Negotiating the Politics of Integrated Disability Management
advertisement

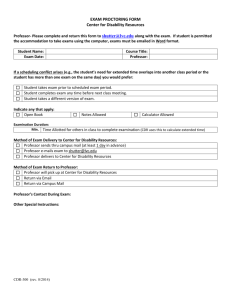
Negotiating Disability: The Politics of Integrated Disability Management * Kenneth Mitchell, Ph.D. UnumProvident Corporation Chattanooga, TN “Disability is subjective and depends ” Integration, Coordination or Segmentation? At the core of the integrated disability management (IDM) process is the notion of negotiated disability. An extensive research record has demonstrated that work disability is subjective and depends on many factors. For example, the employer’s ability or willingness to accommodate the employee’s impairment can extend or shorten the duration of lost time. For some individuals, the injury or illness arrives at a critical juncture in their career or work performance. The employee’s corresponding motivation to stay off work or return to work in a timely manner plays a critical role. Corporate policies define the organizations’ expectations regarding lost time and application of resources. Likewise, supervisors and managers within the organization determine priorities and the overall effectiveness of the strategies applied to reduce the impact of lost time. There needs to be continuity between these two critical drivers within the disability management process. State worker’s compensation statutes and private disability benefit plans are negotiated to define the eligibility e and the appropriate compensation to be paid. Negotiated health insurance and managed care plans define the degree of accessibility of care, the duration of treatment and the desired providers. Empirically, we understand that impairment does not equal disability. Impairment is objective. Disability is subjective. Therefore, disability may and can be negotiated. As an employer begins to consider the integration of the various income replacement, claims administration and lost time management initiatives, effective negotiation of disability begins. As the definitions of disability are negotiated, so is the manner in which disability is managed. Disability is negotiated at two levels. One is at the corporate level, creating the disability management model. The other is at the individual employee level. The initial corporate negotiation step determines the degree of program segmentation, coordination or integration that may exist. Unfortunately, the negotiation is not active or even formal. The disability management process is created in an unsystematic fashion, evolving over time, maintained by habit and successful by luck. * This article was prepared from the presentation made by Kenneth Mitchell, Ph.D. to the New England Chapter of the Disability Management Employer Consortium, Waltham, Massachusetts, September 5, 2001 Negotiated Disability – Page 1 Figure 1 illustrates a disability integration continuum for an organization. The continuum can have different degrees of fragmentation, disability migration, segmentation, coordination and ultimately, some form of integration. Some organizations move through the continuum or become fixed at a particular level. All levels are negotiated to some extent. Figure 1 Integrated Disability Management Continuum Fragmentation Migration Segmentation Coordination Integration Progression of Internal Corporate Integration of Benefits None Mixed Full Fragmentation to Segmentation This is the common silo or commodity product approach to benefits management. This model is negotiated with various competing external vendors, as well as with the internal management. These segments work independently and often in competition. There is little communication between the groups and effective utilization of corporate resources. A segmented model can be relatively benign. A fragmented program encourages excessive lost time and significant corporate financial losses. Rather than being a product of negotiations, the levels of organizational structure may be maintained by the lack of interest or skills in making the organization work in a functionally coordinated fashion. Disability Migration This is the active movement of lost time cases between and within the segment. The intent is to seek the best combination of benefits or reduce the defined risk. The employee and employer often unknowingly negotiate the migration routes between work compensation to short term disability claims or the reverse. Disability migration is the product of disability negotiation that creates unequal incentives or rewards to control lost time. Disability Management Coordination The coordination of benefits is most commonly mistaken for integration. In the coordinated model, the focus is on negotiating communication links and developing agreed upon service hand offs. A clear corporate disability management philosophy serves as a foundation for all benefit management activities. The disability programs may still be managed from different parts of the organization with services provided by different vendors. This negotiated model offers a corporate disability management template for these groups with decentralized benefits management focus or a widely dispersed work force. Negotiated Disability – Page 2 Disability Management Integration A truly integrated disability management program reflects the corporate wide blending of all lost time management. This also includes the various clinical and human resource management functions to control lost time. The integration creates a single claims administration process, as well as a single stay at work and return to work philosophy supported by cohesive set of strategies by management. A single insurance vendor may be used or combined with a self-insurance program. Points of Negotiation Once an employer has determined what level, degree and model of integration fits their program needs and readiness, a more focused level of disability negotiation begins. These negotiating points ultimately determine who is “disabled” and who is not. These decisions determine the application of and the accessibility to corporate disability management resources. Figure 2 identifies the key disability negotiating points. Figure 2 Corporate Negotiating Points Eligibility Thresholds Benefit Focus Access to Care & Iatrogenic Disability All or Nothing Return to Work Thresholds Risk Management Politics Collective Bargaining Agreements Supervisor Incentives & Performance Evaluations Eligibility Thresholds Eligibility for short term disability and worker’s compensation benefits is typically negotiated with the appropriate insurance vendors through guidelines set by state legislatures, regulators and benefit plan designs. The resulting disability definitions and thresholds determine the nature and scope of who is considered disabled or not. They also create the expected time frame a person may be entitled/invited/expected to stay off work. The greater the ambiguity of the definition of disability, the more potential for abuse. The narrower the definition, the greater opportunity for disability migration and perceived unfair treatment. Some employers control risk by negotiating disability definitions rather than managing the post injury or illness adjustment. Benefit Focus All too often the employer, with the encouragement from the insurance provider, focuses on the insurance products rather than the individuals using the various benefits. This is a benefit-centered vs. person- centered approach. The interaction between worker’s compensation and short-term disability should be a common focus. A Negotiated Disability – Page 3 more abstract, but potentially more powerful interaction, may exist between disability benefits and health care utilization. Figure 3 illustrates a sample Pareto distribution of health care utilization by individuals also using the disability benefits. The interaction between health care and disability is critical. The resulting integrated disability management program needs to reflect the reality of this interaction. Figure 3 Sample Pareto Analysis of Benefit Cost Per Employee C o st P er E m p lo yee E m p lo yees N o n -P areto G ro u p L o st T im e P areto G ro u p % of E m p lo yees LTD $ STD/ S ick $ W CI $ W CM $ M ed In s $ A ll B en efits $ % of T o tal C o st 88% 0 154 0 23 1,321 1,499 42% 12% 78 2,895 1,478 1,424 8,816 14,692 58% K ey A n alytic F in d in g : F ocusing m anagem ent initiatives on the 12 percent of em ployees that use 80 percent of LT D , S T D /S ick, and W C I benefits provides the opportunity to im pact 58 percent of T otal H ealth B enefit P rogram costs. T hese high risk group of em ployees have 10 tim es higher costs, on average. As an integrated disability program is created, the ability to influence both lost time and health care utilization is a natural and desired expectation. This will not occur normally and will require close cooperation between the healthcare vendor, the employer and the disability insurance partner. Historically, this has not been a natural alliance. Access to care & Iatrogenic Disability Access to care must become a focused point of negotiation to assist individuals to return to work in a safe and timely fashion. Two treatment protocols commonly negotiated out of a return to work program are: post heat attack cardiac rehabilitation and work hardening transitions following a leave due to depression. The capacity to have access to cardiac rehabilitation and behavioral health has shown to improve return to work outcomes. Both of these treatment programs are tightly controlled within the majority of healthcare plans. Effective negotiation to make these parts of the return to work plan can change the outcomes of the integrated disability product. End of the benefit healing (EBH), i.e. immediate resumption of work the day before the allotted number of days off, is real and may be an indictor of Iatrogenic disability. It suggests a lack of effective management of the lost time case. The use of the duration guideline as the start of the disability management process rather than the end must be eliminated. A formal return to work plan created at the onset of the leave can provide clear guidelines for the employee, employer, as well as the physician. Negotiated Disability – Page 4 Iatrogenic Disability, commonly referred to as treatment or physician created disability, may reflect a lack of attention by the attending physician to offer a formal work prescription (WorkRx). The WorkRx invites the physician to go beyond the presentation of work restrictions, but requires a well-defined set of return to work or stay at work transitions. These transitions not only focus on a return to work date, but how the person should resume full productivity. The All or Nothing RTW Thresholds The 100% or nothing return to work practice has shown to be a costly policy for employers to maintain. This practice is a common residual of the return to work myth held by risk management professionals. Also, this practice, while being applied to non-work related lost time cases, is often discarded when considering a return to work for individuals on worker’s compensation. One of the first steps in building an integrated disability management program is to negotiate 100% of Nothing practice into obscurity. The most effective way to dispel this myth is to closely examine the options in which employees can resume productive work activities in a safe and incremental manner. By establishing employee neutral, RTW pathways in 30-day increments the employer will support a fair and fully integrated approach. Risk Management Politics A regularly negotiated return to work practice is to apply a formal return to work program to individuals off work for an occupational related injury or illness and not for those employees with a non-work related lost time. This negotiation appears to be the product of a risk management program with an exclusive workers’ compensation orientation. This practice has shown to be a significant driver of excess disability costs. Likewise, this type of program fails to recognize that non-work related lost time could be 5 to 7 times greater than the work related lost workdays. As this practice has been modified or negotiated to a level of parity, employers report savings of some 30% to 50% in reduced lost work days and subsequent lost time costs. Collective Bargaining Agreements Historically, collective bargaining agreements (CBA) define the safe working conditions, seniority benefits, etc at the work site. Many employee relations and labor officials have the collective bargaining agreement defer the question of when a person should come back to work to the attending physician. While this is appropriate, the CBA can appropriately define “ how” an individual resumes their work activities. In most cases, the “how” dictates the “when”. All too often, we make how a person comes back to work as a “let’s see what happens” attitude. This ambiguity confuses employees, physicians and supervisors alike. It also can reduce the employee’s motivation to return to work by creating doubt in their ability to do the job. Effectively negotiated RTW pathways offer both guidance and assurance to all. Supervisor Incentives & Performance Evaluations In any political negotiation, self-interests are the fuel for compromises. It must be in the self-interest of the supervisor and individual to secure or support a timely return to work. There are several options: The first step is to expect supervisors to support a timely return to work for their employees. This can be done by making RTW support part of their job description and reinforced by recognition within their performance evaluation. Correspondingly, Negotiated Disability – Page 5 supervisors must be encouraged to resolve employee performance problems through the appropriate human resources solutions rather than encouraging poor performers to go on disability. Poor work performance and disability may appear to be two different issues. They are closely connected and can be effectively managed through a fully integrated disability management program. IDM Program Development Negotiating Strategies When an organization initially considers the development of an integrated disability management program; there are several key negotiating strategies. Figure 4 presents these critical development steps to become an effective disability negotiator. Figure 4 Program Development Steps Understand the impact of lost time Build a single information platform Create a uniform lost time strategy Define policies to achieve desired outcomes Define expected outcomes Define RTW Planning roles and accountability Educate managers, supervisors, labor leaders Reduce segmentation Understand the Impact of Lost Time The key principle of any negotiation is to negotiate from a position of strength. Information is power. The senior management team that understands the impact of lost time within their organization is better able to define the resources needed to control the critical drivers. Without accurate information that defines the real impact, any negotiation is a guess. As the question of disability management integration is considered, the organization needs to define the accurate impact of lost time and the corresponding drivers. Build a Single Information Platform Many organizations look to create a single claims submission process as the basic IDM program. The development of a single information platform that presents clear lost time patterns and trends is the first step. This typically requires effective negotiation between the various benefit vendors or resources to capture the desired variables. Create a Uniform Lost Time Strategy True lost time management springs from a cohesive lost time strategy created by the employer. Without this philosophical or policy base, the organization will default to individual lost time beliefs of its supervisors and employees. On a recent review of an employer return to work program, it was reported that they did not have a formal lost time or injury management philosophy. One was found on a bulletin board in the Employees’ locker room…. It read…. “If you get hurt…Call an attorney”. In lieu of a formal corporate policy, this became the only guidance offered to the work force. Negotiated Disability – Page 6 Define Policies to Achieve Desired Outcomes IDM policies need to define what is expected of all the participants. If a return to work is expected, this needs to be well defined both as to when, but more importantly on how the person should return. Likewise, if the program is purely an income replacement program, do not expect a timely return to work. RTW options and expectations are clearly negotiable. Implement Target Strategies for Expected Outcomes With the development of a uniform database and clear understanding of the impact of lost time within the organization, specific return to work strategies can be applied. The three most effective return to work strategies that support an IDM program are: Formal RTW Planning with a well define WorkRx Transitional Work Program supported by work conditioning RTW Pathways defined prior to the work disruption Define RTW Planning Roles and Accountability - The resumption of work following an injury or illness does not have to be ambiguous, informal or left as an after thought. Clear accountability must be developed to assure that both the employee and the physician understand the nature and scope of the RTW options. This planning role is typically negotiated between the organization and the various disability insurers. In a fragmented program, this function is usually left to happen stance. In a coordinated program it may be provided by one of the disability insurers. In a fully integrated program, the employer will develop the resources to provide such guidance or work collaboratively with the disability insurer driving the IDM process. Educate Managers, Supervisors, Labor Leaders Managers, supervisors and union stewards become the kings and queens of return to work. They often are the people who determine how a person can and will return to work. They control the flexibility of the work site. This is done through negotiation of time, work assignments and productivity demands. A critical strategy is to offer a formal education program that prepares supervisor, managers and union stewards to 1. Understand the impact of lost time both on their organization and the employee and 2. What they can do to mitigate the impact. Reduce Segmentation While many organizations are not ready, capable or interested in a fully integrated disability management program. But, any reduction or consolidation of the disability management fragmentation and segmentation is beneficial. This may mean consolidating several insurance vendors into one, creating a clear RTW template across affiliate operations or creating some degree of RTW planning continuity. Negotiating disability may be a foreign, if not, uncomfortable concept for some. Many insurance, human resource, as well as employers may subscribe to the notion that you are either disabled or you are not. Disability is subjective and depends. Some form of disability negotiation goes on every day, within every organization and physician office. Being an effective disability negotiator can make the difference between excessive cost, meeting productivity expectations or maintaining personal independence. Negotiated Disability – Page 7 Negotiated Disability – Page 8