Perspectives in Nutrition, 8th Edition
advertisement

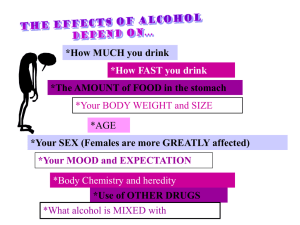
Perspectives in Nutrition, 8th Edition Chapter 8 Outline: Alcohol After studying this chapter, you will be able to: 1. Describe the sources of alcohol and the calories it provides. 2. Define standard sizes of alcoholic beverages and the term moderate drinking. 3. Summarize how alcoholic beverages are produced. 4. Outline the process of alcohol absorption, transport, and metabolism. 5. Define binge drinking and explain how it increases the risk of alcohol poisoning. 6. Explain how alcohol consumption affects blood alcohol concentration. 7. Describe guidelines for using alcohol safely. 8. Discuss potential benefits of using alcohol. 9. Summarize the risks of alcohol consumption. 10. Describe the effects of chronic alcohol use on the body and nutritional status. 11. List the signs of alcohol dependency and abuse. 12. Outline the methods used to diagnose alcohol abuse. 13. List the strategies and resources available for the treatment of alcoholism. 8.1 Sources of Alcohol A. General 1. Common sources vary in alcohol and calorie content (see Table 8-1) a. Beer b. Wine c. Distilled spirits d. Liqueurs e. Cordials f. Hard cider g. Ingredient in foods 2. Alcohol “proof” = twice the percentage of alcohol content 3. Standard drink provides ~15 g alcohol a. 12 ounces of beer b. 10 ounces of wine cooler c. 5 ounces of wine d. 1.5 ounce of hard liquor 4. Moderate alcohol intake a. 1 drink/day for women b. 2 drinks/day for men B. Production of Alcoholic Beverages 1. Carbohydrate-rich foods are fermented by yeast, which convert simple sugars (e.g., glucose or maltose) to alcohol and CO2 at room temperature a. 2. 8.2 Malting is the process of allowing grain to sprout, which produces enzymes that break down starch to simple sugars b. First stage of fermentation is aerobic; yeast cells multiply and produce small amount of alcohol c. Second stage of fermentation is anaerobic d. Fermentation ceases when alcohol content inactivates yeast Alcohol maybe distilled by boiling and condensation to separate it from water and concentrate it; used to produce hard liquor Alcohol Absorption and Metabolism A. Alcohol Absorption 1. Requires no digestion 2. Requires no specific transport mechanisms or receptors to enter cells 3. Rapid absorption by simple diffusion a. Stomach b. Small intestine 4. Rate of alcohol absorption is influenced by types and amounts of foods consumed a. Empty stomach leads to rapid absorption b. High fat meal slows absorption 5. Alcohol is dispersed wherever water is distributed in the body a. Higher lean body mass dilutes alcohol concentration b. Dehydration increases alcohol concentration 6. Alcohol diffusion through cell membranes causes damage to membrane proteins B. Alcohol Metabolism 1. Alcohol cannot be stored; takes priority in metabolism as a fuel source 2. Metabolic pathways a. Alcohol dehydrogenase (ADH) pathway metabolizes majority (90%) of alcohol consumed at low or moderate levels i. Alcohol dehydrogenase converts ethanol to acetaldehyde (toxic) ii. Aldehyde dehydrogenase converts acetaldehyde to acetyl-CoA (yields energy or stored as fat) iii. Cells lining stomach metabolize 10 - 30% of alcohol via ADH pathway iv. Liver is primary site for alcohol metabolism b. Microsomal ethanol oxidizing system (MEOS) helps to metabolize excessive amounts of alcohol i. Liver treats alcohol as foreign substance ii. Also used to metabolize drugs and toxins; because alcohol metabolism takes first priority, use of MEOS for alcohol metabolism may increase risk for drug toxicities iii. Like ADH pathway, produces acetaldehyde and then acetyl CoA, but requires energy to function iv. 3. 4. 5. Increasing efficiency of MEOS with repeated exposure to alcohol contributes to alcohol tolerance: increasing amounts of alcohol are needed to produce a desired effect c. Catalase pathway i. Minor contributor to alcohol metabolism ii. Takes place in liver and other cells ADH, MEOS, and catalase pathways metabolize nearly all alcohol consumed; small percentage is excreted through lungs, urine, and sweat Factors Affecting Alcohol Metabolism a. Ethnicity i. People of Asian descent have normal to high ADH activity, but very low aldehyde dehydrogenase activity; buildup of acetaldehyde leads to flushing, dizziness, nausea, headaches, rapid heartbeat, and rapid breathing b. Gender i. Women produce less ADH in cells of stomach lining, leading to 30 - 35% more alcohol absorption from stomach directly into bloodstream ii. Smaller body size and higher body fat content of women leads to greater concentration of alcohol in blood and other tissues c. Age: enzymes of ADH pathway decline with age d. Alcohol content of beverage e. Amount of alcohol consumed f. Usual alcohol intake Rate of Alcohol Metabolism a. Social drinker, 150 lbs, normal liver function: metabolizes 5 - 7 g alcohol/hour (1/2 drink) b. When rate of alcohol consumption exceeds liver’s metabolic capacity, BAC rises and symptoms of intoxication appear (see Figure 8-1) c. BAC determined by measuring amount of alcohol excreted by the lungs, which is directly related to BAC (breathalyzer test) d. Acute alcohol intoxication (alcohol poisoning) can cause respiratory failure, aspiration of vomit, and death i. Confusion, stupor ii. Vomiting iii. Hypoglycemia iv. Severe dehydration v. Seizures vi. Slow or irregular breathing and heartbeat vii. Blue-tinged or pale skin viii. Hypothermia ix. Unconsciousness 8.3 Alcohol Consumption A. Statistics 1. 62% of North American adults consume alcohol a. 42% are light drinkers (≤3 drinks/week) b. 14% are moderate drinkers (7 - 14 drinks/week) c. 4.8% are excessive drinkers (>7 - 14 drinks/week) 2. 38% abstain from drinking B. Drinking on college campuses 1. Young, white college students are largest drinking population in North America 2. Many drinkers are not of legal drinking age 3. Considered “rite of passage” into adulthood 4. Advertising targets college students 5. Young drinkers may be unaware of the harmful acute and chronic effects of alcohol 6. Binge drinking: 4 or more drinks/occasion for females; 5 or more drinks/occasion for males a. Associated with other problems (see Table 8-5) i. Vandalism ii. Violent crime iii. Traffic accidents and injuries iv. Sexual abuse v. Suicide vi. Hazing deaths vii. Serious acute health risks viii. Poor habits contribute to lifelong problems b. Rate of alcohol dependence is 9% among young adults, compared to 4% among general adult population c. Underage drinkers are more vulnerable to alcohol’s damaging effects and are at much greater risk of alcoholism in adulthood 8.4 Health Effects of Alcohol A. Guidance for Using Alcohol Safely 1. Non-drinkers should not start consuming alcohol because risks often outweigh benefits, but moderate alcohol has some benefits 2. Dietary Guidelines for Americans a. Drink alcohol sensibly and in moderation (up to 1 drink/d for women; up to 2 drinks/d for men) b. Some individuals should not consume alcohol i. Unable to restrict alcohol intake ii. Women of childbearing age who may become pregnant iii. Pregnant and lactating women iv. Children and adolescents v. Use of medication that interacts with alcohol vi. B. C. Certain medical conditions c. Alcoholic beverages should be avoided by individuals engaging in activities that require attention, skill, or coordination Potential Benefits of Alcohol Intake 1. Reduced anxiety and stress 2. Stimulation of appetite among elderly adults 3. Lowered risk of cardiovascular disease and overall mortality; may be due to resveratrol in red wine a. Decreased LDL b. Increased HDL c. Decreased platelet aggregation 4. Reduced risk of type 2 diabetes 5. Reduced risk of dementia Risks of Excessive Alcohol Intake 1. Excessive alcohol consumption contributes to 5 of 10 leading causes of death in North America a. Heart failure b. Cancer c. Cirrhosis d. Motor vehicle and other accidents e. Suicides 2. Figure 8-2 summarizes effects of excessive alcohol on body a. Impaired brain function; brain damage b. Vasodilation and flushing of skin c. Cancer of the oral cavity, throat, larynx, and esophagus (particularly in combination with smoking) d. Heart muscle damage and resulting heart failure e. Breast cancer f. Irritation of the stomach lining and stomach cancer g. Fatty infiltration of the liver, alcoholic hepatitis, cirrhosis, ultimate liver failure h. Impaired pancreatic function, hypoglycemia, pancreatic cancer i. Malabsorption of nutrients in the small intestine j. Abdominal fat deposition and fluid accumulation (ascites) k. Cancer of the colon and rectum l. Osteoporosis m. Intestinal bleeding n. Depressed immune function o. Sleep disturbances p. Impotence q. Abdominal obesity r. High blood triglycerides 3. Cirrhosis of the Liver a. D. Roles of liver i. Nutrient storage ii. Protein and enzyme synthesis iii. Metabolism of protein, fats, and carbohydrates iv. Detoxification v. Drug metabolism b. Progression of alcohol-induced liver disease i. Steatosis (fatty liver); usually reversible ii. Alcoholic hepatitis (inflammation of liver cells), leading to nausea, poor appetite, vomiting, fever, pain, and jaundice; usually reversible iii. Cirrhosis (loss of functioning hepatocytes) leading to decreased production of blood proteins, ascites, and poor nutritional status; irreversible c. Statistics i. 50% chance of death within 4 years without liver transplant ii. Cirrhosis develops in 10 - 15% cases of alcoholism iii. Commonly associated with drinking equivalent of 7 beers/d, but may be less, especially for women d. Susceptibility to cirrhosis i. Amount of alcohol consumed ii. Duration of alcohol consumption iii. Genetic factors iv. Obesity v. Diabetes vi. Exposure to hepatotoxins vii. Iron overload disorders viii. Infections with hepatitis e. Mechanisms for liver damage i. Increased concentration of acetaldehyde may damage liver ii. Accumulation of fat in liver cells causes inflammation and cell damage iii. Increased production of free radicals f. Impact of nutritional status i. Even with nutritious diet, alcoholism still causes liver damage ii. Nutrient deficiencies increase vulnerability of liver to toxicity Effects of Alcohol Abuse on Nutritional Status 1. General a. Alcohol abusers tend to replace some or all of food with alcohol, a poor source of nutrients b. Protein-energy malnutrition can result c. Micronutrient deficiencies result from poor intake and impaired absorption or metabolism of nutrients 2. E. Water-Soluble Vitamins a. Thiamin deficiency (Wernicke-Korsakoff Syndrome): alcohol is a poor source of thiamin i. Irreversible paralysis of eye muscles ii. Loss of sensation in lower extremities iii. Loss of balance with abnormal gait iv. Memory loss b. Niacin deficiency: alcohol metabolism requires large quantities of niacin c. Vitamin B-6 deficiency: alcohol metabolism increases urinary excretion of vitamin B-6 i. Increased risk of anemia ii. Peripheral neuropathy d. Vitamin B-12 deficiency: excessive alcohol intake can impair absorption of vitamin B-12 e. Folate deficiency 3. Fat-Soluble Vitamins a. Vitamins A, D, E, and K: chronic alcohol abuse damages liver and pancreas, which impairs secretion of bile and pancreatic lipases b. Vitamin A: alcohol abuse decreases liver’s rate of breakdown and excretion of vitamin A and decreases liver’s production of the protein that transports vitamin A throughout the body; deficiency may lead to night blindness c. Vitamin K: decreased ability to synthesize vitamin K-containing compounds for blood clotting d. Vitamin D: decreased ability of liver to convert vitamin D to active form; increased risk for osteoporosis 4. Minerals a. Calcium: low intake and poor absorption due to decreased ability of liver to convert vitamin D to active form b. Magnesium: increased urinary excretion; leads to tetany c. Zinc: decreased absorption and increased urinary excretion; leads to changes in taste and smell, loss of appetite, and impaired wound healing d. Iron: damage to gastrointestinal tissues causes bleeding and poor iron absorption Alcohol Consumption during Pregnancy and Breastfeeding 1. Pregnancy a. Slows nutrient and oxygen delivery to developing fetus; retards growth and development, especially in first trimester, when organogenesis occurs b. Alcohol displaces nutrient-dense foods in maternal diet c. 30 of 1000 births are affected by alcohol consumption during pregnancy d. Within minutes of consumption, alcohol reaches fetus through maternal blood supply 2. 8.5 i. Small size ii. Immature metabolism e. Fetal alcohol syndrome (see Figure 8-4) i. Facial malformations ii. Growth retardation (e.g., low height, weight, and head circumference) iii. CNS defects (e.g., mental retardation, small brain size) f. Fetal alcohol effects i. Behavioral problems ii. Learning difficulties (e.g., short attention span, hyperactivity) iii. Nervous system abnormalities g. No safe level of alcohol consumption during pregnancy is known h. Women planning pregnancy should avoid alcohol because first trimester, when many women do not know they are pregnant, is time of highest vulnerability Breastfeeding a. Reduces milk production b. Decreases infant milk consumption c. Leads to disrupted sleep patterns for infant d. Alcohol consumption is not advised for breastfeeding mothers, but if consumed, limit amount and wait 3 - 4 hours before breastfeeding Alcohol Use Disorders: Alcohol Abuse and Alcoholism A. General 1. Alcohol abuse (at least one of the following) a. Failing to fulfill major responsibilities at work, school, or home b. Drinking when it is physically dangerous (e.g., driving) c. Having recurring alcohol-related legal problems d. Having social or relationship problems that are worsened by alcohol intake 2. Alcohol dependency (alcoholism) a. Craving b. Loss of control c. Withdrawal symptoms (e.g., nausea, sweating, anxiety, shaking) d. Tolerance e. Unsuccessful attempts to cut down on alcohol use 3. Statistics a. 1 in 3 Americans abuses or becomes dependent on alcohol over a lifetime b. 8.5% of US population meet criteria for alcohol abuse or dependence c. 30% of US population is at high risk of developing alcohol-related problems B. Genetic Influences 1. 2. C. D. E. F. 8.6 Account for 40 - 50% of risk May be due to genetic polymorphisms of enzymes of alcohol metabolism, antioxidant enzymes, neurotransmitters or receptors, or immune factors 3. Those with family history of alcohol dependence should be alert for early signs Effect of Gender 1. Men are at higher risk for alcohol dependency: 4 male:1 female 2. Women are more susceptible to adverse effects of alcohol due to smaller size, lower body water content, and lower alcohol dehydrogenase in stomach a. Liver disease b. Heart muscle damage c. Cancer d. Brain injury Age of Onset of Drinking 1. Underage alcohol consumption contributes to 4500 deaths/year in US 2. 45% of youth who drink before age 14 develop alcohol dependence, compared to 10% of those who delay drinking until after age 21 3. 40% of high school youth report current alcohol consumption Ethnicity and Alcohol Abuse 1. High use a. Native American Indians i. High rate of motor vehicle accidents and unintentional injuries due to alcohol ii. High rate of alcohol-related suicide and domestic abuse iii. High rate of fetal alcohol syndrome b. Alaska Natives c. Native Hawaiian 2. Low use a. Asian Americans i. Uncomfortable side effects from low aldehyde dehydrogenase activity Mental Health and Alcohol Abuse 1. Alcohol abuse may aggravate or cause depression or anxiety disorders 2. People with mental health disorders may seek alcohol to self-medicate 3. Majority of suicides and interfamily homicides are alcohol-related Medical Perspective: Diagnosis and Treatment of Alcoholism A. 2-phase problem 1. Problem drinking 2. Alcohol addiction B. Signs of alcoholism (in addition to those listed in section 8.5) 1. Alcohol odor 2. Flushed face 3. CNS disorders (e.g., tremors) 4. 5. 6. 7. C. D. Unexplained work absences Frequent accidents Falls or injuries of vague origin Laboratory tests a. Impaired liver function b. High triglycerides c. High uric acid concentration Determining Whether a Problem with Alcohol Intake Exists 1. CAGE questionnaire (1 or more positive responses) a. C: Have you ever felt you ought to cut down on drinking? b. A: Have people annoyed you by criticizing your drinking? c. G: Have you ever felt bad or guilty about your drinking? d. E: Have you ever had a drink first thing in the morning (eye-opener) to steady your nerves or get rid of a hangover? 2. Other questions for health professionals to ask a. Development of tolerance b. Memory lapses c. Continued drinking despite health problems d. Withdrawal symptoms e. Taking part in high-risk behaviors when under the influence of alcohol f. Alcohol-related trouble at work, school, home, or in relationships with others g. Need alcohol to get through day or unwind, to cope with stressful events, or escape from ongoing problems 3. Michigan Alcohol Screening Test (MAST) is another tool to diagnose alcoholism 4. 75% of those with alcohol problems do not seek treatment Recovery from Alcoholism 1. Behavioral therapy a. Identify ways to compensate for the loss of pleasure from drinking b. Total abstinence is the ultimate objective c. Co-existing mental health disorders must be treated 2. Medication a. Naltrexone (ReVia): blocks craving for alcohol and pleasure of intoxication b. Acamprosate (Campral): acts on neurotransmitter pathways to decrease desire to drink c. Disulfiram (Antabuse): causes physical reactions (e.g., vomiting) with alcohol consumption 3. Self-help programs a. Alcoholic Anonymous b. Al-Anon for friends and family members 4. Recovery rates are 60% or higher for job-related alcoholism treatment programs 5. Successful recovery depends on early detection and intervention