Chapter 15: The Immune System
advertisement

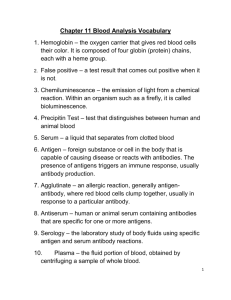
Chapter 15: The Immune System Defense Mechanisms Against pathogens constitute the immune system Can be grouped into 2 categories: _____________________ (nonspecific) immunity is inherited as part of structure of each organism Adaptive (specific) immunity is a function of lymphocytes and changes with exposure Innate Immunity Distinguishes between “self” and “non-self” Is __________________ of defense against invading pathogens Includes epithelial barriers, high acidity of gastric juice, phagocytosis, and fever Phagocytosis Is triggered in response to pathogen-associated molecular patterns (PAMPs) produced only by microorganisms Best known are lipopolysaccharide (LPS) and peptidoglycan from gram +bacteria Some immune cells have receptors for PAMPs (called _______ receptors) Is performed by 3 classes of phagocytic cells: Neutrophils - 1st to arrive at infection sites Mononuclear phagocytes - macrophages and __________________ Organ-specific phagocytes in liver, spleen, lymph nodes, lungs, and brain Fixed phagocytes line sinusoids of liver, spleen, and lymph nodes and remove pathogens Connective tissue and blood contain mobile leukocytes (WBCs) These are attracted to infection (_________________) by chemokines WBCs from blood exit capillaries by extravasation (diapedesis) and ingest pathogens Pseudopods from phagocyte surround pathogen Forming a vacuole that fuses with lysosomes which digest pathogen Fever Appears to be component of innate immunity __________ are released by WBCs in response to endotoxin from gram– bacteria Interferons Are polypeptides produced by cells infected with virus that provide short-acting, non-specific resistance to viral infection in nearby cells Adaptive Immunity Is __________________ ability to defend against specific pathogens by prior exposure to those pathogens Is mediated by production of specific ___________________ by lymphocytes Are molecules that elicit production of antibodies that specifically bind those antigens Are usually large molecules that are foreign to the body Immune system can distinguish “self” molecules from non-self antigens Normally makes antibodies only against non-self antigens Large, complex molecules can have a number of ____________ determinant sites Haptens Are small non-antigenic molecules that become antigens when bound to proteins Immunoassays Are tests that use specific antibodies to identify a particular antigen The binding of antibody to antigen causes clumping (___________________) which can be visualized Lymphocytes Are derived from stem cells in bone marrow Lymphocytes seed thymus, spleen, and lymph nodes with self-replacing colonies T lymphocytes (T Cells) Develop from lymphocytes that seed thymus Do not secrete antibodies Attack infected host cells, cancer cells, and foreign cells Thus they provide _____________________________ immunity B Lymphocytes (B Cells) Fight bacterial infections by secreting antibodies into blood and lymph Thus provide humoral immunity Thymus Is located below the thyroid gland Grows during childhood, gradually regresses after puberty Then, repopulation is by production in 2o ____________________ organs Secondary Lymphoid Organs Lymph nodes, spleen, tonsils, and Peyer’s patches In areas where antigens could gain entry to blood or lymph Lymphocytes migrate constantly through blood and lymph Enhances chance that antibody will encounter its _________________ Local Inflammation Occurs when bacteria enter a break in the skin Inflammatory reaction is initiated by _____________________ mechanisms Complement activation attracts phagocytes to area Attachment of antibodies to antigens amplifies nonspecific responses because of complement activation And promotes phagocytic activity of neutrophils, macrophages, and monocytes ( ______________________) Leukocytes move by chemotaxis to inflamed site Neutrophils arrive 1st, then monocytes, then T cells Mast cells secrete heparin, histamine, prostaglandins These produce redness, warmth, swelling, pus, and pain Recruit more _____________________ If infection continues, endogenous pyrogens are released B Lymphocytes (B Cells) Have antibodies on surface that are receptors for antigens When bound to antigen, are stimulated to divide and secrete antibodies When B cells divide, some progeny become memory cells Others become ______________________ that produce about 2000 antibodies/sec that are specific for original antigen This provides active immunity Binding of B cells to antigen also triggers a cascade of reactions that activate complement proteins which can kill antigen-bearing cells and promote phagocytosis Antibodies Are proteins called _______________________________ Antibodies have same basic structure but their differences provide for antibody specificity Antibody Structure Is in shape of “Y” 2 long heavy (H) chains are joined to 2 shorter light (L) chains Stalk of Y is constant and ___________________________ fragment (Fc) Arms of Y is antigen-binding fragment (Fab) and variable for antibody specifity Antibody Diversity Each person has about 1020 antibody molecules With a few million different specificities for any antigen a person might encounter If a few hundred genes code for Hs and a few hundred for Ls, Recombination of these in developing lymphocytes of marrow produces antigen-independent diversity Diversity is increased via somatic __________________________ B cells undergo antigen dependent proliferation in 2o lymphoid tissues The Complement System Is part of nonspecific defense system Activity is triggered by binding of antibodies to antigens (classic pathway) and by bacterial coat polysaccharides (____________________ pathway) Antibodies label targets for complement system attack and also stimulate opsonization Is a series of proteins whose activation forms a membrane _______________ complex which perforates a cell causing it to lyse Complement proteins can be subdivided into 3 functional groups: C1 - recognition C4, C2, C3 - _________________________ C5-C9 - attack (complement fixation) These form the membrane attack complex Membrane Attack Complex: creates large ____________ in membrane, causing osmotic influx of H2O, lysis, and cell death Complement Fragments Attracts phagocytes (chemotaxis) Serve as bridge for phagocytes to victim cell Stimulate __________________ cells to secrete histamine Which increases blood flow and capillary permeability, bringing in more phagocytes Killer or Cytotoxic T Cells Carry _______________ cell surface marker Destroy body cells that possess foreign antigens Usually from a pathogen, malignancy or self cells never seen by immune system Kill by cell-mediated destruction Secreting perforins which create a pore in victim's membrane and cause lysis Also secrete ________________ which cause destruction of victim's DNA Helper and Suppressor T Cells Helper Ts carry CD4 surface marker Indirectly participate by enhancing responses of both killer T cells and B cells ____________________ Ts decrease responses of killer Ts and B cells Carry CD25 surface marker (and CD4) Help protect against autoimmune responses Lymphokines Are _____________________ secreted by lymphocytes Usually called interleukin-1, 2, 3 . . . or IL-1, IL-2 . . . T Cell Receptor Proteins Only protein antigens are recognized by most T cells Foreign antigens are presented on surface of _________________________ cells Macrophages and dendritic cells Dendritic Cells Originate in marrow, then migrate to most tissues Prominent where pathogens might enter body Engulf protein antigens, partially digest them, and display polypeptide fragments on surface for T cells to "see" Fragments are associated on surface with ________________________antigens to activate Ts Dendritics migrate to secondary lymphoid organs to attract Ts Histocompatibility Antigens Are on surface of all body's cells except mature RBCs Also called _____________________________ antigens (HLAs) Are coded for by group of 4 genes on chromosome 6 called the major histocompatibility complex (MHC) The 4 genes have multiple alleles creating many possible MHC types MHC MHC genes produce 2 types of cell surface molecules: class-1 and class-2 Class-1s are made by all cells except _______________ Class-2s are made only by antigen-presenting cells and B cells Antigen is co-presented with a specific MHC marker because Killer T coreceptor CD8 interacts only with class-1s Helper T coreceptor ___________ interacts only with class-2s Interactions Between Antigen Presenting Cells and Lymphocytes T Cell Response to a Virus When virus infects body, it is phagocytized Partially-digested pp fragments are displayed Complexed with class-2 MHC molecules, it’s presented to helper T cells Macrophage-T cell Interaction Macrophages then complex with T cells and secrete IL-1 and TNF (tumor necrosis factor) IL-1 stimulates cell __________________ and proliferation of helper Ts Activated helpers promote macrophage activity and activate B cells Killer T cell Activity Killer Ts destroy infected cells if class-1 markers are present Helper T cell-B cell Interactions Activated helper Ts promote _____________________l response of B cells by binding to their surface antigens and MHC class 2s Causes proliferation of Bs, conversion to plasma cells, and their secretion of antibodies Destruction of T cells Ts have a surface receptor called FAS After infection, Ts begin to produce FAS ligand Binding of FAS to FAS ligand triggers _________________ (cell suicide) Active Immunity Primary and Secondary Responses 1st exposure to pathogen, btw 5-10 days, produce specific antibodies (primary response) Antibody levels plateau after few days and decline after a few weeks Subsequent exposure to same antigen causes _____________________ response Antibody production is much more rapid and sustained Clonal Selection Theory Is mechanism by which secondary immune responses are produced Each B cell produces only 1 kind of antibody and related antigen receptor Exposure to its antigen stimulates a B cell to divide and produce ________ Some become plasma cells to secrete antibodies Some become memory cells to produce antibodies in the 2o response Germinal Centers Develop in ___________________ and spleen from a cloned and activated B cell Which proliferate and undergo hypermutation Generating and secreting diverse antibodies for the 2o immune response Active Immunity Development of a 2o response provides active immunity Immunizations induce primary responses by inoculating people with __________________ or destroyed pathogens (vaccinations) Cause development of B cell clones that can provide 2o response Immunological Tolerance Tolerance requires continuous exposure to an antigen Some self-antigens, such as lens protein in eye, are normally hidden from blood Exposure to such self-antigens results in production of ______________________ Killer T cells that attack self-antigens are called autoreactive T cells 2 possible mechanisms for tolerance: Clonal deletion theory: tolerance occurs because T cells that recognize self-antigens are destroyed Clonal ______________: lymphocytes directed against selfantigens are present throughout life but don't attack self-antigens Appears to underlie tolerance in B cells Passive Immunity Is immune protection by transfer of _____________________ antibodies to a recipient from a donor Donor was actively immunized Used to treat snakebite, rabies, tetanus, hepatitis Occurs naturally before and after birth Antibodies from mother pass placenta to fetus in pregnancy and provide immunity 1st 3 days of nursing, mother makes ___________________, rich in antibodies, gives immunity Immunological competence (ability to mount a specific immune response) does not develop until 1 month after birth Monoclonal Antibodies Prepared for use in research and diagnostic tests Exhibit ______________________ for only 1 antigenic determinant Animal (usually mouse) is injected with antigen, and its B cells harvested from spleen Bs are hybridized with cancerous myeloma cells to make them immortal Individual Bs are screened and the one with right antibody selected Allowed to multiply in culture and its clones (________________) are source of large quantity of antibodies Tumor Immunology Tumor cells arise often but are killed by immune system When cancer shows, the immunological surveillance system of T and natural killer cells has __________________ Most tumors are clones whose mitosis is uncontrolled by normal inhibitory mechanisms Tumor cells dedifferentiate Produce surface antigens recognized by immunological _________________ and destroyed Presence of such antigens provides basis of laboratory diagnosis for some cancers Natural Killer (NK) Cells Are lymphocytes related to T cells Provide first line of cell-mediated defense (innate) Have surface ____________________ that help fight viruses, bacteria, parasites and malignant cells NK cells destroy tumors in a non-specific fashion; backed up by specific response of killer Ts Kill with perforins and granzymes Immunotherapy for Cancer Most strategies involve boosting, or directing, patients own immune responses _______________________ and interleukins have been useful in treatment of some forms of cancer Effects of Aging and Stress Little is known about why susceptibility to cancer is so variable Cancer risk increases with age Thymus function declines with age Tumors grow faster in ________________ animals Autoimmune Diseases Are produced by failure of immune system to recognize and tolerate self-antigens Autoreactive T cells are formed and B cells produce _________________ Afflicts women twice as often as men Failure of self-tolerance may be due to: An antigen that does not normally circulate in blood being presented to immune system E.g. in Hashimoto's thyroiditis, antibodies are stimulated to attack _________________ (normally hidden from immune surveillance) Combination of a self-antigen, that is otherwise tolerated, with a foreign hapten E.g. in thrombocytopenia (low platelet count), platelets are destroyed because they combine with victim's medications Antibodies being produced that are directed against other antibodies Happens with _____________________ arthritis Antibodies against foreign antigens cross-reacting with self-antigens This can happen with rheumatic fever Self-antigens being presented to helper T cells together with class-2 MHC molecules This happens in Type I diabetes Immune Complex Diseases Involve formation of immune complexes that are free and not attached to a cell These activate complement proteins and promote ____________________ Can result from infections by bacteria, parasites, viruses Can result from formation of complexes between self-antigens and autoantibodies This occurs in rheumatoid arthritis and lupus Allergy (Hypersensitivity) Is an abnormal immune response to allergens Comes in 2 forms: immediate and ______________________ hypersensitivity Immediate is due to abnormal B cell response to allergen; causes effects in secs to mins Caused by foods, bee stings, pollen Delayed is abnormal T cell response that causes symptoms 24-72 hrs after exposure Immediate Hypersensitivity Dendritic cells stimulate helper Ts; B and plasma cells secrete IgE antibodies IgEs do not circulate in blood; are attached to mast cells and ______________________ When re-exposed to same allegen, IgE bind it and stimulate secretion of histamine Producing allergy symptoms Histamine increases capillary permeability and enhances immune response Delayed Hypersensitivity Symptoms take longer to develop (hrs to days) Is a cell-mediated T cell response Symptoms caused by secretion of _______________________, not histamine Antihistamines provide little benefit Examples include contact dermatitis caused by poison ivy, oak, or sumac Chapter 16: Respiratory Physiology Respiration Includes: ventilation, gas exchange, and O2 utilization (___________ respiration) Ventilation moves air in and out of lungs for gas exchange with blood (external respiration) Gas exchange between blood and tissues, and O2 use by tissues is _______________________ respiration Gas exchange is passive via diffusion Structure of Respiratory System Air passes from mouth to trachea to right and left bronchi to bronchioles to terminal bronchioles to respiratory bronchioles to alveoli Gas exchange occurs in respiratory bronchioles and alveoli ( ___________ zone) All other structures constitute the conducting zone Gas exchange occurs across the 300 million alveoli (60-80 m2 total surface area) Only 2 thin cells are between lung air and blood: 1 alveolar and 1 endothelial cell Alveoli Are polyhedral in shape and clustered at ends of ________________ bronchioles, Air in 1 cluster can pass to others through pores Conducting Zone Warms and humidifies inspired air Mucus lining filters and cleans inspired air Mucus moved by cilia to be expectorated Thoracic Cavity Is created by the ___________________, a dome-shaped sheet of skeletal muscle Contains heart, large blood vessels, trachea, esophagus, thymus, and lungs Intrapleural space is thin fluid layer between visceral pleura covering lungs and ____________________ pleura lining thoracic cavity walls Physical Aspects of Ventilation Ventilation results from pressure differences induced by changes in lung volumes Air moves from higher to lower pressure Compliance, elasticity, and ________________ _______________ of lungs influence ease of ventilation Intrapulmonary and Intrapleural Pressures Visceral and parietal pleurae normally adhere to each other so that lungs remain in contact with chest walls And expand and contract with thoracic cavity Intrapleural space contains a thin layer of lubricating fluid During inspiration, ________________ _________________is about -3 mm Hg pressure; during expiration is about +3 mm Hg Positive transmural pressure (intrapulmonary - intrapleural ) keeps lungs inflated Boyle’s Law (P=1/V) Implies that changes in intrapulmonary pressure occur as a result of changes in lung volume Pressure of gas is _____________________ proportional to volume Increase in lung volume decreases intrapulmonary pressure causing inspiration Decrease in lung volume raises intrapulmonary pressure causing expiration Compliance Is how easily lung expands with pressure Or _______________in lung volume per change in transmural pressure (DV/DP) Is reduced by factors that cause resistance to distension Elasticity Is tendency to return to initial size after distension Due to high content of elastin proteins Elastic tension __________ during inspiration and reduced by recoil in expiration Surface Tension (ST) And elasticity are forces that promote alveolar collapse and resist distension Lungs secrete and absorb fluid, leaving a thin film of fluid on alveolar surface This film causes ST because H20 molecules are attracted to other H2O molecules _________________________________ states that pressure in alveolus is directly proportional to ST; and inversely to radius of alveoli Thus, pressure in smaller alveoli would be greater than in larger alveoli, if ST were same in both Surfactants Consists of phospholipids secreted by ___________________ alveolar cells Lowers ST by getting between H2O molecules, reducing their ability to attract each other via hydrogen bonding Prevents ST from collapsing alveoli Surfactant secretion begins in late fetal life __________________ are often born with immature surfactant system (= Respiratory Distress Syndrome or RDS) Have trouble inflating lungs Mechanics of Breathing Pulmonary ventilation consists of inspiration (= __________________) and ____________________ (= exhalation) By alternately increasing and decreasing volumes of thorax and lungs Quiet Breathing Inspiration occurs mainly because diaphragm contracts, increasing thoracic volume vertically Parasternal and external intercostal contraction contributes a little by raising ribs, increasing thoracic volume laterally Expiration is due to ____________________ recoil Deep Breathing Inspiration involves contraction of extra muscles to elevate ribs: scalenes, pectoralis minor, and __________________________________ muscles Expiration involves contraction of internal intercostals and abdominal muscles Pulmonary Function Test Assessed clinically by spirometry, a method that measures volumes of air moved during inspiration and expiration Anatomical dead space is air in conducting zone where no gas exchange occurs ____________ _____________ is amount of air expired/breath in quiet breathing Vital capacity is amount of air that can be forcefully exhaled after a maximum inhalation = sum of inspiratory reserve, tidal volume, and __________ ___________ Pulmonary Disorders Are frequently accompanied by dyspnea, a feeling of shortness of breath Asthma results from episodes of obstruction of air flow thru bronchioles Caused by inflammation, mucus secretion, and ______________________ Provoked by allergic reactions that release IgE, by exercise, by breathing cold, dry air, or by aspirin _____________________ is a chronic, progressive condition that destroys alveolar tissue, resulting in fewer, larger alveoli Reduces surface area for gas exchange and ability of bronchioles to remain open during expiration Collapse of bronchiole during expiration causes ____________________, decreasing gas exchange Commonly occurs in long-term smokers Chronic Obstructive Pulmonary Disease (COPD) Chronic Obstructive Pulmonary Disease (COPD) involves chronic inflammation accompanied by narrowing of airways and destruction of alveolar walls Most people with COPD are ___________________ Factors Affecting Gas Exchange Partial pressure is pressure that a particular gas in a mixture exerts independently Dalton’s Law states that total pressure of a gas mixture is the __________ of partial pressures of each gas in mixture Atmospheric pressure at sea level is 760 mm Hg PATM = PN2 + PO2 + PCO2 + PH2O = 760 mm Hg Gas Exchange in Lungs Is driven by differences in partial pressures of gases between alveoli and _______ Is facilitated by enormous surface area of alveoli, short diffusion distance between alveolar air and capillaries, and tremendous density of capillaries Partial Pressure of Gases in Blood Henry’s Law says blood O2 depends on _____________ of O2, blood temperature (constants), and partial pressure of O2 (PO2), which varies with _____________ Blood PO2 and PCO2 Measurements At normal PO2 arterial blood has about 100 mmHg PO2 PO2 is about 40 mmHg in systemic veins PCO2 is 46 mmHg in systemic veins Pulmonary Circulation _______________ of blood flow through pulmonary circuit equals flow through systemic circulation Pulmonary arterioles constrict where alveolar PO2 is low and dilate where high This matches ____________________ to perfusion Lung Ventilation/Perfusion ratios Normally, alveoli at apex of lungs are underperfused and overventilated Alveoli at base are overperfused and underventilated Control of Ventilation Brain Stem Respiratory Centers Automatic breathing is generated by a _________________ _________________ in medulla oblongata Consists of inspiratory neurons that drive inspiration and expiratory neurons that inhibit inspiratory neurons Pons Respiratory Centers Inspiratory neurons stimulate spinal motor neurons that innervate respiratory muscles Expiration is passive and occurs when _______________________ are inhibited Chemoreceptors Automatic breathing is influenced by activity of chemoreceptors that monitor blood PCO2, PO2, and pH Central chemoreceptors are in medulla Peripheral chemoreceptors are in large arteries near heart (____________ bodies) and in carotids (carotid bodies) Effects of Blood PCO2 and pH on Ventilation Chemoreceptors modify ventilation to maintain normal CO2, O2, and pH levels PCO2 is most _________________ because of its effects on blood pH H2O + CO2 H2CO3 H+ + HCO3 Hyperventilation causes low CO2 (hypocapnia) Hypoventilation causes high CO2 (hypercapnia) Brain chemoreceptors are responsible for greatest effects on ventilation H+ can't cross BBB but ______________ can, which is why it is monitored and has greatest effects Peripheral chemoreceptors do not respond to PCO2, only to H+ levels Effects of Blood PO2 on Ventilation Low blood PO2 (_________________) has little effect on ventilation Influences chemoreceptor sensitivity to PCO2 PO2 has to fall to about half normal b4 ventilation is significantly affected Emphysema blunts chemoreceptor response to PCO2 Often ventilation is stimulated by _______ drive rather than PCO2 Hemoglobin (Hb) and O2 Transport Loading of Hb with O2 occurs in lungs; unloading in tissues Each Hb has 4 ____________ polypeptide chains and 4 heme groups that bind O2 Each heme has a ferrous ion that can bind 1 O2 So each Hb can carry 4 O2s Most O2 in blood is bound to Hb inside RBCs as ______________________ Each RBC has about 280 million molecules of Hb Hb greatly increases O2 carrying capacity of blood Methemoglobin contains ferric iron (Fe3+) -- the oxidized form Lacks electron to bind with O2 Blood normally contains a small amount Carboxyhemoglobin is heme combined with _____________________________ Bond with carbon monoxide is 210 times stronger than bond with oxygen So heme can't bind O2 O2-carrying capacity of blood depends on its Hb levels In __________________, Hb levels are below normal In polycythemia, Hb levels are above normal Hb production controlled by erythropoietin (EPO) Production stimulated by low PO2 in kidneys Hb levels in men are ____________ because androgens promote RBC production High PO2 of lungs favors loading; low PO2 in tissues favors unloading Oxyhemoglobin Dissociation Curve Reflects loading and unloading of O2 Affinity decreases when pH decreases (_________ _________)or temp increases Occurs in tissues where temp, CO2 and acidity are high Effects of 2,3 DPG on O2 Transport RBCs have no mitochondria; can’t perform aerobic respiration __________________ is a byproduct of glycolysis in RBCs Its production is increased by low O2 levels Fetal hemoglobin (HbF) has 2 g-chains in place of b-chains of HbA HbF can’t bind DPG, causing it to have higher O2 affinity Facilitates O2 transfer from mom to baby Sickle-cell Anemia Sickle-cell anemia affects 8-11% of __________________ Americans HbS has valine substituted for glutamic acid at 1 site on b chains At low PO2, HbS crosslinks to form a “gel” inside RBCs Makes RBCs less flexible and more _____________ Thalassemia Thalassemia affects primarily people of Mediterranean descent Has decreased synthesis of a or b chains; increased synthesis of g chains Myoglobin Is a red pigment found exclusively in ___________________ muscle Slow-twitch skeletal and cardiac muscle fibers are rich in myoglobin Has only 1 globin; binds only 1 O2 Has higher ______________ for O2 than Hb; is shifted to extreme left Releases O2 only at low PO2 Serves in O2 storage, particularly in heart during systole CO2 Transport and Acid-Base Balance CO2 transported in blood as dissolved CO2 (10%), carbaminohemoglobin (20%), and bicarbonate ion, HCO3-, (________) In RBCs carbonic anhydrase catalyzes formation of H2CO3 from CO2 + H2O Chloride Shift High CO2 levels in tissues Results in high H+ and HCO3- levels in RBCs HCO3- diffuses down conc and charge gradient into blood causing RBC to become more _____________________ So Cl- moves into RBC (chloride shift) Reverse Chloride Shift In lungs, CO2 is breathed out Binding of O2 to Hb decreases its affinity for H+ H+ combines with HCO3- and more CO2 is formed Cl- diffuses down conc and charge gradient out of RBC (___________________) Acid-Base Balance in Blood Blood pH is maintained within narrow pH range by lungs and kidneys (normal = 7.4 ) Most important _________________ in blood is bicarbonate H2O + CO2 H2CO3 H+ + HCO3 Excess H+ is buffered by HCO3 Kidney's role is to excrete H+ into urine 2 major classes of acids in body: A ________________________ can be converted to a gas E.g. CO2 in bicarbonate buffer system can be breathed out H2O + CO2 H2CO3 H+ + HCO3 All other acids are nonvolatile and cannot leave blood E.g. lactic acid, fatty acids, ketone bodies ______________________ is when pH < 7.35; alkalosis is pH > 7.45 Respiratory acidosis caused by hypoventilation Causes rise in blood CO2 and thus carbonic acid Respiratory alkalosis caused by _____________________________ Results in too little CO2 Metabolic acidosis results from _________________ of nonvolatile acids E.g. excess ketone bodies in diabetes or loss of HCO3- in diarrhea Metabolic alkalosis caused by too much HCO3- or too little nonvolatile acids (e.g. from vomiting out stomach acid) Normal pH is obtained when ratio of HCO3- to CO2 is _____________ Henderson-Hasselbalch equation uses CO2 and HCO3- levels to calculate pH: pH = 6.1 + log [HCO3-] [0.03PCO2] Respiratory Acid-Base Balance Ventilation usually adjusted to ____________ rate to maintain normal CO2 levels With hypoventilation not enough CO2 is breathed out in lungs Acidity builds, causing respiratory acidosis With hyperventilation too much CO2 is breathed out in lungs _________________ drops, causing respiratory alkalosis Exercise and Altitude Effects Ventilation During Exercise During exercise, arterial PO2, PCO2, and pH remain fairly constant During exercise, breathing is deeper and faster, more air going to lungs (________________________) With neurogenic mechanism, sensory activity from exercising muscles stimulates ventilation; With ______________ mechanism, either PCO2 and pH may be different at chemoreceptors than in arteries Chapter 17: Physiology of the Kidneys Kidney Functions Regulate plasma and __________________________fluid Thru urine formation, kidneys regulate: Volume of blood plasma, Waste products in blood Concentration of electrolytes, Plasma pH Structure of Kidneys Paired kidneys are on either side of the vertebral column and below the diaphragm. About the size of fist ________________ contains many capillaries and outer parts of nephrons Medulla consists of renal pyramids separated by renal columns Pyramid contains minor calyces which unite to form a major calyx Major calyces form renal pelvis which conducts urine to ureters and into bladder Bladder has a smooth muscle wall, ______________________ muscle Stretch can cause spontaneous APs and contraction Also innervated and controlled by parasympathetic Nephron Is __________________ unit of kidney; forms urine. >1 million nephrons/kidney Is a long tube and has associated blood vessels Blood enters kidney through renal artery, interlobar arteries, arcuate arteries and then interlobular arteries give rise to afferent arterioles which supply glomeruli A mass of capillaries in ___________________________ capsule producing filtrate into nephron tubule Efferent arteriole drains glomerulus into peritubular capillaries (vasa recta) Blood from peritubular capillaries enters veins Nephron Tubules Glomerular capsule leads into _______________________ convoluted tubule (PCT), to descending and ascending limbs of Loop of Henle (LH), and ___________________ convoluted tubule (DCT) Tubule ends where it empties into collecting duct (CD) Glomerular (Bowman’s) Capsule Surrounds glomerulus. Together they form renal _______________________ Is where glomerular filtration occurs. Filtrate passes into PCT Proximal Convoluted Tubule Walls consist of single layer of cuboidal cells with millions of microvilli Which increase surface area for ______________________________ Type of Nephrons Cortical nephrons originate in outer 2/3 of cortex Juxtamedullary nephrons originate in inner 1/3 cortex. Have long LHs Glomerular Filtration Glomerular capillaries and Bowman's capsule form a filter for blood Glomerular Caps are fenestrated—allows any plasma molecule to pass Filtrates pass through narrow _________________________________ between pedicels (foot processes) of podocytes of glomerular capsule Plasma proteins are mostly excluded from the filtrate because of large size and negative charge Some protein (albumin) normally enters the filtrate but most is reabsorbed Defects in slit diaphragm allows protein in the urine (__________) Glomerular Ultrafiltrate Is fluid that enters glomerular capsule, whose filtration was driven by bld pressure Glomerular Filtration Rate Is _________________________ of filtrate produced by both kidneys/min Averages 115 ml/min in women; 125 ml/min in men Totals about 180L/day (45 gallons. Most filtered water must be reabsorbed Regulation of GFR Is controlled by extrinsic and intrinsic (autoregulation) mechanisms Constriction/dilation of _____________________ arterioles affects rate of blood flow to glomeruli & GFR Sympathetic Effects: Sympathetic activity ______________________ afferent arteriole Helps maintain BP and shunts blood to heart and muscles Renal Autoregulation Allows kidney to maintain a _________________ GFR over wide range of BPs When average BP drops to 70 mm Hg afferent arteriole dilates When average BP increases, afferent arterioles constrict Is also maintained by negative feedback between afferent arteriole and volume of filtrate _________________________________ feedback) Increased flow of filtrate sensed by macula densa in thick ascending LH Signals afferent arterioles to constrict Functions of Nephron Segments Reabsorption of Salt and H2O PCT returns most molecules and H2O in filtrate back to _____________________ capillaries About 180L/d of ultrafiltrate produced; only 1–2L of urine excreted/24h Urine volume varies according to needs of body Minimum of 400 ml/day urine necessary to excrete metabolic wastes (______________________________________) Return of filtered molecules is called reabsorption Water is never transported Other molecules are transported and water follows by ________________ Significance of PCT Reabsorption ~65% Na+, Cl-, and H2O is reabsorbed in PCT and returned to bloodstream An additional 20% is reabsorbed in descending loop of Henle The other 15% is reabsorbed variably, depending on level of ___________ Descending Limb LH Is permeable to H2O. Is impermeable to, and does not ___________________ salt H2O diffuses out of filtrate and is reabsorbed by capillaries Ascending Limb LH Impermeable to H2O; permeable to salt; thick part ATs salt out of filtrate AT of salt causes filtrate to become ___________________ by end of LH Countercurrent Multiplier System Countercurrent flow and proximity allow descending and ascending limbs of LH to interact and build ____________________________ in medulla Salt pumping in thick ascending part raises osmolality around descending limb, causing more H2O to diffuse out of filtrate Vasa Recta: Is important component of countercurrent multiplier Permeable to salt, H2O (via aquaporins), and ___________________ Reabsorbs H2O coming out of descending limb Descending area has urea _______________________. Ascending area has fenestrated capillaries Effects of Urea Urea contributes to high osmolality in medulla Deep region of collecting duct is _____________ to urea and transports it Collecting Duct (CD): Plays important role in water conservation Is impermeable to salt in medulla. Permeability to H2O depends on levels of ADH ADH Is secreted by post pituitary in response to dehydration Stimulates insertion of ___________________________ (water channels) into plasma membrane of CD When ADH is high, H2O is drawn out of CD by hi osmolality of interstitial fluid Renal Clearance Ability of kidney to remove substances from blood and excrete them in urine Occurs by filtration and by _________________________ Reabsorption decreases renal clearance; secretion increases clearance ____________________ rate = (filtration rate + secretion rate) - reabsorption rate Secretion of Drugs Many drugs, toxins, metabolites are secreted by membrane transporters in PCT Many ______________________ molecules (xenobiotics) are eliminated by this system at a more rapid rate than by glomerular filtration Inulin Measurement of GFR Inulin, a fructose polymer, is useful for measuring GFR because is neither reabsorbed nor secreted. Amount filtered ___________ amount excreted Renal Plasma Clearance (RPC) Vol. of plasma from which a subst is _______________________ removed/min by urine excretion If subst is filtered but not reabsorbed then all filtered will be excreted RPC = GFR If substance is filtered and reabsorbed then RPC ___________ GFR If substance is filtered but also secreted and excreted then RPC will be > GFR (=120 ml/ min) RPC = V x U/P Clearance of Urea Urea is __________________ filtered into glomerular capsule Urea clearance is 75 ml/min, compared to clearance of inulin (120 ml/min) Thus 40-60% of filtered urea is always reabsorbed Measurement of Renal Blood Flow ___________________ of blood in glomerulus is filtered Rest passes into efferent arteriole and back into circulation Substances not filtered can still be cleared by AT (secretion) into tubules Total Renal Blood Flow Using PAH PAH clearance is used to measure ________________ renal blood flow Normally averages 625 ml/min It is totally cleared by ______________________ pass through a nephron So it must be both filtered and secreted Total renal blood flow = PAH clearance/0.55 Glucose and Amino Acid Reabsorption Filtered glucose and amino acids are normally _________ reabsorbed from filtrate Occurs in PCT by carrier-mediated cotransport with Na+ Glycosuria Is presence of glucose in urine Occurs when glucose > 180-200mg/100ml plasma ( renal ___________________ Glucose is normally absent because plasma levels stay below this value Hyperglycemia has to exceed renal plasma threshold Diabetes mellitus occurs when hyperglycemia results in ______________ Electrolyte Balance Kidneys regulate Na+, K+, H+, HCO3-, Cl-, & PO4-3, match excretion to ingestion Role of Aldosterone in Na+/K+ Balance 90% filtered Na+ and K+ reabsorbed before DCT Regulated by _________________ (controls K+ secretion and Na+ reabsorption) K+ Secretion Is only way K+ ends up in urine Is directed by aldosterone and occurs in DCT and cortical CD High K+ or low Na+ will increase aldosterone and K+ secretion Juxtaglomerular Apparatus Specialized region in nephron where afferent arteriole & ________________ ascending limb meet Renin-Angiotensin-Aldosterone Stsyem Is activated by release of renin from __________________ cells within afferent arteriole Renin converts angiotensinogen to angiotensin I which is converted to Angio II by angiotensin-converting enzyme (ACE) in lungs Angio II stimulates release of aldosterone Regulation of Renin Secretion Inadequate intake of NaCl always causes _____________________blood volume Because lower osmolality inhibits ADH, causing less H2O reabsorption Low blood volume and renal blood flow stimulate renin release Macula Densa Cells respond to levels of Na+ in filtrate Inhibit ________________ secretion when Na+ levels are high Causing less aldosterone secretion, more Na+ excretion Atrial Natriuretic Peptide (ANP) Is produced by atria due to stretching of walls. Acts opposite to aldosterone Stimulates salt and H2O ____________________. Acts as an endogenous diuretic Renal Acid-Base Regulation Kidneys help regulate blood pH by excreting H+ and/or reabsorbing HCO3 Most H+ secretion occurs across PCT wall in exchange for Na+, Na+/H+ antiporter Normal urine is acidic (____________), kidneys reabsorb almost all HCO3- & excrete H+ Reabsorption of HCO3- in PCT When urine is _________________, HCO3- combines with H+ to form H2CO3, catalyzed by CA H2CO3 splits into HCO3- and H+ ; HCO3- diffuses into blood Urinary Buffers Nephron _______________ produce urine with pH < 4.5 Excretes more H+ by buffering H+s with HPO4-2 or NH3 before excretion Diuretics: Used to ______________ blood volume in hypertension, congestive heart failure, or edema Increase volume of urine by increasing proportion of glomerular filtrate that is excreted ______________ diuretics are most powerful; inhibit AT salt in thick ascending limb of LH Kidney Diseases In acute renal failure, kidney function is impaired Rise in blood creatinine and ____________________ in RPC of creatinine In renal insufficiency, nephrons have been destroyed as a result of a disease Clinical manifestations include salt and H2O retention and uremia (high plasma urea levels) Treatment includes _________________________ Urea and other wastes are removed Chapter 18: The Digestive System Functions of GI Tract Motility: Is movement of food through GI tract by means of: Ingestion--taking food into mouth Mastication--chewing food and mixing it with saliva ___________________--swallowing food Peristalsis--rhythmic wave-like contractions move food through GI tract Secretions: Includes release of exocrine and endocrine products into GI tract Exocrine secretions include: HCl, H2O, HCO3-, _____________, lipase, pepsin, amylase, Endocrine includes hormones secreted into stomach and small intestine to help regulate GI system. E.g. gastrin, secretin, CCK, GIP, GLP-1, guanylin, ______. Absorption: Is passage of digested end products into blood or lymph Storage & Elimination: Temp storage and elimination of indigestible components of food Digestive System Is composed of GI tract (alimentary canal) and accessory digestive organs GI tract is 30 ft long; extends from mouth to anus Organs include oral cavity, pharynx, esophagus, ________________, small & large intestine Accessory organs are teeth, tongue, salivary glands, liver, gallbladder, & pancreas Layers of GI Tract are called tunics: mucosa, submucosa, muscularis, and serosa Mucosa: Is the absorptive and secretory layer lining lumen of GI tract Highly folded with villi to increase _____________________ area Contains lymph nodules, mucus-secreting goblet cells, and thin layer of muscle Submucosa: Is a thick, highly vascular layer of connective tissue where absorbed molecules enter blood and lymphatic vessels Contains _________________ & nerve plexuses that carry ANS activity to muscularis mucosae Muscularis: Is for segmental contractions and peristaltic movement through GI Has an inner circular and outer longitudinal layer of smooth muscle These layers move food through tract while pulverizing and mixing it _______________________ plexus between these layers is major nerve supply to GI tract Serosa: Is outermost layer; serves to bind and protect Consists of areolar connective tissue with layer of simple squamous epithelium From Mouth to Stomach Mastication (chewing) mixes food with saliva which contains salivary _________ An enzyme that catalyzes partial digestion of starch Deglutition (swallowing) begins as voluntary activity Oral phase is voluntary and forms a food ___________ Pharyngeal and esophageal phases are involuntary and cannot be stopped Larynx is raised so that epiglottis covers entrance to respiratory tract Esophagus connects pharynx to stomach Upper third is skeletal muscle, then mixture of skeletal and smooth Last portion has only smooth, passes thru diaphragm via esophageal hiatus _________________ propels food thru GI tract (wave-like muscular contractions) Food in stomach, the gastroesophageal sphincter constricts, stops reflux Stomach: Is most distensible part of GI tract; Empties into the duodenum For food storage, initial digestion of proteins; killing bacteria with high acidity; moving soupy food mixture (_____________) into intestine Is enclosed by gastroesophageal sphincter on top and pyloric sphincter on bottom Is divided into 3 regions: Fundus, Body, Antrum Inner surface of stomach is highly folded into _____________________ Contractions of stomach churn chyme, mixing it with gastric secretions Gastric mucosa has gastric pits in its folds Cells that line folds deeper in the mucosa, are exocrine _____________________ Gastric glands contain cells that secrete different products that form gastric juice Goblet cells secrete mucus Parietal cells secrete HCl &intrinsic factor (for B12 absorption in intestine __________________________ secrete pepsinogen (precursor for pepsin) Enterochromaffin-like cells secrete histamine and serotonin G cells secrete gastrin; D cells secrete somatostatin HCl in Stomach Is secreted in response to the hormone gastrin; and ACh from vagus Both stimulate release of histamine causing parietal cells to secrete HCl Makes gastric juice very acidic; ___________________________ proteins to make them more digestible Converts pepsinogen into pepsin; Pepsin is more active at low pHs Digestion and Absorption in Stomach Proteins are partially digested by pepsin _________________ digestion by salivary amylase is soon inactivated by acidity Alcohol and aspirin are the only commonly ingested substances that are absorbed Gastric and Peptic Ulcers Peptic ulcers: erosions of mucous membranes of stomach or duodenum by _____ Helicobacter pylori infection is associated with ulcers; Antibiotics are useful Small Intestine Longest part of GI ; appr.3m long; Duodenum: 1st 25cm after pyloric sphincter _________________ is next 2/5s; Ileum is last 3/5s; empties into large intestine Absorption of digested food occurs in SI; Helped by long length and surface area Surface area increased by foldings and projections; Large folds: plicae circulares Micr. finger-like projections are villi; Apical hair-like projections are __________ Each villus is covered with columnar epithelial cells interspersed with goblet cells Epithelial cells of villi exfoliate and replaced by mitosis in crypts of Lieberkuhn Inside each villus are lymphocytes, capillaries, and _______________________ Hair-like microvilli projecting from surface of epithelial cell create a brush border Intestinal Enzymes attached to microvilli are brush border enzymes not secreted in lumen Enzyme active sites are exposed to chyme Intestinal Contraction and Motility Peristalsis is weak and slow; pyloric end pressure greater than distal end _____________________________ is major contractile activity of SI Is contraction of circular smooth muscle to mix chyme Large Intesine (LI) or Colon Has no digestive function; absorbs H2O, electrolytes, folic acid, B and K vitamins, Has no ______________or________________; has microflora of about 400 sps of commensal bacteria which produce folic acid and vitamin K and ferment indigestible food fatty acids Extends from ileocecal valve at end of SI to anus; bulges to form pouches (haustra Chyme enters cecum, ascending, transverse, descending, sigmoid colon, rectum, Fluid and Electrolyte Absorption in LI SI absorbs most water but LI absorbs __________ of water it receives, by osmosis Salt and water reabsorption stimulated by aldosterone LI can also secrete H2O via AT of NaCl into intestinal lumen Defeacation After electrolytes and water have been absorbed, waste material passes to rectum, creating urge to defecate Liver Liver is the largest internal organ __________________________ form hepatic plates that are 1–2 cells thick Plates are separated by sinusoids which are fenestrated and permeable even to proteins. Contain phagocytic ______________________ cells A damaged liver can regenerate itself from mitosis of surviving hepatocytes In some cases, such as alcohol abuse or viral hepatitis, regeneration does not occur. Can lead to liver fibrosis and ultimately _________________ Hepatic Portal System Food absorbed in SI is delivered 1st to liver Capillaries in digestive tract drain into the _________________ ______ vein which carries blood to liver. Hepatic vein drains liver. Liver also receives blood from hepatic artery Liver __________________ are functional units formed by hepatic plates In middle of each is central vein. At edge of each lobule are branches of hepatic portal vein and artery which open into sinusoids Bile is secreted by hepatocytes into bile canaliculi which empty into ________ ________________ which flow into hepatic ducts that carry bile away from liver Functions of the Liver Bile production and secretion amounts to 250–1500 ml/day ____________________ (bilirubin) is produced in spleen, bone marrow, and liver Is a derivative of heme groups (minus iron) from Hb Detoxification of Blood Liver can remove hormones, drugs, and other biologically active molecules from blood by: Excretion into bile. _______________________ by Kupffer cells Chemical alteration of molecules: Liver converts ammonia to urea Secretion of Glucose, Triglycerides, and Ketones Liver helps regulate blood glucose by removing it from or releasing it to blood Removes it via glycogenesis and lipogenesis Or produces it via __________________________ and gluconeogenesis Can convert free fatty acids into ketone bodies (ketogenesis) Production of Plasma Proteins ___________________ makes up 70% of total plasma protein and contributes most of the colloid osmotic pressure of blood Globulins transport cholesterol and hormones, and are involved in blood clotting Gallbladder and Pancreas Is a sac-like organ on inferior surface of liver, stores and conc bile from liver When SI is empty, sphincter of Oddi in common bile duct closes and bile is forced into ___________________. Expands as it fills with bile When food is in SI, sphincter of Oddi opens, gall bladder contracts, and bile is ejected thru cystic duct into common bile duct then to duodenum Pancreas Is located behind stomach. Has both endocrine and exocrine functions Endocrine function performed by ________________________________ Secretes insulin and glucagon Exocrine secretions include bicarbonate solution and digestive enzymes Pass in pancreatic duct to SI. Exocrine secretory units are _______ Pancreatic Juice Contains water, bicarbonate, and digestive enzymes Digestive enzymes include amylase for starch, _____________ for proteins and lipase for fats Most pancreatic enzymes are produced in inactive form (zymogens) Trypsin is activated by brush border enzyme, enterokinase, Trypsin activates others Neural and Endocrine Regulation ___________nerve is heavily involved in regulating and coordinating digestive activities Endocrine hormones include secretin, gastrin, CCK, and GIP Regulation of Gastric Function Gastric motility and secretion occur automatically Extrinsic control of gastric fxn includes cephalic, gastric, and intestinal phases Cephalic Phase: Refers to control by brain of vagus activity Stimulated by sight, smell, and taste of food Activation of vagus causes: Chief cells to secrete pepsinogen; G cells to secrete gastrin Indirectly stimulates parietal cells to secrete HCl Gastric Phase: Arrival of food in stomach stimulates gastric phase Gastric secretion caused by distension of stomach and chemical nature of chyme Short pp and aa stimulate G cells to secrete gastrin and chief cells -___________; Secretion of HCl is also regulated by a negative feedback mechanism: HCl secretion decreases if pH < 2.5; at pH 1 gastrin secretion stops Intestinal Phase Begins when chyme enters the SI This causes a neural reflex that inhibits gastric __________________ and secretion Enteric Nervous System Peristalsis is controlled by enteric NS ACh and substance P stimulate smooth muscle contraction above bolus NO, VIP, and ATP stimulate smooth muscle relaxation below bolus Secretion of Pancreatic Juice Secretion of pancreatic juice and bile is stimulated by ______________ and ____ Secretin is secreted in response to duodenal pH < 4.5 CCK is secreted in response to fat and protein content of chyme in duodenum Stimulates production of __________________ enzymes Digestion and Absorption of Carbohydrates Most CH2O are ingested as starch Salivary amylase begins starch digestion Pancreatic amylase converts starch to _________________________ Oligosaccharides hydrolyzed by SI brush border enzymes Digestion and Absorption of Protein Begins in stomach when pepsin digests proteins to form polypeptides __________________ (trypsin, chymotrypsin,) cleave peptide bonds inside of pp Exopeptidases (carboxypeptidase, aminopeptidase) cleave ends of polypeptides Protein digestion in SI results in free amino acids, dipeptides, and tripeptides Which are transported into SI cells where di- and tripeptides are broken down to amino acids and are secreted into blood Digestion and Absorption of Lipids Occurs in SI. Arrival of lipids in duodenum causes secretion of bile Fat is __________________ by bile salt micelles Forms tiny droplets of fat dissolved in bile salt micelles Greatly increases surface area for fat digestion Pancreatic lipase hydrolyzes triglycerides to free fatty acids and monoglycerides __________________ breaks down phospholipids into fatty acids and lysolecithin Products of fat digestion dissolve in micelles forming mixed micelles Free fatty acids, monoglycerides, and lysolecithin leave micelles and enter epithelial cells Inside epithelial cells, they are _________________________ into triglycerides and phospholipids Triglycerides and phospholipids combine with protein to form small particles called _________________________ Which are secreted into central lacteals of SI villi Cholesterol and triglycerides from liver form VLDLs which take triglycerides to cells Once triglycerides are removed, VLDLs become LDLs LDLs transport __________________ to organs and blood vessels HDLs transport excess cholesterol back to liver High ratio of HDL-cholesterol to total cholesterol is believed to confer protection against _____________________________ Chapter 19: Regulation of Metabolism Nutritional Requirements Living tissue is maintained by constant expenditure of energy (ATP) ATP derived from glucose, fatty acids, ketones, amino acids, and others ____________________ of food is commonly measured in kilocalories (1 kcal = 1000 calories) Carbohydrates and proteins yield 4kcal/gm; fats-9kcal/gm Metabolic Rate and Caloric Requirements Metabolic rate (MR) is total rate of body metabolism = amount of __________________ consumed by body/min Basal metabolic rate (BMR) is MR of awake relaxed person 12–14 hrs after eating and at a comfortable temperature BMR depends on age, sex, body surface area, _____________________ level, and thyroid hormone levels Hyperthyroids have high BMR; hypothyroids have low BMR Metabolism Is all chemical reactions in body Includes synthesis and energy storage reactions (____________________); and energy liberating reactions (________________________) Anabolic Requirements Anabolic reactions synthesize DNA and RNA, proteins, fats, and carbohydrates Must occur constantly to replace molecules that are hydrolyzed in catabolic reactions Turnover Rate Is rate at which a molecule is broken down and ________________________ Average turnover for Carbs is 250 g/day Some glucose is reused so net need ~150 g/day Average turnover for protein is 150 g/day Some is reused for protein synthesis so net need ~35 g/day 9 _______________________ amino acids must be supplied in diet because can't be synthesized Average turnover for fats is 100 g/day Little is required in diet because can be synthesized from ___________ 2 essential fatty acids must be supplied in diet Vitamins Are small organic molecules that serve as coenzymes in metabolism or have highly specific functions Must be obtained in diet because body does not produce them, or does so in insufficient amounts Can be placed in 2 classes ___________-solubles include A, D, E, and K _____________-solubles include B1, B2, B3, B6, B12, pantothenic acid, biotin, folic acid, and vitamin C Serve as coenzymes in metabolism Minerals (Elements) Are needed as _______________ for specific enzymes and other critical functions Sodium, potassium, magnesium, calcium, phosphate, and chloride are needed daily in large amounts Iron, zinc, manganese, fluorine, copper, molybdenum, chromium, and selenium are ________________ elements required in small amounts/day Free Radicals Are highly reactive and oxidize or reduce other atoms Because they have an ____________________ electron in their outer orbital The major free radicals are reactive oxygen or reactive nitrogen species NO radical, superoxide radical, and hydroxyl radical Serve important physiological functions Help to destroy bacteria Can produce vasodilation Can stimulate cell proliferation In excess can exert __________________________ contributing to disease states Can damage lipids, proteins, and DNA Promote apoptosis, aging, inflammatory disease, degenerative, and malignant growth Body uses enzymatic and nonezymatic means to protect itself against oxidative stress Enzymes like ____________________ neutralize free radicals Nonenzymes like vitamin C and E react with free radicals Regulation of Energy Metabolism Blood contains glucose, fatty acids, amino acids, and others that can be used for energy _____________________ energy substrates Control of Adipose Tissue Levels Body appears to have negative feedback loops (an adipostat) to maintain a certain amount of adipose tissue Adipose cells (adipocytes) store and release fat under ________________ control And may release their own hormone(s) to influence metabolism Development of Adipose Tissue Number of adipocytes increases greatly after birth Differentiation promoted by high levels of ___________________ Endocrine Functions of Adipocytes Adipocytes secrete regulatory hormones called adipokines Regulate hunger, metabolism, and insulin sensitivity The adipocyte hormones TNFa, resistin, retinol BP4, and leptin are increased in ____________________ and Type II diabetes Leptin signals the hypothalamus on how much fat is stored, thereby regulating hunger and food intake Low Adiposity: Starvation Starvation and malnutrition diminish immune function Low adipose levels cause low leptin levels _________________________ cells have leptin receptors Low leptin thus diminishes immune function Leptin may play role in timing of puberty and in the amenorrhea of underweight women Obesity Childhood obesity involves increases in both size and number of adipocytes Weight gain in adulthood is due mainly to _________________ in adipocyte size Obesity is often diagnosed by using using a body mass index (BMI) BMI = w/h2 w = weight in kilograms, h = height in meters Healthy weight is BMI between 19 – 25 Obesity defined as BMI > 30 60% of pop in US is either ___________________ (BMI>25) or obese (BMI>30) Regulation of Hunger Is at least partially controlled by hypothalamus Involves a number of NTs: endorphins (promote overeating), Norepi (promotes overeating), serotonin (____________________ overeating) Calorie Expenditure of body Has 3 components: Number of calories used at the BMR make up 60% of total Number used in response to temperature changes and during digestion/ absorption (adaptive ______________________) make-up 10% of total Starvation can lower MR 40%; eating raises MR 25-40% (thermic effect of food) Number used during physical activity depends on type and intensity Absorptive and Post absorptive States Absorptive state is ______ hr period after eating Energy substrates from digestion are used and deposited in storage forms (anabolism) Postabsorptive or fasting state follows absorptive state Energy is ___________________ from storage (catabolism) Hormonal Regulation of Metabolism Balance between anabolism and catabolism depends on levels of insulin, glucagon, GH, thyroxine, and others Pancreatic Islets of Langerhans Contain 2 cell types involved in energy homeostasis: α cells secrete _____________________ when glucose levels are low Increases glucose by stimulating glycogenolysis in liver β cells secrete insulin when glucose levels are high Reduces blood glucose by promoting its uptake by tissues Insulin and Glucagon Secretion Normal ______________________ glucose level is 65–105 mg/dl Insulin and glucagon normally prevent levels from rising above 170mg/dl after meals or falling below 50mg/dl between meals Insulin Overall effect is to promote anabolism Promotes storage of digestion products ____________________ breakdown of fat and protein Inhibits secretion of glucagon Stimulates insertion of GLUT4 transporters in cell membrane of skeletal muscle, liver, and fat Transports by _______________________ diffusion Oral Glucose Tolerance Test Measures response to drinking a glucose solution Assesses ability of β cells to secrete insulin and insulin's ability to ____________________ blood glucose In non-diabetics, glucose levels return to normal within 2 hrs Glucagon Maintains blood glucose concentration above 50mg/dl Stimulates glycogenolysis in liver Stimulates _________________________, lipolysis, and ketogenesis Skeletal muscle, heart, liver, and kidneys use fatty acids for energy