Health Psychology – Cardiovascular Disease
advertisement

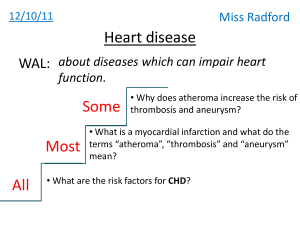
Health Psychology – Cardiovascular Disease What is cardiovascular disease? Cardoivascular system pumps blood through the body, providing a rapid transport system for oxygen, nutrients, and disposal of wastes. Cardiovascular system = heart and the blood vessels. By contracting and relaxing, heart muscle pumps blood that circulates the body. Circulation of blood allows transport of oxygen to body cells and removal of carbon dioxide and other waste from cells. Entire circuit takes about 20 minutes when body at rest. Heart = 4 chamber muscular pump circulating blood. In healthy adult heart rate of 45 to 60 beats per minute. A large increase in cardiac oxygen requirement met by increase in coronary blood flow. Strenuous exercise. Blood travels from right ventrile of heart to the lungs where heamoglobin becomes saturated with oxygen. From lungs, the oxygenated blood travels back to the left atrium of the heart, then to the left ventricle and finally out to the rest of the body. The arteries carry oxygenated blood, which branches into smaller diameter called arterioles and finally in capillaries (tiny that connect arteries and veins). Oxgen diffuses out to body cells, and carbon dioxide and other chemical wastes pass into blood to be disposed of. Blood that has been stripped of oxygen returns to the heart by way of a system of veins (beginning with tiny venuoles and ending with two large veins that empty into the right atrium, the upper right chamber of the heart. Blood supply to the heart muscle, or the myocardium, by coronary arteries. Aorta – the main artery that carries oxygenated blood from the heart. Left and right coronary arteries divide into smaller branches, provide blood supply to the myocardium. With each beat, heart makes a slight twisting motion which moves coronary arteries. Problems – Cardiovascular Disorders 1. Ateriosclerosis = loss of elasticity of arteries … “hardening of the arteries”. Beating of heart pushes blood through arteries, great force and elasticity necessary. Loss of elasticity makes cardiovascular system less capable of tolerating increased in cardiac blood volume. 2. Atherosclerosis = formation of fatty plaques (plaque consists of cholesterol and other lipids, cell debrit and other substances.) on inner lining of artery walls. Plaques grow and calcify into hard bony substance that thickens the artery walls. Resulting occlusion of the arteries. These two often occur together. When coronary arteries affected, heart oxygen supply might be threatened. 3. Coronary heart disease. Is the result of atherosclerosis and ateriosclerosis in coronary arteries (arteries that supply the heart muscle itself). No outward sign. Build up and person unaware. If coronary arteries become narrowed, 1 insufficient blood reaches heart muscle. Restriction of blood flow is called ischemia. Heart deprived of oxygen wont flow properly. One result of temporary/partial deprivation is experiences as severe pain, called angina pectoris. Usually precipitated by exercise or strain (ie extra demands). Rarely lasts more than a few minutes. Relieved by “angenine” which dilates coronary arteries. Most likely to occur on a Monday. A complete blockage of either coronary artery results in death of myocardial infarction, or heart attack. Tissue dies and disrupts heart beat. Feelings of weakness, dizziness, nausea, difficulty breathing, crushing pain in the chest, arms or maybe rapid loss of consciousness and death. People who survive (about half), damaged portion of heart wont regrow or repair, usually get scar tissue which doesn’t have normal elasticity so reduces normal heart capacity and functioning. 4. Stroke. Cardiovascular accident. Atheriosclerosis and arteriosclerosis can also affect arteries that serve head, neck and into brain. Again may be blockage to an area of the brain. Oxygen deprivation causes death of brain tissue within 3 to 5 minutes – stroke. (other causes of stroke include blood clots, bubble of air - air embolism, ruptures. (aneurism – sac formed by weakening of artery wall then bursting). 5. Hypertension (high blood pressure). Heart pumps blood, considerable force to get around the system. Narrowing of arteries and loss of elasticity tent raise blood pressure (pressure = force/area). And make cardiovascular system less capable of coping with demands of exercise and stress. Systolic pressure = pressure generated by heart contraction Diastolic pressure = pressure between contractions, reflects elasticity of vessel walls. Abnormally high blood pressure – “silent” illness and is single best predictor of both heart attack and stroke. Essential hypertension has no particular cause. Indeed, blood pressure, is most common measure of cardiovascular function. Can also measure electrical activity of the heart (ECG). Can see abnormalities is resting heart beat, but can’t show build up of plaque. Measurement of heart’s electrical activity (ECG) during exercise is called the stress test. (better for discovering coronary artery blockage, walking or treadmill up a slope or bike with increasing pedal resistance). Exercise increased body’s demand for oxygen and heart increases its action. If coronary arteries partially blocked, blood cannot be delivered fast enough to keep up with increased demand. Restriction results in characteristic pattern of electrical activity. Most accurate measurement of cardiac function is cardiac catheterization or angiography. Heart is injected with a dye (by catheter threaded inserted into the femoral artery and up though the circulatory system to the heart). Heart pumps dye into coronary arteries and x-ray can see extent of blockage. Usually awake, uncomfortable procedure and people very anxious (mortality rate .2% or 2 in a 1000). 2 Surgical interventions. 1. Coronary bypass – veins from leg used to bypass blocked sections of arteries 2. Angioplasty – catheter with inflatable tip inserted into obstructed artery and tip is inflated. Catheter flattens fatty deposits and therefore improves circulation. Risk factors for CHD Alameda county study, Framingham Heart Study (Brown, 1988, Dauber, 1950) popularized notion of “risk factors”. Large-scale epidemiological study began in 1948, more than 5000 men and women (5208) in the town of Framingham, Massechusets. Risk factors = variable associated with disease, not cause nor mechanism, but can determine probability that a person will develop a disease. Prospective design – all people free of heart disease at beginning of the study. Original plus follow over 20 years, study has now continued for 50 years with over half of the original participants dead. Not precise prediction, cigarette smoking 2 x as likely to develop/die of heart disease than if you don’t, on population basis. Well over 2000 characteristics of individuals or societies have been identified as risk factors for CHD. All known together account for less than half newly diagnosed cases of CHD. Inherent Risk Factors (non-modifiable). Inherent risk factors result from your genetic or physical conditions that cannot be changed through modification of lifestyle (nonmodifiable risk factors). 1. Age. Older people more likely to develop heart disease (risk increases with age). Not because aging causes CHD, but because of the the years deposits of cholesterol have more opportunity to build up in blood vessels. Risk of MI doubles with each decade of added age. Average age of men with first MI is approximately 55 years, but mean age of first MI for women is 65 years. 2. Family history. More likely to die of heart disease, heritibility, not simple action of a pair of genes. 3. Gender. Men more likely at all ages, most notably, male death rate 5.3X higher than female death rate for the 35-59 age group. (little research on women) 4. Ethnicity/Ethnic background. In US, African Americans at increased risk. In Australia, CHD mortality rates about 2x among Aboriginal people. European and Asian immigrants lower age of mortality than people born is Oz. Can’t change, but people with identified risk factors can minimize their overall risk profile through behaviour management and adjustments to lifestyle. 3 Physiological conditions / risk factors. 1. Hypertension. Common rule of thumb = systolic blood pressure about 140 and diastolic blood pressure about 90. Hypertension has no overt symptom – but indicates that heart is working harder than normal (heart may become enlarged).. High blood pressure can result in hardening or artery walls and is a major risk factor for MI, stroke, and kidney disease. 85% of cases, no known cause – essential hypertension. Framminham study, high blood pressure risk for heart disease (obesity best predictor of hypertension) – sodium seems to be critical determining factor. Serum cholesterol level. Level of cholesterol circulating in the blood stream. Cholesterol is a waxy, fatty substance essential for human life. Is a compound of cell membrane etc, liver manufactures cholesterol and comes from diet. But high levels of cholesterol are dangerous. Frammingham study also determined, total cholesterol not best predictor. Low-density lipoprotein (LDL) related to heart disease (“bad” cholesterol) but high-density lipoprotein (HDL) negatively related (ie protective, good cholesterol). When too much LDL in blood, cholesterol may be deposited on artery walls, whereas HDL retrieve and transport to liver for disposal... Ratio important – 2 behaviours related to elevated HDL (moderate alcohol consumption and exercise). Lower LDL and high % calaries for saturated fats (red meat, whole milk, eggs), relatively difficult to change by diet or drugs by more than 20-25%. Lifestyle factors … Smoking. Most important modifiable risk factor for CHD. People who smoke are 2x more likely to contract heart disease. Smoking changes composition of the blood. Chun, Dobson, and Heller (193) male smokers 2.9x female and 3.5x male more likely to suffer an MI than nonsmokers were. Stopping smoking may have greatest effect in reducing cardiovascular risk than changes in any other risk factor. Smoking increases autonimic activity, affects serum cholesterol levels and clotting of blood. Physical inactivity (Paffenbarger, 1985). Slow or reverse atherosclerosis, reduce incidence of arrhythmia, and or reduce hypertension. Meta-analysis – regular moderate physical activity is associated with lower CHD risk. Regular exercise increased cardiopulmonary efficiency, exercise affects serum cholesterol and hypertension. Obesity. Risk factor for CHD puzzling. Australians are fatter than ever before, over 40% are obese or overweight, but CHD mortality rates have fallen. Unlikely to be an independent risk factor for CHD, but is risk factor for hypertension. Diet. Body weight, sodium intake – blood pressure. Also cholesterol. 4 Psychological Risk Factors 1) Workforce Status. Unemployed men increased change of sudden cardiac death than employed. Occupational prestige. As occupational prestige increases, risk of CHD decreases among men (25 to 54 years) Walws and Bennet, 1995). CHD affects poorest groups in wealthy countries. 2 longitudinal studies (Marmot, 194, and Marmot and Mann, 1996), male british civil servants, lower grade clerical workers had lifestyles with pooper diets and less exercise than administrators. Job-demand hypothesis. Karaseck in the 1980s and early 90s. Jobs with high levels of psychological demand but low decision control (eg fire fighter) tend to have higher rates of CHD than less demanding jobs. Stress – increased heart beat, strengthening contractions, release of hormones, raises blood pressure. When stress chronic, cumulative effect over time can be excessive wear on cardiovascular system. 2) Personality. Type-A behaviour pattern. Most extensively studies risk factor for coronary heart disease. Cardiologists, Friedman and Roseman (1959) initially defined Type A in terms of excessive competitiveness, impatience, hostility, vigorous speech, and time urgency. Type B behaviour pattern, lower levels of competitive drive, more relaxed, less hostile. Initial evidence of relationship between Type A behaviour and CHD in 2 large scale epidemiological studies in 1960s and 1970s. In Western Collaborative Group Study, > 3000 healthy men, 39-59 years, followed for 8.5 years. Structured interview at beginning for Type A behaviours. After 8.5 years, Type A 2x more likely to develop clinically significant CHD than Type Bs. Difference remained even after statistically controlling for smoking, blood pressure, and cholesterol levels (Rosenman, 1975). Frammingham Heart Study (45-77 year old men and women). At beginning > 1600 questionnaires. After 8 years, Type A women 2x more likely to develop CHD and 3x more likely to experience angina pectoris than Type B. Type A men 2x more likely for both. Framington Type A Scale 1) I want to be the best at everything 2) I can be described as domineering 3) I like to compete 4) I eat too quickly 5) I often feel stressed 6) I have often thought about work after work 7) I feel mentally and physically exhausted after work 8) I get impatient when I have to wait 9) I have often felt stressed at the end of the working day 10) I have often felt uncertain, worried, and dissatisfied with how well I have accomplished my tasks at work. 5 More studies in 1980s, Type A still considered risk factor for CHD. However, later studies less so. Particularly those in populations already at risk for CHD (eg smokers). Discrepancy may be due to population vs samples. May also be due to measures. 1. Friedman and Rosennan developed the Structured Interview. Person asked about characteristic ways of responding to situations involving potential impatience, competitivementt and hostility. Also assess interviewee’s responses to challenges in the interview and aspects of expressive style (eg vocal speed, volume, and explosiveness – types and categories) 2. Self-report questionnaires. Jenkins activity survey (JAS) developed in 1971, based on structured interview, consists of 52 items. Reliably differentiate type As and Bs on SI in WECS. Other shorter measures (continuum, strong A to strong b, but most in between). Meta-analyses (Booth-Kewley and Friedman, 1987) show more consistent results for SI than JAS. 3. What is Type A? Conceptually a global set of traits. Later studies make it clear it actually involves several components. Suggests may be one toxic element. Mechanisms for a relationship between Type A and CHD. Not sure, best evidence. Type As respond differently to stress, at both psychological and physiological level. Specifically, Type As appraise challenging situations as more stressful. More involvement in competitive games, deny and suppress aversive emotions, evaluate their task performances more harshly. Type As appear to show physiological hyperactivity in response to stress. Ie show greater change in heart rate blood pressure, and hormone levels (catacholamines and corticosteroids) than Type Bs. Since 1980, prospective studies of relationship between Type A and CHD have been negative. Moreover, more recent re-analyses of Western Collabrative Group Study found no association between Type A and CHD at 8.5 or 22 year follow-up (Rogland and Brown, 1988). In Framingham study, further follow-up showed Type A men and Type B had almost identical rates of MI. Allen (1998). Type A Behaviural Pattern may have been typical of middle-aged, middle-class males in a particular historical period. Between 1950s and 1980 this group was also very likely to develop CHD”. Hostility. Separate out components of Type A, show hostility most consistent relationship to CHD (Booth-Kewley and Friedman, 1987; Rhodewalt and Smith, 1991). Global Type A is not a risk factor for coronary heart disease. 6 1980s Ted Dembroski and associates suggested “hostility”. Williams (1989) specific element of hostility – cynical hostility – especially harmful. People who mistrust others, think the worst of humanity. Several measures of hostility. Most common is the Cook-Medley, which measures suspiciousness, resentment, frequent anger, and cynical mistrust of others. Found hostility better predictor of heart disease and all cause mortality than Type A behaviour. Chesnet et al (1988) hostility strongest correlate of physiological hyperreactivity. Hostility/Disagreeableness: 1) 2) 3) 4) 5) Once in a while I cannot control my urge to harm others I can’t help being a little rude to people I don’t like When someone makes a rule I don’t like I am tempted to break it Other people always seem to get the breaks I commonly wonder what hidden reason another person may have for doing something nice for me 6) I can’t help getting into arguments when people disagree with me 7) Unless someone asks in a nice way, I won’t do what the person wants 8) My motto is “never trust strangers” 9) Whoever insults or my family is asking for a fight 10) If somebody annoys me, I am apt to tell him what I think of him Niaura et al., 2002 – Men who are in the higher 80% in hostility are much more likely to develop CHD than those who are lower in hostility. But hostility is related to other risk factors (age, gender, low SES). Indicate may not be an independent risk factor, but work because associated with these other things. Several large scale more recent studies (80 and 90s) have failed to replicate earlier findings [see notes for copy of hostility questionnaire]. Narrower to specific components of hostility – cynicism and expresse danger better predictors of heart disease and death than global concept of hostility (anger out not anger in). Expressions of anger increase cardiac reactivity (in men but not women). Sufficient research indicates that both the expression and suppression of anger may be potentially unhealthy. Siegman (1993) people learn to recognize anger, but express it calmly and rationally. Research evidence not unanimous, does suggest that hostility, defined as the physical and or verbal expression of anger, may be a behavioral risk factor for the development of cardiovascular disease. Personality factors not a strong risk as traditional risk factors (eg smoking, hypertension, high cholesterol levels). Risk factors interact, so a person with more risk factors more vulnerable to CVD than a person with only one. 7 3) Social Support Marital status linked to likelihood person will die of heart disease. Greater deaths for single, divorced or widowed. Married also more likely to survive after a heart attack. 4) Psychological stress. Role of stress of hotly debated. Some argue occupations stress increases CHD, others disagree. But stress may trigger MI in people already affected. Dobson et al (1991) effect of Newcastle earthquake. Found 6 fatal heart attacks during earthquake period, slight increase on what expected during same time period. (very old people seem to die on their birthday celebrations). Emotional stress popularly believed to be involved in cardiac arrest. Acute and Chronic Risk Factors As you may know cardiac events are often triggered by specific events (person gets excited, overexerts themselves physically, something stressful happens, fit of anger … basically things that put extreme stress on heart). Therefore, the chance of having a cardiac event (myocardial ischemia, myocardial infarction, arrhythmia) combination of acute and chronic risk factors. The next figure shows how the risk factors combine. Threshold for a clinical cardiac event. 8 Modifying Risk Factors Changing behavioral risk factors Talked about in our lectures on health behaviors (smoking, diet, alcohol, etc). Example of an exam question that might ask you to integrate information from 1st and 2nd half of the lecture series. 1. Tobacco smoking – talked about previously 2. Hypertension – Drugs, no symptoms, number of side-effects, low compliance. 3. Cholesterol levels. Drugs cost money and have side effects. Dietary modification, low cholesterol seems to decrease heart disease in men (but not women). Diets low in fatty food help maintain healthy cholesterol levels, but once elevate, total cholesterol levels are resistant to change. Use drugs to get down, institute life changes and then can keep off medication. Multiple factor intervention trials for prevention of CHD have produced mixed results. Large trials (eg WHO collaborative trial) and MRFIT (Multiple Risk Factor Intervention Trial) altered risk factors but did not reduce CHD. WHO (1986) 60 881 men 40-59 years for 6 years follow-up. No difference on CHD or overall mortality. MRFIR (1982) 12866 high risk US men. Intervention 7 years. Risk factors declined for special intervention group, but CHD mortality did not differ. Cardiac rehabilitation Psychology has a role to play in CHD by 1. Predicting and changing behavioural risk factors 2. Rehabilitation of sufferers MI – half people die, if survive first few days, rest (hospitalization in coronary care unit), return home to long road to recovery. Need to cut down on activities and lack physical stamina. Goal of cardiac rehabilitation help patients reach optimal physical, medical and psychological status. Education – told what to expect, what symptoms might occur, medications, placed on low salt/cholesterol diets, told to quit smoking (only 30-40% do), lose weight, training and supervision in an exercise program, walking, cycling, (30 minutes 3x per week). Exercise can improve self-concept, quality of life in general, adherence, ½ quit exercising within first 6 months. High initial levels of anxiety and depression. Encourage to go back to work/support groups. Stress management, sexual functioning (people afraid), strong social support. People who have had a heart attack. Friedman and Ulmer (1984). People who suffered from a heart attack to standard rehabilitation and group therapy oriented toward changing Type A behvaiours. End of 3rd year, therapy changed behaviour and reduced number of heart attacks. Decreased risk for heart attach recurrence by half. 9