Isolation of genomic DNA from whole blood
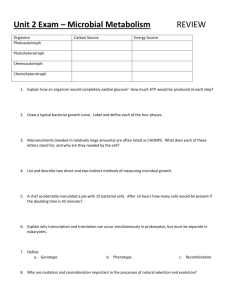
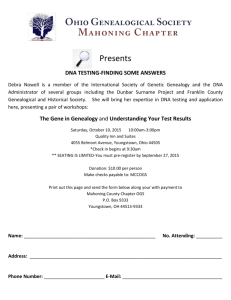
advertisement

COLORECTAL CANCER FAMILY REGISTRY UNIVERSITY OF SOUTHERN CALIFORNIA NORRIS CANCER CENTER 1 COLORECTAL CANCER FAMILY REGISTRY UNIVERSITY OF SOUTHERN CALIFORNIA NORRIS CANCER CENTER __________________________________________ _ PROTOCOL MANUAL for HANDLING OF BIOLOGICAL SPECIMENS BIOSPECIMEN PROCESSING Banking Flow Chart Biospecimen Availability A. Peripheral blood Flow Chart About blood collection Guideline for receiving blood After the blood arrives Summary 1. Blood Spot Preparation 2. Plasma and Buffy Coat Separation 3. Ficoll Separation B. Frozen tissue C. Paraffin-embedded tissue D. Others: Buccal Smears, etc. Supplies FINAL CELLULAR AND GENETIC MATERIAL PREPARATION A. DNA 1. from fresh whole blood 2. from buffy coat 3. from dry blood stains 4. from frozen tissue 5. from paraffin-embedded tissue 6. from others (plasma, urine, buccal smear...) B. RNA 1. from fresh whole blood 2. from buffy coat 3. from cells C. Lymphoblastoid cell line Supplies Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 2 University of Southern California, Department of Preventive Medicine Revised Nov 23, 1998 AD 3 STORAGE, PACKING AND SHIPPING A. Storage Location of all storage Preventive maintenance B. Packing and shipping Supplies SPECIMEN DATABASE A. Scheme for specimen ID assignment B. Scheme for location assignment of biospecimens C. Biospecimen labeling guideline D. Biospecimen data records and report E. Biospecimen database tables Supplies QUALITY CONTROL Summary of Routine QC for all specimens A. Routine QC for DNA B. Routine QC for RNA C. Routine QC for Cell Cultures D. Special QC for DNA E. QC Exchange Plan General Protocol for Lab QC and QA Supplies STANDARDIZED LAB WORKSHEETS USC COORDINATING LABORATORY SETUP A. Resource and Environment B. Safety Requirement 1. Biosafety 2. Radiation safety C. Contamination Control 1. For PCR-based experiment 2. For RNA-based experiment 3. For tissue culture work D. USC Safety Resource REFERENCES Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Nov 23, 1998 AD 4 BIOSPECIMEN PROCESSING 5 Biological Specimen Banking for the COLORECTAL CANCER FAMILY REGISTRY STUDY SUBJECTS DNA back up source: Buccal swabs... Peripheral Blood Archival specimens Paraffin blocks or slides EDTA, purple Blood spots Store at room temperature DNA ACD, yellow Centrifugation Plasma Buffy Coat preparation preparation Ficoll separation of white blood cells Store in liquid nitrogen Lymphoblastoid Cell Lines Freeze at -70 degrees centigrade PLASMA Colorectal Cancer Family Registry - Coordinating Center Laboratory Uni versity of Southern California, Department of Preventive Medicine Freeze at -70 degrees centigrade DNA and DNA RNA Drafted November 6, 1997 Revised October 2, 2002 6 CFR Biospecimen Availability (Draft modified from CFRBCS and CFRCCS) Biospecimen products available to researchers from CFR participants Product Original Amount Aliquots Storage Condition Available to Comments researchers? Plasma 10-12mL 18-24 -70C Yes Nonrenewable product Room temperature No Nonrenewable; @ 0.5mL each Blood Spots DNA 44 spots of 20ul 2 cards of 22 spots each each 0.4-0.5mg from Upon request For QC and back up -20C Yes EDTA Preferred product for distribution; Inexpensive more from EBV Ficoll-separated WBCs from 10mL blood ~4 aliquots Liquid N2 No @ 2x106 cells each EBV-transformed WBC Theoretically NA Source of EBV lines and non-EBV RNA; Nonrenewable product Liquid N2 Yes unlimited Provides DNA and RNA; Only renewable product in CFR. H&E stained paraffin- 2 slides per block (possible 2 slides @ 5 embedded tissue multi-blocks per case) um thickness Paraffin-embedded 10 sections per block 10 slides @ 5 um tissue on ProbeOn (possible multi-blocks thickness Plus slides per case) Paraffin-embedded 16-26 sections per 16-26 slides @ tissue on regular slides block (possible multi- 5 um thickness Room temperature No Nonrenewable; Upon request Room temperature Yes Nonrenewable; For immunohistochemical analyses Room temperature Yes Nonrenewable; Provides DNA. blocks per case) Paraffin-embedded 4 sections per block 4 sections @ 5 um Room tissue in 1.5 ml (possible multi- thickness in 4 1.5- ml tubes temperature microcentrifuge tubes blocks per case) unmounted on any slides Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Yes Nonrenewable; Provides DNA. Drafted October 10, 1998 Revised December 30, 2002 7 A. Processing the peripheral blood 8 PROCESSING THE BLOOD SAMPLES Receive three tubes of EDTA blood (3 X 10 ml purple tops) and one ACD tubes (1 X 8.5 ml yellow tops) 3 X 10 ml EDTA tubes 24-30 ml only 23-29 ml from EDTA tubes 1 ml from EDTA tubes 1 X 8.5 ml ACD tubes Removes granulocytes and 2/3 of DNA Consider reclamation of granulocytes for DNA/RNA Ficoll separate WBC 22 Blood spots of 20 ul ~12 ml plasma Aliquot in 0.5 ml tubes Freeze at -700C Buffy coat Aliquot in 1.5 ml tubes Cryo 4 x 2x106 cell aliquots in liquid N2 Extract DNA now or freeze buffy coat at -700C EBV lines can be used as inexhaustible sources of both RNA and DNA For future EBV transforming 5 micrograms DNA/ 1 million WBCs 1 ml whole blood = 5 million WBCs 9 ml whole blood = 225 micrograms of DNA = 225,000 nanograms Usual PCR reaction takes 25 nanograms > 9000 reactions / 9 ml of blood T75 flask contains only 3-5 million cells CFRBCS uses [50 ug/ml] DNA ( Feb 25, 1997 minutes) 9cc of blood resulting in 6cc of plasma ( June 11, 1998 minutes) Anh’s revision 10-02-02 Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Nov 23, 1998 AD 9 About blood collection Blood will be drawn from Sunday to Thursday and shipped from Monday to Thursday. Please allow 72 hours notice for shipments that occur under special circumstances, such as shipments that will arrive on a weekend or a holiday. Any blood not received by the lab within 24 hours of it being drawn will be rendered unusable for ficoll separation. In this case, the blood will be used for plasma and buffy coat. All blood should be shipped at room temperature using the “Two-Layer Insulation Method”. If the temperature of the blood exceeds room temperature during shipping, ice packs should be used. The blood should never be in direct contact with these ice packs. If drawing an amount below the minimal request, a second draw should be set up, if feasible. Once received, the blood should be kept at room temperature until processed. All samples sent to the lab will use study ID numbers only. Priority of collecting blood samples The goal of the phlebotomy visit is to collect 4 tubes of blood in the following order: -1 ACD tube (~8.5cc blood each): Shipped to Coriell by USC after ficoll separation for future establishment of cell lines. -3 EDTA tubes (~7.5cc to 10cc blood each) Shipped to USC lab to be used for DNA extraction. When conducting the blood draw, always begin with filling the EDTA tubes. Only after all 3 EDTA tubes are filled should the ACD tube be filled. In all cases, filling of the EDTA tubes take precedence. Filling the blood collection tubes Tubes should be filled to the indicated, colored line on the manufacturer’s label, which is about ¼” below the stopper. Time between blood draw and arrival at lab The goal is to have blood samples arrive at the lab within 24 hours of the blood draw. Any blood not received by the lab within 24 hours of being drawn will be used for DNA isolation only, not for plasma. If the time between the blood draw and shipping is delayed, so that more than 24 hours elapse between draw and processing at the lab, a second draw should be requested if feasible. No samples are ever to be discarded even in a blood drawing error! Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Dec 30, 2002 AD 10 Guideline for receiving blood Between Coordinating Centers and Processing Lab in USC As soon as a blood draw is scheduled, please inform immediately all lab staffs who work for this study (give at least 72 hours advance notice). They will primarily oversee and process the biological specimen for the registry. Once the blood is sent out, inform the lab the date and the number of subjects of the shipment. If the lab is to expect the shipment on a weekend or a holiday, please also include the tracking number of the shipment and sent directly to the lab. If no confirmation is returned from the lab about the receiving schedule, please find to inform them in person. After the shipment arrives, bring it to the lab at room 5427 where a section of Thanh’s bench is designated to receive samples for the registry. Unpack and leave the blood tubes standing upright in the assigned rack. Information such as the subject’s study ID, date and time (Pacific time) drawn must be provided. Finally, the lab should be informed promptly if there is any cancellation. Anh Diep Ehab El-Khouly Thanh Diep Evgenia Ter-Karapetova e-mail address atdiep@hsc.usc.edu elkhouly@hsc.usc.edu thanhtdi@hsc.usc.edu terkarap@hsc.usc.edu work number (323) 865-0713 (323) 865-0582 (323) 865-0583 (323) 865-0714 emergency contact (818) 361-7503 (818) 265-9431 (818) 365-8095 (626) 296-2766 Lab address (when a shipment is to be sent on a weekend or a holiday) Anh T. Diep c/o Haile’s Lab USC SCH of MED-Norris Cancer Center Topping Tower 5427, 5429 1441 Eastlake Ave. Los Angeles, CA 90033 Lab Telephone Line #1: (323) 865-0585 Lab Telephone Line #2: (323) 865-0586 Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised July 8, 1999 AD 11 Blood Delivery Notification Procedure 1. As soon as a blood draw is scheduled, please inform the following people: Email address atdiep@hsc.usc.edu Anh Diep Evgenia Ter-Karapetova terkarap@hsc.usc.edu thanhtdi@hsc.usc.edu Thanh Diep 2. Work number (323) 865-0713 (323) 865-0714 (323) 865-0583 Emergency contact (818) 361-7503 (626) 296-2766 (661) 799-9726 Ship the blood directly to our processing lab in USC. The attention line and the address are: Anh Diep c/o Haile’s Lab USC Norris Cancer Center 1441 Eastlake Ave, NOR 5427 Los Angeles, CA 90033 3. The labels for blood tubes should be preprinted with these information: Study ID Time Drawn Initial of phlebotomist Date Drawn Time Zone (EST, CST, PST, ...) Stick the labels on top of the writing area of the tube. 4. Once the blood draw is confirmed, email all the above three personnel using the following format: Name of Center......................... Study ID.................................... Drawn In...................................(name of state the blood was drawn in) Date Drawn............................... FedEx Tracking #...................... Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted July 11, 1999 TD Revised July 8, 1999 AD 12 Special instructions for shipments that will arrive on a weekend Please provide 72 hours notice for shipments that will arrive on a weekend. Please follow the special instructions for these types of deliveries: When filling out the FedEx forms for weekend delivery of bloods, you must: 1. Sign the air bill so shipments can be dropped off even without obtaining a signature from the lab. 2. Write a note for FedEx (next to our address on the forms) which says: "Please do not deliver before 10:30 am (PST)." It is imperative that this is done because FedEx only makes one delivery attempt for a Saturday delivery, and we can't afford to miss it. USC observes 14 holidays in 2001 - please do not schedule bloods to arrive at USC on these days: New Year’s Day Martin Luther King, Jr. Day President’s Day Memorial Day Observed Independence Day Labor Day Thanksgiving Day Day after Thanksgiving Day Christmas Eve Christmas Between Christmas and New Year’s Day New Year’s Eve (observed) Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Monday, January 1, 2001 Monday, January 15, 2001 Monday, February 19, 2001 Monday, May 28, 2001 Wednesday, July 4, 2001 Monday, September 3, 2001 Thursday, November 22, 2001 Friday, November 23, 2001 Monday, December 24, 2001 Tuesday, December 25, 2001 December 26, 27 and 28, 2001 Monday, December 31, 2001 Drafted July 11, 1999 TD Revised July 8, 1999 AD 13 Labeling blood collection tubes Each blood collection tube must be labeled with the following information: Study ID Date of draw, Time of draw and time zone (see Time Zone Table) Phlebotomist’s initials Study identifier: CFR The label must be placed vertically along the length of the tube covering the writing area of the tube so that lab will be able to view the level of the blood in the tube. Avery Labels Style 5667 (0.5” x 1.75”, height x length) is suggested for use. All samples sent to the lab will be labeled with study ID numbers only. Do not include any personal identifiers such as name or address. If possible, blood tube labels should be preprinted at the data collection centers using the Excel blood collection tube label generator. Time Drawn_____________EDT These labels include the Study ID and corresponding bar code, date of draw, time of Phlebotomist: 1234 CFR draw and time zone (see Time Zone Table), phlebotomist’s ID, and the study identifier, CFR. *111111* 01/02/01 In cases where the phlebotomist or the date of draw is unknown or may change, leave the respective fields blank in the label generator and the label shown at left will be generated: The date of draw and phlebotomist ID can be handwritten in just prior to the blood draw. US Time Zone Table The following table contains time zones in Standard and Daylight Savings Time for each center’s registry catchment’s areas. If the blood draw is done by a physician or outside phlebotomy service in another time zone, then that time zone should be recorded on the tube label. US Center Arizona Cleveland Minnesota North Carolina Colorado Dartmouth USC Standard Time Through 3/31/01 10/28/01-4/6/02 10/27/02-4/5/03 PST EST CST EST MST PST PST Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Daylight Savings Time 4/1/01-10/27/01 4/7/02-10/26/02 4/6/03-10/25/04 PDT EDT CDT EDT MDT PDT PDT Drafted October 10, 1998 Revised Nov 22, 2001 AD 14 Packaging the blood collection tubes for shipment “Two-layer insulation packing method” Supplies required: 5-tube foam carrier Ziploc bags Insulated foam carton Cardboard box Absorbent wadding material Tape for sealing boxes Biohazard label Express shipping air bill 1. 2. 3. 4. 5. 6. Blood collection tubes are placed in the 5-tube foam carrier, which is then taped shut. The sealed 5-tube foam carrier is placed in a Ziploc bag with absorbent material. The 5-tube carrier is then placed in the large insulated box with additional absorbent material. The foam box is securely taped shut and placed in the cardboard outer box. Affix a bright orange biohazard label to the cardboard outer box. The cardboard box is then securely taped shut and the completed air bill is affixed. Blood shipment temperature All blood should be shipped at room temperature using the two-layer insulation packing method. This system plus sufficient taping is the best blood shipment method. Do not include ice packs when using this system. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Nov 22, 2001 AD 15 After the blood arrives At the USC Coordinating Center Laboratory During the initial founding of the registry, the USC laboratory staff will be archiving blood samples to facilitate future analysis. No analysis will be done at this point. However, by collecting a maximum amount of blood and through careful storage, we will create a potentially inexhaustible resource. Participants are asked to donate less than 40cc. Three EDTA tubes and one ACD tube will be processed differently, so that the EDTA tubes become a source of plasma and buffy coat, and the ACD tubes become a source of white blood cells. Processing the EDTA tubes From the 16cc to 20cc of blood in the EDTA tubes, 1cc in homogeneous phase will be drawn immediately to make 44 blood spots on filter paper, which will be stored at room temperature. This will serve both as a back-up source of DNA as well as a quality control source for DNA. Our data from previous studies have shown that a 3mm square (from 3ul of whole blood) of dried bloodstain provides enough DNA for 2 to 5 PCR reactions. Thus, 44 blood spots theoretically can yield sufficient DNA for about 1000 PCR reactions. The remaining 15cc to 19cc of whole blood from these two EDTA tubes are separated by centrifugation and aliquoted into 0.5ml tubes of plasma and 1.0ml tubes of buffy coat. Separation needs to be done within 48 hours after the blood was drawn. The plasma and the buffy coat will each be saved separately and frozen at -70C. The plasma will be used for later phenotypic studies, and the buffy coat will serve as a source of DNA once funding is available for DNA extraction. The amount of plasma collectible from 15-19ml blood is 10-12ml. The amount of buffy coat from 15cc to 19cc whole blood should provide enough DNA for 15,000 PCR reactions (20-25ng DNA template). Genotyping of any marker takes about 50ng DNA as a template, which is enough for 2 PCR reactions. Thus, the DNA allows us to genotype more than 7000 markers. Also, to characterize genes that are already cloned and identified as causes of colorectal cancer by screening the entire gene to assess presence/absence of a mutation, our current work suggests we will need a minimum of 25 ug DNA or 1-5 cc of blood for 8-12 kb in length. Thus, the DNA allows us to screen a number of genes. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Nov 23, 1998 AD 16 Processing the ACD tubes For the one ACD tube of about 10cc whole blood, we will separate the white blood cells through Ficoll gradient columns. These cells will be stored at -70C for future lymphoblastoid cell line establishment. Culturing these cells would provide us with an inexhaustible source of RNA and DNA. 10cc whole blood requested from the subjects after Ficoll separation will provide 4 ampules of white blood cells. We will cryopreserve in liquid nitrogen for EBV transformation. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Dec 30, 2002 AD 17 Summary Aliquots made from >20 ml EDTA blood into: 2 cards of 44 blood spots (22 per card, 20 ul each spot) for direct PCR 20 to 24 aliquots (0.5 ml each) of plasma 3 to 5 buffy coat aliquots (0.75 ml each) for DNA isolation at room temp in -70oC in -70oC Aliquots from 10 ml ACD blood into: 4 aliquots (1 ml) of white blood cells in LN 1-15 ml tube of residual cells from both EDTA and ACD tubes for more DNA collection in -70oC If less than 20 ml EDTA blood is received: Always reserve 2 cards of blood spots regardless of the volume of blood received. Make less blood pellets for DNA isolation. Make less aliquots of plasma for phenotyping. If less than 10 ml of EDTA blood is received, a second draw should be setup if feasible. If less than 5 ml ACD blood is received: Make less aliquots of white blood cells. If less than 5 ml of ACD blood is received, a second draw should be setup if feasible. If only ACD blood is received and second draw is not feasible: Since ACD tubes will be drawn first. Always reserve 2 cards of blood spots. Regardless of the volume of blood or the type of blood tube received. Make blood pellets for DNA isolation from this only one ACD tube (<8.5mL blood). Make as many aliquots of plasma as possible from that one ACD tube (<5.0mL plasma). Make note for this “no ficoll seperated WBCs” specimen. If blood cannot be processed within 48 hours of it being drawn, and second draw is not feasible: Reserve 2 cards of blood spots as always from EDTA tubes. Make blood pellets for DNA isolation from EDTA tubes. Make as many aliquots of plasma as possible from EDTA tubes. There will be no aliquot of white blood cells for EBV cell line. Make note for this “ no ficoll seperated WBCs” specimen. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Dec 30, 2002 AD 18 1. Blood Spot Preparation (Modification of Brockmoeller et al. and Lin 1992 ) Dot on filter paper 44 spots from 1 ml whole blood. Reserve for quality control and a DNA back up source. Reagents and Equipment: 75% alcohol aerosol resistant tips balance banker box Betadine biohazard waste containers: bench top and step can bleach blue under pad dotting grid envelopes gloves kimwipes P20 pipetmen rack for 15 ml tubes S&S 903 filter papers* stop removers Blood protective pads TainerTop Safety Closure wax paper Stepwise Procedure: a. Mix blood thoroughly by gentle inversion to have a homogeneous phase before starting. Blood drawn in purple top vacutainer (EDTA as the anticoagulant). b. Wipe top of vacutainers with ethanol before opening the cap. Open the blood tubes with stop removers. c. Pipet 20 ul of blood and dot onto the paper. Recap blood drawing tubes with TainerTop Safety Closure during processing to prevent cross-contamination. d. Make two full blood cards of 22 spots each. e. Airdry thoroughly. f. Store in paper envelopes at room temperature. *Sharing from N. Lindor: Guthrie Spots: One "pearl" that I was able to glean from Schliecher and Schuell is that of circumspect in regards to printing circles for blood spots. S&S uses only inert inks, and printing presses that are used expressly for that purpose. In contrast, having S&S paper printed at a local printer, while saving money, may compromise the DNA extraction process. Only biologically inert inks, such as soy-based, should be used, and even then the ink may be contaminated by ink used in the previous printing job. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Nov. 26, 2001 AD 19 2. Plasma and Buffy Coat Separation (Gustafson et al.1987) Centrifuge at 1300-1500g for 15 to 30 minutes. Pipet out the supernatant plasma with a transfer pipette. The plasma is the yellowish hue top layer. Then with another transfer pipette, carefully transfer the buffy coat to fresh tubes. The buffy coat is a broad band of white blood cells with heterogeneous density. Store both this plasma and buffy coat for further application. Reagents and Equipment: 0.5 ml screw cap microcentrfuge tubes 2.0 ml screw cap microcentrfuge tubes 1 x Hanks’ Balanced Salt Solution balance Betadine biohazard waste containers: bench top and step can bleach blue under pad gloves glycerol freezing solution horizontal rotor 221 IEC HN-SII bench top centrifuge kimwipes racks for 15 ml centrfuge tubes and microcentrfuge tubes rubber adaptors transfer pipets storage box Stepwise Procedure: a. Mix the fresh whole blood by gentle inversion. Blood drawn in purple top vacutainer (EDTA as the anticoagulant). Recap blood drawing tubes during processing with TainerTop Safety Closure to prevent cross contamination. b. Centrifuge vacutainers at 1500xg for 30 min to separate plasma from others. Make sure tubes are balanced before centrifuging. Make sure tubes are recapped tightly. Use IEC HN-SII bench model centrifuge, horizontal rotor 221; Can hold 6x15 ml centrifuge tubes. Set speed at 3/4, about 2000-3000 rpm for 1500xg. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Nov 12, 1998 AD 20 c. Remove plasma with transfer pipets to 0.5 ml screw cap microtubes. The sample should have three distinct layers: i, Plasma (yellowish hue)--Top layer. ii, Buffy coat (white)-- thin interface. iii, Red blood cells---bottom layer. d. Fill tubes to 0.5 ml only and make as many aliquots as possible. e. Carefully pipet out the dense interface of buffy coat with a transfer pipet into 2.0 ml screw cap microtubes. f. Fill tubes to 0.75 ml only and also make as many aliquots as possible. It is acceptable to have some red cells mix with buffy coat. Efforts to avoid red cells can lead to considerable loss of white cells and diminished DNA/RNA yield. g. Overlay the white cells with the glycerol freezing solution (GFS) to 1:1 blood to GFS (with a maximum of 1.5 ml final volume). Gently mix by inversion. Glycerol freezing solution( pH 7.4 ) Reagent MW (g) Amount per 0.5 L Final concentration (mmol/ L) Citric acid, sodium salt 294 7.35g 50 Sodium phosphate, monobasic, 138 1.38g 20 monohydrate NaH2PO4-H2O Sodium phosphate, dibasic, anhydrous 142 1.32g 20 NaH2PO4 99% glycerol 200mL Filter sterilization using 0.2 u cellulose acetate or hydrophillic polyethersulfone low binding protein membrane h. Place the buffy coat tubes into a rate-control freezing container and freeze in -70C freezer. i. Transfer residual cells from remaining blood to a 15 ml centrifuge tube. j. Raise the volume of the 15 ml tube to 7.5 ml with GFS for more DNA collection. k. Store all tubes in -70oC immediately. 20-24 0.5 ml micro tubes of plasma, 3-4 2.0 ml micro tubes of buffy coat and one 15ml centrifuge tube of residual cells. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb. 14, 2000 AD 21 3. Ficoll Separation (modified from NYCOMED PHARMA AS Diagnostics Lymphoprep protocol) Reagents and Equipment: Alcohol, 70%--in a spray bottle DMSO (Dimethyl Sulfoxide) FBS (Fetal Bovine Serum) HBSS (Hanks' Balanced Salt Solution), 1X Lymphoprep (from Life Technologies) RPMI Medium 1640, 1X Trypan Blue Stain, 0.4% Adapters, for rotor, each accommodates 8 of 15 mL tubes Adapters, for rotor, each accommodates 3 of 50 mL tubes Beaker containing bleach for blood waste BloodBloc Pads Burner Centrifuge tubes, 15 mL Centrifuge tubes, 50 mL Cryogenic vials, 1.2 mL Hemacytometer Hood Sterilized with 75% alcohol and UV shined for half an hour before and after every procedure Microscope Microtubes, 0.5 mL Pipet-Aid Pipetman and aerosol barrier tips, 20 ul Pipetman and tips, 200ul Serological pipets, 1 mL Serological pipets, 2 mL Serological pipets, 5 mL Serological pipets, 10 mL Serological pipets, 25 mL Sterilized transfer pipets Centrifuge--Sorvall RC 26 Plus Rotor, swing-out bucket—SH-3000, hold 4 buckets Stepwise Procedure a. Record down total blood volume (subtract 1.5 mL of ACD solution from each vaccutainer). Dilute the blood with HBSS (1:1) and mix well. Blood drawn in yellow top vacutainer (ACD as the anticoagulant) b. Carefully overlay the diluted blood over Lymphoprep (the volume of Lymphoprep is half the volume of the diluted blood). Avoid mixing. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised on July 14, 1999 by TD 22 c. Centrifuge at 2000 rpm, 18-22C for 30 min with BRAKE OFF. d. Discard most of the top layer (plasma) without disturbing the next layer that contains lymphocyte. e. Remove the lymphocyte layer to a new centrifuge tube. Avoid picking up ficoll. f. Wash the harvested lymphocyte with HBSS. Mix well. g. Centrifuge at 1000 rpm for 10 min. h. Discard the supernatant. i. Resuspend the pellets with 13 mL of RPMI. Mix well. Save 10L of this solution in a microtube for cell counting purpose. Centrifuge the rest at 1000 rpm for 10 min. j. Discard the supernatant. k. Suspend the cells from every 2 mL of blood in 1 mL of freezing media. (63.5%RPMI + 30%FBS + 6.5%DMSO). DO NOT add DMSO until ready to freeze the cells. l. Divide the suspended cells to the pre-labeled cryogenic vials (0.5 mL per tube). m. Place the cryogenic vials into a rate-control freezing container and freeze in -80C freezer. n. Remove them to the cryogenic container on a weekly basis. o. Rinse vacutainers (both ACD and EDTA) and tubes with 1x HBSS and combine all in a 15 mL centrifuge tube to save the residual cells for more DNA collection. p. Prepare counting solution: Add 190 L of Trypan Blue to the microtube with 10 L of the cell suspension solution (20 x dilution). Mix well. q. Count the cells. Keep separate counts of healthy and dead cells. r. Calculations: Total number of cells yielded = X= Total counts / 2 / 4 * 20 * 10000 * 13 Lymphocyte Counts per ml of blood = X / Total Blood Volume Viability = Counts of Healthy Cells / (Counts of Both Healthy + Dead Cells) * 100% Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised on July 14, 1999 by TD 23 B. Processing the frozen tissue 24 If frozen tissue from a participant is available, it has to be frozen in liquid nitrogen immediately after surgery and sent to the USC biospecimen-processing lab for further processing. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised _______________ 25 C. Processing of Paraffin-embedded tissue USC PHASE III Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 26 Information needed for selecting PETs: For TMA CCF Only Accessing the paraffin-embedded-tissue block/slides a. Tracking b. Accessing Protocol for paraffin-embedded-tissue section preparation (For CCF Only) Reagents and Equipment A. Order of the paraffin-embedded-tissue sections B. Preparation of the paraffin-embedded-tissue sections The Alternative Protocol for Centers that cannot provide the complete protocol with 42 sections Reagents and Equipment A. Order of the paraffin-embedded-tissue sections B. Preparation of the paraffin-embedded-tissue sections Tissue Micro-array standard operating procedure(Phase II) a. Equipment & Accessories b. Reagents and supplies c. Preparation of the blank recipient array block d. Preparation of the donor blocks and slides e. Designing and constructing the Array (with cell carry-over free instruction). f. Align the punch g. Complete PET processing protocol and the order of the PET banking procedure h. After the construction of a full array block is completed and before sectioning i. Sectioning the blocks (donor and array) j. Tape-sectioning the array block 0.6 mm in diameter and spacing between two k. Hematoxylin And Eosin Staining Procedure Specimen, Reagents, Stepwise, Result, References, Troubleshooting l. Instruction to use the four block indexer m. Instruction to use the depth stop kit n. Maintenance of the Tissue Arrayer o. Worksheets p. Barcode labels q. Storage r. Data file s. Software for Spot Imaging Documentation (TO COME) t. TROUBLESHOOTING guide for manual tissue array construction u. FREQUENTLY ASKED QUESTIONS APPENDIX 1. Protocols for Pathology Reporting and Sample Collection APPENDIX 2. Material Specification of the barcoded labels for glass slide APPENDIX 3. Shipment Notification Procedure For Paraffin Embedded Tissue APPENDIX 4. TMAs Supplies/Reagents Ordering Checklist REFERENCE Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 27 For USC CCFR PHASE III Study, due to the newly revised protocol for the adaptation of TMA (tissue micro-array), the requested paraffin-embedded tissue (PET) will come only as a block, (CCF will be the only exceptional site that blocks will not be available for USC lab to process, they will continue to send the PET material in sections of the block). Information needed for selecting PETs: For TMA: If a PET block is available for the registry to retain, we will perform the TMA and keep the block in our repository. The pathology lab from the site will select the tissue block as follows: a. The preferred minimum dimension of the tissue is 4 mm x 4 mm x 4 mm. b. Consist of approximately 70-80 % tumor cells. c. Although normal DNA can be obtained from blood samples, blocks or sections should be selected to have some normal cells. If available, a block of normal tissue should be retained for each patient, particularly if deceased and/or if blood is not available. For sites that a PET block is not available for the registry to retain and the pathology lab is unable to perform the TMA, we request that a block be sent to us to process. Selection criteria of blocks for sectioning are the same as the above. The block will be returned within one month from the date that we received it. Note: Fixative type has a direct bearing on the quality of extracted DNA. i, Ethanol fixation: Although not routinely used in most pathology laboratories, it is an especially good preservative of DNA. ii, Mercury chloride: It contains fixatives such as B5 that have a deleterious effect on DNA integrity. However, it is sometimes adequate for PCR. iii, Bouin’ s solution: This also has a deleterious effect on DNA integrity. Just like B5, it is sometimes adequate for PCR. Duration of fixation is also important. Fortunately, PETs are routinely processed and fixed for less than 24 hours. However, the inhibitory effects of certain fixatives can be overcome by further phenol-chloroform extraction from DNA extracts. CCF Only. A PET block is not available for the registry to retain, we request: a. 10 sections with a thickness of 5 microns for immunostaining. b. 16 sections with a thickness of 5 microns for the microdissecting of DNA. c. 4 sections with a thickness of 5 microns for the extraction of composite DNA. d. 2 sections with a thickness of 5 microns for H&E (hematoxylin and eosin) staining. Please refer to the following protocol for section preparation The tests that will be performed on the PETs are destructive. Therefore, the slides or sections will not be returned. All remaining unused sections should be returned. e. Selection criteria of blocks for sectioning are the same as the above. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 28 Accessing the paraffin-embedded-tissue block/slides a. Tracking 1. The lab MUST be notified prior to the shipment. 2. Include the following information in your e-mail. Send to all personnel below: Ofeliya Avetisyan: Qingru Feng: Anh Diep: E-mail: oavetisy@usc.edu; Tel #: (323) 865-0583 E-mail: qfeng@usc.edu; Tel #: (323) 865-0581 E-mail: atdiep@usc.edu; Tel #: (323) 865-0713 Attach a copy of the standard lab TUMOR SHIPPING LOG sheet. Provide the FedEx tracking #. 3. Package should be sent to the lab using the following shipping address: Anh Diep c/o Haile’s Lab USC Keck School of MED – Norris Cancer Center Topping Tower 5421, 5427 and 5429 1441 Eastlake Ave. Los Angeles, CA 90033 Lab Line #: (323) 865-0585 Fax #: (323) 865-0140 4. The lab will acknowledge the arrival of the package immediately upon receiving (with a “cc” to Pat Harmon). Then follow with a report of the tumor accessing status within the next few days. 5. After processing (one month turn around time), the lab will be responsible to return the tissue to the coordinators. 6. As soon as the coordinators receive the package, the lab requests a confirmation sheet (the form will be enclosed in the package) signed and faxed back to the lab for the return of the material. b. Accessing 1. Have a complete pathology report with all pages. 2. Thoroughly deface all subject personal information: name, social security number, and date of birth. 3. Pathology report should be readable. 4. Highlight the pathology # and the study ID #. 5. Log in the “LOG BOOK” the number of the items received. 6. Take note for any discrepancy. 7. Report to the center immediately the discrepancy, then follow up on all correction actions. 8. Fill out ALL information (don’t leave blank) in a block processing log sheet (including information of tissue source). 9. In case of a tissue that is not ON LOAN and we can keep the block, create a separate logsheet for the block with a different Specimen ID. 10. Make a copy of the shipment log and staple them together with the block processing log sheet for every single block. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 29 Protocol for paraffin-embedded-tissue section preparation: (For CCF Only) Reagents and Equipment: Alcohol, 75%--in a spray bottle 1.5 ml microcentrifuge tube Permanent marker Regular slide ProbeOn Plus slide Xylene Microtome Microtome blade Floating bath Gloves Kimwipe Toothpick Tweezers Brush A. Order of the paraffin-embedded-tissue sections Section # Thickness in microns 5 Uses Prepared as H & E stained regular slide 2-11 (10 sections) 5 future immunohistochemical analyses ProbeOn Plus slide 12-27 (16 sections) 5 DNA extraction regular slide 28-37 (10 sections) optional 5 DNA extraction regular slide 38-41 (4 sections) 5 extraction of composite DNA 42 5 H & E stained unmounted on any slides each section is placed in a 1.5 ml micro tube* regular slide 1 *use regular slides to mount the section, if it is unfeasible to work with microtubes. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 30 B. Preparation of the paraffin-embedded-tissue sections DNA-based experiments where PCR is widely used require cells free from attached molecules to be an effective substrate for the molecular analysis. The purity of cells from paraffin-embedded tissue is essentially equivalent to analyzing pure cell lines. This list of precautions must be followed to prevent carryover from one specimen to another. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Slides and microcentrifuge tubes should be labeled with markers that stay permanent when in contact with EtOH and xylene. Label slides and tubes with the block id and section numbers according to the order of sectioning. Use adhesive (ProbeOn) Plus slides or comparable slides for immunostaining. Use regular slides for both H&E staining and microdissecting of DNA. Air-dry all slides. DO NOT bake slides. Use 1.5 ml microtubes for future constitutional DNA extraction. Use regular slides to mount the section, if it is unfeasible for the pathology lab to work with micro-centrifuge tubes. Only touch the edge of slides. Completely place the PET sections within 1.5 ml microtube without overhang. Do not touch the rims or insides of caps when opening and closing tubes. The microtome and work area are cleaned twice with ethanol or xylene between specimens to remove excess paraffin, tissue fragments and debris. The microtome blade is changed after sectioning each case. Each block is refaced before sectioning. Floating bath must be changed for each case. The temperature for the bath: 48C to 52C. Soaking the blocks on ice or a ice tray is required. A new pair of disposable gloves will be used for handling and sectioning each case. Brushes for picking up the sections must be cleaned with ethanol and UV radiated between each case. Toothpicks may be used in place of brushes. Drafted October 10, 1998; Revised Feb 11, 2004 AD Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 31 The Alternative Protocol for Centers that cannot provide the complete protocol with 42 sections: Reagents and Equipment: Alcohol, 75%--in a spray bottle 1.5 ml microcentrifuge tube Permanent marker Regular slide ProbeOn Plus slide Xylene Microtome Microtome blade Floating bath Gloves Kimwipe Toothpick Tweezers Brush A. Order of the paraffin-embedded-tissue sections Section # Thickness in microns 5 Uses Type of Slides Used H & E stained regular slide 2-17 (16 sections) 5 DNA extraction regular slide 18-27 (10 sections) 5 future immunohistochemical analyses charged (ProbeOn Plus is preferred) slide 28 5 H & E stained regular slide 1 Drafted October 10, 1998; Revised May 11, 2001 AD Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 32 B. Preparation of the paraffin-embedded-tissue sections DNA-based experiments where PCR is widely used require cells free from attached molecules to be an effective substrate for the molecular analysis. The purity of cells from paraffin-embedded tissue is essentially equivalent to analyzing pure cell lines. This list of precautions must be followed to prevent carryover from one specimen to another. 1. 2. Slides and microcentrifuge tubes should be labeled with markers that stay permanent when in contact with EtOH and xylene. Label slides and tubes with the block id and section numbers according to the order of sectioning. 3. Air-dry all slides. DO NOT bake slides. 4. 5. Only touch the edge of slides. The microtome and work area are cleaned twice with ethanol or xylene between specimens to remove excess paraffin, tissue fragments and debris. 6. The microtome blade is changed after sectioning each case. 7. Each block is refaced before sectioning. 8. Floating bath must be changed for each case. 9. The temperature for the bath: 48C to 52C. 10. Soaking the blocks on ice or a ice tray is required. 11. A new pair of disposable gloves will be used for handling and sectioning each case. 12. Brushes for picking up the sections must be cleaned with ethanol and UV radiated between each case. Toothpicks may be used in place of brushes. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 33 Tissue Micro-array standard operating procedure(USC Phase III) a. Equipment & Accessories 1. Manual Tissue Arrayer MTA-2 from Beecher Instruments, Inc. Sun Prairie, WI, (To order: Tel # (608) 837-8847 or Fax # (608) 837-7118) www.beecherinstruments.com; support@beecherinstruments.com Model MTA-2 includes: 2 sets of 0.6mm punches 1 recipient block holder, 11 additional will be ordered 1 donor block bridge operating manual and tools two sets of punches: 0.6 and 1.0 mm; 1.5 and 2.0 mm. Optional: Depth Stop Kit (DSK) 2. A magnifying glass model Wave + A/R from LUXO, Port Chester, NY. (Purchase can be processed through VWR); www.luxo.com 3. Tape sectioning system (Cat # PSA) from Instrumedics, Inc. Hackensack, NJ (To order: Tel # (201) 343-1313); www.instrumedics.com System includes: UV Curing Lamp, Cat # PSA-LMP PSA Curing Lamp bulb, Cat # PSA-BLB Hand roller, Cat # HR Voltage Transformer, Cat # PSA-TR TPC Solvent can, Cat # PSA-CAN CureMount II, Cat # CMII (60 ml/bottle) b. Reagents and supplies Donor blocks Glass slides Blank (recipient, array) block Regular paraffin Mold (for preparation of blank block), 5-10mm thick. Cassette (as above) Plastic block holder Knife Alcohol, 70% (in a small bottle) Kimwipes, small Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 34 THIS IS THE EQUIPMENT WE HAVE MANUAL ARRAYER (MTA-II) Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 35 c. Preparation of the blank recipient array block 1. Melt regular paraffin at temperature 55-580C, pour the melted paraffin into a mold. 3. Place a cassette on top of the melted paraffin until the complex is cooled. The mold is ready to be removed. 4. Cut all irregularities from the plastic block holders and check for any holes (air bubbles) in the block. d. Preparation of the donor blocks and slides 1. Prepare a fresh H&E– stained slide from each block. 2. Circle or mark the sampling sites on the corresponding H&E slide. e. Designing and constructing the Array (with cell carry-over free instruction). 1. Each recipient block will contain 384 samples divided into four quadrants. 2. 1.0 mm spacing between the centers of two adjacent samples is maintained. This will make adding increments to the micrometer a lot easier. 3. Leave 2.5mm margins on the top and the bottom of the array block. 4. Leave 3.0mm on the left and the right edge of the array block. (See worksheet “Diagram of TMA organization: Design of the array with positions of the punches) 5. Insert the empty recipient block in the holder and tighten the clamping screws to prevent the block from slipping. 6. Place the holder firmly against the location curbs. 7. Make the hole in the first position in recipient block (at this point, the micrometer should be set to zero). *The smaller punch is used to create the hole. 8.Align the H&E slide and the corresponding tissue block. Retrieving the sample from the donor and empty the tissue core into the hole created by the smaller punch. *The larger punch is used to take sample tissue. 9. Prepare the array (recipient) blocks according to the preplan TMAs organization. 10. Between cases, to ensure cell carry-over free for subsequent DNA_PCR-based block to clean up the larger punch. analysis, punch at least 10 times into blank 11. Make sure the punched-blank-paraffin core including its residual cleanly empty from each punch. To obtain the best cleaning result, creating a small horizontal motion of the punch by slightly moving the turret to help break the punch free from the inserted tissue core. f. Align the punch 1. Check the positioning and alignment of punches before beginning to construct the first array. 2. To verify alignment, place a blank paraffin block in the block holder and put this complex in position on the arrayer as if it were a recipient block. 3. Press the smaller punch down until it leaves a mark in the paraffin surface. 4. Move the turret to switch the larger sampling punch in position, and again make a mark on the paraffin surface. 5. Adjustment is needed if the marks are not coincidental. 6. Front to back alignment is adjusted by setscrews recessed in the inboard side of the plastic v-blocks holding the punches. 7. To correct left-right alignment, use the largest hex key to turn the left-right setscrews on each lower side of the turret. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 36 g. Complete PET processing protocol and the order of the PET banking procedure PET Banking task order 1st # of arrays or Section # 1 section donor block Thickness in microns/diameter in mm 5 um Uses Prepared as/ for H & E stained regular slide blocks and areas selection 2nd 121.5 ml micro tubes 0.6 mm cores 8T + 4 N cores per donor block Direct extraction of composite DNA 0.6 mm - 3 cores per donor block 1 adenomas, 1 tumor and 1 normal 25% duplicates from 48 tissue of larger tumors oriented with a set of 3 normal cores in quadrant A of the block: central area of selected region NOT inserted in TMAs each core is placed in a 1.5 ml micro tube 1 A/C/N TMA (Adenomas, Carcinomas and normal array) A set of 3 A/C/N TMAs will be made if adenomas tissue is available, always include 25% of duplicates 3rd 1 array block Array ID labeled ACN01 A1a, A1b, A1c 4th 4 array blocks 0.6 mm-4 cores per donor block Array ID subdivision labeled A to H 1 tumor and 1 normal, 190 pairs 25% duplicates from 24 tissue of larger tumors oriented with 4 blank spots in 4 quadrants, localization: A1a, B1a, C1a and D1a 5th 8 array blocks Array ID subdivision labeled I to P 0.6 mm-4 to 8 cores per donor block 1 tumor core per array block 96 duplicate pairs adjacent to each other (randomly localized) as a QC 25% duplicates from 48 tissue of larger tumors oriented with 3 normal cores in 3 quadrants, localization: 4 T/N TMAs (Tumor and Normal arrays) totally 166 subjects with 24 subjects in duplicate A set of 2 T/N TMAs, make 4 sets 4 to 8 T-only TMAs (Tumor only arrays) totally 332 subjects per block with 48 subjects in duplicate A1a, B1a, C1a 1 breast tissue core in D1a 6th 7th 8th *9th 1 section donor block 5 sections donor block 10 sections donor block 5 um H & E stained 5 um DNA analyses 5 um IHC analyses 1 section per array recipient block 5 um H & E stained Taping-sectioning method regular slide punched spots verification regular slides for QC ProbeOn Plus slides for QC Finished full TMAs (332) 4 T/N TMAs, 8 T-only TMAs and 1 A/C/N TMA 13 Adhesive coated slides for spots confirmation and localization *cell carry-over free procedure conducted between cases. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 37 h. After the construction of a full array block is completed and before sectioning, the array block surface must be smooth and leveled. 1. Place the finish recipient array block in a warm chamber (37C) for 10-15 min to promote adherence of the tissue to the walls of the holes in the array block and make wax flexible to handle. 2. level the surface of the block after it has warmed by a clean glass slide. Apply even pressure to push all tissue cores on the array to the same level. 3. The array block is now ready for sectioning. i. Sectioning the blocks (donor and array). 1. 2. 3. 4. Use standard microtome sectioning techniques to cut the sections of the donor block. Use a adhesive-coated tape sectioning aid system to collect the H&E stained section from each recipient block. Use current routing technique to collect sequential sections from the punched donor block: the first after-punched section is for H&E staining, the rest of the sections will be mounted on uncharged slides. Use the tape-sectioning aid to cut the H&E section for the array recipient blocks. j. Tape-sectioning the array block 0.6 mm in diameter and spacing between two adjacent array Paraffin tape-transfer slides Tape windows TPC solvent CureMount II Ultra-violet curing lamp PSA curing lamp bulb Hand roller Voltage transformer TPC solvent can 1. Trim the paraffin block to expose the tissue face. 2. Remove the section of mylar that says “ PEEL THIS OFF” from the pink tape to expose the adhesive layer. Adhere the tape window to the block face, using the handle roller with firm pressure. Be sure not to trap bubbles. If bubbles are trapped remove the tape and try again. 3. Using a sharp blade cut the section, which is supported and captured by the tape. 4. Laminate the tape with the section-side-down onto the adhesive-coated slide using the hand roller. Be sure that you have removed the mylar film from the slide. The lamination step is very important. Be sure the section is flat against the adhesive layer and that bubbles are not trapped under the section. Check for bubbles by examining the underside of the slide. 5. Place the slide, section-side-down, on the Curing lamp tray. 15 slides fit comfortably on the tray. 6. Turn on the UV light and the tray under the lamp. Polymerization of the adhesive coating into a plastic layer usually takes 30-60 seconds. If the coating is not polymerized, leave slied under the UV light for a longer time. 7. Immerse the slide, with the tape window still in place, in the TPC solvent in the solvent can. IMMEDIATELY REVOVE THE TAPE, by slowly and carefully peeling it away from the slide. Solvent should be between the slide and the tape as you peel the tape away. 8. The slide is ready to be deparaffinized. Some paraffin need a longer time than others in xylene to completely deparaffinize. Once hydrated the section is ready for your protocol. For H&E staining see the enclosed instructions. (When ready to cover slip dehydrated and cleared sections, use the CureMount mounting medium included with system. Instructions are enclosed.) k. Hematoxylin And Eosin Staining Procedure: Hematoxylin and eosin staining is performed on a regular basis on all received specimens as a first step in the diagnostic procedure. Specimen type: 1. Frozen tissue may or may not be embedded in O.C.T. 2. Paraffin blocks or precut slides obtained from referring laboratories. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 38 Reagents: 3. 4. 5. 6. 7. 8. Acetone. ( See Standard Operating Procedure for Hazardous Chemicals, LAB SAFETY SECTION ). Store at room temperature. Harris Hematoxylin Solution Modified ( Sigma Diagnostics Cat. #HHS-32). Store at room temperature until expiration date. 1% Acid Alcohol ( 100 parts 70% ethanol + 1 part 37% hydrochloric acid ). Store at room temperature for 12 months. Scott’s Tap Water Substitute Concentrate “10x” ( 1 part Scott’s Tap Water + 9 parts distilled water). ( Sigma Diagnostics Cat. # S 5134). Store at room temperature until expiration date. Eosin Y Solution, Alcoholic ( Sigma Diagnostics Cat # HT 110-1-32). Store at room temperature until expiration date. 95%, 100% Ethanol. Store at room temperature. Stepwise Procedure: 9. Paraffin slides are dried in a 60- 65C over for at least an hour. Deparaffinize sections in FRESH xylene (35 min); rehydrate in graded ethanol (2 min each) and transfer to distilled water. (Frozen sections are fixed in picric acid para-formaldehyde or in 95% alcohol for 15 minutes, then transferred to distilled water.) Stain the slides in hematoxylin solution for 5 minutes. Rinse in running tap water, to remove excess hematoxylin, for 2 minutes. Differentiate in acid alcohol for 15 seconds. Rinse in running tap water for 2 minutes. Put the slides in Scott’s tap water substitute for 30 seconds – 1 minute. Rinse in running tap water for 2 minute. Counter stain the slides in eosin for 3 minutes. Rinse in 2 changes of 95% ethanol, 2 changes 100% ethanol ( 2 minutes ). Rinse in 3 changes of xylene ( 2 minutes each). Cover slip with permount. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. Result: Nuclei will stain “Blue” Cytoplasma will stain into various shades of “pink”, identifying different tissue components. References for the H&E staining procedure: 1. Luna LG(ed.). Routine Staining Procedures: Hematoxylin and Eosin Stains in Manual of Histologic Staining Methods of the Armed Forces Institute of Pathology. Third Edition. McGrawHill book Company. 1968; 32-41 2. Sheehan DC, Hrapchak BB. Theory and practice of Histotechnology. Second Edition. Battelle Press. Columbus, Richalnd. 1987; 144-5. Troubleshooting for the H&E staining procedure: If sections appear too blue at step 7, re-immerse them in acid alcohol for a few seconds, then repeat steps 5 to 7 and recheck. If sections appear too plate at step 7, re-immerse them in the hematoxylin for further staining, then repeat step 3 to 7. The alcohol used in step 9 serve a dual purpose: dehydration of the tissue, as well as removal of excess eosin. By passing too rapidly through these alcohols, excess eosin will remain in the section and overshadow many diagnostic features. Occasionally, the used reagents are know to be working satisfactorily, yet some sections fail to show nuclear staining. This can be due to: a) autolysis of the tissue section, b) prolonged storage of the wet tissue in non-buffered formalin, c) dried or burned tissue. Basophilic staining properties may be restored by treatment of the hydrated sections with one of the following solutions: (1). 5% aqueous sodium bicarbonate overnight followed by a 5- minutes wash in tap water before staining, or Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 39 (2). 5% aqueous periodic acid overnight, followed by 3 changes of distilled water before staining. l. Instruction to use the four block indexer (OPTIONAL for MTA-I only) The Four-Block Indexer (4BI), which holds four standard recipient blocks in its turntable simultaneously, make it easier for users to construct concurrent arrays. With the 4BI in place, each of the four different recipient blocks may be quickly indexed into position. Introduction 1. Insert the 4BI in position, it has three slots on the underside. Any one of these slots fits over the shorter silver bar that braces the standard recipient block holders (RBH) in place. 2. Circular finger rests for rotating indexer, thumb rest corner for swinging bridge plate to the left, access grooves for setscrews. 3. The cassettes of array blocks are held in the pockets of the turntable with a pair of setscrews for each block. m. Instruction to use the depth stop kit The Depth Stop Kit (DSK) provides the additional capabilities of: (a) controlling the depth of the donor punch in the donor blocks, and (b) holding the donor punch just above the surface of the recipient block during the transfer of the tissue core from the donor punch to the recipient block. Introduction 1. The DSK includes 5 aluminum (silver color) donor transfer stops and 5 brass (yellow color) donor block stops. Each is numbered with the depth in millimeters, 2,3,4,5, or 6. If wishing to extract 3 mm long cores and place them in 3 mm deep holes in the recipient block, and then choose the #3 donor transfer stop and the #3 donor block stop. 2. The donor transfer stop fits on top of the depth stop block, with the higher end toward the back. 3. The donor block stop fits directly onto the donor punch hub, with its number upright and toward the user. The circular part of the donor block stop placed underneath the punch hub so that the punch needle goes through the slot in circular part. 4. To operate the donor block stop, simply move the turret downward in the usual manner, until the bottom of the donor block stop contacts the top of the donor block. The needle will now be the selected depth into the donor block. n. Maintenance of the Tissue Arrayer 1. Use Kimwipe to clean any residual paraffin from the punches, sampling block and block holders. 2. Use alcohol (or xylene ) to wipe parts. DO NOT SOAK ANY PARTS, PUNCHES IN A SOLVENT. DO NOT USE SUCH A SOLVENT FOR CLEANING THE X-Y OR Z RAILS. 3. Punches need to be periodically replaced after several hundred or a thousand punches. o. ID assignment system 1. Specimen ID is given sequentially by the database. This ID will be labeled on the donor blocks and to the slides. The ID numbering system consists of a first 3 digits “121”, which is coded for “BLOCK”, while “120” is coded for “BLOOD”; with a hyphen to separate the subsequent 6 numerical digits, to uniquely identify each individual block. To the slides, there will be an additional sub # to identify the order of the section. Therefore, the Specimen ID will look like: 121-123456-01 2. Array Specimen ID is given by the TMA operator using a system of 4 numerical digits and 1 alphabetical digit. The first 4 numerical digits will be coded for an array set of replicated blocks derived from a set number of donor blocks (332 blocks totally). The 5 th alphabetical digit is used to identify the type of arrays, either they are consisted of tumor/normal tissues (T/N) or tumor tissue only (T-only) or adenomas/carcinomas/normal tissues (A/C/N). A to H have been used to assign for 8 of the replicate T/N array blocks and I to P have been used to assign for 8 of the replicate Tonly array blocks. Except for A/C/N array blocks, the ID system will be different. Each A/C/N array block will be labeled as ACN01 sequentially as it will be made for blocks that adenomas tissues are available. Therefore, the Array Specimen ID will look like: Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 40 1234A to 1234H for T/N array blocks 1234I to 1234P for T-only array blocks ACN1 for A/C/N array blocks p. Worksheets 3. PET block accessing log. Worksheet 1 4. Localization checkerboard of the T/N TMAs. Worksheet 2 5. Localization checkerboard of the T-only TMAs. Worksheet 3 4. Localization checkerboard of the A/C/N TMAs. Worksheet 4 Notes: If a hole in one array block was damaged, skip that hole which means one replicate block lesser for the set of array blocks. If the tumor is large enough to make an extra series, these duplicates will consider the QC for the assay. In any mean, always make the same localization in a set of array blocks for the same donor tumor. 5. Diagram of the TMA organization. General 6. Design of the array: position of punches 7. Diagram of the TMA organization. Example of localization assignment 8. Diagram of the TMA organization. T/N array 9. Diagram of the TMA organization. T-only array 10. Diagram of the TMA organization. A/C/N array 11. PET blocks and slides log sheet. Worksheet 5 Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 41 Worksheet 1. PET block accessing log. PET BLOCK ACCESSING LOG Date Received Center Block ID # # of Blocks Received Date/Tech Screened Date/Tech Processed Date/Tech Returned Comment Worksheet 2. Localization checkerboard of the T/N TMA (X for spotted, 4 duplicates/ quadrant) Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 42 Array Specimen ID 1 2 3 4 QUADRANT 1 (circle): 1 1 1 A 1 1 B 2 1 1 1 3 1 C 1 1 4 1 1 1 5 D 1 1 1 6 1 1 1 7 1 1 1 8 a b c d e f g h i j k l # OF DONOR BL _______________________________________________________________________________________________________________________________________________ # OF DUPLICATE______________________________________________________________________________________________________________________________________________ Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 43 1 Worksheet 3. Localization checkerboard of the T-only TMA (X for spotted, 8 duplicates/quadrant) Array Specimen ID: 1 5 QUADRANT (circle): 8 8 1 8 8 8 2 2 6 3 7 A 8 8 8 B 3 8 8 8 4 8 C 4 8 8 8 D 5 8 8 8 6 8 8 8 7 8 8 8 8 a b c d e f g h i j k l # OF DONOR BL _______________________________________________________________________________________________________________________________________________ # OF DUPLICATE______________________________________________________________________________________________________________________________________________ Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Jan 29, 2004 AD 44 8 Worksheet 4. Localization checkerboard of the A/C/N TMA (X for spotted) Array Specimen ID QUADRANT (circle): 1 1 1 1 1 1 2 A 1 B 1 1 3 1 C 1 1 4 1 D 1 1 5 1 1 1 6 1 1 1 7 1 1 1 8 a b c d e f g h i j k l # OF DONOR BL _______________________________________________________________________________________________________________________________________________ # OF DUPLICATE______________________________________________________________________________________________________________________________________________ Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD 1 Diagram of TMA organization. General a b c d e f g h i j k l B a b c d e f g h i j k l 8 8 7 7 6 6 5 5 4 4 3 3 2 2 1 A a b c d e f g h i j k l 1 8 8 7 7 6 6 5 5 4 4 3 3 2 2 1 1 a b c d e USC Genetic Epidemiology Laboratory Keck School of medicine, department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine D f g h i j k l Date drafted: April 21, 2004 Anh T. Diep Drafted October 10, 1998 Revised Feb 13, 2004 AD C 8.8 8.8 Design of the Array : Position of the punches (size in mm) 0.8 5.2 a b c d e f g h i j 5.2 5.2 l a k 8 5 5.2 b c d e f g h i j k l 8 Y=22 11 7 0.8 0.2 7 6 6 5 5 4 4 3 3 5.6 B 2 1 1 D 2 1 0.8 1 R = 0.3 1 11 1 X=35 8 A 5 a b c d e f g h 4 i j k l 7 7 6 6 5 5 4 4 3 3 2 2 1 1 0.8 4 8 0.8 a b c d e f h 4 i j k l 4 8.8 Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine g 8.8 Drafted October 10, 1998 Revised Feb 13, 2004 AD 11 C 5.6 11 Diagram of TMA organization. Example of Localization assignment. a b c d e f g h i j k l B a b c d e f g h i j k l 8 8 7 7 6 6 5 5 4 4 3 3 2 D 2 1 1 Localization A7g A a b c d e f g h i j k l 8 8 7 7 6 6 5 5 4 4 3 3 2 2 1 1 a b c d e USC Genetic Epidemiology Laboratory Keck School of medicine, department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine f g h i j k l Date drafted: April 21, 2004 Anh T. Diep Drafted October 10, 1998 Revised Feb 13, 2004 AD C j k l k l i i j h f f h e e g d d g c c 4 5 6 7 8 b l l b k k a j j 7 6 5 4 3 3 blank 4 5 6 7 8 blank blank 1 2 2 1 blank 8 7 6 5 4 3 3 USC Genetic Epidemiology Laboratory Keck School of medicine, department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD blank C blank blank A a 1 2 2 1 blank a i i f f h e e h d d g c c g b b 8 a B D Diagram of TMA Organization. Tumor-and-Normal TMA Location Date drafted: April 22, 2004 Anh T. Diep i j k l i j k l f f h e e h d d g c c g b b l l a k k 7 6 7 4 5 6 5 3 4 2 3 1 2 1 8 Breast Normal 8 2 3 4 5 6 7 7 6 5 4 3 2 USC Genetic Epidemiology Laboratory Keck School of medicine, department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine C Normal A 1 1 Normal a j j 8 8 i f f i e e h d d h c c g b b g a a B D Diagram of TMA Organization. Tumor-only TMA Location Drafted October 10, 1998 Revised Feb 13, 2004 AD Date drafted: April 22, 2004 Anh T. Diep j k l j k l i i f f h e e h d d g c c g b l l b k k 7 6 2 3 4 5 6 5 4 3 2 8 1 1 8 C A a 1 2 3 4 5 6 7 7 6 5 4 3 2 1 Normal a j j 8 i f f i e e h d d h c c g b b g a 7 8 a B D Diagram of TMA organization. Adenomas-Carcinomas-and-Normal TMA Location USC Genetic Epidemiology Laboratory Keck School of medicine, department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD Date drafted: April 22, 2004 Anh T. Diep PET slides log sheet. Worksheet 5 (Available only from the ACESS database) Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD q. Barcode labels (NOT ADAPT YET) 1. For the array recipient blocks: (Making 2 labels per array block/ Array Spec ID) L-1002-10 laser printable sidewall Tough-tags 0.25” x 1.5” (prefer to be smaller 0.25” x 1.0” and clear instead of white) will be used. This specially designed labels is super durable. They are carefully engineered to strongly adhere to all plastics and other materials. Labels will withstand organic solvents, caustic agents, humid incubators, boiling water baths, refrigerators and freezing temperatures without peeling. Our lab has routinely use them for PCR plates which have undergone cycles of different temperatures and then long term stored in –20°C or -80°C. This label is now applied on the wax cassette that hold PET tissue. The cassettes will be undergone icy cold water soaking before sectioning and then will long term stored at controlled ambient atmosphere or 4°C condition. Therefore, a simple test has be performed in our lab by soaking the tough-tag labeled paraffin cassette in cold water for many hours, then observe the adhesive by peeling and the writing (laser printing) for it legibility. The result has confided our choice for this purpose. 2. For the glass slides: (Randomly, uniquely for each slide, hand label the slide sequential #) A pre-printed barcode FLAP labels will be applied to the glass slides of this study. This FLAP Label was designed for use on microscope slides. The FLAP Label construction was developed for use in the laboratory and other high stress, chemically rigorous environments, such as cytology, histology and cytogenetics. Material Specification TS822 (Appendix 3) describes the list of chemicals and stains that these labels have been tested for. The feature of FLAP uniquely designed with an overlaminate flap that is placed over the image after printing for additional image protection against harsh chemical environments. The adhesive is formulated to permanently bond to most demanding surfaces and microscope slide will be one of them (label should be applied to the painted or frosted sections of glass slides to insure maximum bond. To assure the described performance, our lab tested the labels on 10 tested microscopic glasses using a simple design: After applying the labels on the slides, barcode scanned the specimen ID, then conducting our routine H&E staining procedure in which the following chemical and temperature have been included: In 60- 65C for at least an hour >> In FRESH xylene 15 min >> Rehydrate in graded ethanol ~10 min >> Transfer to distilled water >> Stain the slides in hematoxylin solution for 5 minutes >> Rinse in running tap water for 2 minutes >> Differentiate in acid alcohol for 15 seconds >> Rinse in running tap water for 2 minutes >> Put the slides in Scott’s tap water substitute for 30 seconds – 1 minute >> Rinse in running tap water again for 2 minute >> Counter stain the slides in eosin for 3 minutes >> Rinse in 2 changes of 95% ethanol for 2 minutes each >> Rinse in 2 changes 100% ethanol for 2 minutes each >> Rinse in 3 changes of xylene for 2 minutes each >> After above conditions, the slides were scanned again to examine the quality of printing. The adhesive was also carefully examined by physical peeling. The test confide our choice of labels for this study. Preprinted information is designed specifically to have 11 digits in total with the last digit a "MOD 10-human readable interpretation" check digit. There is also a capital letter that shows in front of barcode number. This series of a letter followed with 10 sequential digits plus a MOD-10 check digit are all human-readable on the label that is scanned. The printing symbology code is 128. The product cat. #: TS822. Provided by: DELTA-ONE Software, Inc. (2841-G Saturn St. Brea, CA 92821, Telephone # (714) 528-7226, Fax # (714) 528-7236, Sale Rep. For USC-CFR is Marilyn Fox) The graphic design of the label approved by our lab is (this is only a sample label temporarily used for the first 10,000 cryovials, the final approved label is described above): Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD 7/8” USC Genetic Epi 3/4” A1234567890 3. Other labels need for worksheet, donor blocks, etc will use AVERY common office type labels. r. Storage 1. store the array recipient blocks in a embedding ring filing cabinet brand name Sakura Finetek Tissue-Tek. This stackable cabinets accommodate 1000 rings/blocks. File the blocks chronologically. Store at room temperature in a climate controlled laboratory or 4C walk in cold box. (purchase information: VWR cat # 25608-866) 2. store the slides in a steel micro slide storage cabinet “Boekel”. It is also a stackable unit with interlocking tabs and removable drawers for transporting to work areas. The 6-drawer cabinet can hold up to a total of 5000 standard micro slides. The slides are filed and stored at room temperature in a climate controlled laboratory. (purchase information: VWR cat # 48466-500) s. Data File (TO COME) t. Software for Spot Imaging Documentation (TO COME) Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD u. TROUBLESHOOTING guide for manual tissue array construction 1. When depositing the samples to the recipient (tissue array) block, the tissue core does not seem to go exactly to the location of the hole created for it with the small punch. Make sure that you are not accidentally moving the turret while pushing down the sample. Punch alignment may have changed (for example, after replacing the punch). Realign the punch. 2. Spacing between adjacent array samples seems to vary, causing a distortion in the tissue array. Make sure the punch handles are always turned to a consistent position. The punch may be bent. Check it and change if necessary. 3. The punch does not extract a tissue or wax core sample. This situation can be corrected by gently pushing the stylet down against the sample before trying to extract it (tamping). Placing pressure on the top of the sample causes it to compress axially and expand radially, thus creating a tighter fit within the punch tube. Rotating the needle handle slightly also helps break the sample from its base. Longer core samples are also easier to extract than shorter core samples. This is particularly important with the larger punches (1.0, 1.5, and 2.0 mm diameter). 4. The tissue core does not come out of the punch easily. There seems to be resistance at the tip of the punch. The sharpened edge of the punch tip is probably distorted. Change the punch. 5. The tissue core was accidentally pushed too deep and will cause a hole in the tissue array. Can something be done to fix this? Yes. Just remove that sample with the small punch and place a new sample in the same position. 6. I have now arrayed 200 specimens, and it seems like the middle part of the tissue array is higher than the edges. It looks like a small hill. What causes this and can it be fixed? If the array block is made in very high density, there may be an accumulation of residual paraffin, partly caused by the slight size difference between the sample tissue cores and the holes in the array. This makes the middle part of the tissue array protrude upwards, and this phenomenon becomes visible after arraying a large number of samples. In essence, you may be trying to fit too many samples in too little a space. To prevent this, either increase the spacing between adjacent array samples or make the holes in the array block deeper. To flatten any existing outgrowths in the tissue array, warm the block to 35-37°C for 15 minutes. While the block is still warm and elastic, place a clean microscope slide on top of the array block, and carefully press downward until all the specimens are at an even level. Let the block cool before removing the slide. 7. One of the micrometers is difficult to move Make sure that both its locknuts are completely loose: the black knurled ring near the base of the handle and the silver knurled knob at the side of the slide. Tighten the turret pivot screw in 1/8-inch increments until the swinging turret motion is just blocked--do not overtighten. If the digital readout does not respond to the control buttons or knob, or if the readout is dim, the micrometer battery may be too old and needs to be replaced. Batteries are located on the underside of the micrometers, and are accessible through the circular holes in the base plate. Reposition the arrayer carefully to gain access to the battery covers. Insert a new battery with the positive (+) side away from the cover, tighten the cover, and check to verify that the micrometer numbers change as you twist the handle. You may need to reinsert the battery two or three times before the battery correctly activates the readout. We recommend Renata, Sanyo, or Duracell type 2450 batteries because some other makes may not fit. A small booklet specifically about the micrometers is included with the arrayer and will provide more information about the micrometers. Recipient block holders are held very firmly in place by two magnets located on the base plate. Two strips of tape also help hold the recipient block holders securely by increasing friction. Users who exchange recipient block holders frequently may want to facilitate the exchange by increasing 8. The turret wobbles 9. Micrometer readout problems Difficulty exchanging recipient blocks Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD the tape thickness by adding another layer. This increases the gap between the magnets and the recipient block, thereby reducing the magnetic force. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD v. FREQUENTLY ASKED QUESTIONS General questions regarding tissue arrays: 1. What about tumor heterogeneity and tissue arrays? How many punches do you need to get a good representation? Depends on tissue type and the purpose of the study. As a rule of the thumb, making tissue arrays from normal breast epithelium, normal kidney and cancers with high degree of regional heterogeneity probably require 2-4 punches per tissue whereas most cancers are well represented with 1-2 punches. See Camp et al, and Torhorst et al, for technology validation papers discussing the use of tissue arrays in evaluating prognostic markers. 2. How many specimens can you include per array block? Number of specimens per array depends on the size of the punches and the desired array density. Using 0.6 mm punches you can construct tissue arrays with 500 or more specimens per block using regular tissue cassettes. Using 2 mm punches allows construction of tissue arrays with about 50-100 specimens. 3. How long does it take to make tissue arrays? Making tissue arrays should be considered as a project that involves many steps. Array construction itself is relatively fast as compared to the other, necessary preparatory steps that include marking of the representative tissue areas for punching. It is realistic to reserve a couple of weeks for completing tissue array construction project for an array consisting of 400 specimens. Because setting up an arraying project takes a considerable amount of time, it often makes sense to construct multiple replicas of the array blocks simultaneously. Making multiple replicate tissue array blocks is faster and more convenient with the automated arrayer than with the manual arrayer. See Arrayer comparison table for estimated core transfer rates for the automated and manual instruments. 4. How do you cut sections from the array block? Some users prefer to cut sections using regular microtome sectioning techniques; some prefer to use adhesivecoated slides from Instrumedics. The advantage of using coated slides is that even beginners can make good sections with the system and you have precise control over the orientation of the tissue array sections on the microscope slides. If you decide to apply conventional sectioning techniques, briefly heating the block at 35-37 degrees C for about 20-30 minutes (and letting the block to cool back to room temperature) before sectioning improves the section quality. 5. How many sections can you cut from typical tissue arrays? Depending on the height of the original donor tissue blocks you can cut 100-300 sections from tissue arrays. 150 sections is a reasonable expectation for a typical tissue array. 6. Can you make frozen tissue arrays with Beecher's instruments? It is possible to make small frozen tissue arrays with the manual instrument. See Fejzo et al for description. However, this approach is relatively difficult and keeping the tissue array quality high is challenging. Beecher is currently working on a prototype frozen tissue arrayer device. This instrument is not yet available for sale, but you can contact us regarding custom arraying. Questions about the manual arrayer: 7. How to align punches in the manual arrayer? First, to verify punch alignment, place a blank paraffin block in the block holder and put this complex in position on the arrayer as if it were a recipient block. Press the smaller punch down until it leaves a mark in the paraffin surface. Move the turret to switch the larger sampling punch in position, and again make a mark on the paraffin surface. Adjustment is needed if the marks are not coincidental. Punch holes that appear one in front of the other need front to back adjustment; holes to the side of each other require left-to-right alignment. The blue arrow points to the left-to-right setscrews, the orange arrow indicates the location of front-to-back setscrews. Adjusting front-back alignment of a punch with the setscrew located in front of the arrayer. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD Questions arise during the construction of the TMAs: 8. For USC CFR protocol, what percentage of tissue can be taken from one block? Remove tissue NOT to exhaust the block, so that large section can be cut after all arrays have been made is: about 20% of tissue per block. 9. If there is not enough tissue from a block and a second block from the same subject is available, can the second block be used to provide more cores for the TMAs? Yes. Make sure Spec ID be documented. 10. Should tissues from different blocks of the same subject be taken to deposit on the array block? Ideally and scientifically, same source of tissue should be taken for the same array block, especially for the A/C/N array which tumor progression can be studied. 11. If a hole in one array block was damaged, what should we do? Skip that hole which means one replicate block lesser for the set of array blocks. If the tumor is large enough to make an extra series, these duplicates will consider the QC for the assay. In any mean, always make the same localization in a set of array blocks for the same donor tumor. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD APPENDIX 1. Protocols for Pathology Reporting and Sample Collection (revised March 1, 2001) 1. All cancer diagnoses should be verified where possible (death certificates, registries, reports, pathology review), 2. 3. 4. 5. 6. 7. 8. 9. 10. and method of verification should be recorded. Pathology review is the gold standard for verification, and when possible using the CRFCCS Colorectal Cancer form on http://www.cfr.epi.uci.edu/colon web site. Tumor blocks should consist of approximately 70-80% tumor cells. If available, a block of normal tissue should be retained for each patient, particularly if deceased and/or if blood is not available. Preferably, the same tumor block should be used to obtain sections for MSI (microsatellite instability) and IHC (immunohistochemistry). If the block containing the highest percent tumor cells contains insufficient tissue for both MSI and IHC sections, a second tumor block may be used for IHC. One H&E-stained (hematoxylin and eosin) section representative of the tumor block should be made. If sufficient material is available, the first and last sections of a block should be stained with H&E. Protocol for IHC: Tumor tissue only required. Prepare 10 x 5 (or 4) micron paraffin sections from tumor block and mount on Probe-On slides (no coverslip). Five slides will be used for IHC testing of MLH1, MSH2 and MSH6 proteins. One H&E slide should be shipped to the IHC testing center along with the five Probe-on slides. The remaining slides will be stored at the original site as back-up or for future molecular studies. QC for IHC should include review by an independent observer. Protocol for MSI: Both tumor and normal tissue required. Prepare either: I) 20 x 5 micron tumor sections on unbaked slides (no stain/coverslip) where normal and tumor can be isolated separately. or II) 10 x 5 micron sections from tumor block (containing >80% tumor) and 10 x 5 micron sections from normal block on unbaked, unstained slides or in separate sterile microcentrifuge tubes. Normal DNA can also be obtained from blood samples if normal block is unavailable. For sections requiring microdissection, an H&E slide must be prepared from the same block. MSI testing is to be performed on all CFRCCS probands and preferably on all colon cancer cases. Where possible, MSI testing to be performed on two cancers per family, or three when only one of the two gives a positive result (MSI-H). An endometrial cancer may be used in place of colorectal cancer for MSI testing. IHC testing for absence of MLH1 and MSH2 (and at some centers MLH6) protein expression should be performed on all probands and affected relatives with tumors that are MSI positive with greater than 30% of a minimum of 5 markers, or show MSI with any mononucleotide marker (including: BAT25, BAT26, BAT40 and BAT34C4). Some centers are funded to test for additional proteins and/or cases. If blocks need to be returned prior to preparing sections for IHC/MSI, a mini-block containing sufficient tissue for the required sections may be made and stored. Following IHC and MSI testing at off-site facilities, all slides (stained, unstained and H&E) will be returned to the original site for permanent storage. Slides/sections should be stored in the dark under conditions that insure greatest integrity of the specimen. Both stained and unstained slides can be stored at room temperature in slide boxes or stacked vertically in slide trays /cabinets. Storing at 4 C may better maintain protein integrity. Back to Molecular Characterization & Pathology Main Minutes Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD APPENDIX 2. Material Specification of the bar-coded labels for glass slide. DeltaOne Software 714-528-SCAN Material Description TS822 DESCRIPTION: TS822 label material is designed with an overlaminate flap that is placed over the image after printing. This “Flap” is for additional image protection against many harsh chemical environments. The adhesive is formulated to permanently bond to the most demanding surfaces including textured and contoured surfaces or in applications where a slightly thicker adhesive is required. This construction is intended for use in histology, cytology, and research laboratories. The labels are resistant to water, xylene, alcohol, ethanol, methanol and other common histological stains. Labels must be applied to the painted or frosted sections of glass slides to insure maximum bond. CONSTRUCTION: OVERLAMINATE Thickness .002” nominal Material clear polyester Adhesive .001” nominal clear acrylic TOP COATING Thermal transfer receiver coat compatible with hard resin ribbons BASE MATERIAL Thickness . 002" nominal Material white polyester ADHESIVE Thickness .002" nominal Material high holding acrylic LINER Thickness .0032" nominal Weight 55 lb. Material densified, bleached, kraft paper RIBBON COMPATIBILITY: Datamax All except Ovation & E-class series Zebra All Models except T402 Eltron For Desktop Models Intermec For Models 3240/3440 1st Choice TR611 TR611Z TR611HZ TR611Z 2nd Choice TR601 TR601Z TR613HZ TR601Z CHARACTERISTICS: Service Temperature Range: -40 F to +257 F (-40 C to +125 C) Minimum Application Temperature: +50 F (+10 C) Typical Minimum Narrow Bar Width: Step Ladder Orientation - .010, Picket Fence Orientation - .005 Using certain printer, ribbon, heat, and speed combinations a smaller narrow bar width may be achieved. Typical Automatic Applicator/Dispenser Use: Not Tested Poor Fair Good Excellent Label size and orientation will affect performance. Specific designs must be individually tested. To assure maximum performance, Sigma Systems materials have been designed and tested for compatibility between the label stock and thermal transfer ribbon. All Sigma Systems materials are sold as a package, containing label stock, thermal transfer ribbon and a print head cleaning pen. All technical information and recommendations are believed to be accurate but do not constitute a guarantee or warranty. Suitability for any given application is the responsibility of the user. Computype reserves the right to change specifications without notice. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD If you have further questions, please call DeltaOne Software 714-528-7226 . Issue Date: 02/24/00 Revised: 12-18-01 Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD APPENDIX 3. Shipment Notification Procedure For Paraffin Embedded Tissue 1. The lab MUST be notified prior to the shipment. 2. Include the following information in your e-mail. Send to all personnel below: Ofeliya Avetisyan E-mail: oavetisy@usc.edu Tel #: (323) 865-0583 Qingru Feng E-mail: qfeng@usc.edu Tel #: (323) 865-0581 Anh Diep E-mail: atdiep@usc.edu Tel #: (323) 865-0713 Attach a copy of the standard lab TUMOR SHIPPING LOG sheet. Provide the FedEx tracking #. 3. Package should be sent to the lab using the following shipping address: Anh Diep c/o Haile’s Lab USC Keck School of MED – Norris Cancer Center Topping Tower 5421, 5427 and 5429 1441 Eastlake Ave. Los Angeles, CA 90033 Lab Line #: (323) 865-0585 Fax #: (323) 865-0140 4. The lab will acknowledge the arrival of the package immediately upon receiving (with a “cc” to Pat Harmon). Then follow with a report of the tumor accessing status within the next few days. 5. After processing (one month turn around time), the lab will be responsible to return the tissue to the coordinators. We will notify the coordinators in advance with FEDEX tracking information through e-mail As soon as the coordinators receive the package, the lab requests a confirmation also through e-mail. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD APPENDIX 4. TMAs SUPPLIES/REAGENTS ORDERING CHECKLIST Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD APPENDIX 5. Rationales for TMA The Colorectal Cancer Family Registry (Colon CFR) is an NCI-supported, international consortium, with six major centers in the U.S., Canada, and Australia (with over 20 participating institutions). The Colon CFR represents the largest single resource in the world for studies of the causes, prevention, and clinical management of families at enhanced risk of colorectal cancer. Collectively, to date there are greater than 11,000 families participating in the Colon CFR. The Colon CFR collects blood samples, extensive questionnaire data on risk factors, and clinical follow-up on participants. Pathology reports and pathology specimens are considered a critical core element of the Colon CFR. All centers are required to obtain tumor tissue and normal margin derived from paraffin-embedded tissue (PET) from probands and selected other cases in the participating families. Some centers are also collecting fresh frozen tissue to facilitate proteomics analysis and other analyses that are not feasible from PET samples. In the past, PET samples were simply sectioned; however, most centers are now either obtaining cores or plan to obtain cores to facilitate tissue micro-arrays (TMAs), which will provide future scientists with a rich and flexible source of tumor and normal tissue. Having access to tumor and normal tissue is critical to the success of the Colon CFR, since the ability to study PET-derived material is an integral part of the overall research plan of the Colon CFR. Examples of ongoing research that involve pathology specimens include the following: 1. Determination of MSI status on over 8,000 cases, representing the largest study of MSI in the world. This is a critical variable since evidence suggests that the causes of MSI-H, MSI-L, and MSS tumors are different from each other, as is the clinical prognosis and response to chemotherapeutic drugs. 2. Conduct of immunohistochemistry (IHC) tests for expression of the mismatch repair (MMR) genes that cause hereditary non-polyposis colorectal cancer (HNPCC). Studies are underway that are assessing the agreement between MSI status, IHC results, and MMR mutation status, with results that will likely change the testing protocols for HNPCC and the MMR genes. 3. Studies of hypermethylation of hMLH, which represents a very important alternative means of “shutting down” the hMLH1 gene (one of the MMR genes). 4. Studies of somatic mutations in BRAF, which appears to be strongly associated with a CPG island methylator phenotype (CIMP), an important alternative pathway for causing colorectal cancer. 5. A study to identify the mechanism for the “second hit” in tumors from subjects with a germline mutation in one of the MMR genes. 6. MSI and IHC results are used to triage who gets tested for germline mutations in the MMR genes, which will then enable investigators to estimate the lifetime risk of colorectal cancer among mutation carriers and identify what environmental or lifestyle factors modify this risk. Pathology results are also used to triage families into new gene linkage studies to map new colorectal cancer genes. Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD Plans for future research using PET samples include: 1. A study of methylation events in 20 genes in about 8,000 cases, the most comprehensive study of methylation in colorectal cancer in the world. 2. Greatly expanded studies of somatic mutations, including BRAF, kras, p53, and other genes. 3. Use of pathology variables (MSI and IHC) to triage families into a planned genome-wide association study. 4. Use of MSI, IHC, and MMR mutation status as key variables in four funded studies of candidate gene pathways: a) folate/vitamin D/calcium; b) NSAIDs; c) lipid peroxidation; and d) obesity/metabolic syndrome, IGF). 5. Studies of comparative genome hybridization (CGH) in different types of colorectal cancer (MSI-H, MSI-L, MSS) and in samples from normal margin compared to adenomatous changes compared to cancer. Studies of mRNA expression in PET samples are also planned. In summary, molecular studies of PET samples are critical to the objectives of the Colon CFR to better understand the causes of colorectal cancer and their biological mechanisms. With this enhanced understanding, our ultimate goal is to develop more effective preventive strategies, perhaps tailored to each subject based on their genotypes and the molecular profile of any precursor lesions such as adenomas, and to develop more targeted therapies. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD D. Processing of Other types of biospecimens Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD FINAL CELLULAR AND GENETIC MATERIAL PREPARATION Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD A. Preparation of DNA Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD DNA extraction from buffy coat A. Diep, 9/91; Modifications from F. Baas, H. Bikker, et al.(Hum. Genet. 67, 301(1984), Gustafson et al. (Analytical Biochem. 165, 294-299 (1987) and Paul et al. (Hum. Genet. 75, 264269 (1984). The protocol yields DNA of good quality with a standardized procedure designed to minimize the number of steps and manipulations. To frozen buffy coat, add lysis buffer (144 mM NH 4Cl, 14 mM NH4HCO3) after transferring to a 15 ml plastic tube. Mix gently by inversion and let sit for 5 minutes. Add the pellet with pellet buffer (10 mM Tris pH 8.0, 10 mM EDTA, 150 mM NaCl). To the homogenous suspension, at room temperature, add proteinase K, 10% SDS, and RNAse (optional) all in the 15 ml tube. Gently invert the tube, and then incubate at 50 C for ~16 hours. The solution should be reasonably clear after proteinase digestion. The purification is carried out by adding protein-denaturant buffers, phenol and chloroform. Mix well. Separate phases by centrifuging at 3500 rpm for 15 minutes. Remove the bottom phase and discard. Check and repeat the extraction until all particles have gone to the interphase, leaving a clear DNA aqueous phase. Precipitate by adding NaCl to make a final concentration of 100-250 mM and 2 volumes of cold Ethanol. Mix to obtain a tight white precipitate. Cold spin at 3500 rpm for 30 minutes. Aspirate the supernatant . Air dry the pellet. Resuspend it in TE (10 mM Tris, 0.1 mM EDTA, pH 8.0). Mix the tube until the DNA is completely resuspended. After the DNA is completely dissolved, remove some aliquots to determine its purity, concentration, integrity, and digestibility. Store the working DNA solution at 4C and the back ups at -20C. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 11, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD STEPWISE PROCEDURE Protocol designed to have: The information of when a step can be interrupted. Condition on hold. Volume for the aliquots prepared. Reagents and Equipment -20C, -80C freezers 0.6x TBE, pH 8 10 ml tube racks 10% SDS (w/v) 10 x Ficoll loading buffer 12x75 mm borosilicate disposable culture tubes 37C, 50C water bath 4C refrigerator 5 M NaCl Aqueous alcohol (70%, v/v) Biohazard waste container Black sharpie pen Blood protective pads Blood protective pads Centrifuge Chloroform Cold absolute ethanol Compet dispenser Sterile 10 ml disposable pipettes ddH2O Disinfectant: Bleach solution, 0.1% phenol Disposable latex gloves Electrophoresis apparatus Ethidium bromide (5 mg/ml) Fluorometer Foil Fume hoods Glass beakers waste Glass bottle for organic waste Glass waste container Hind III and 10X reaction buffer Hoechst dye Ice bucket Isoamyl alcohol Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 11, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Kimwipes Lysis buffer Mixer Molecular biology grade agarose MW markers P20, P200, P1000 Pipettemen Parafilm Pellet buffer pH meter: HCl, NaOH Phenol Pipetaid Proteinase K RNase A Spectrophotometer Sterile aerosol-preventive pipette tips Sterile polypropylene 15 ml centrifuge tubes Stirrer TE, pH 8 Transfer pipettes Solution Preparation: Lysis Buffer (500 ml) 0.144 M NH4Cl [MW=53.49] 0.0144 M NH4HCO3 [MW=79.06] Raise to 500 ml with sterile ddH20. Filter-sterilize. 3.851 g 0.553 g 5M NaCl (500 ml) 146.1 g NaCl, raise to 500 ml with sterile ddH20. Pellet Buffer 10 mM Tris-HCl, pH 8.0 10 mM EDTA 150 mM NaCl Stock Solutions: 1M Tris-HCl, pH 8.0 0.5M EDTA 5M NaCl Sterile ddH2O Total volume 0.5 ml 1.0 ml 1.5 ml 47.0 ml 50.0 ml Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine 1.0 ml 2.0 ml 3.0 ml 94.0 ml 100.00 ml Drafted Jan. 11, 1999 Revised Feb 4, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD TE, pH 8.0 10 mM Tris-HCl, pH 8.0 1 mM EDTA, pH 8.0 Stock Solutions: 1M Tris-HCl, pH 8.0 5 ml 0.5M EDTA 1 ml Raise to 500 ml with sterile ddH20. Autoclaved. Phenol Preparation 1. Melt phenol by heating @ 650 C. 2. Add 1 volume of 0.5M Tris pH 8.0. Shake vigorously. 3. Separate by using separatory funnel. Discard aqueous layer ( top layer ). 4. Repeat step 2 again. 5. Check pH of both phenol and aqueous phase : pH of phenol 6.5 - 7.0; pH of aqueous phenol. 6. Separate phases. 7. Transfer phenol to brown bottle and add 1/3 volume of TE. 8. Store at 40C Proteinase K A frozen stock is prepared by dissolving Proteinase K lyophilized powder at 10 mg/ml in dissolving solution as instructed by the manufacturer. Once dissolved, the solution is aliquotted into smaller volume. Store at -20 oC. The enzyme is stable at least one year. RNase A Frozen stock of 5 units/l is prepared by dissolving 1 g of RNase lyophilized powder in sufficient sterile water to give 5 units of RNase/l, followed by boiling 15 minutes to inactivate DNases. The stock is cooled, make 1 ml aliquots into sterile 2 ml tubes, and stored frozen at -20 oC. Hoechst dye Solution (“ fluorometry solution””) Add 12 g NaH2PO4 ( monobasic, anhydrous) or 13.8 g NaH2PO4.H2O, 233.8 g NaCl, and 4 ml of 500 ug/ml Hoechst dye. Raise volume to 2 liters with ddH2O. Adjust pH to 7.4 with 10 N NaOH (~20 ml). Store at -20C in 1 ml aliquots using brown or foil-wrapped bottles or tubes. Solution can be stored at -20C up to 6 months. 10 x TBE, pH 8 ( 1 L) 90 mM Tris-HCl, pH 8.3 [FW=121.1] 108 g 90 mM Boric acid 55 g 2 mM EDTA 40 ml 0.5 M EDTA (or 7.44 g EDTA [FW=372.2] ) Raise to 1 L with sterile ddH20. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 11, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD 250 ml Nuclei Lysis Mixture: (freshly prepared) In wash bottle, add 235 ml pellet buffer 12.5 ml 10% SDS 2.5 ml 10 mg/ml Proteinase K 1L Phenol: 25: 500 ml Chloroform: 24: 480 ml Isoamyl alcohol 1 20 ml Stepwise Procedure: Isolation of Nuclei: 1. Thaw the frozen pellets. Mix 5-7 times by gentle inversion. 2. Transfer the pellet from 2-ml microcentrifuge tube into the labeled sterile 15 ml polypropylene centrifuge tube. Wipe top of tubes with ethanol before opening the cap. Do not use glass tube, because DNA will stick to glassware. Polypropylene tubes must be used, because chloroform which is used later in the organic extraction is a solvent for polystyrene. 3. Rinse the tube with a equal volume of lysis buffer. Let the tube sit on ice for 5 minutes to disrupt cell membrane. !!!Freeze at -80C until further extraction. 4. Thaw the frozen pellets by placing the 15 ml tube in room temperature water bath. 5. When thawed, resuspend in 3 times the original volume of pellet buffer. For large scale setup, bring all tubes to same final volume with pellet buffer. 6. Keep the tube on ice for at least 5 minutes to complete lysis of the nuclei membrane. Invert at 20-30 second interval several times. !!!Store at 4C until further extraction. Dissociation of nucleic acid-protein complexes 7. Add Proteinase K to a 200 g/ml final concentration. Optimal proteolytic activity need at least 100 ug of Protinase K per 10 cells. There is ~5x106 cells in 1 ml whole blood; ~20 ml whole blood collected from this study. 8. Add 10% SDS (w/v) to a 1% final concentration. Mix gently by inversion. Solution is now viscous as DNA is released from cells. For large scale setup, SDS and Proteinase K can add together with pellet buffer in one step by making nuclei lysis mix. Again, bring all tubes to the same final volume. 9. Incubate tube in a 50C waterbath overnight (16 hours) without agitation. RNA removal (optional): RNase may be added at this time, though generally not necessary. 10. Add RNase A to a concentration of 100 g/ml. 11. Incubate at 370 C for 30 minutes. Spin to collect volume. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 12, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Organic Extraction to deproteinize DNA: 12. First extraction, add equal volume of phenol only. Mix gently until solution forms an milky emulsion. 13. Centrifuge at room temperature at 3500 rpm for 15 minutes. Remove phenol, lower phase by sterile transfer pipette. Discard phenol. The white precipitates at the bottom of the top interphase layer are proteins and are to be extracted out from the DNA solution. An extensive white film indicates incomplete digestion with Proteinase K. More digestion should be performed. Do not use glass pipette, because DNA will stick to glassware. DNA should not be left in the presence of denaturants. 14. Second extraction, add equal volume of the mixture of denaturing agents, 25:24:1 phenol: chloroform: Isoamyl. Mix gently until solution is milky. 15. Centrifuge at room temperature at 3500 rpm for 15 minutes. Remove the mixture of denaturing agents, lower phase by sterile transfer pipette. Discard. 16. Add equal volume of chloroform only. Mix thoroughly. Spin at 3500 rpm for 15 minutes. Remove lower phase, chloroform to be discarded. At this step, carefully work tip around the tube and get as much as you can the white film of precipitates at the bottom of the top layer without disturbing the clear DNA layer on the top. Keep bottom layers of phenol and chloroform in case DNA is fail to be obtained in the top layer. Precipitation of DNA: 17. Add 5 M NaCl to a final concentration of 100-250 mM NaCl. 18. Add 2 volumes of cold absolute ethanol. Mix immediately by inverting the tube for at least 30 seconds. Observe for the formation of a visible mass of cloudy, white threadlike strands of DNA. If no precipitate is seen because DNA is fragmented, freeze the sample at -80C for 30 minutes to pellet the DNA before centrifugation. !!!Freeze at -80C until further extraction. 19. Centrifuge at room temperature at 3500 rpm for 30 minutes. The DNA will be visible as a small white pellet at the bottom of the tube. 20. Decant the supernatant by invert the tube. The DNA pellet is very loose at this point and care must be used to avoid losing the pellet. 21. Wash the DNA pellet and the sides of the tube with 2 ml of 70% ethanol for several times. Centrifuge at room temperature at 3500 rpm for 1 minute. (optional) 22. Remove most of the supernatant by invert the tube upside down on a clean absorbent paper for about 5 minutes. Do not leave tube in this position for too long, because the pellet will drop down on the paper. 23. Continue to air dry the pellet thoroughly for 30 minutes. The pellet should not be overdried. Over dehydration of DNA can cause denaturation of the DNA. !!!Store at 4C until further extraction. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 12, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Rehydration of DNA: 24. Resuspend the dry pellet in 1-1.5 ml 1xTE by gently invert tube at 370C for 4 hours or room temperature for overnight. The DNA will continue to dissolve at 40C for 1-2 days. Make sure the TE volume added sufficient to rehydrate the pellet, at the same time try to obtain a high concentration DNA. Make certain that the DNA is homogeneous before the determination of its concentration. Although viscous, the solutions should look homogeneous with no large “ globs” of partially undissolved DNA. Average yield for genomic DNA from whole blood or buffy coat is 25-40 g/ ml of blood. !!!Store working solutions at 4C and back ups at -20C. Quantitation of DNA by OD260 determination: Prepare a series of dilution of small aliquots of the DNA in ddH2O in labeled Ubottom microtitrate plate. (Usually 1, 2, and 5 l to a final volume of 100 l). Mix diluted samples well with pipetteman. A blank must always be used to zero the Spectrophotometer. This is the same ddH2O used for diluting DNA. Using the Beckman DU Series 600 Spectrophotometer: 1. From the main menu, click A:\Nucleic Acid from the Custom Applications list. 2. The next screen should have three columns, OD260nm, OD280nm and OD260/OD280. Make sure “UV on” near the bottom of the screen. 3. Insert the blank, and click on “Blank” on the bottom left of the screen. 4. Insert your samples and click on “ReadSamples” on the top left of the screen after each sample. Clean the cuvette with water and alcohol. Invert and tap onto paper towels to dry the cuvette as much as possible. Dry the outside of the cuvette carefully with Kimwipes or lens paper. 5. When you have gone through all your samples, turn off UV. Then click on “SaveClear” . Click on “A:\” to toggle between A drive (in computer) and B drive (disk). Click on “ Work_Res” to change the name of the file. Click on “QUIT” to exit. It will ask you if you want to save changes in method A:\ Nucleic Acid and you should click “YES” . 6. From the main screen, choose “FILE UTILITIES” under the Utilities list. 7. Click on “Disk status” . In B:\FIX_DATA there should be B:\filename. DUF where filename is what you re-named “ Work_Res” in step 5. Click on this filename and then click on “Convert” . Choose destination drive [B] by clicking on [A]. Choose what kind of file by toggling between [LOTUS] and [ASCII]. (Haile’ s lab has Lotus.) Then click on “OK” . “Quit” to exit. After bringing the disk to your computer, open Lotus 1-2-3 and then open the disk. Under “ Lotus” have the computer look for files with the ending “WKS” by changing “WG?” Try to save the file as an excel file so you can open Excel and calculate the OD260 / OD280 Ratio andDNA Concentration in ng/ul. OD260* dilution factor * coefficient for DNA Where dilution factor is usually 100, 50 and 20, and the coefficient for DNA is 50. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 12, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Quantitation of DNA using fluorometer: For each sample, make 10 ul DNA solution in 2 ml Hoechst dye solution. Vortex 30 seconds to mix. Let sit at least 15-20 minutes for dye reaction. For the same batch of measurement, make sure that all samples will have the same amount of reaction duration. Use 12x75 mm borosilicate disposable culture tubes. Turn on fluorometer, allow 15 minutes to warm up. Set GAIN to 10 and SPAN all the way counter clockwise. Adjust blank to zero by turning the ZERO knob until span reading indicates 000. Read samples and record. If reading is higher than 2000 ug/ml or above the linear range, dilute DNA 3:1 with dye solution and read again. Blank using 2 ml Hoechst dye solution. Wipe tube with kimwipes or lens paper. Using the Sequoia-Turner M450 fluorometer: 1. The standard curve is made using 0-2000 ug/ml calf thymus DNA with stock concentration of 100 ng/ul in 1 ug/ml Hoechst dye solution. 3. Plotting mean span vs. concentration of standard curve: Prepare DNA standards in duplicate, as listed in the table below: Concentration, [ ___ ng/200 ul] Volume of 100 ng/ul stock DNA to use, in ul 0 50 100 200 300 500 1000 2000 0 0.50 1.00 2.00 3.00 5.00 10.00 20.00 Volume of fluorometry solution to use, in ul 2000.0 1999.5 1999 1998 1997 1995 1990 1980 Make sure the standard curve is in linear range. *A new standard curve should be prepared for each new batch of Hoechst dye solution. Determination of DNA purity by taking OD260/OD280 ratio: The quality of the DNA sample isolated will be evaluated before use by checking its absorption spectra. Calculate the ratio of absorbance at 260 to 280 nm. Ratio should be optimal from 1.8-2.0. Very low ratio (<1.6) may indicate significant protein contamination. Very high ratio (>2.0) may indicate significant RNA contamination. Samples that have consistently low or high ratios may require re-extraction; increase the sample incubation time with Proteinase K; more ethanol washes to remove trace phenol. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 12, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Determination of DNA Integrity: Run uncut DNA on a 1% agarose gel with a standard of known concentration. Observe for the intact band of DNA at high molecular weight and no sign of degradation shown as a smear near the lowering part of the gel. Precautions should be taken to maximize genomic DNA molecular weight by minimizing shearing force due to not gentle mixing during extraction steps. Visually check DNA purity by observing no sign of RNA which migrate at very low molecular weight. Determination of DNA Digestibility: The absence of trace organic solvents, salts, cellular proteins and proteinase K in the final DNA solution is important for susceptibility of the genomic DNA to restriction enzyme action. Cut 200 ng of isolated DNA with 1 to 5 units of Hind III in the presence of 10X reaction buffer, and appropriate cocktail for the enzyme. Incubate overnight at 37 oC . Electrophoresis run the digested product and same amount of undigested DNA on 1% agarose in 0.6x TBE, then UV visualizing the ethidium bromide stained material to examine its digestibility. Samples digestible with these restriction enzymes will appear as an even smear on the gel and have no sign of high molecular weight bands. Repeat digestion of any samples that were not digestible with either restriction enzymes. If sample is consistently indigestible, it may require re-extraction or replacement. Uncut samples that are severely degraded require replacement also. DNA Typing for mix-up clarification by microsatellite analyses : Use microsatellite that has high discriminating power to QA&QC test of a small number of randomly picked DNA samples. Microsatellite analysis allows us to compare the genotypes between aqueous DNA source and DNA from bloodstain. PCR setup of less than 20 ng of DNA using D1S80 that is mapped at the distal of Chromosome 1 and has the discriminating power of 95-98%. PCR product of 350 bp-1 kb size will be electrophoresed on native agarose gel and then UV-visualize the genotype. Samples that are identified as mix-up will be excluded or hold for further resolution. Data Records and Reports Extraction Sheet Concentration Sheet Digestion Sheet DNA Typing Sheet DNA inventory log-in Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Feb 4, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD DNA extraction from dry blood stains Elkhouly, Liu et al.(Haile’s 3/2000), modified from Brockmoeller et al., and Lin’s Reagents and Equipment: 1.2 mm-HARRIS MICRO-PUNCH Micro-titrate plate, V-bottom 5% Chelex ddH2O Stir bar Stirrer Glass beaker P20, P200 Pipettemen Sterile aerosol-preventive tips Disposable latex gloves Glass waste container Kimwipes 01% phenol sterilized toothpick Solution Preparation: 5% Chelex Add 5g of Chelex 100 Resin in 100 ml ddH2O STEPWISE PROCEDURE Making blood spot: 1. Place the bloodstain onto the cutting mat. 2. Gently push the 1.2mm-HARRIS MICRO-PUNCH downward onto the sample, rotating the barrel clockwise and counter-clockwise. 3. Lift the barrel up from the sample. 4. Transfer the spot over a micro-titrate well, push it out by pressing the plunger, release it with a sterilized toothpick. 5. Decontaminate the hole-puncher with 0.1% phenol between samples. Extraction: To each micro-titrate well with a blood spot, 1. Add 10ul of methanol. Air dry thoroughly. 2. Add 10ul BSA to the final concentration of 2ng/ul. 3. Heat for 20 minutes at 95C on a thermal cycler. 4. The sample is ready to use for PCR reaction (suggested volume is10 ul). Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Mar 14, 2000 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD DNA extraction from paraffin-embedded-tissue (USING THE QIAamp DNA MINI KIT) Notes: - Use PCR-grade water and reagents - Use filter tips - Ensure that buffer AL, buffer AW, and proteinase K have been prepared according to instructions (see below). If a precipitate has formed in buffer AL or buffer ATL, dissolve by incubating at 55oC for 2 min - Prepare a 55oC water bath for use in step 7, and a 70oC water bath for use in steps 9 and 16 - Equilibrate buffer AE or water to 70oC for elution in step 16 - All centrifugation is carried out at room temperature To the buccal cell pellet add 180ml buffer ATL Add 20ml of proteinase K stock solution, mix by vortexing, and incubate at 55oC for 3 hours. Vortex occasionally during incubation to disperse the sample Add 200ml buffer AL to the sample, mix again thoroughly by votexing, and incubate at 70oC for 30min Note: A white precipitate may form on addition of buffer AL. In most cases it will dissolve during incubation at 70oC. The precipitate does not interfere with the QIAamp procedure, or with any subsequent application. Add 200ml of ethanol (96-100%) to the sample and mix thoroughly by vortexing. Note: A white precipitate may form on addition of ethanol. It is essential to apply all of the precipitate to the QIAamp spin column. This precipitate does not interfere with the QIAamp procedure, or with any subsequent application. Place QIAamp spin column in a 2ml collection tube (provided). Carefully apply the mixture from step 10 (including the precipitate) to the QIAamp spin column without moistening the rim, close the cap, and centrifuge at 6000 x g (8000rpm) for 1min. Note: If the lysate has not completely passed through the column after centrifugation, centrifuge again at higher speed until the QIAamp spin column is empty. Place the QIAamp sping column in a clean 2ml collection tube (provided) and discard the tube containing the filtrate. Carefully open the QIAamp spin column and add 500ml buffer AW1. Centrifuge at 6000 x g (8000rpm) for 1min. Place the QIAamp spin column in a clean 2ml collection tube (provided) and discard the collection tube containing the filtrate. Carefully open the QIAamp spin column and add 500ml of buffer AW2. Centrifuge at full speed for 3min. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Mar 14, 2000 AD The additional full speed spin removes all traces of buffer AW from the QIAamp spin Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD column before elution. Place the QIAamp spin column in a clean 1.7ml microfuge tube (not provided) and discard the collection tube containing the filtrate. 16. Carefully open the QIAamp spin column. Elute the DNA once with 50ml buffer AE. Incubate at room temperature for 1min, then centrifuge at full speed for 1min. Reagents and Solutions: QIAamp DNA Mini Kit (QIAGEN Cat. # 51304 (50 preps), Cat. # 51306 (250 preps)) Proteinase K stock solution: Add 1.4ml of distilled water to the lyophilized QIAGEN proteinase K. Store at –20oC. Buffer AL: Prepare buffer AL by decanting all of reagent AL1 into buffer AL (Reagent AL2). Mix thoroughly by shaking. Buffer AL is stable for at least 1 year when stored in the dark at room temperature. Do not add QIAGEN proteinase K directly to buffer AL Buffer AW: Buffer AW is supplied as a concentrate. Before using for the first time, add the appropriate amount of ethanol (96-100%) to buffer AW concentrate as indicated on the bottle. Buffer AW is stable for at least 1 year when stored closed at room temperature. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Mar 14, 2000 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD B. Preparation of RNA (To Come) Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD C. Preparation of Lymphobastoid cell line (To Come) Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD STORAGE, PACKING AND SHIPPING OF BIOLOGICAL SPECIMENS Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD 1. Storage A number of technical issues may limit the usefulness of the biospecimens stored for many years in a biological bank: The temperature of storage, which affects stability. The availability of the appropriate biological material needed for a given analysis. The amount of the blood samples recruited per subject which may limit the number of the laboratory analyses The size of each aliquot should be the smallest increment possible, to avoid thawing and re-freezing the samples, a process which may damage some analytes. In this section, we documented the methods of storage for different cellular and genetic material preserved from 30cc to 40cc blood of each subject, as well as the availability of the resources and the size of the aliquots for this study: A. Blood cards a. Each participant will have one blood card with 22 x 20ul-blood spots. b. This card will be wrapped with a weighing paper and put in a coin envelope. c. File the envelope in a banker box chronologically. d. Store at room temperature in a climate controlled laboratory. The capacity of a 2-drawer banker box: about 150 envelops per drawer. B. Plasma a. Each participant will have 20-30 of 0.5 ml aliquots of plasma from 30 ml blood. b. The number of aliquots obtained will be split into two batches per subjects. c. Store in two different -70 oC freezers. C. Buffy coat/Red Blood Cell Residual from EDTA blood a. Transfer buffy coat/blood residual into 3-15ml centrifuge tubes respectively. b. The three buffy coat/blood residual tubes will be temporarily stored at -20 oC for DNA extraction. c. Extract the DNA from these tubes in two batches. First extraction batch will only be for blood tube #1. The others will be extracted in second batch. D. WBCs from ACD blood a. Each participant will have about 4 of the 1 ml aliquots of WBCs with less than 2x106 cells per aliquot. b. Store in two different liquid nitrogen tanks. E. DNA a. From blood spots: DNA extracted from this source is for direct PCR only, no storage required. b. From EDTA buffy coat/ residual rbc or EBV cell lines: All extracted DNA from each subject will be stored in two different -70 oC freezer. Preserve DNA in high concentration allows us to provide the researchers with different concentrations according to their studies. However, at least one 10-g aliquot of original stock must be reserved, until a cell line has established. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Dec 30, 2002 AD 2. Packing Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD A. Specimen preparation for packing 1) Allow samples to thaw if aliquots need to be made. Aliquot the amount of sample requested into the corresponding size of tubes. 2) Check that all the caps are tightened. 3) Check all tubes or specimens in general against the shipping list. B. Packing 1) If only a few samples are shipped: a. Wrap tubes onto cardboard panels and in bubble wrap. b. Place in brown cardboard shipping boxes. 2) If many samples are shipped: a. Place individual sample in storage boxes or mailers. b. Secure the specimens with sufficient fillers. c. Secure storage boxes with rubber bands. d. Wrap in bubble wrap. e. Place storage boxes in cardboard shipping boxes. f. Again secure the storage boxes with sufficient fillers. 3) Packing the blood cards: a. Separate the blood cards from different subject by placing each card in an envelope. b. Pack all blood cards in a ziplock bag or cardboard box with sufficient desiccants (calcium sulfate, CaSO4 ). 4) Surrounding the plasma container with sufficient amount of dry ice. 5) Pack the DNA with sufficient amount of ice pack. Otherwise, dry down the DNA. 3. Shipping A. Shipping condition: 1) Blood cards: at room temperature. 2) Plasma: at -20oC. Samples should remain frozen at all time. 3) DNA: cold at ~ 4oC. Dry DNA pellets can be shipped at room temperature. 4) WBCs: at least under -20oC. Samples should remain frozen at all time. B. Shipping: 1) Include in the box the following documentation: a. Shipping information sheet b. Receiving confirmation sheet (with condition-on-arrival filled out) c. Special handling instruction d. Biohazard warning statement Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Mar 14, 2000 AD Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD 2) Make sure the following information will be included on the outside of the shipping box: a. Mailing address of recipient: b. Brightly colored self-adhesive warning label: DO NOT DELAY - BIOLOGICALS PACK IN________________(DRY ICE, ICE PACK) IMMEDIATELY ________________(FREEZE AT -70C) UPON ARRIVAL 3) For international packages: a. Use the warning label in the language of the recipient country b. Place shipper’s certifications in plastic envelops on the outside of the package c. The shipper’s certification letter will state clearly the shipping content and they are not restricted 4) All domestic shipments are sent via ___with a guaranteed second day delivery. 5) Log in the tracking number and monitor the progress of the shipment. Always ship the biospecimens of any subject in two batch! Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted Jan. 11, 1999 Revised Mar 14, 2000 AD Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD SPECIMENS DATABASE Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD Scheme for specimen ID Each sample is assigned a study ID number when the subject is recruited by the coordinating center. The study ID will appear only on the database but not on any label. All tubes and blood cards will have a barcode label with seven digits followed by one check digit for a total of eight digits. Each label will have the letters “CFR” to indicate the sample belongs to this study. The seven digit numbering system will begin with 0000001 and follow sequentially. Each label will have a different barcode number. The check digit is a calculated number that is a function of the other seven numbers of the barcode. The purpose of the check digit is to verify the correct barcode number is being typed during data entry. Additionally, each specimen will have more specific information about it built into a series of Access 97 database tables. The entire Access 97 database is called “CFR” and the following list details the 13 tables within this CFR database. (list) These tables will all be linked together by the study ID (or the barcode?). Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Dec 30, 2002 AD Blood cards Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Feb 13, 2004 AD A bar code will be given to every envelope of 2 blood cards. Plasma A bar code will be given to each tube. Buffy coat from EDTA blood A bar code will be given to each tube. WBCs from ACD blood A bar code will be given to each tube. Residual cells from both ACD and EDTA blood A bar code will be given to each tube. Paraffin-embedded-tissue slides A bar code will not be given. Paraffin-embedded-tissue section in the tube A bar code will be given to each tube. Frozen tissue ??? DNA A bar code will be given to each tube. RNA A bar code will be given to each tube. EBV cell lines ??? Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Sept. 9, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Scheme for location assignment of biospecimens Aliquots from each specimen will be split into two batches, which will be stored in two different freezers. This will ensure that one set of aliquots will be unharmed in case of a power failure. Blood cards Each card will have a location assignment such as 0001-01: 1. first 4 digits assigned for the subdivision, only file 10 cards per a subdivision, 2. next 2 digits identified the order where the card will be placed. Plasma Buffy coat from EDTA blood WBCs from ACD blood Residual cells from both ACD and EDTA blood Paraffin-embedded-tissue slides Each slide will have a location assignment such as 0001-01: 1. The first 4 digits are assigned for each individual block, it is also the subdivision number of the system. 2. The next 2 digits will identify the order where the slide will be placed in that subdivision. Frozen tissue DNA RNA EBV cell lines Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Sept. 9, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Guidelines for labeling specimens 1. make sure the blood tube labeling information corresponds to blood ticket provided by the USC coordinating center upon receiving. 2. use a permanent marker to label if a printout is not supplied. 3. paraffin-embedded slides should be labeled with Superfrost Marker as any other ink will be removed in the xylene. Slides should never have barcode labels on them. 4. pre-label all materials (tubes or slides) before working with the specimens. 5. place the 8 digit barcode on the side of the tube. 6. label the 7 digit alphanumeric code on the cap of the tube. 7. cryogenically approved labels should be used with ink that is stable under freezing condition. Thus, each specimen will require about 17 study ID printouts: 1 for blood log sheet 1 for the envelope of the blood cards 2 for blood cards 5 for QC assays 8 for DNA/RNA isolation/lymphoblastoid cell line setup Each specimen also will require about 36 barcode labels: 20 to 24 for plasma 3 to 5 for EDTA buffy coat 10 for Ficoll-separated WBC aliquots 1 for residual cells from both EDTA and ACD tubes Each specimen will require one 7 digit alphanumeric code label on the cap of each tube. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised _______________ Drafted October 10, 1998 Revised Feb 13, 2004 AD Biospecimen data records and report 1. Blood Log Sheet: The following will be written on a Blood Log Sheet before and during processing: a. study ID# b. name of center c. date drawn d. time drawn (PST) e. time of arrival (PST) f. date of arrival g. date processed h. total blood volume in milliliters of EDTA tubes and ACD tubes Vacutainer tubes contain the indicated amount of blood when filled 1/4” below the stopper. i. number of aliquots of plasma and lymphocytes j. processing end time (PST) Aliquots will be temporarily stored in a designated freezer location until a permanent location is assigned. Once the permanent location is entered into the database, the tubes will be moved. 2. Detailed report for each specimen 3. Inventory Samples will be tracked using a high density laser scanner for barcode labels (once we know, indicate the type). As previously stated, the CFR database in Access 97 will provide the lab with more specific information about each sample. The CFR database will be accessible to a limited number of staff, and will be stored on an computer in Room 5429 that is not on a network. A workgroup security system within Access 97 will be activated, allowing only specified individuals with the password to edit the database. These individuals are Anh Diep, Thanh Diep, and Owen Duffy. Immediately following each data entry session, the database will be saved to the designated computer, a backup ZIP disk that will be stored in the lab, and a backup ZIP disk that will be stored at an offsite location. This backup procedure is specifically for the lab’s recordkeeping, and is separate from the department’s usual archiving system. A periodical updates of the database to Darthmouth via the internet or electronic transfer. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised Sept. 9, 1999 AD Drafted October 10, 1998 Revised Feb 13, 2004 AD Biospecimen database tables Blood table Blood subtable Paraffin block table Paraffin Slides table Tissue table Buccal smear table DNA table RNA table Blood aliquot dispatch table Paraffin block dispatch table Paraffin slides dispatch table Tissue dispatch table DNA dispatch table RNA dispatch table Destination table Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised _______________ Drafted October 10, 1998 Revised Feb 13, 2004 AD QUALITY CONTROL Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD 1. Mix-up QC. To evaluate the quality of the biospecimen handling throughout the entire process by performing routine QC assays for randomly selected 10% of the specimens. As described in DNA preparation protocol, DNA typing using microsatellite analyses with high discriminating power allows us to compare the genotypes between aqueous DNA source and bloodstain DNA source or any others from the same individual. It is the PCR setup of less than 20 ng of DNA using D1S80 that is mapped at the distal of Chromosome 1 and has the discriminating power of 95-98%. PCR product of 350 bp-1 kb size will be electrophoresed on native agarose gel and then UV-visualize the genotypes. Samples that are certified for future research will be confirmed to have identical genotype patterns to that for other source of DNA from the same individual. Samples that are identified, as mix-up will be excluded or hold for further resolution. 2. DNA Preparation QC After every batch of DNA extraction, a series of assays are required to evaluate the quality of this long term preserved genetic materials: a. Determine DNA purity by taking its absorption spectra to obtain OD260/OD280 ratio. b. Determine DNA integrity by running undigested DNA on a 1% agarose gel with a standard of known concentration to observe for the intact band of DNA at high molecular weight and for the smear at low molecular weight, which is the sign of the degradation. c. Optional to determine DNA digestibility with Hind III or Ecor I to ensure the absence of trace organic solvents, salts, cellular proteins and proteinase K in the final DNA solution, assuming that above a. and b. performance will be sufficient to certify the DNA quality for long term storage. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised _______________ Drafted October 10, 1998 Revised Feb 13, 2004 AD Summary of Routine QC for all specimens (Adapted from BCSCFR) Every six months, chose 5 individuals at random to test: 1) Cell lines - transform 5 cases recover freezes from last 5 cases to test for re-growth, and to compare genotypes vs. DNA made last time, and then refreeze EBV cell line will be provided by Coriell and each lab will perform PCR tests for mycoplasma contamination and Hoechst staining if possible - likely to be done in BNE at first 2) DNA 3) RNA] - isolate DNA from BP freeze from the same 5 test cases and matching Guthrie spots (if not already done for other purposes) and from LCL to check: OD 260/280 Agarose gel Cut + uncut (high and low salt) Eco RI: Hind III PCR [4 STRs and Y- chromosome PCR] isolate RNA from the same 5 test cases from WBC freeze (if not already done) and check: OD 260/280 or Orcinol Agarose gel (1.2%) RT-PCR using AS promers (~ 1 kb) and PGK primers (247 bp) Once a year, send DNA, RNA to another group to test. At six month intervals: . . . . Transform one aliquot of frozen white blood cells from 5 individual Prepare DNA from whole blood from 5 individuals Prepare DNA from blood spots from the same 5 individuals Prepare RNA from one aliquot of frozen white blood cells from 5 individuals Lymphoblastoid Cell Line: . Viability . Myoplasma contamination (PCR)1 DNA from whole blood: . OD260/OD280 . Agarose gel electrophoresis . Restriction digest with EcoRI and HindIII . Microsatellite analysis with two markers; D10S526 and D22S4172 . Gender analysis if there is a problem Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised _______________ Drafted October 10, 1998 Revised Feb 13, 2004 AD DNA from Blood Spots: . Microsatellite analysis with two markers; D10S526 and D22S4172 . Confirm that this pattern is identical to that for DNA from whole blood from the same individual. DNA from whole blood: . OD260/OD280 or Orcinol . Agarose gel (1- 2%) electrophoresis . RT-PCR using 2 sets of primers: p53 (1248 bp), PGK (247 bp)3 See Detailed Protocol Section from Philadelphia See addendum to Minutes of February 25, 1997 for sequences and PCR conditions See addendum to Minutes of January 27, 1997 for sequences and PCR conditions Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised _______________ Drafted October 10, 1998 Revised Feb 13, 2004 AD General protocol for QC and QA Sample processing 1. Adopt a barcode system to ensure tight specimen control and handling. 2. General laboratory biosafety and contamination control protocols have to be followed (sterilization, for DNA/RNA/cell line, etc) 3. Ensure specimen viability (cells and cell lines ) by routine QC test. 4. Ensure specimen integrity by routine QC test and inter-center exchange plan. During experiment 1. Again, strict laboratory contamination control has to be followed (sterilization, for DNA/RNA/cell line, etc) See lab setup protocol for details regarding biosafety, PCR, creating a ribonuclease-free environment, etc. 2. All assays will include a “positive” control and a “negative” control. 3. For high volume experiments, no consecutive samples should be run by the same technician. 4. If the study provides high yield specimens and has sufficient funding, all samples should be run in duplicate. 5. If discrepancies are found from QC test, repeat experiments will be run by a different lab technician in a blind manner. 6. If discrepancies are found from QC test, we can even have the collaborator repeat the experiment in a blind manner. 7. Repeat experiments will be performed for all “positives” detected in a study when “positives” (mutants) are rare. 8. Randomly pick from original materials to repeat some “positives” detected when the “positives” rate is high. 9. All repeat QC test will work from redrawn blood, or QC source (blood spots), or stock DNA in a blind manner (instead of previous amplified PCR products). Data analysis 1. Data will be scored by multiple readers. 2. Each reader will independently score the data in a blind manner. Data entry 1. 2. 3. Records will be scored into database independently. A second reader also will confirm the score independently. Have strict editing protection by: limited access of lab staff to database ( password permission ). have a record of date and time editing monitored by computer software. Colorectal Cancer Family Registry - Coordinating Center Laboratory University of Southern California, Department of Preventive Medicine Drafted October 10, 1998 Revised _______________ Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD Date:__________Int’ :____equipment used: DNA Extraction Worksheet From Buffy Coat DNA quantitation by spectrophotometer Record of sample ID, A260, A280 and A260/A280 from 1 ul of DNA solution. Calculate DNA concentration in ng/ul. (OD260*dilution factor*coefficient for DNA where dilution factor is 100, and the coefficient for DNA is 50. ) Calculate total DNA yield and record working dilution preparation. Tape on this the OD reading printouts*. Highlight samples that have A260/A280 not in 1.8 -2.0 range. (These samples are to be re-extracted again.) Comments: __________________________________________________________________________________________ Colorectal Cancer Family Registry - Coordinating Center Laboratory Uni versity of Southern California, Department of Preventive Medicine Drafted Feb. 8, 1999 Revised Feb 11, 1999 AD Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD DNA Extraction Worksheet From Buffy Coat Date:__________Int’:___ Examine DNA integrity and digestibility by gel electrophoresis Make sure digestion sample list is correspond to extraction sample list. # of samples Reaction setup 1x, ul DNA 50 ul ddH2O 3.5 ul 10x buffer 6 ul [DNA] 4 ng/ul Enzyme 0.5 ul DNA amount, ul 200 ng, 50 ul Total digestion volume 60 ul Enzyme Hind III from Gibco BRL Boost digestion (if need) [enzyme] 10 u/ ul ddH2O Enzyme amount, ul 1-5 u, 0.5 ul 10x buffer buffer system REact 2 50 mM Tris-HCl, pH 8.0 10 mM MgCl2 50 mM NaCl Additional digestion V Incubation T and duration 37C, 4 hrs ____x, ul Enzyme Gel loading prep digestion mixture 18 ul 10x loading buffer 2 ul Total loading volume 20 ul Run cut and uncut DNA* with a standard of known concentration. Highlight to repeat digestion of any samples that were either undigestible with restriction enzymes or samples that are severely degraded. * Make sure gel running sample list is correspond to extraction sample list. Apparatus model horizotal Gel kind Agarose Gel % 1% Photo of gel Gel size Gel Component g/ml buffer Comb size Well capacity 20-25 ul Buffer 0.6 x TBE Direct Current Time : to : Notes: Comments: __________________________________________________________________________________________ Colorectal Cancer Family Registry - Coordinating Center Laboratory Uni versity of Southern California, Department of Preventive Medicine Drafted Feb. 8, 1999 Revised Feb 11, 1999 AD Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD DNA Extraction Worksheet From Buffy Coat Date:__________Int’’: DNA Typing by VNTR analyses * Make sure typing sample list is correspond to extraction sample list. Marker Information VNTR Order PCR setup [stock] [final] 1x, ul 1 ddH2O — — 7.4 ul 16-bp repeat unit Locus D1S80 2 10x buffer — 1x 2 ul Chromosomal localization 1p distal 3 dNTPs 2.5 mM 0.25 mM 2 ul Allele size range 350 bp-1 kb 4 Primer 1 2 uM 4 pmol 2 ul Heterozygosity 90% in Caucasians 5 Primer 2 2 uM 4 pmol 2 ul Allelic frequency 29 alleles identified 435 possible genotypes 6 DNA polymerase 5 u/ ul 2u 0.4 ul Discrimination power 95-98% Primer code 7 XB20, XC01 8 AmplFLP D1S80 Allelic Ladder PERKIN ELMER N808-0064 27 amplified alleles MgCl2 25 mM 1.5 mM 1.2 ul Total Master Mix — — 17 ul Template 10 ng/ ul 30 ng Final volume ____x, ul 3 ul 20 ul allele #14, 16-41 PCR Profile: 1 cycle @ 94C for 4 min. 35 cycle of 94C denaturation for 1 min, 65C annealing for 1 min and 72C elongation for 8 min. 1 final cycle of 72C elongation for 5 min. Hold @ 4C for further steps. AmplFLP D1S80 Allelic Ladder, lab code Run PCR product with AmplFLP D1S80 Allelic Ladder. * Make sure gel running sample list is correspond to extraction sample list. Apparatus model horizontal Gel kind Agarose Gel % 1.5% Photo of gel Gel size Gel Component g/ml buffer Comb size Well capacity 20-25 ul Buffer 0.6x TBE Loading buffer ficoll dye Loading volume 22.5 ul Direct Current Time : to : Notes: Load mixture of 5 ul /lane Allelic Ladder + 2.5 10x dye = 22.5 ul + 15 ddH2 O Load 20 ul (-) = 22.5 ul (-) PCR control PCR cont. Comments: __________________________________________________________________________________________ Haile’s Genetic Epidemiology Laboratory Uni versity of Southern California, Department of Preventive Medicine Drafted Feb. 8, 1999 Revised Jun 21, 2001 AD Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD Mix-Up Quality Control for DNA Blood spot or other DNA source Buffy coat extract DNA Is OD 260/280 ratio between 1.7-1.9? No perform purification Is undigested DNA giving intact band by agarose gel electrophoresis? Yes No extract DNA from another aliquot or from other source Is undigested DNA giving intact band by agarose gel electrophoresis? No extract DNA No Yes Perform microsatellite analyses Certify for CFR Repository Is OD 260/280 ratio between 1.7-1.9? Yes Perform microsatellite analyses Is it feasible to obtain PCR product? Is microsatellite pattern identical with other DNA source? No Ship DNA as instructed Request Submission Colorectal Cancer Family Registry - Coordinating Center Laboratory Drafted October 10, 1998 University of Southern California, Department of Preventive Medicine Revised Feb 13, 2004 AD