Evaluation of the risk of HBV transmission by organ , tissues and
advertisement

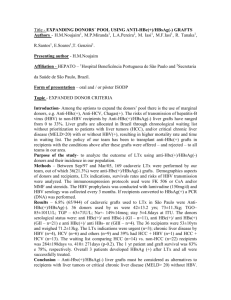
INFECTIVITY OF ORGAN, TISSUE AND CELL TRANSPLANTS IN THE PRESENCE OF SEROLOGICAL MARKERS OF HEPATITIS B VIRUS Challine Dominique1, Bouvier-Alias Magali1, Gourlain Karine1, Darthuy Françoise, Rémiré Jocelyne, Pawlotsky Jean-Michel1 1 Department of Virology and INSERM U635, Hôpital Henri Mondor, Créteil, France Prevention of hepatitis B virus (HBV) infection through organ, tissue or cell transplantation is principally based on the exclusion of donors with serological HBV markers. If HBs antigen (Ag) screening is performed universally, the need for systematically testing donors for antiHBc antibodies (Ab) and anti-HBs Ab is still debated, as well as the utility of HBV DNA testing to improve viral safety in transplantation. AIMS: To establish the potential infectivity of organ, tissue or cell grafts by seeking for HBV DNA in the blood of donors with serological markesr of HBV. METHODS: Among 11,155 organ, tissue and cell donations systematically tested in our laboratory between May 2000 and May 2004, 626 blood samples from 520 donors (106 were retested at day 90 after quarantine) were found to have at least one of three serological HBV markers: HBsAg, anti-HBc Ab, anti-HBs Ab (vaccinated donors with only anti-HBs Ab were excluded). All samples were tested for the presence of HBV DNA and HBV DNA was quantified by means of a highly sensitive real-time PCR-based assay, Cobas TaqMan HBV (Roche Molecular Systems; dynamic range of quantification : 6 to 1.1E8 international Units (IU)/ml, 1 IU/ml = 5.8 Cobas Taqman copies/ml). RESULTS : N HBsAg pos Recovery profile HBcAb Other HBcAb + HBsAb alone Brain-dead organ 199 17/20(85.0%) 0/121 2/53 2/5 (40.0%) donors (3.8%) Living organ donors 13 0/0 0/10 0/3 0/0 Tissue donors 165 2/2 (100.0%) 0/130 0/33 0/0 (excluding cornea) Stem cell donors 75 3/5 (60.0%) 0/61 0/9 0/0 Cord blood donors 56 2/2 (100.0%) 0/44 0/10 0/0 Cornea donors 118 1/8 (12.5%) 3/62 (4.8%) 2/21 1/27 (3.7%) (9.5%) (i) HBV DNA was detected in most HBsAg-positive donors (mean HBV DNA levels: 3.3, 2.5 and 2.0 log IU/ml, respectively). (ii) HBV DNA was rarely detected in HBsAg-positive cornea donors, suggesting false positive HBsAg detection. (iii) HBV DNA was never detected in patients with a recovery profile, except cornea donors. Among the 3 HBV DNA-positive cornea donors with this profile (HBV DNA: 1.5-3.2 log IU/ml), 2 had detectable HBsAg on initial determination not confirmed by neutralization. (iv) HBV DNA was detected in a significant number of donors with anti-HBc Ab only. (v) Two organ donors and one cornea donor with the 3 HBV markers were HBV DNA positive (mean HBV DNA: 3.5 log IU/ml). CONCLUSIONS: HBV DNA is detected in most HBsAg-positive organ, tissue and cell donors, but the level of replication is lower than in patients with chronic hepatitis B. (ii) HBV DNA can be detected in donors with anti-HBc Ab alone, reinforcing the need for systematic anti-HBc screening. (iii) HBV DNA is not detected in organ, tissue (except cornea) or cell donors with both anti-HBc and anti-HBs Ab, emphasizing the utility of systematic anti-HBs testing. (iv) Cornea donors, often sampled after death, may yield false-positive and falsenegative HBs Ag results. (v) Systematic HBV DNA testing in organ, tissue and cell donors appears useful to further improve viral safety in transplantation.