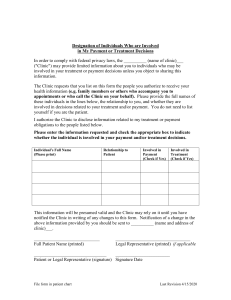
Guidelines for Medical Clinics
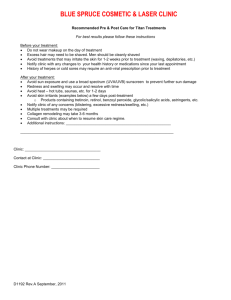
advertisement

Iowa Department of Public Health Mary Mincer Hansen, R.N., Ph.D. Director Patricia Quinlisk, M.D. Medical Director/Epidemiologist Division of Acute Disease Prevention & Emergency Response Mary J. Jones, BSEMS, PS, Division Director Attachment 12: Guidelines for Management of Surge Capacity in Medical Clinics May 2006 Medical Facilities Point of Contact: JohnMarch Carter, RN, 2006 P.S., MPA Hospital Bioterrorism Coordinator Center for Disaster Operations and Response 321 E. 12th Street Lucas State Office Building, 5th floor Des Moines, IA 50319-0075 515-242-5096 (phone) 515-281-0488 (fax) www.idph.state.ia.us Iowa Department of Public Health Center for Disaster Operations & Response Table of Contents Section Overview of Emergency Response Introduction I. Pre-planning issues A. Emergency Response Plan B. Scope of Planning Process C. External Planning Considerations D. Surge Demand Plan II. Incident Command Structure A. Identification of Command Staff B. Emergency Operations Center Policy C. Communications within Command Structure D. Communications with Response Partners Page 3 5 5 6 6 6 8 10 10 10 III. Clinic Operations A. Patient Flow Plan B. Notification Policies C. Rapid Triage Plan D. Disease Reporting E. Infection Control 11 11 11 11 12 IV. Staffing A. Evaluate Workload B. Policy Considerations C. Use of Volunteers D. Staffing Support Strategies E. Communication with Staff F. Mental Health Issues 13 13 13 13 14 14 V. Clinic Environmental Operations A. Security B. Laundry/Linen C. Housekeeping/Custodial Services D. Water/Sanitation E. Parking F. Visitor/Guest Management 14 14 14 15 15 15 Iowa Department of Public Health Center for Disaster Operations & Response VI. Supplies and equipment A. Supply Inventory System B. Assessment of Medical Supply Inventory C. List of Vendor for Commonly Needed Items D. Assessment of Pharmaceutical Inventory E. Assessment of Biomedical Equipment Inventory F. Access to Non-Traditional Sources for Inventory Assistance G. Assessment of Laboratory Inventory VII. Special Considerations A. Fiscal Issues B. Patient Care Documentation and Tracking 16 17 17 17 17 17 17 18 18 Appendices A. Patient Evacuation Plan Template B. Sample Incident Command Organizational Chart C. Sample Job Action Sheets D. Clinic Self-Assessment Worksheet E. Sample Exercise Scenarios, After-Action Report, and Improvement Plan F. Additional Resources Iowa Department of Public Health Center for Disaster Operations & Response Overview of Emergency Response The State of Iowa has adopted a multi-hazard approach to managing the consequences of emergency/disaster response. Underlying this approach is the principle that a standard set of generic functional capabilities can be employed to effectively address a wide variety of hazardous conditions and categories of incidents, whether these have a known probability of occurring or are totally unforeseen. The Code of Iowa, Chapter 29C establishes the Iowa Homeland Security and Emergency Management Division as a Division within the Department of Public Defense and provides for the appointment of an administrator. The Division's mission is to support, coordinate, and maintain state and local homeland security and emergency management activities to establish sustainable communities and assure economic opportunities for Iowa and its citizens. The Division is tasked with administering the Iowa Emergency Response Plan. The plan is composed of Basic Plan, which provides a broad operational blueprint of the State of Iowa’s approach to an emergency/disaster response. The scope of this Plan section is state-government-wide, versus a focus on the operations associated with a specific agency, function, hazard, or incident type. The intended audience is the set of state government executive decision-makers. The plan also contains a group of functional Annexes, which focus on information needed to carry out a specific function, such as public information or resource management. The intended audience is the set of agencies or other entities that provide a primary or supporting role in carrying out the function. Annexes are directly attached to the Basic Plan. The Iowa Dept. of Public Health is the Lead Agency for four annexes: Radiological Emergencies Public Health Medical Services Mass Fatalities It is a support agency for eight annexes: Research, Analysis and Planning Public Information Sheltering Human Services / Disaster Mental Health Hazardous Materials Search and Rescue Terrorism Incident Response Infectious Animal Disease Disasters Iowa Department of Public Health Center for Disaster Operations & Response The Iowa Dept. of Public Health will carry out its mission by implementing the State of Iowa Bio-emergency Response Plan. The plan is divided into four main sections. The first contains introductory information, the second contains the Iowa Department of Public Health’s bio-emergency response objectives and associated information, the third contains supporting information in the form of several attachments, and the fourth contains information that applies specifically to selected diseases. The Iowa Dept. of Public Health has developed guidelines and templates that will assist local planning efforts. These documents are not intended to provide all information, but rather to serve as a starting point for those facilities who are in the process of writing or upgrading plans or policies. These guidelines and templates include: Guidelines for Management of Surge Capacity in Hospitals Guidelines for Management of Surge Capacity in Medical Clinics Guidelines and Templates for Off-Site Medical Facilities Iowa Department of Public Health Center for Disaster Operations & Response Introduction There is a general consensus that a collaborative and sustainable process is needed to develop, maintain and systematically evaluate a clinic’s disaster and emergency preparedness response. Implicit in this process is the understanding that an ‘emergency’ is to be considered a natural or manmade event that significantly disrupts the environment of care (e.g., damage to physical structure); that significantly disrupts care, treatment and services (e.g., loss of power, water or telephone due to weather); or, circumstances within the clinic or in its community that results in sudden, significant changes or increased demands for the clinic’s services (e.g., pandemic, terrorist attack, building collapse, airplane/train crash). With an established and functional planning process in place, there is strong evidence that clinics and the communities they serve will be able to craft a variety of response plans to meet the anticipated multitude of risks and hazards. This document is designed to provide clinics with information to assist them in creating a disaster plan. It is very important that once a plan is created, exercises should be held to determine if changes are needed. Sample exercise scenarios can be found in Appendix E. I. Pre-planning issues A. Emergency Response Plan 1. Devise an organizational structure that gives planning and oversight of the clinic’s disaster and emergency preparedness response. Include the following areas: a. Clinic Administration b. Medical Staff c. Nursing Staff d. Pharmacy (if applicable) e. Laboratory (if applicable) f. Radiology (if applicable) g. Finance Staff 2. Other considerations: The size of the clinic will likely dictate some aspects of the selection process. Where/when available, key personnel in areas of medical records administration, information systems, telecommunications, and EMS/medical transportation are a source of key advice and counsel. 3. The selected work group should be given a ‘mission statement’ that establishes a clear framework within which to function. Key components of group’s job description should include the following: a. Statement of Purpose b. List of Members c. Meeting Frequency d. Reporting Lines e. Responsibilities f. Tasks Iowa Department of Public Health Center for Disaster Operations & Response g. Relationships h. Accountabilities B. Scope of Planning Process 1. Disaster and emergency preparedness requires a thorough examination of five distinct phases of assessment and analysis. The phases are: a. Mitigation Phase: Those activities that a clinic undertakes to lessen the severity and impact of a potential emergency. b. Preparedness Phase: Those activities that a clinic undertakes to build capacity and the identification of resources, both internal and external, that may be needed if an emergency incident occurs. c. Response Phase: Those policies, procedures and protocols that will be implemented under certain identified conditions and circumstances. d. Recovery Phase: Those activities that a clinic undertakes to bring operations to a stable and reliable level of performance during and after an emergency incident has occurred. e. Evaluation and Improvement Phase: Like all planning processes, disaster and emergency preparedness planning demands an ongoing effort to measure performance and implement improvements as may be necessary to meet established performance objectives. C. External Planning Considerations 1. Collaborate and plan with a variety of community, civic, governmental and private organizations. 2. Be familiar with the County’s All-Hazards Response Plan and the health and medical component presented in Annex G of the plan, which is developed by hospital, local public health, community clinics, mental health resources, and EMS. 3. Assure that hospitals and clinics collaborate regarding transportation and referral plans. It is imperative that clinics maintain communication with the hospitals in their community to assure that all parties understand how patients will be referred, what advice they will be given during telephone triage, and how patients will be directed to the hospital if appropriate. D. Surge Demand Plan 1. Each clinic will have its own unique issues and circumstances, but there are a number of common characteristics and considerations that should be addressed in preparation of a clinic’s surge demand plan: a. Establish a defined incident management structure within the clinic and ensure that it is fully integrated with adjunct community and regional incident management structures. Become competent with the Incident Command System (ICS). Use common nomenclature. Iowa Department of Public Health Center for Disaster Operations & Response b. Key staff members should be assigned Incident Command System positions and trained to function with an incident management structure. Clinics should design their incident management structure around the operating scope and talent of the institution. Training is necessary to achieve a level of familiarity that will be necessary to have an effective execution of incident management system. c. Reaffirm the Clinic’s participation in a community or regional planning process. Ensure this process includes active participation from a broad representation of the county’s health, medical agencies and organizations. d. Review the assumptions and components of the clinic’s supply chain management process to better prepare for the challenges and obstacles that may develop during a medical surge event. Recognized that the just-in-time economic environment has reduced supply inventories. Expanding procurement contracts to increase the number of vendor suppliers may be beneficial. Another option is to develop sharing/exchange agreements with neighboring clinics and/or hospitals within a host network. Procurement of drugs, medical gas and blood products may be challenging during an event. These specialized commodities require forethought and analysis to identify and capture new channels of supply and distribution. e. Review host health network expectations to insure that assumptions on patient referrals, transfers and admissions are consistent with corporate goals. f. Review the procedures/protocols that have been devised by the clinic’s county for activating the county’s Emergency Operations Center (EOC). The use of Emergency Operations Center-type communication structures is integral to the National Preparedness Plan and state, regional and local response plans. It is important that the county’s Annex G clearly delineate the health and medical component of the county’s Emergency Operations Center. g. Review patient transportation plans and assumptions with the expectation that normal and routine sources may not be available in a timely fashion. Moving a large number of patients may require a partnership between clinics, hospitals, EMS providers and others in order to effectively stay ahead of the surge capacity curve. Iowa Department of Public Health Center for Disaster Operations & Response It may be necessary to cohort border-line litter patients and transport them by unconventional means such as by buses, thereby allowing staff to be used more productively. Determination of which organization will take the lead in expanding transportation resources and how staffing will be achieved are best addressed as part of a collaborative pre-event planning process. h. Identify strategies and tactics that will enable the clinic to meet its service delivery expectations with a minimum impact on the clinic’s standard of care. Under what many may call ‘battlefield conditions’ as the apex of a surge event approaches, there will be an inescapable shift to doing the greatest good for the greatest number. Implicit are the process of triage and the resulting allocation of scarce resources. Create mutual assistance pacts and inter-institutional agreements when possible. II. Incident Command Structure A. Identify a command staff. It is recommended that each command staff position have at least two to three personnel trained and familiar with the function of the assigned position. Some personnel may have to become familiar with more than one ICS position. With limited staff, one person may assume the duties of multiple positions. Job action sheets should be available for all of the following positions: 1. Incident Commander. a. Gives overall direction for the direction/mitigation of incidents. b. One person should be dedicated to this role. c. Recommended for clinic administrator or management personnel most familiar with total system/facility operations. (Chief Executive Officer, Chief Operating Officer, Chief Financial Officer) 2. Public Information Officer. a. Provides information to the news media. b. Person should be skilled at dealing with public and or have experience in Public relations. 3. Liaison Officer. a. Functions as incident contact person for representatives from other agencies. b. Since supplies and transportation will be the most pressing need, consider using the materials manager in this role. 4. Safety and Security Officer. a. Monitors and has authority over the safety of rescue operations and hazardous conditions. b. Organizes and enforces scene/facility protection and traffic security. Iowa Department of Public Health Center for Disaster Operations & Response c. Consider the facilities or infection control coordinator for this role. 5. Logistics Chief. a. Organizes and directs those operations associated with maintenance of the physical environment, and adequate levels of food, shelter and supplies to support the medical objectives. b. The person most suited for this position should have an intimate knowledge of supplies and available resources (Materials Manager, Purchasing Specialist) 6. Planning Chief a. Organizes and directs all aspects of planning section. b. Ensures the distribution of critical information/data. c. Compiles scenario/resource projections from all section chiefs and effects long range planning. d. Documents and distributes facility Action Plan. e. Consider using a clinical person, such as the Director of Nursing, in this role since planning will require knowledge of the disease process and be able to project resource needs and consumption rates of supplies. 7. Finance Chief a. Monitors the utilization of financial assets. b. Oversees the acquisition of supplies and services necessary to carry out the clinic’s medical mission. c. Supervises the documentation of expenditures relevant to the emergency incident. d. Consider using Chief Financial Officer or budget management personnel (Account’s Payable/Receivable section). e. Person should have authority to purchase emergency supplies or authorize expenditures as needed. 8. Operations Chief a. Organizes and directs aspects relating to the Operations Section. b. Carries out directives of the Incident Commander. c. One person should be dedicated to this role. This person should be very familiar with total system/facility operations. (Chief Executive Officer, Chief Operations Officer, Chief Financial Officer) 9. Medical Officer a. Organizes, prioritizes, and assigns physicians to areas where medical care is being delivered. b. Advises the Incident commander on issues related to the Medical Staff. c. Organizes and directs the overall delivery of medical care in all areas of the clinic. d. This position is usually an MD/DO; however, a PA or ANP may fill the role. 10. Other incident command positions Iowa Department of Public Health Center for Disaster Operations & Response a. Develop a clearly understandable process to fill the other positions in the Incident Command System as necessary. B. Emergency Operations Center Policy (activation, staffing, location, supplies/equipment) 1. Primary and secondary locations should be selected well in advance and identified within the clinic’s emergency plan. 2. Location selection should focus on a space large enough to accommodate command staff with some consideration given to “overflow” which includes outside agencies and additional appropriate positions as determined by ICS organizational chart. 3. Emergency Operations Center Policy should make clear who can authorize activation of Emergency Operations Center and notification list of personnel to contact (and by what methodology) when activation is initiated. 4. Appropriate supplies should be located within Emergency Operations Center (or in close proximity and easily transported). Supplies should include at least the following: A. Incident Command System vests B. Job Action sheets C. Writing material D. Communication devices (Radios, telephones, etc.) E. State, Regional and Local maps; blueprints of facilities, etc. F. Computers, Television and other AV equipment G. White boards, bulletin board, flip charts or other visual aids. This list is provided only as a guide to assist in the set-up of an Emergency Operations Center and not intended to act as a total needs list. Each Emergency Operations Center will have these common components, but some may need additional supplies and/or equipment based on location and specific facility. C. Communications with command structure (e.g. portable radios). 1. Consider that phone service (including cellular phones) may be disrupted during a large scale event. 2. Devise solutions that can be easily implemented and simple to use (for example, two-way family radios). 3. Communication devices should have a written operations/ directions page for those employees not accustom to their use (a “how-to” guide). 4. A policy on use (when, where, and how) should be developed and consideration should be made for necessary preventative maintenance and routine checks for operational readiness. D. Communication with response partners (e.g. Emergency Operations Center interface). 1. Policy should be developed on communicating with County Emergency Operations Center personnel or Joint Information Center Iowa Department of Public Health Center for Disaster Operations & Response (JIC). This written guide should include who is authorized (usually Public Information Officer, Liaison, or Incident Commander) and by what methodology (Radio, telephone. FAX or other means). 2. Contact lists for County Emergency Operations Center personnel should be kept current as needed. 3. Maintain current information from Iowa Dept. of Public Health website (www.idph.state.ia.us) III. Clinic Operations A. Patient flow plan 1. Clinics should have a plan that clearly shows the ingress and egress of patients during a disaster. 2. Since patient throughput will be an issue during a disaster, consideration should be given to how this process will be expedited. This could include delaying diagnostic tests for patients, or suspending the use of “phone-in” prescriptions to pharmacies. 3. Work with home healthcare agencies to arrange at-home follow-up care for patients who may require it. 4. Allow family members to stay with children, if possible. Consider evaluating adults and their children in the same room, if possible. B. Notification policies 1. The plan should include a description of how staff will be notified of the disaster. This includes addressing such issues as when staff will be recalled, notification systems, and phone trees. C. Rapid triage plan 1. Consider creating an alternative triage system when a large number of patients are presenting. This includes both trauma and medical patients. 2. Consider setting up a “telephone triage” system, which patients could call for information. 3. Consider assigning a “triage coordinator” to manage patient flow, including deferring or referring patients who do not require immediate care. D. Disease reporting 1. The plan should outline how disease will be reported to both local and state public health departments. 2. If revised surveillance techniques will be used (for example, daily reporting of Influenza like Illnesses), this should be included in the plan. Iowa Department of Public Health Center for Disaster Operations & Response E. Infection Control 1. CDC Guidelines for isolation including using standard precautions on all patients and droplet, contact and airborne precautions should be utilized when indicated in health care settings. 2. Within health care settings, respiratory hygiene and cough etiquette guidelines should be developed. 3. All health care workers are expected to provide care for patients with known or suspected infectious diseases, as well as comply with personal protection equipment, infection control and public health recommendations. 4. Decisions regarding the need for escalating infection control measures will be based on disease activity and transmission risks. 5. When available, adequate personal protection equipment supplies and equipment will be determined and maintained. 6. Educational materials related to use of personal protection equipment and supplies will be developed. 7. During a pandemic of any size, all infection control professionals will need to formally monitor and reinforce compliance with personal protective equipment measures and policies. 8. Infection control professionals will not only implement appropriate infection control measures, but will also cease ineffective practices. 9. Staff members may be designated to assist infection control professionals during outbreaks (e.g. staff may be placed in patient care areas to assist with proper use of personal protective equipment). 10. Visual alerts will recommend respiratory hygiene precautions. 11. Masks should be available for patients prior to them entering the Emergency Department/outpatient facilities. 12. Patient movement. a. Movement and transport of patients with infectious diseases should be limited as much as possible. If a patient must be transported, adhere to the following guidelines: Place surgical mask on patient. Always notify recipient area prior to patient transport. Follow a pre-designated alternate route designated for transport of patients with infectious diseases (separate from main traffic route). Visitors should be limited to reduce the likelihood of infectious disease transmission among patients, and health care workers. 13. Surveillance a. The clinic should have mechanisms in place to: Conduct surveillance to detect and increases in patients being seen that may indicate the presence of specific diseases. Monitor employee absenteeism for increases that might indicate early cases of specific diseases. Iowa Department of Public Health Center for Disaster Operations & Response IV. Develop assessment guidelines for staff that may be showing signs or symptoms of disease. Staffing A. Evaluate Workload 1. Determine what adjustments can be made for patient acuity 2. Determine what patients can be placed together 3. Determine which of your services can be downsized or shut down and those personnel reassigned. 4. Determine process to transition non-clinical workers into assuming clinical duties. B. Policy Considerations 1. Agency support a. Maintain written agreements. b. Staffing pools 2. Consider restricting vacation policies. 3. Consider using nursing students as assistive personnel. 4. Consider reassigning Quality Management and Risk Management nurses to clinical areas. 5. Maintain staff skills in infection control. 6. Plan to protect high risk staff from complications of the disease. C. Use of Volunteers 1. Credentialing. a. Consider how outside staff will be credentialed and used. b. Consider where this staff will present for duty, and how they will be identified (badges, etc.). c. Pre-designate areas where volunteer staff will be given assignments. 2. Training a. Predetermine what training will be needed for outside volunteers. b. Consider designing just-in-time training tools for volunteers. D. Staffing support strategies 1. Consider flexible and staggered staffing as needs arise. 2. If a large number of clinic staff do not live in the immediate area, consider written agreements with local motels to assist with sleeping arrangements for staff. 3. Consider in-clinic dependant adult and child care arrangements for staff family. 4. Consider written agreements with local veterinarians for pet care. 5. Consider using staff from affiliated clinics and/or hospitals if available. 6. Consider providing transportation for staff if needed. Iowa Department of Public Health Center for Disaster Operations & Response 7. Assign staff recovering from the applicable disease to care for patients affected by that disease. V. E. Communicate with staff 1. Ensure that your staff has a family preparedness plan. 2. Provide staff with regular situational updates. 3. Recognize that a reduced standard of care may induce staff concerns. 4. Assure that adequate rest periods for staff are addressed. F. Mental Health Issues 1. Recognize that the mental health issues related to a disaster may require additional assistance for patients and staff, such as social workers and clergy. 2. Recognize that Critical Incident Stress Debriefings may be needed. 3. Consider using Child Life Specialists or staff that are trained in comforting and educating pediatric patients during procedures. Clinic Environmental Operations A. Security 1. Consider how the clinic will perform security duties, such as lockdowns and monitoring doors. 2. Consider the challenges of large crowds waiting in line for services and the dynamics that can arise with these people. 3. Ensure that Security Staff has communication with the Incident Command Center. 4. Ensure that all clinic staff knows how to contact the next level of responsibility when needed (radio channel and staff title, telephone number, etc). B. Laundry/Linen 1. Consider establishing agreements with local laundries or related businesses that can provide pick-up and delivery to supplement your clinic’s laundry service. 2. Consider increasing your clinic’s current inventory of linens to be stocked to provide the necessary early response to a surge event. C. Housekeeping/Custodial Services 1. Consider: a. List the main areas to be serviced on a regular basis. Recognize that the demands may be more than one person can keep up with initially. b. Establish agreements with local vendors to purchase bulk supplies quickly as needed, such as cleaners, disinfectants, paper towels, brooms/mops, buckets, etc. c. Consider accumulating additional supplies to build up your inventory without significantly affecting the budget. This will Iowa Department of Public Health Center for Disaster Operations & Response allow you to keep up with the increased cleaning needs, deplete your supplies more slowly, and provide more lead time in procuring additional supplies when needed. d. Consider establishing written agreements with local cleaning agencies (SercviceMaster, AmeriClean, etc) for emergencies. D. Water/Sanitation 1. If there is an interruption to the clinic or community water supply system: a. Consider the possible duration of the interruption and the need to provide portable temporary toilets (remember to provide handicapped accessible units as well). Also, predetermine the best location of these units to coordinate with patient and staff access as well as the need for daily servicing. b. Determine which services in your clinic require water (radiology, lab, laundry, etc), and determine which of these could be scaled back to conserve water in the event of an outage. E. Parking 1. On a site map of your Clinic/Campus a. Pre-plan where clinic staff will park to avoid congestion/conflicts with patient/visitor parking. b. Coordinate the flow of staff/patients/visitors to avoid congestion and conflict- remember the need for emergency vehicle access (police, ambulances, fire, etc) c. Consider the possible need to secure your staff’s parking area so it remains available for rotating shifts and will not be used by patients/visitors/guest. d. Pre-plan for the increased parking needs of patients. Consider using neighboring businesses, open lots, etc. (consider the need for potential snow removal). e. Provide signage at points of entry directing patients and visitors to the designated areas. f. Consider using Volunteers to assist with parking- Possibly Boy Scouts, Kiwanis, Rotary Clubs, etc. g. Plan for extended usage of flashlights and other lighting mechanisms. F. Visitor/Guest Management 1. Establish one point for entry, registration and exit for visitors and guests. 2. Consider a sign-in and sign-out log including passes or badges for visitors and guests to better know who is in the clinic at any given time. Passes and/or badges should be returned – this is more easily monitored if there is one point of entrance and exit. With an Iowa Department of Public Health Center for Disaster Operations & Response appropriate checklist of duties, volunteers with minimal orientation or training required in an emergency could staff this position. 3. Pre-determine who will be allowed to visit patients—consider only the immediate family during a surge event to keep the number of extra people in the clinic to a minimum. 4. Ensure that staff is aware of the visitor and guest policies, including passes and/or badges, so they can assist in monitoring people in the clinic. Have a plan for assisting non-registered visitors and guests back to the registration area. 5. Consider written guidelines to be handed out to the visitors and guests after they register. Identify language-specific and reading-level appropriate materials for patients, family members and visitors. 6. Train Intake and Registration staff to detect patients with disease signs and symptoms and to implement immediate measures to prevent transmission. 7. Post signs for respiratory hygiene/cough etiquette- provide needed supplies to enforce these protocols (mask, tissues, frequent waste basket changes, etc.). 8. Create a plan for getting translators when needed. 9. Consider assigning separate waiting areas for persons with respiratory symptoms. 10. Consider the limited mobility issues of non-ambulatory, elderly, and special needs patients. 11. Consider the special needs of patients who may be pregnant, post organ transplant patients, and renal dialysis patients. VI. Supplies and Equipment A. Supply Inventory System. 1. These procedures must include review of daily material usage to determine if increased demand warrants the activation of surge plans. Special tracking of pre-identified supplies will give a clear and advanced reading of changing situations. 2. Evaluating the existing system for tracking available medical supplies in the clinic to determine whether it can detect rapid consumption, including items that provide personal protection (i.e., gloves, masks). 3. Improve the system as needed to respond to growing demands for resources during an influx of patients. 4. Utilize planning software to apply numbers to your assumptions. Iowa Department of Public Health Center for Disaster Operations & Response B. Assessment of medical supply inventory level/duration and order ship time. 1. Anticipate that several clinics and hospitals will identify the change in demand and request the same supplies from the same vendors at the same time. 2. Assess anticipated needs for consumable and durable resources and determine a trigger point for ordering extra resources. Examples include: hand hygiene supplies (antimicrobial soap and alcohol-based, waterless hand hygiene products), disposable N95 surgical and procedural masks, face shields, gowns, gloves, facial tissues, central line kits, morgue packs, batteries, etc. C. List of vendors for commonly needed items. 1. Update a list of primary and backup suppliers. 2. Determine their ability to support your needs. 3. Maintain written agreements. D. Assessment of pharmaceutical inventory levels/duration and order ship time. 1. Establish contingency plans for situations in which primary sources of medical supplies become limited. E. Assessment of biomedical equipment inventory level/duration and order ship time. 1. Stockpiling of equipment is very costly. Review of clinic’s capability and capacity is tantamount to the development of a supportive plan. 2. Cooperative community planning with neighboring clinics will enhance your plan. 3. Estimate the need for respiratory care equipment. 4. Develop a strategy for acquiring additional equipment if needed. 5. Clinics might consider developing inventories of equipment with neighboring clinics or affiliates, and determining whether and how that equipment might be shared during times of need. F. Access to non-traditional sources for inventory assistance 1. Assure that mechanisms are in place to obtain assistance from other clinics or hospitals in your network. G. Assessment of laboratory inventory levels/duration and order ship time 1. Assure that your laboratory is included in supply decisions Iowa Department of Public Health Center for Disaster Operations & Response VII. Special Considerations A. Fiscal Issues to Consider and Plan for: 1. Incremental expenses related to the event. a. Payroll / salary increases. Overtime expenses. Additional staffing, i.e.; temp staff. Ensure that all financial transactions are documented in case Federal reimbursement should become available. b. Increased supply purchases. Balances on supplies used during the event may come due when the event is over and when the revenues (income) from interrupted operations are diminished. Stockpiling supplies prior to an event is discouraged without a robust plan to rotate stock to avoid obsolescence or outdates. 2. Cash flow demands. a. Decreased revenue from decrease of elective procedures. Consider business interruption insurance for departments, clinic, or staff (physicians) who may experience a significant loss of income due to interruptions of routine operations. 3. Coding and billing considerations. a. Maintain contact with appropriate federal agencies to determine changes in coding that may be necessary. For example, the following website contains information related to Hurricane Katrina: http://www.cms.hhs.gov/Emergency/02_Hurricanes.asp B. Patient Care Documentation and Tracking 1. Use familiar systems to avoid loss in efficiency. 2. Consider/identify minimum acceptable standards for medical documentation and physician dictation. 3. Ensure that reliable and redundant systems are in place to accurately track, account for, and report on incident victims. Iowa Department of Public Health Center for Disaster Operations & Response Appendix A: Patient Evacuation This form addresses the relocation of patients, staff and visitors and/or facility to other designated areas. (This form can be modified to meet the evacuation criteria for your clinic) 1. In case of emergency, contact: <Insert Name> at (insert phone numbers). 2. In case of a service outage, clinic services can be found at <Insert emergency relocation site, such as neighboring clinic or acute care facility>. 3. The Clinic Administrator is responsible for determining when this facility is not able to care for patients. 4. In the absence of the Clinic Administrator, <Insert Name> is assigned the task of determining evacuation necessity. 5. Patient evacuation prioritization (triage) will be handled by <Insert Name>. 6. If patients are not going to be transported away from the site, they will be held at <Insert Location>. 7. If patients require transportation to an acute care facility, transportation will be arranged through <Insert EMS Services and contact information> 8. Facilities (neighboring clinic or acute care facility) which are pre-approved to accept patients from this clinic are: <Insert Clinic Names and Address> 9. Staff will provide the patient with the following prior to leaving the clinic: Copy of medical record Medicines necessary for 48 hours of treatment Name/address of destination 10. In the event that there is only minor damage causing the clinic to divert its patients, interim care will be administered at the following temporary location sites: <Insert Clinic Names and Locations> 11. The following emergency attending physicians are authorized to serve in this clinic: <Insert Physician Names> Iowa Department of Public Health Center for Disaster Operations & Response Appendix B: Incident Command Organizational Chart Iowa Department of Public Health Center for Disaster Operations & Response Appendix C: Sample Job Action Sheets Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM INCIDENT COMMANDER Job Action Sheet INCIDENT COMMANDER Position Assigned To: Command Center: Telephone: Mission: Organize and direct Emergency Operations Center (EOC). Give overall direction for off-site facility operations and if needed, authorize evacuation. Immediate ____ Initiate the Incident Command System by assuming role of Incident Commander. ____ Read this entire Job Action Sheet. ____ Put on position identification vest. ____ Appoint all Section Chiefs and the Medical Staff Unit Leader positions; distribute the four section packets which contain: Job Action Sheets for each position Identification vest for each position Forms pertinent to Section & positions ____ Appoint Public Information Officer, Liaison Officer, and Safety Officer; distribute Job Action Sheets (may be pre-established). ____ Announce a status/action plan meeting of all Section Chiefs and Medical Staff Unit Leader to be held within 5 to 10 minutes. ____ Assign someone as Documentation Recorder/Aide. ____ Receive status report and discuss an initial action plan with Section Chiefs and Medical Staff Unit Leader. Determine appropriate level of service. ____ Obtain patient census and status from Planning Section Chief. Emphasize proactive actions within the Planning Section. Call for a patient projection report for 4, 8, 24 & 48 hours from time of incident onset. Adjust projections as necessary. ____ Authorize a patient prioritization assessment for the purposes of designating appropriate early discharge, if additional beds needed. ____ Assure that contact and resource information has been established with outside agencies through the Liaison Officer. ____ Authorize resources as needed or requested by Section Chiefs. ____ Designate routine briefings with Section Chiefs to receive status reports and update the action plan regarding the continuance and termination of the action plan. ____ Communicate status to base hospital ____ Consult with Section Chiefs on needs for staff, physician, and volunteer responder food and shelter. Consider needs for dependents. Authorize plan of action. ____ Approve media releases submitted by Public Information Officer. ____ Observe all staff, volunteers and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM SAFETY OFFICER Job Action Sheet SAFETY OFFICER Positioned Assigned To: You Report To: Command Center: (Emergency Incident Commander) Telephone: Mission: Monitor and have authority over the safety of rescue operations and hazardous conditions. Organize and enforce scene/facility protection and traffic security. Immediate ____ ____ ____ ____ ____ ____ ____ ____ ____ Intermediate ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ Receive appointment from Incident Commander. Read this entire Job Action sheet and review organizational chart. Put on position identification vest. Obtain a briefing from Incident Commander. Implement the facility's disaster plan emergency lockdown policy and personnel identification policy. Establish Security Command Post. Remove unauthorized persons from restricted areas. Establish ambulance entry and exit routes in cooperation with Transportation Unit Leader. Secure the E.O.C., triage, patient care, morgue, and other sensitive or strategic areas from unauthorized access. Secure areas evacuated to and from, to limit unauthorized personnel access. Initiate contact with fire, police agencies through the Liaison Officer, when necessary. Advise the Incident Commander and Section Chiefs immediately of any unsafe, hazardous or security related conditions. Assist Labor Pool and Medical Staff Unit Leaders with credentialing/screening process of volunteers. Prepare to manage large numbers of potential volunteers. Confer with Public Information Officer to establish areas for media personnel. Establish routine briefings with Incident Commander. Provide vehicular and pedestrian traffic control. Secure food, water, medical, and blood resources. Inform staff to document all actions and observations. Establish routine briefings with Safety & Security staff. Observe all staff, volunteers and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM LIAISON OFFICER Job Action Sheet LIAISON OFFICER Positioned Assigned To: You Report To: Command Center: (Emergency Incident Commander) Telephone: Mission: Function as incident contact person for representatives from other agencies. Immediate ____ ____ ____ ____ ____ ____ ____ ____ Intermediate ____ Receive appointment from Incident Commander. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Obtain briefing from Incident Commander. Review county and municipal emergency organizational charts to determine appropriate contacts and message routing. Coordinate with Public Information Officer. Obtain information to provide the interhospital emergency communication network, municipal Emergency Operations Center (EOC) and/or county Emergency Operations Center as appropriate, upon request. The following information should be gathered for relay: Patient Care Capacity Any current or anticipated shortage of personnel, supplies, etc. Current condition of facility structure and utilities (facility’s overall status). Number of patients to be transferred by wheelchair or stretcher to another locations. Any resources which are requested by other facilities (i.e., staff, equipment, supplies). Establish communication with the assistance of the Communication Unit Leader with the interhospital emergency communication network, municipal EOC or with county EOC/County Health Officer. Relay current hospital status. Establish contact with liaison counterparts of each assisting and cooperating agency (i.e., municipal EOC.). Keeping governmental Liaison Officers updated on changes and development of hospital's response to incident. Request assistance and information as needed through the interhospital emergency communication network or municipal/county EOC. Iowa Department of Public Health Center for Disaster Operations & Response Extended ____ Respond to requests and complaints from incident personnel regarding inter-organization problems. ____ Prepare to assist Labor Pool Unit Leader with problems encountered in the volunteer credentialing process. ____ Relay any special information obtained to appropriate personnel in the receiving facility (i.e., information regarding toxic decontamination or any special emergency conditions). ____ Assist the Medical Staff Unit Leader and Labor Pool Unit Leader in soliciting physicians and other hospital personnel willing to volunteer as Disaster Service Workers outside of the hospital, when appropriate. ____ Inventory any material resources which may be sent upon official request and method of transportation, if appropriate. ____ Supply casualty data to the appropriate authorities; prepare the following minimum data: Number of casualties received and types of injuries treated Number hospitalized and number discharged to home or other facilities Number dead Individual casualty data: name or physical description, sex, age, address, seriousness of injury or condition ____ Observe all staff, volunteers and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. ____ Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM PUBLIC INFORMATION OFFICER Job Action Sheet PUBLIC INFORMATION OFFICER (P.I.O.) Position Assigned To: You Report To: (Emergency Incident Commander) Command Center: Telephone: Mission: Provide information to the news media. Immediate ____ ____ ____ ____ ____ Intermediate ____ ____ ____ ____ Extended ____ ____ ____ ____ ____ Receive appointment from Incident Commander. Read this entire Job Action sheet and review organizational chart. Put on position identification vest. Identify restrictions in contents of news release information from Incident Commander. Establish a Public Information area away from E.O.C. and patient care activity. Ensure that all news releases have the approval of the Incident Commander. Issue an initial incident information report to the news media with the cooperation of the Situation Unit Leader. Relay any pertinent data back to Situation Unit Leader. Inform on-site media of the physical areas which they have access to, and those which are restricted. Coordinate with Safety Officer. Contact other at-scene agencies to coordinate released information, with respective Public Information Officers. Inform Liaison Officer of action. Obtain progress reports from Section Chiefs as appropriate. Notify media about casualty status. Direct calls from those who wish to volunteer to Labor Pool. Contact Labor Pool to determine requests to be made to the public via the media. Observe all staff, volunteers, and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM LOGISTICS SECTION Job Action Sheet Logistics Section Chief LOGISTICS SECTION CHIEF Positioned Assigned To: You Report To: Logistics Command Center: (Emergency Incident Commander) Telephone: Mission: Organize and direct those operations associated with maintenance of the physical environment, and adequate levels of food, shelter, and supplies to support the medical objectives. Immediate ____ Receive appointment from the Incident Commander. Obtain packet containing Section's Job Action Sheets, identification vests, and forms. ____ Read this entire Job Action Sheet and review organizational chart. ____ Put on position identification vest. ____ Obtain briefing from Incident Commander. ____ Appoint Logistics Section Unit Leaders: Communications Unit Leader, Materials Supply Unit Leader, and Transportation Unit Leader; distribute Job Action Sheets and vests (may be preestablished). ____ Brief unit leaders on current situation; outline action plan and designate time for next briefing. ____ Establish Logistics Section Center in proximity to E.O.C.. ____ Obtain information and updates regularly from unit leaders and officers; maintain current status of all areas; pass status info to Situation-Status Unit Leader. ____ Communicate frequently with Incident Commander. ____ Obtain needed supplies with assistance of the Finance Section Chief, Communications Unit Leader, and Liaison Officer. ____ Assure that all communications are copied to the Communications Unit Leader. ____ Document actions and decisions on a continual basis. ____ Observe all staff, volunteers and patients for signs of stress and inappropriate behavior. Report concerns to Psychological Support Unit Leader. Provide for staff rest periods and relief. ____ Other concerns: Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM LOGISTICS SECTION Job Action Sheet Transportation Unit Leader TRANSPORTATION UNIT LEADER Positioned Assigned To: You Report To: (Logistics Section Chief) Logistics Command Center: Telephone: Mission: Organize and coordinate the transportation of all casualties, ambulatory, and non-ambulatory. Arrange for the transportation of human and material resources to and from the facility. Immediate ____ Receive appointment from Logistics Section Chief. ____ Read this entire Job Action Sheet and review the organizational chart. ____ Put on position identification vest. ____ Receive briefing from Logistics Section Chief. ____ Assess transportation requirements and needs for patients, personnel and materials. ____ Establish ambulance off-loading area in cooperation with the Triage Unit Leader. ____ Assemble gurneys, litters, wheelchairs, and stretchers in proximity to ambulance off-loading area and Triage Area. ____ Establish ambulance loading area in cooperation with the Operations Section Chief. ____ Contact Safety & Security Officer on security needs of loading areas. ____ Provide for the transportation/shipment of resources into and out of the facility. ____ Secure ambulance or other transport for discharged patients. ____ Identify transportation needs for ambulatory casualties. ____ Maintain transportation assignment record in Triage Area, Discharge Area, and Material Supply Pool. ____ Keep Logistics Section Chief apprised of status. ____ Direct unassigned personnel to Labor Pool. ____ Observe and assist any staff who exhibits signs of stress or fatigue. Provide for staff rest periods and relief. ____ Other concerns: Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM LOGISTICS SECTION Job Action Sheet Communications Unit Leader COMMUNICATIONS UNIT LEADER Positioned Assigned To: You Report To: Logistics Command Center: (Logistics Section Chief) Telephone: Mission: Organize and coordinate internal and external communications; act as custodian of all logged/documented communications. Immediate ____ Receive appointment from Logistics Section Chief. ____ Read this entire Job Action Sheet and review organizational chart back. ____ Put on position identification vest. ____ Obtain briefing from Incident Commander or Logistics Section Chief. ____ Establish a Communications Center in close proximity to E.O.C. ____ Request the response of assigned amateur radio personnel assigned to facility. ____ Assess current status of internal and external telephone system and report to Logistics Section Chief ____ Establish a pool of runners and assure distribution of 2-way radios to pre-designated areas. ____ Use pre-established message forms to document all communication. Instruct all assistants to do the same. ____ Establish contact with Liaison Officer. ____ Receive and hold all documentation related to internal facility communications. ____ Monitor and document all communications sent and received via the interhospital emergency communication network or other external communication. ____ Establish mechanism to alert Code Team and Fire Suppression Team to respond to internal patient and/or physical emergencies, i.e. cardiac arrest, fires, etc. ____ Observe all staff, volunteers, and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. ____ Other concerns: Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM LOGISTICS SECTION Job Action Sheet Materials Supply Unit Leader MATERIALS SUPPLY UNIT LEADER Positioned Assigned To: You Report To: (Logistics Section Chief) Logistics Command Center: Telephone: Mission: Organize and supply medical and non-medical care equipment and supplies. Immediate ____ ____ ____ ____ ____ ____ ____ ____ Extended ____ ____ ____ ____ ____ Receive appointment from Logistics Section Chief. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Receive briefing from Logistics Section Chief. Meet with and brief Materials Management and Central/Sterile Supply Personnel. Establish and communicate the operational status of the Materials Supply Pool to the Logistics Section Chief, E.O.C. and Procurement Unit Leader. Collect and coordinate essential medical equipment and supplies (prepare to assist with equipment salvage and recovery efforts). Develop medical equipment inventory to include, but not limited to the following: Bandages, dressings, compresses, and suture material Sterile scrub brushes, normal saline, anti-microbial skin cleanser. Waterless hand cleaner and gloves. Fracture immobilization, splinting, and casting materials. Backboard, rigid stretchers. Non-rigid transporting devices (litters). Oxygen-ventilation-suction devices. Advance life support equipment (chest tube, airway, major suture trays). Identify additional equipment and supply needs. Make requests/needs known through Logistics Section Chief. Gain the assistance of the Procurement Unit Leader when indicated. Determine the anticipated pharmaceuticals needed with the assistance of the Medical Unit Leader. Coordinate with Safety & Security Officer to protect resources. Observe and assist staff who exhibit signs of stress or fatigue. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM PLANNING SECTION Job Action Sheet Planning Section Chief PLANNING SECTION CHIEF Positioned Assigned To: You Report To: Planning Command Center: (Emergency Incident Commander) Telephone: Mission: Organize and direct all aspects of Planning Section operations. Ensure the distribution of critical information/data. Compile scenario/resource projections from all section chiefs and effect long range planning. Document and distribute facility Action Plan. Immediate ____ Receive appointment from Incident Commander. Obtain packet containing Section's Job Action Sheets. ____ Read this entire Job Action Sheet and review organizational chart. ____ Put on position identification vest. ____ Obtain briefing from Incident Commander. ____ Recruit a documentation aide from the Labor Pool ____ Appoint Planning unit leaders: Situation Unit Leader and Labor Pool Unit Leader, distribute the corresponding Job Action Sheets and vests (may be pre-established). ____ Brief unit leaders after meeting with Incident Commander. ____ Provide for a Planning/Information Center. ____ Ensure the formulation and documentation of an incident-specific, facility Action Plan. Distribute copies to Incident Commander and all section chiefs. ____ Call for projection reports (Action Plan) from all Planning Section unit leaders and section chiefs for scenarios 4, 8, 24, & 48 hours from time of incident onset. Adjust time for receiving projection reports as necessary. ____ Instruct Situation Unit Leader and staff to document/update status reports from all disaster section chiefs and unit leaders for use in decision making and for reference in post-disaster evaluation and recovery assistance applications. ____ Obtain briefings and updates as appropriate. Continue to update and distribute the facility Action Plan. ____ Schedule planning meetings to include Planning Section unit leaders, section chiefs and the Incident Commander for continued update of the facility Action Plan. ____ Continue to receive projected activity reports from section chiefs and Planning Section unit leaders at appropriate intervals. Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response ____ Assure that all requests are routed/documented through the Communications Unit Leader. ____ Observe all staff, volunteers and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. ____ Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM PLANNING SECTION Job Action Sheet Situation Unit Leader SITUATION UNIT LEADER Positioned Assigned To: You Report To: (Planning Section Chief) Planning Command Center: Telephone: Mission: Maintain current information regarding the incident status for all hospital staff. Ensure a written record of the hospital's emergency planning and response. Develop the hospital's internal information network. Monitor the maintenance and preservation of the computer system. Immediate ____ ____ ____ ____ ____ ____ ____ ____ Intermediate ____ ____ ____ ____ Extended ____ ____ Receive appointment from Planning Section Chief. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Obtain briefing from Planning Section Chief. Obtain status report on computer information system. Assign recorder to document decisions, actions, and attendance in EOC. Establish a status/condition board in EOC with a documentation aide. Ensure that this board is kept current. Assign recorder to Communications Unit Leader to document telephone, radio, and memo traffic. Ensure that an adequate number of recorders are available to assist areas as needed. Coordinate personnel with Labor Pool. Supervise backup and protection of existing data for main and support computer systems. Publish an internal incident informational sheet for employee information at least every 4-6 hours. Enlist the assistance of the Public Information Officer and Labor Pool Unit Leader. Ensure the security and prevent the loss of medical record hard copies. Observe all staff, volunteers, and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM PLANNING SECTION Job Action Sheet Labor Pool Unit Leader LABOR POOL UNIT LEADER Positioned Assigned To: You Report To: (Planning Section Chief) Planning Command Center: Telephone: Mission: Collect and inventory available staff and volunteers at a central point. Receive requests and assign available staff as needed. Maintain adequate numbers of both medical and non-medical personnel. Assist in the maintenance of staff morale. Immediate ____ ____ ____ ____ ____ Receive appointment from Planning Section Chief. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Obtain briefing from the Planning Section Chief. Establish Labor Pool area and communicate operational status to E.O.C. and all patient care and non-patient care areas. ____ Inventory the number and classify staff presently available. Use the following classifications and sub-classifications for personnel: A. Physician (Obtain with assistance of Medical Staff Unit Leader.) 1. Critical Care 2. General Care 3. Other B. Nurse 1. Critical Care 2. General Care 3. Other C. Medical Technicians 1. Patient Care (aides, orderlies, EMTs, etc.) 2. Diagnostic ____ Establish a registration and credentialing desk for volunteers not employed or associated with the base hospital. ____ Obtain assistance from Safety Officer in the screening and identification of volunteer staff. Iowa Department of Public Health Center for Disaster Operations & Response Intermediate Extended ____ Meet with Clinic Unit Leader, Medical Staff Unit Leader and Operations Section Chief to coordinate long term staffing needs. ____ Maintain log of all assignments. ____ Assist the Situation Unit Leader in publishing an informational sheet to be distributed at frequent intervals to update the hospital population. ____ Maintain a message center in Labor Pool Area with the cooperation of Situation Unit Leader. ____ Brief Planning Section Chief as frequently as necessary on the status of labor pool numbers and composition. ____ Develop staff rest and nutritional area ____ Document actions and decisions on a continual basis. ____ Observe all staff, volunteers and patients for signs of stress and inappropriate behavior. ____ Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM FINANCE SECTION Job Action Sheet Finance Section Chief FINANCE SECTION CHIEF Positioned Assigned To: You Report To: Finance Command Center: (Incident Commander) Telephone: Mission: Monitor the utilization of financial assets. Oversee the acquisition of supplies and services necessary to carry out the facility's medical mission. Supervise the documentation of expenditures relevant to the emergency incident. Immediate ____ Receive appointment from Incident Commander. Obtain packet containing Section's Job Action Sheets. ____ Read this entire Job Action Sheet and review organizational chart. ____ Put on position identification vest. ____ Obtain briefing from Incident Commander. ____ Appoint Time Unit Leader, Procurement Unit Leader, and Cost Unit Leader; distribute the corresponding Job Action Sheets and vests (may be pre-established). ____ Confer with Unit Leaders after meeting with Incident Commander; develop a section action plan. ____ Establish a Financial Section Operations Center. Ensure adequate documentation/recording personnel. ____ Approve a "cost-to-date" incident financial status report submitted by the Cost Unit Leader every eight hours summarizing financial data relative to personnel, supplies, and miscellaneous expenses. ____ Obtain briefings and updates from Incident Commander as appropriate. Relate pertinent financial status reports to appropriate chiefs and unit leaders. ____ Schedule planning meetings to include Finance Section unit leaders to discuss updating the section's incident action plan and termination procedures. ____ Assure that all requests for personnel or supplies are copied to the Communications Unit Leader in a timely manner. ____ Observe all staff, volunteers, and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. ____ Other concerns: Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM FINANCE SECTION Job Action Sheet Time Unit Leader TIME UNIT LEADER Positioned Assigned To: You Report To: Chief). (Finance Section Finance Command Center: Telephone: Mission: Responsible for the documentation of personnel time records. The monitoring and reporting of regular and overtime hours worked/volunteered. Immediate ____ ____ ____ ____ ____ Intermediate ____ ____ Extended ____ ____ ____ Receive appointment from Finance Section Chief. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Obtain briefing from Finance Section Chief; assist in the development of the section action plan. Ensure the documentation of personnel hours worked and volunteer hours worked in all areas relevant to the facility's emergency incident response. Confirm the utilization of the Section Personnel Time Sheet by all section chiefs and/or unit leaders. Coordinate with Labor Pool Unit Leader. Collect all Emergency Incident Time Sheets from each work area for recording and tabulation every eight hours, or as specified by the Finance Section Chief. Forward tabulated Section Personnel Time Sheets to Cost Unit Leader every eight hours. Prepare a total of personnel hours worked during the declared emergency incident. Observe all staff, volunteers, and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM FINANCE SECTION Job Action Sheet Procurement Unit Leader PROCUREMENT UNIT LEADER Positioned Assigned To: You Report To: (Finance Section Chief) Finance Command Center: Telephone: Mission: Responsible for administering accounts receivable and payable to contract and non-contract vendors. Immediate ____ ____ ____ ____ ____ ____ Intermediate ____ Extended ____ ____ ____ Receive appointment from Finance Section Chief. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Obtain briefing from Finance Section Chief; assist in the development of the section action plan. Ensure the separate accounting of all contracts specifically related to the emergency incident; and all purchases within the enactment of the emergency incident response plan. Obtain authorization to initiate purchases from the Finance Section Chief, or authorized representative. Forward a summary accounting of purchases to the Cost Unit Leader every eight hours. Prepare a Procurement Summary Report identifying all contracts initiated during the declared emergency incident. Observe all staff, volunteers and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM FINANCE SECTION Job Action Sheet Cost Unit Leader COST UNIT LEADER Positioned Assigned To: You Report To: Chief) Finance Command Center: (Finance Section Telephone: Mission: Responsible for providing cost analysis data for declared emergency incident. Maintenance of accurate records of incident cost. Immediate ____ Receive appointment from Finance Section Chief. ____ Read this entire Job Action Sheet and review the organizational chart. ____ Put on position identification vest. ____ Obtain briefing from Finance Section Chief; assist in development of section action plan. ____ Meet with Time Unit Leader and Procurement Unit Leader to establish schedule for routine reporting periods. ____ Prepare a "cost-to-date" report form for submission to Finance Section Chief once every eight hours. ____ Inform all section chiefs of pertinent cost data at the direction of the Finance Section Chief or Incident Commander. ____ Prepare a summary of all costs incurred during the declared emergency incident. ____ Observe all staff, volunteers, and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. ____ Other concerns: Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM OPERATIONS SECTION Job Action Sheet Operations Section Chief OPERATIONS SECTION CHIEF Positioned Assigned To: You Report To: Operations Command Center: (Incident Commander) Telephone: Mission: Organize and direct aspects relating to the Operations Section. Carry out directives of the Incident Commander. Coordinate and supervise the Medical Staff Unit, Triage Unit, and Clinic Unit. Immediate ____ Receive appointment from Incident Commander. Obtain packet containing Section's Job Action Sheets. ____ Read this entire Job Action Sheet and review organizational chart. ____ Put on position identification vest. ____ Obtain briefing from Incident Commander. ____ Appoint Medical Staff Unit Leader, Triage Unit Leader, and Clinic Unit Leader; transfer the corresponding Job Action Sheets (may be pre-established). ____ Brief all Operations Section directors on current situation and develop the section's initial action plan. Designate time for next briefing. ____ Establish Operations Section Center in proximity to EOC. ____ Meet with the Medical Unit Leader Director and Clinic Unit Leader to plan and project patient care needs. ____ Designate times for briefings and updates with all Operations Section directors to develop/update section's action plan. ____ Brief the Incident Commander routinely on the status of the Operations Section. ____ Assure that all communications are copied to the Communications Unit Leader; document all actions and decisions. ____ Observe all staff, volunteers, and patients for signs of stress and inappropriate behavior. Provide for staff rest periods and relief. ____ Other concerns: Intermediate Extended Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM Medical Staff Unit Leader Job Action Sheet MEDICAL STAFF UNIT LEADER Positioned Assigned To: You Report To: Chief) (Operations Section Planning Command Center: Telephone: Mission: Collect available physicians, and other medical staff, at a central point. Credential volunteer medical staff as necessary. Assist in the assignment of available medical staff as needed. Immediate ____ ____ ____ ____ ____ ____ ____ Intermediate ____ Extended ____ ____ ____ ____ ____ ____ ____ ____ Receive assignment from Operations Section Chief. Read this entire Job Action Sheet and refer to organizational chart. Put on position identification vest. Obtain briefing from Incident Commander or Operations Section Chief. Establish Medical Staff Pool in predetermined location and communicate operational status to EOC and base hospital. Obtain documentation personnel from Labor Pool. Inventory the number and types of physicians, and other staff present. Relay information to Labor Pool Unit Leader. Register and credential volunteer physician/medical staff. Request the assistance of the Labor Pool Unit Leader and Safety Officer when necessary. Meet with Labor Pool Unit Leader, Clinic Unit Leader, and Operations Section Chief to coordinate projected staffing needs and issues. Assign medical staff to patient care and treatment areas. Establish a physician message center and emergency incident information board with the assistance of Labor Pool Unit Leader. Develop a medical staff rotation schedule. Maintain a log of medical staff assignments. Brief Operations Section Chief as frequently as necessary on the status of medical staff pool numbers and composition. Develop a medical staff rest and nutritional area. Document actions and decisions on a continual basis. Observe and assist medical staff who exhibit signs of stress and other fatigue. Iowa Department of Public Health Center for Disaster Operations & Response HOSPITAL EMERGENCY INCIDENT COMMAND SYSTEM TRIAGE UNIT LEADER Job Action Sheet OPERATIONS SECTION Triage Unit Leader Positioned Assigned To: You Report To: Chief) (Operations Section Planning Command Center: Telephone: Mission: Sort casualties according to priority of injuries or illness, and assure their disposition to the proper treatment area. Immediate ____ ____ ____ ____ ____ ____ ____ Intermediate ____ Extended ____ ____ ____ ____ ____ ____ Receive appointment from Incident Commander. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Receive briefing from previous shift Triage Unit Leader. Maintain patient Triage Area; consult with Transportation Unit Leader to designate the ambulance off-loading area. Ensure sufficient equipment for Triage Area. Assess problem, triage-treatment needs relative to specific complaint using <INSERT LANGUAGE REGARDING TRIAGE SYSTEM> Coordinate movement of patients to patient care areas. Give patient report to Emergent Treatment Area RN, Extended Treatment Area RN, or Clinic RN as appropriate. Report emergency care equipment needs to Operations Chief. Ensure that the disaster chart and admission forms are utilized (coordinate with Medical Records Clerk). Keep Incident Commander apprised of status, number of injured in the Triage Area or expected to arrive there. Observe and assist any staff who exhibit signs of stress and fatigue. Provide for staff rest periods and relief. Review and approve the area documenter's recordings of actions/decisions in the Triage Area. Send copy to Communications Unit Leader. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response HOSPITAL EMERGENCY INCIDENT COMMAND SYSTEM MINOR CARE AREA MANAGER Job Action Sheet OPERATIONS SECTION Minor Care Area Manager Positioned Assigned To: You Report To: (Clinic Unit Leader) Operations Command Center: Telephone: Mission: Maintain the Minor Care Area capabilities to the best possible level to meet the needs of patients who are triaged to that area. Immediate ____ ____ ____ ____ ____ ____ ____ Intermediate ____ ____ Extended ____ ____ ____ ____ ____ Receive appointment from Clinic Unit Leader. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Receive briefing from previous shift Minor Care Area Manager. Assess current critical care patient capabilities. Project immediate and prolonged capabilities to provide services based on known resources. Develop action plan in cooperation with other In-Patient Area unit managers and the Clinic Unit Leader. Request the assistance of the Clinic Unit Leader to obtain resources if necessary. Provide assignments to Paramedic in Minor Care Area. Coordinate EMS transportation of patients with Transportation Unit Leader. Report equipment/material needs to Clinic Unit Leader. Ensure that all area and individual documentation is current and accurate (coordinate with Communications Unit Leader). Keep Clinic Unit Leader apprised of status, capabilities, and projected services. Observe and assist any staff who exhibit signs of stress and fatigue. Provide for staff rest periods and relief. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response INCIDENT COMMAND SYSTEM EMERGENT TREATMENT AREA MANAGER Job Action Sheet OPERATIONS SECTION Emergent Care Area Manager Positioned Assigned To: You Report To: (Clinic Unit Leader) Operations Command Center: Telephone: Mission: Maintain the Emergent Treatment Area capabilities to the best possible level to meet the needs of patients who are triaged to that area. Immediate ____ ____ ____ ____ ____ ____ ____ Intermediate ____ ____ Extended ____ ____ ____ ____ ____ Receive appointment from Clinic Unit Leader. Read this entire Job Action Sheet and review organizational chart. Put on position identification vest. Receive briefing from previous shift Emergent Treatment Area RN. Assess current critical care patient capabilities. Project immediate and prolonged capabilities to provide services based on known resources. Develop action plan in cooperation with other In-Patient Area unit leaders and the Clinic Unit Leader Request the assistance of the In-Patient Areas Supervisor to obtain resources if necessary. Provide assignments to Paramedic in Emergent Treatment Area. Coordinate EMS transportation of patients with Transportation Unit Leader. Report equipment/material needs to Clinic Unit Leader. Ensure that all area and individual documentation is current and accurate (coordinate with Communications Unit Leader). Keep Clinic Unit Leader apprised of status, capabilities and projected services. Observe and assist any staff who exhibit signs of stress and fatigue. Provide for staff rest periods and relief. Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response HOSPITAL EMERGENCY INCIDENT COMMAND SYSTEM Job Action Sheet OPERATIONS SECTION MEDICAL SERVICES SUBSECTION Registered Nurse Registered Nurse Positioned Assigned To: You Report To: Operations Command Center: (Clinic Unit Leader) Telephone: Mission: Assist in all Treatment Areas within your scope of practice in order to meet the needs of the patients in that area. Immediate ____ Check in and receive a briefing from Clinic unit Leader. ____ Read this entire Job Action Sheet and review the organizational chart. ____ Put on position identification vest. ____ Receive briefing from previous shift Registered Nurse in the treatment area you are assigned. ____ Assess the current care needs and provide care based upon your scope of practice and the resources that are available. ____ Request resources from the area manager assigned to your treatment area. ____ Complete work assigned to you by the area manager in charge of your treatment area. Extended ____ Ensure that all area documentation is current and accurate. ____ Keep the area manager of your treatment area appraised of status, capabilities, and project services. ____ Observe and assist any staff who exhibit signs of stress and fatigue. ____ Other concerns: Iowa Department of Public Health Center for Disaster Operations & Response Appendix D: Clinic Self-Assessment Worksheet Iowa Department of Public Health Center for Disaster Operations & Response Health Clinic Self-Assessment Survey for Disaster and Emergency Preparedness Clinic Background Clinic Name: Note: If clinic is a satellite or part of a network, also indicate name of parent organization. County: Clinic Type (check all that apply): □ □ □ □ □ □ Primary Care Clinic - Community Clinic Primary Care Clinic - Free Clinic Federally Qualified Health Clinic (FQHC) Migrant Health Center Rural Health Clinic (95-210 clinic) County Clinic □ □ □ □ □ □ Tribal or Urban Indian Health Clinic Specialty Care Clinic - Surgical Clinic Specialty Care Clinic - Chronic Care Clinic University Clinic Hospital or Health Plan Based Outpatient Clinic Other: _______________________ How many miles is your clinic from the nearest emergency department (range of miles if there are multiple sites)? miles Emergency Planning Expectations (Y=Yes/N=No/DK=Don’t Know/NA=Not Applicable) If a major disaster (such as a large earthquake, bioterrorism attack, pandemic, etc.) created a large number of injured or ill patients in the community you serve: Item Will ill and injured patients will come to or be brought to your clinic? Will people with minor injuries or no injuries come to your clinic for information, reassurance or counseling? Will your clinic participate in the county’s medical response to the event by receiving overflow casualties from hospitals, providing clinic staff at other sites, or by providing space in the clinic for medical responders? Do you plan to close your clinic and refer patients to other sources of care? Do you plan to keep your clinic open or re-open your clinic if closed? Do you plan to expand the number of hours your clinic would operate? Would the county will provide your clinic with support for its response? Y N DK N/A Iowa Department of Public Health Center for Disaster Operations & Response Clinic Emergency Preparedness Status (Y=Yes/N=No/DK=Don’t Know/NA=Not Applicable) Internal Emergency / Evacuation Plan Does your clinic have a plan for responding to fires and other internal emergencies in the clinic? Has your clinic’s plan been updated within the past two years? Does your clinic have emergency or back up power? Disaster Planning Does your clinic have a plan for responding to disasters in the community it serves (external disasters)? Has your disaster plan been updated within the past two years? Does the disaster plan address caring for a mass influx of patients? Does the disaster plan make provisions for addressing the health needs of older adults, children, or people with disabilities? Does the disaster plan address the language needs of your clinic’s limited English proficient patients? Does the plan specifically address bioterrorism preparedness? Does your clinic participate in community planning for disasters? Other Policies and Procedures Does your clinic have the following policies and procedures in place: Clinic Evacuation? Patient care during a disaster? Handling patients who are exposed to biological or chemical events? Training and Drills Do clinic staff members receive training in disaster awareness, preparedness and response? Does the training include preparedness for chemical or biological terrorism events? Within the past two years, did your clinic participate in a disaster drill? Communications Does your clinic have a plan to contact staff after hours in an emergency? Does your clinic have high speed Internet access (other than dial up)? Are procedures in place for establishing emergency communications between the clinic and the county or local government? Y N DK N/A Y N DK N/A Y N DK N/A Y N DK N/A Y N DK N/A Additional Comments: ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________ Iowa Department of Public Health Center for Disaster Operations & Response Barriers to Effective Disaster Preparedness in Your Clinic Please prioritize the three (3) most concerning barriers to your clinic; indicate by marking 1, 2 or 3 next to the three selected barriers with #1 used for the most concerning barrier): Physical location is unlikely to be hit by a major disaster There is a lack of information about how to provide medical care to large numbers of disaster victims There is a lack of information about how to care for victims who may be exposed to biological or chemical agents There is a lack of everyday health care capacity (limited space and providers) There is a lack of time for staff to train, develop plans and conduct exercises There is a lack of relationships with county emergency management office, hospitals or local health department: Specify____________________________________________ There is a lack of funds to purchase supplies / equipment There is a lack of funds to support staff training or back-filling key positions while they receive training There is a lack of reimbursement for costs incurred during disaster response Technical Assistance Priorities for Your Clinic Please prioritize the three (3) most important technical assistance priorities needed to be addressed by your clinic; indicate by marking 1, 2 or 3 next to the three selected priorities with #1 used for the most important need): 5.1 Planning and preparedness tools and templates 5.2 Disaster organization structure, response management and decision making tools 5.3 Policy and procedure templates 5.4 Procedures for communications with staff (e.g., staff callback) 5.5 Procedures for communications with government emergency system and responders 5.6 Establishing emergency medical supplies caches 5.7 Disaster response equipment requirements 5.8 Training – General disaster 5.9 Training – Bioterrorism 5.10 Technical advice, coaching and information Iowa Department of Public Health Center for Disaster Operations & Response Technical Assistance Details (select all that apply): Identify the technical assistance needs for your clinic by placing an “X” next to each in the Yes column. Prioritize those that are selected, with “One” being this highest priority. Planning Emergency plan for fire, evacuation and internal emergencies Disaster plan for responding to external (community) disasters Plan for response to bioterrorism attack Use of personal protective equipment, (e.g., protective suits, masks or kits) Procedures for handling large numbers of patients with infectious diseases Defining clinic role in a disaster (e.g., close, remain open, or re-open) Development of a disaster response management structure and decision process (e.g., Incident Command System) Managing mass influx of patients Meeting the needs of vulnerable populations (e.g., elderly, disabled, children)? Meeting needs of culturally and linguistically diverse populations Staff Safety / Continuity of Clinic Operations Restoration of clinic services following a disaster Housing and feeding clinic personnel for 72 hours Home and self-care during disasters for staff, patients and community Responding to Disaster Victims Extending regular clinic hours in a disaster situation Triaging patients to appropriate hospitals and other treatment centers Transportation for triaged patients to appropriate facilities) Emergency cache of supplies Policies and Procedures Establishing disaster response teams Security / lock-down policy Personnel recall Clinic evacuation Patient care during a disaster Report of suspicious symptoms to the county health department Handling patients who are exposed to biological or chemical contaminants Coordination with Emergency Response Agencies Working with county or local other healthcare providers to develop plans for and coordinate response to disasters Working with volunteers Obtaining emergency supplies from vendors, county or other sources Training and Exercises Staff training in disaster awareness, preparedness and response Training in preparedness for chemical or biological terrorism events Training for medical staff to identify and properly/safely remove biological and chemical contaminants Planning and conducting disaster drills Participating in local emergency services drills and exercises Yes Priority Yes Priority Yes Priority Yes Priority Yes Priority Yes Priority Iowa Department of Public Health Center for Disaster Operations & Response Appendix E: Sample Exercise Scenarios, After-Action Report, and Improvement Plan Iowa Department of Public Health Center for Disaster Operations & Response Mass Casualty Exercise Scenario Natural Disaster (Slow Onset): Heat Wave and Drought Severe Winter Storm NOTE: These exercises are intended to raise considerations for “slow onset” disasters, i.e., those that arise from sustained environmental conditions, rather than from a single catastrophic incident. There are significant differences between the effects of a summer heat wave and drought, as compared to a winter storm and extended severe cold. Nevertheless, there are also similarities in planning and preparation, and in recognizing the consequences of an extended hazard and in taking steps to mitigate the effects before conditions become severe. HEAT WAVE AND PERSISTENT DROUGHT It is mid-August during the hottest summer in a ten-year period of record-breaking summer temperatures. Across the nation, communities have struggled with persistent drought that has scorched lawns and forests, decimated agriculture and produce, and reduced municipal water supplies to record level lows. Lakes and reservoirs have been reduced to such a degree that electrical power generation has been affected nationwide. Temperatures have surpassed all records, with significant impact on some sectors of the local community. Hardest hit have been the poorest communities, where air conditioning is infrequently available and ventilation in high-rise apartment buildings is poorest. In retirement and convalescent homes the heat and humidity have had a serious impact on the elderly, particularly with shortages in electrical power limiting the use of air conditioning. In rural communities, wells have been running dry, necessitating the delivery of water in trucks, or the use of less well-monitored water sources. Summer school programs, sporting events and organized recreational activities have all been curtailed or modified, in order to reduce risks due to over-exertion. For the last three weeks, there has been a noticeable rise in heat-related illnesses throughout the region. EMS in your area has responded to as many as eight calls per day for injuries and conditions attributable to heat and physiological stress. For the first time this summer, there were two heat-related deaths in your area within the last week. Topics of Discussion 1. 2. 3. What specific heat-related injuries or illnesses would you want your medical staff to be particularly prepared to receive and diagnose? What demographic groups in your area are most at risk for heat related illnesses? What precautions can those groups take to limit exposure and hazard? What steps should your facility take to protect its own staff during a possible increase in patient load and working hours? What institutional or seasonal factors might contribute to overwork and staff stress during this period? Iowa Department of Public Health Center for Disaster Operations & Response 4. 5. What impact is a long-term heat wave and drought likely to have on your facility and its infrastructure? What precautions should your facility take to ensure its ability to maintain service and quality of care? What assistance can or should your facility provide to local municipal leadership in coping with this situation? How can your region’s medical community combine its resources and pool assets to assist in a sustained emergency of this sort? Iowa Department of Public Health Center for Disaster Operations & Response SEVERE WINTER STORM After the severe storms and record-breaking snows of the previous winter, it was not expected that this year would be as bad. However, for the second consecutive year, records are being broken across the central and eastern United States for severe winter conditions. There have been persistent freezing temperatures for nearly six weeks, coupled with several winter storms. Accumulated snow has reached record levels, with snow banks along plowed highways and streets exceeding six feet in many places. With the highest costs of home heating oil since the first months of the autumn, many homes and smaller buildings have gone without heat. As a consequence, the freezing of interior spaces has resulted in a significant demand on plumbing services and public works departments to repair damaged piping systems throughout the area. Unfortunately, there are few signs of a break in the weather. Long-term predictions are for freezing weather to continue for at least another month. There is also another winter storm approaching from the northwest which is anticipated to arrive in the region within the next week. Topics of Discussion 1. What are the routine medical emergencies that can be anticipated with a prolonged period of cold weather in your region? 2. In the event that expectations are exceeded and bad weather endures, what impact might those conditions have on such aspects as staffing? 3. What weather-related illnesses or conditions would you expect to see over time? Would confining the local population to homes and indoor activities exacerbate or reduce routine winter medical conditions like influenza, hypothermia, and exposure? Iowa Department of Public Health Center for Disaster Operations & Response Mass Casualty Exercise Scenario Influenza In early Spring, the ProMED online newsletter reported that an unknown illness had afflicted a number of Singapore residents. The illness exhibited the classic symptoms of influenza, including persistent cough and congestion of the chest and throat; high fever and malaise; general aching of the muscles, and loss of appetite. However, of the thirteen verified cases, eight died within 48 hours of the first symptoms. The other five were in local hospitals and two were in critical condition. Singapore authorities had immediately initiated an emergency medical alert, and the victims and their families where placed in isolation for observation. During the next three days, 22 other cases emerged among the Singaporean populace, and other similar cases had been reported in Tapei, Kuala Lumpur, Jakarta and Bangkok. Within a week, worldwide news services had begun to focus attention on the mysterious illness, and public health officials of the World Health Organization and Pan American Health Organization had issued medical alerts. During the next two weeks, 67 new cases of the illness (unofficially dubbed the Singapore Flu) had been reported world-wide, including six cases in Russia and two in Sweden. Of those, there had been 19 reported fatalities, all within 72 hours of diagnosis. There was no specific demographic group or age affected, as victims of the illness included two school children, healthy working-age men and women, and several elderly patients. In the United States there was a growing concern among the public health community. The Centers for Disease Control and Prevention issued a warning, and focused particular attention on the west coast and Hawaii. U.S. news reports had begun referring to the 1918 influenza epidemic and its affect on the U.S. society. In your community, there has been front-page coverage of the disease in newspapers and on local television. Numerous queries had begun coming in to hospital emergency rooms and to local physicians. Topics of Discussion 1. 2. 3. 4. At this point, what actions might your healthcare facility or clinic begin considering? At what point would you place those plans into action? What actions might your facility take to reassure the public in your community, and how should that information be disseminated? Does your healthcare facility have a public relations specialist, spokesman or designated physician who is known throughout your community and who regularly speaks on behalf of your facility? What concrete actions could your facility recommend that individual citizens take to reduce the likelihood of their being exposed to a contagious illness of this sort? What are the vulnerable populations in your community, and what actions might be taken on their behalf? Iowa Department of Public Health Center for Disaster Operations & Response Update Within six days the number of cases triples, with definite outbreaks of the illness identified in Rome, Hamburg, Moscow, Sydney, and Toronto. Diagnosed cases result in hospitalization 66% of the time, and the mortality rate remains consistent at 21%. Infants are the most susceptible and those above the age of 60, although one-third of the fatalities are healthy adults. Five weeks after the emergence of the first cases, two positive diagnoses are made in Hawaii, and three others in Seattle. The nation’s airlines, which had been monitoring Pacific-based passenger bases, issues an urgent travel notification, and begins to screen passengers for signs of flu or colds. Media attention, and concern on the part of the public, begins to rise. Topics of Discussion 5. What precautions should be taken at your facility to ensure positive identification and diagnosis of cases that might arise in your community? 6. What has your facility done to reassure your own staff, support personnel and their families? Update Twelve weeks after the first diagnosed case, your facility examines admits a patient who exhibits symptoms of the “Singapore Flu,” a 36 year-old male who had recently returned from a business trip to Mexico City. Topics of Discussion 7. What actions should your facility take to diagnose this case, and which medical authorities should be notified of the details? 8. What actions should your clinic initiate to isolate the patient? What steps should be placed in motion to protect your own staff and clinic personnel? Iowa Department of Public Health Center for Disaster Operations & Response Clinic After Action Report Template Facility: Date of Exercise: Report Completion Date: Other exercise/event participants and numbers: Emergency Management # Local Public Health # EMS # Laboratory # Environmental health # Other (List out, include numbers) Type of Exercise: Full-scale1 Functional2 Tabletop3 Please Describe Exercise: What worked well with your exercise? Exercise Objectives Objective Met? Y or N 1. 2. 3. 4. Yes No Yes No Yes No Yes No The intended purpose of 'full-scale' exercise is to test operational strategies and procedures. The exercise should be scripted to be as real as possible with full movement of personnel and equipment. The Emergency Operations Center (EOC) should be activated and engaged in communicating with key exercise participants. 2 The intended purpose of a 'functional' exercise is to test tactics and procedures. The exercise should be scripted to focus on one or more components of a plan or response procedure with the active participation of multiple disciplines and/or agencies. No movement of personnel or equipment is required during a functional exercise. 3 The intended purpose of a 'tabletop exercise is to generate an open and non-confrontational discussion and analysis of current plans, strategies and procedures. The simulated tabletop exercise does not require movement of personnel or equipment. 1 Improvement Plan Matrix Utilize objectives that were identified on the previous page to complete this matrix. Issue/Areas for Improvement Recommendation Responsible Timeline Party(ies)/Person(s) Iowa Department of Public Health Center for Disaster Operations and Response Appendix F: Additional Resources Iowa Department of Public Health www.idph.state.ia.us The Iowa Department of Public Health website will contain up-to-date information on public health issues affecting Iowa. Iowa Homeland Security and Emergency Management Division www.iowahomelandsecurity.org The Iowa Homeland Security and Emergency Management Division website contains information specific to disaster planning and response in Iowa. Agency for Healthcare Research and Policy http://www.ahrq.gov/browse/bioterbr.htm#tools The AHRQ website contains tools, resources, and information related to terrorism response. Centers for Disease Control and Prevention www.cdc.gov The CDC website contains information on a wide range of public health issues, including bioterrorism and disaster planning. The National Academy http://www.nap.edu/shelves/first/ The National Academy website is a search engine designed to find content related to disaster preparedness. Note: In the event of a public health emergency that generates questions from healthcare or public health officials, the Iowa Dept. of Public Health may open it’s Medical Call Center. If this center is established, you will receive information regarding phone numbers and hours of operation. 60