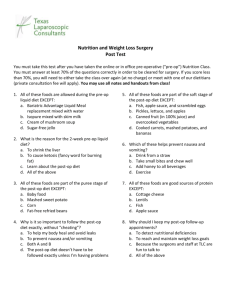
Laparascopic adrenalectomy for
advertisement

Laparascopic adrenalectomy for phaeochromocytoma (The Feast Approach) Pre-op The patient is usually admitted a week pre-op to increase their alpha blockade. The patient will invariably already be taking phenoxybenzamine and this dose will be increased every 48 hours or so by Mr Harrison or his team until the patient has significant postural hypotension and nasal stuffiness. Beta blockers are not usually used as they will produce postural hypotension for a lower degree of alpha blockade (by preventing the reflex tachycardia that normally compensates) and thus mask the fact that the patient in not properly alpha blocked. It may occasionally be necessary to beta block as well if the reflex tachycardia is too severe. Vasodilating the patient with phenoxybenzamine will also increase the effective intravascular volume and this is countered by encouraging the patient to drink plenty during this stage. Inadequate fluid intake at this stage may produce postural hypotension despite the patient still being under blocked. The night before the op, the patient will usually have had a cannula inserted and intravenous fluids given overnight. The phenoxybenzamine dose is given as normal on the morning of surgery and I also pre-med the patient with temazepam. (No longer bother) Other specific issues I tend to cover during anaesthetic consent include the risk of blood transfusion and the possibility of an asleep epidural if the surgery is converted to open with a large incision (though I have never yet inserted one in these circumstances). (Done once) An HDU bed should already have been booked. Intra-op Despite the pre-med, patients are usually hypertensive in the anaesthetic room and often receive further doses of midazolam. If the cannula in situ is small (as is usually the case) a 16G cannula is now inserted under local anaesthetic. An arterial line is also inserted under local. Induction: -pre-oxygenate -remifentanil 1mcg/kg over 60secs then 0.2mcg/kg/min (now use 0.5 mcg/kg – reduces risk of bradycardia as atropine and glycopyrrolate can trigger catecholamine release – occasionally spectacularly) -propofol -vecuronium (have now used atracurium a few times with no problem) -check with nerve stimulator that paralyzed before intubating (NG tube if lateral approach – remove at end of op, throat pack if prone) Urinary catheter (large volumes of fluid given intra/post-op) CVP line asleep Use metaraminol and fluid to treat hypotension occurring at this point. Will be relatively insensitive to alpha agonists as alpha blocked so may need generous doses if used. Positioning: If prone then turn prone on bed. Check ventilation pressures. Transfer prone onto table. Check ventilation pressures. Position with knees down. Check ventilation pressures. If difficulty ventilating consider abandoning prone approach and doing lateral approach. CO2 is insufflated at higher than normal pressure into retro- peritoneal (potential) space. Absorption increases rapidly after about 45 mins such that even if easy to ventilate initially will often need PCV 35/5-7, X18, 1:1. This will still often only just keep ET CO2 < 10. If difficulty ventilating before starting, there will be no scope to increase ventilation after insufflation. They will also tend to develop surgical emphysema with CO2, which will still be present in recovery but which needs no treatment. It will, however, tend to keep the ET CO2 raised even when insufflation has ceased. If lateral, then will need to raise head of bed as break is applied to table to keep neck straight. Once bean bag is deflated and solid DO NOT move the table again as this will split the bean bag and make Mr Harrison say rude words. Over-breaking the table may kink the IVC, obstruct venous return and cause significant hypotension. Consider unbreaking the table if hypotensive. Maintainance: I use remifentanil @ 0.2 mcg/kg/min but do not increase the dose in response to hypertensive episodes as higher doses just make the patient more bradycardic. I use isoflurane in air/oxygen with an ET iso of typically 1.3 to 1.5. With this combination I assume hypertensive episodes are related to catecholamine release not surgical stimulation. Whichever approach is used the patient needs to be kept paralyzed intraoperatively. I treat hypertensive episodes with phentolamine 1mg boluses. This is kept in the fridge in theatre 5 as 10mg in 1 ml, which I dilute to 10ml with normal saline. I use labetolol 5mg to treat tachycardia only (not hypertension) and the patients are invariably sensitive to this, with the heart rate slowing significantly often accompanied by a rise in BP (Now use 1mg as starting dose as less dramatic effects on heart rate. If already beta blocked pre-op may need larger doses). I have found the best cardiovascular stability comes from trying to avoid giving any vaso-active drugs as far as possible and tolerating a BP of 160 systolic. The more closely I have tried to control the blood pressure, the more it has tended to fluctuate. Lidco Rapid can be very useful to look at trends and at what happens if the blood pressure rises. A rise in SVV may also indicate IVC obstruction from kinking or direct surgical pressure. When the last draining vein has been clamped, the patient will often become hypotensive. This will often respond to fluid resuscitation (1000ml colloid typically following 2l crystalloid before this) a reduction in ET iso and if necessary noradrenaline infusion. If noradrenaline is used, it will often need to start at 1mcg/kg/min as insensitive due to alpha blockade. Almost invariably by the time the patient is awake, the noradrenaline will be switched off. Blood glucose will also need to be monitored. This is often raised intra-op due to circulating catecholamines, but falls dramatically after adrenalectomy. It will have frequently have halved by the time the patient reaches recovery and the may require dextrose infusion post-op to maintain it. The phaeos are usually drowsy and take a while to wake up (compared to the nonphaeo adrenalectomies). Thus I only give them 10mg morphine in theatre with iv paracetamol – I tend to avoid NSAIDs). The prone adrenalectomies tend to be less painful post-op, but the lateral ones may require a PCA. We have generally sent the patients to POSU, but a young, fit patient with no post-op blood pressure problems could go to the ward if necessary. There will however be the occasional patient who needs noradrenaline for a period of time post-op.