continuation cards, letters and results and note relevant significant events and diagnosis Add this information to the computerised medical record in chronological order Enter appropriate date for onset of each new problem, the year and month Enter read code, and in free text section, add any additional information that helps give specific detail about problem (egg site, left or right, summary of diagnostic evidence, investigations etc) Record cause (=main diagnosis) of all hospital admissions Record all fractures – specify left or right as free text Record all chronic diseases Record all abnormal and significant normal investigations (egg normal US, CT or MRI scans are usually significant Recurrent conditions need not be entered beyond date started Record all out-patient investigations and diagnoses (when a firm diagnosis is reached, use the free text to summarise the evidence for this diagnosis) it may be necessary to edit the preceding related codes (see editing summary later) Record all overdoses Record all psychiatric history Record obstetric history inc TOP’s Record allergies (as attached procedure) Record all immunisations via template If on repeat medication, there should be a diagnosis in summary list to show indication for drug and the repeat item should have an attached title Record significant family history Normal & abnormal cytology will be added via the practice administrator and the health care assistant, who will pass all abnormal data to the relevant clinician for action. Record useful health status data (last BP, Smoking status entry, Last cholesterol) via template USE OF READ CODES: Please use practice templates selecting CEG as preference (No History of codes H/O These start with a letter: e.g. Transient cerebral ischemia G65 (Not H/O TIA 14AB) If choice of suitable codes, go for ones starting with a single letter rather than codes starting with & These should only be used if no alternative Use higher level codes in general rather than sub codes Try not to use NOS (not otherwise specified) and NEC (not easily coded Fractures enter as appropriate, may need to add left or right in free text Operations e.g. appendectomy rather than appendicitis Cancers enter according to anatomical site (B codes) and enter histology and staging as free text Allergies Adverse reaction: To enter allergies correctly, so that they are linked to prescribing (to flash warnings if you prescribe inadvertently) and file in allergy section do not use standard codes route. There is a specific way to enter data that links to BNF chapters. Drug allergy 1: In clinical [choose allergy] 2: Enter as either [new drug] or [non drug allergy] 3: If [non drug] type in allergy and then read code and put in to summary. 4: If [drug] type in name of drug action as allergy/acute. 5: Add all this into the summary and into active. What sort of problem? Active titles Significant and ongoing e.g. chronic diseases such as diabetes, hypertension, asthma, COPD, hypothyroidism, on going psychiatric problems, ongoing cancers. If a patient is on repeat medication there should be an active problem to give the indication. Summary Diseases or events that happened at a particular point in time e.g. MI (through ischemic heart disease would be an active ongoing problem) cardiac catheterisation, operations, fractures etc Weed out and shred duplicate letters and any none clinically relevant letters to reduce volume of written notes where possible Immunisations Although the practice administrator looks and puts this information onto the system it is always best to check that the immunisations are on the system should you come across them in records? The easiest way to enter them is via [protocols] and then [child health] or [infectious dis/prevention control] Also what is very useful is adding any Flu vaccinations that have been to the patient within the last 12 months. And all pneumococcal vaccinations should be entered as well via either [infectious dis/prevention control] This information should also be dragged up into the summary Safety Netting If you come across a problem that you think might need a Doctors attention please leave a yellow sticker attached with tape to the notes once completed, in a Doctors tray e.g. if there are abnormal tests done just as the patient left the previous practice that doesn’t seem to have been actioned or followed up Finished When finished enter notes summarised on computer [code 9344] as summary entry with person summarising entering their details as free text. It is vital that this code is entered for future audits. If you have noted anything that should be followed up with the patient or clarified, pass the details on as per safety netting