Item 4b - Hertfordshire County Council
advertisement

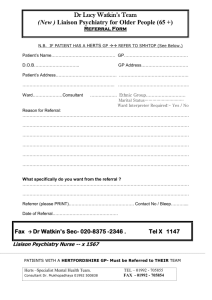
Appendix 9 West Hertfordshire Hospitals NHS NHS Trust SCRUTINY REPORT WEST HERTS and EAST and NORTH HERTS NHS TRUSTS 1. What are the arrangements in place within the relevant agencies to identify babies at high risk and could they be improved? All relevant organisations share a duty under Section 11 of The Children Act 2004 to ensure that their functions are discharged with regard to the need to safeguard and promote the welfare of children. Arrangements are in place within West Hertfordshire Hospitals NHS Trust and East and North Herts NHS Trust to identify the Unborn Babies who are potentially at risk. See Flow Chart. The midwife carries out a booking visit around 8 weeks gestation that obtains medical, obstetric and social history. Information from the GP is also obtained at this stage. Safeguarding training is given yearly to ensure that staff are competent in identifying possible triggers of increased risk to children whilst carrying out their assessments. 2. Once an agency identifies actual or potential significant harm to a young child what action is taken, what is the engagement of all relevant services and could this be improved? Automatic referral is done to Hertfordshire County Councils Children, Schools and Families Department (CSF) where there is domestic violence, drug and alcohol abuse, mental health problems and or learning disabilities. The named midwife also receives any domestic abuse alerts from the police and is then able to forward this information onto the midwife to follow up and make referral to CSF if necessary. A copy of any social information is then put into the mother’s hospital notes. Improvements need to be around the roll out of the introduction of and training to under take Common Assessment Framework (CAF) Assessments and identifying a lead professional. This was acknowledged as part the recent Hertfordshire Intensive Support Visit process as was the need to allocate additional time required to participate in the CAF assessment process. The midwives do not currently carry out CAF Assessments. As an alternative, midwives are asked to hold a multi agency professional meeting at approx 30 weeks gestation so a plan of care can be put in place. If a CSF referral has been made this is put onto an electronic system, which will alert staff if a woman is admitted. A copy of the relevant information also goes into the social file, which is on each ward area, including the Neonatal Unit. In East and North Herts a copy is placed into a confidential child protection folder held on the delivery suites. The midwives check this social file for every woman that is admitted into the maternity unit and have to document in notes that they have done this. See flow chart for further detail re multi agency working If the woman is booked at another hospital the Named Midwife or midwife will liaise with the Safeguarding Midwife at that hospital and fax any relevant information to them. If a woman presents without her notes or unbooked the staff will check the folder containing the out of area missing alerts from CSF. They will also phone the original hospital and if necessary childrens social services in the area where the woman has presented from. If a woman does not give any information the duty team at CSF is contacted and informed and a referral would be made. 3. What are the communication issues and are there any barriers that could be removed? The communication issues could be improved between CSF and health and other members of multi agency teams if midwives had access to their mobile numbers. A lot of time is spent trying to get updates from the relevant social workers. West Herts and the West CSF Team have recognised this and have recently commenced joint meetings between the managers at CSF and the Named Midwife so cases can be discussed and updated. We have also now invited the Named Nurses from Hertfordshire Community Health services (HCHS) to join this weekly meeting. East and North Herts have monthly maternity liaison professionals meetings, which a social worker attends and all cases are discussed and progressed. The named midwife then communicates any updates back to the midwife in charge of the case. A professionals’ telephone line within CSF would be an excellent resource to save having to try and contact social workers through the main call centre. This would also be beneficial if an urgent referral needed to be made quickly, or a case needed to be discussed urgently. 4. Once risks are identified and the child is on a protection plan, are the right agencies enagaged in assessing and improving parenting to reduce the risks? Teenage Mothers are offered parenting courses and have intensive parent craft sessions which are run by the teenage pregnancy midwives. West Herts have identified that a vulnerable adult midwife would be beneficial to the service via a business case to NHS Hertfordshire (PCT) and once this happens then more intensive parent craft classes could be undertaken with all vulnerable groups. There are concerns that mothers that have been identified as having learning difficulties and mental illness are often not seen as meeting the threshold for support. However although their learning disability/ mental illness may be considered “mild” there is no actual assessment on their ability to parent and it is often not until after the birth that the lack of ability becomes apparent. This needs to be addressed. There is a joint consultant obstetric and psychiatric clinic to review women with mental illness. In East and North a Consultant Obstetrician who has a special interest in mental health reviews them. West Herts has recently appointed a lead Obstetrician for perinatal mental health. There is also a joint Paediatric/Obstetric clinic to review clients with drug and alcohol use and plans are put in place for observing baby following birth. A plan of care is then formulated and put into the notes and any concerns re safeguarding relayed back to the Named Midwife who then informs CSF. In East and North Herts a monthly meeting to discuss psycho-social issues is held in the NICU, attended by Neonatal staff and the Named Midwife. Care plans for socially vulnerable babies are made. Prior to discharge meetings are held including CSF to plan for the discharge of the baby. 5. Would co-location of any of the professionals involved improve identification, assessment and management of risk? We have a significant population of vulnerable families and to have a social worker on site would enable assessments and planning to be carried out quickly if needed. The social worker could attend all the psychosocial meetings and would be aware of the families within the hospital. Sometimes if issues only become apparent in the postnatal period, they need to be risk assessed and managed very quickly to ensure a baby is kept safe from harm This would be much easier if a social worker was on site.