The Urinary System - People Server at UNCW
advertisement

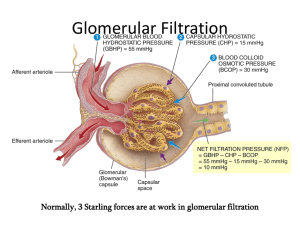
THE URINARY SYSTEM Name some by-products of cellular metabolism of nutrients. carbon dioxide, nitrogenous wastes, excessive water, and heat What are nitrogenous wastes? Nitrogenous wastes, such as ammonia and urea, are formed as a result of protein catabolism (breakdown). What do essential ions, such as sodium, chloride, sulfate, phosphate, and hydrogen ions, tend to do in the extracellular fluids? accumulate in excess of the body’s needs What is the role of the urinary system in maintaining normal body homeostasis? The kidneys excrete water, nitrogenous wastes, some bacterial toxins, hydrogen ions, essential ions, some heat, and some carbon dioxide from the body in the form of urine. Name, and then give a brief description of, three other ways in which the body rids itself of waste products. lungs -- The lungs excrete carbon dioxide, heat, and water into exhaled air. sudoriferous glands -- The sudoriferous glands excrete water, ions, urea, and heat into sweat. gastrointestinal tract -- The gastrointestinal tract excretes feces, water, ions, and heat. Identify the structures of the urinary system. The urinary system consists of: kidneys (2) ureters (2) urinary bladder urethra What is the primary function of the urinary system? How is this accomplished? The primary function of the urinary system is to help maintain homeostasis by controlling the composition, volume, and pressure of blood. It does so by removing and restoring selected amounts of water and solutes from the blood. 319 A. KIDNEYS Identify and give a brief description of the five major functions of the kidneys. regulate blood volume and composition by removing wastes, ions, and water to form urine regulate blood pressure by secreting renin, which activates the angiotensin-aldosterone pathway secrete erythropoietin in response to decreased blood oxygen to stimulate erythropoiesis participate in the synthesis of calcitriol, the active form of vitamin D participate in glucose metabolism by performing gluconeogenesis during fasting or starvation 1. EXTERNAL ANATOMY Describe the kidneys as follows: location -- The paired kidneys are located just above the waist, between the parietal peritoneum and the posterior abdominal wall (retroperitoneal). They lie at vertebral levels T12 - L3 and are partially protected by ribs 11 and 12. shape and size -- The average adult kidney is about 4 - 5 inches long, 2 - 3 inches wide, and 1 inch thick. It is shaped like a bean, with its concave medial surface facing the vertebral column. hilus -- Near the center of the medial concave border is the hilus, an indentation through which the ureter, renal artery and vein, nerves, and lymphatics enter and exit the kidney. The hilus serves as the entrance to a cavity in the kidney called the renal sinus. renal fascia -- Surrounding each kidney are three layers of connective tissues. From outermost, these layers are the renal fascia, the adipose capsule, and the renal capsule. Renal fascia is a thin layer of dense connective tissue that anchors the kidney to its surrounding structures, to the abdominal wall, and to its partner on the opposite side. 320 adipose capsule -- The adipose capsule is a mass of fatty tissue that surrounds the two kidneys. It is used to protect the kidneys from the trauma and help hold them in place within the abdominal cavity. renal capsule -- The renal capsule is a thin, transparent dense connective tissue that forms the outer surface of the kidney itself. It serves as a barrier against trauma and the spread of infection to the kidney. 2. INTERNAL ANATOMY Describe the kidneys as follows: appearance in coronal section -- In coronal (frontal) section, the kidney presents an outer area, the cortex, a middle region, the medulla, and an innermost area, the renal pelvis. renal pyramids -- Within the medulla are 8 - 18 cone-shaped structures called renal (medullary) pyramids that look striated due to a high number of straight parallel tubules (collecting ducts) and blood vessels. The bases of the renal pyramids face the cortex, while their apices, called renal papillae (papilla is singular) face toward the center of the kidney, opening into the renal sinus. renal columns -- The cortex is the smooth-textured area extending from the renal capsule to the bases of the pyramids and into the spaces between the pyramids, forming the renal columns. cortical zones -- The cortex is divided into the outer cortical zone and the inner juxtamedullary zone. Together, the cortex and renal pyramids form the parenchyma (functional portion) of the kidney. The parenchyma consists of about 1 million microscopic tubules called nephrons. The nephron is the functional unit of the kidney. calyces -- In the renal sinus of the kidney is a large cavity called the renal pelvis, the edge of which contains cup-like extensions called major (2 - 3) and minor calyces (8 - 18). Each minor calyx receives urine from a renal pyramid and delivers it to a major calyx. From there, urine drains into the renal pelvis and out through the ureter to the urinary bladder. 321 3. NEPHRON Name, and then briefly describe, the three basic functions nephrons. filtration -- In filtration, most substances in the blood are permitted to pass from the blood into the lumina of the nephrons, while others are kept out. This is called filtration, like in capillary exchange, because it is driven by pressure across an endothelium. reabsorption -- As the filtered liquid, known as filtrate, flows through nephrons, useful materials are returned to the blood by the process of reabsorption. Reabsorption occurs by diffusion and active transport. secretion -- As filtrate moves through the nephrons, cells of the nephron (tubule cells) secrete some additional materials (particularly hydrogen ions) directly into the filtrate. a. b. PARTS OF THE NEPHRON CORTICAL AND JUXTAMEDULLARY NEPHRONS List in order of appearance the sections of a nephron. 1--Bowman’s capsule, 2--proximal convoluted tubule, 3--proximal straight tubule, 4--loop of Henle, 5--distal straight tubule, 6--distal convoluted tubule, and 7--collecting duct. Describe the nephron as follows: renal corpuscle -- A nephron consists of two portions: a renal corpuscle, where plasma is filtered into the nephron, and a renal tubule, into which the fluid passes. The renal corpuscle has two components -- a tuft of capillaries called glomerulus, surrounded by a doublewalled cup known as Bowman’s (the glomerular) capsule. Describe Bowman’s capsule. The outer wall of Bowman’s capsule is the parietal layer and the inner wall is the visceral layer. Between the two layers is the capsular space, into which the blood is filtered. It is through the visceral layer that water and most of the solutes of plasma in the glomerulus pass 322 into the capsular space. Plasma proteins and formed elements do not cross the visceral layer. glomerulus -- The glomerulus is a tuft of capillary loops sitting in the “cup” formed by Bowman’s capsule. Blood enters a glomerulus via an afferent arteriole and exits glomerulus via an efferent arteriole. This is a significant departure from the usual vascular pattern of artery, capillary, vein. renal tubule -- From the capsular space, filtrate moves into the renal tubule, which has three main sections: the proximal convoluted tubule (PCT), the loop of Henle, and the distal convoluted tubule (DCT). It is within these sections that tubular reabsorption and tubular secretions occur. collecting duct -- The terminal ends of many DCTs enter a single collecting duct. Collecting ducts are gathered to form renal pyramids, and eventually merge to form the large papillary ducts that open into the minor calyces to drip newly formed urine into the renal pelvis. loop of Henle -- In a nephron, the loop of Henle connects the PCT with DCT. The first portion of the loop, the descending limb dips into the medulla, while the ascending limb, returns to the cortex. The loop itself is formed of proximal and distal straight segments (simple cuboidal cells) and the loop portion, formed of simple squamous cells. cortical nephrons -- A cortical nephron has its glomerulus in the outermost portions of the cortex and its loop barely reaches the medulla. juxtamedullary nephrons -- A juxtamedullary nephron has its glomerulus deep in the cortex, close to the medulla. Its loop is quite long, reaching deep into the medulla to approach the renal papillae. Only 15 - 20% of all nephrons are of the juxtamedullary type. These are the nephrons that allow the formation of either very dilute or very concentrated urine. 323 c. HISTOLOGY OF THE NEPHRON What is the endothelial-capsular membrane? Histologically, the renal corpuscle consists of the visceral layer of Bowman’s capsule and the endothelium of the glomerular capillaries. It is this endothelial-capsular membrane that acts as a filter for the blood. Describe the following: endothelium -- The endothelium of the glomerulus consists of a single layer of fenestrated simple squamous cells. The endothelium prevents passage of the formed elements from the blood into the filtrate, but allows all other blood components to pass. basement membrane -- The basement membrane of the glomerulus consists of the fused basement membranes of the endothelium and the visceral layer epithelium of Bowman’s capsule. It acts to restrict passage of the larger plasma proteins but allows all other solutes to pass into the filtrate. visceral layer -- The epithelial cells of the visceral layer of Bowman’s capsule are specialized cells called podocytes. Each cell has thousands of foot-like processes called pedicels, between which are open spaces called filtration slits. The pedicels function to hold the visceral layer of Bowman’s capsule to the glomerular capillaries. The filtration slits do not present much of a barrier to filtration, although the pedicels are negatively charged and help prevent passage of anions. As a result of these barriers to filtration, the formed elements and plasma proteins remain in the blood of the glomerulus while all other solutes freely pass from glomerulus into the filtrate. Describe the histology of the following: proximal tubule -- The simple cuboidal cells of the proximal tubule have an extensive brush border (microvilli) for increased surface area for tubular reabsorption. Thus, some 65% of water and almost 100% of some solutes in filtrate move back into the blood via the proximal tubule. 324 loop of Henle-- The loop of Henle is composed of simple squamous cells, indicative of an area where rapid transport of materials occurs. The loops of Henle are particularly important in the formation of concentrated urine, especially those of the juxtamedullary nephrons. distal tubule and collecting duct -- The distal tubules and collecting ducts are formed of simple cuboidal cells that lack a brush border. However, most of the cells, called principal cells, bear receptors for the hormones ADH and aldosterone, and are involved in the control of water excretion. On the basal surface of the cells are extensive infoldings and mitochondria. It is in this area that many solutes are pumped back into the blood. 4. BLOOD AND NERVE SUPPLY Describe the arterial supply, capillary arrangements, and venous drainage of the kidneys. Since the role of the kidneys is to filter the blood, it is not surprising that they have an abundant blood supply. The right and left renal arteries carry 25% of resting cardiac output to the kidneys (1,250 ml/min). Each renal artery enters its respective kidney at the hilus, and then divides several times before it enters the parenchyma, where the branching continues down to the level of the afferent arteriole. There is one afferent arteriole leading into each nephron, dividing within the cup of Bowman’s capsule to form the glomerulus. The glomerular capillaries merge to exit Bowman’s capsule as the efferent arteriole. The efferent arteriole has a smaller diameter than the afferent arteriole; this helps to raise glomerular blood pressure higher than would be found in a normal tissue capillary bed. The efferent arteriole leaves Bowman’s capsule and participates in the formation of two separate capillary networks: peritubular capillaries surround the PCT and DCT, while the vasa recta follow the loop of Henle. 325 These capillary beds merge to form venules, then veins, which eventually merge to form the right and left renal veins that leave the respective kidney at the hilus and join the inferior vena cava. Describe the juxtaglomerular apparatus as follows: location -- The juxtaglomerular apparatus is a combined structure that is formed where the final portion of the ascending limb of the loop of Henle (beginning of the distal convoluted tubule) comes to lie in contact with the afferent arteriole. macula densa -- At the point of contact, the cells of the DCT are specialized to form macula densa cells that monitor flow of filtrate. juxtaglomerular cells -- Also at the point of contact, the smooth muscle cells of the afferent arteriole are specialized to form juxtaglomerular cells. They function in monitoring blood pressure in the afferent arteriole and to secrete the molecule renin when blood pressure in the afferent arteriole falls too low. function -- Together, the macula densa and the juxtaglomerular cells form the juxtaglomerular apparatus. It is involved in the regulation of blood pressure and the rate of blood filtration by the kidneys by secreting renin when blood pressure is too low and by decreasing its secretion of an as yet unnamed vasoconstrictor substance when there is decreased delivery of sodium, chloride, or water in the filtrate.. Describe the nerve supply of the kidney. The nerves supplying the kidneys are derived from the renal plexus of the sympathetic nervous system. These nerves are associated with the blood supply, particularly the afferent and efferent arterioles, and thus regulate blood flow to the glomerulus (and therefore the rate of filtrate formation) by regulating the diameters of the arterioles. B. PHYSIOLOGY OF URINE FORMATION Identify the three important functions carried out by the nephrons. 1. 2. 3. control blood concentration and volume by removing selected amounts of water and solutes. regulate blood pH remove toxic wastes from the blood 326 What is the net effect of these functions? As the nephrons accomplish these functions, they remove materials from the blood, return the ones that the body requires, and excrete (eliminate) from the body the remainder as urine. Urine formation requires three processes. Name them in order of when they occur in the nephron. 1. 2. 3. 1. glomerular filtration by the renal corpuscle tubular reabsorption by the renal tubule tubule secretion by the renal tubule GLOMERULAR FILTRATION a. NET FILTRATION PRESSURE Define the principle of filtration. Filtration is the forcing of fluids and solutes through a membrane by mechanical pressure (all capillaries move fluids in this manner). Name the membrane across which filtration occurs in the kidney. Filtration occurs in the renal corpuscle across the endothelial-capsular membrane. What is the driving force for glomerular filtration? Blood hydrostatic pressure forces water and solutes from plasma through the endothelial fenestrations, the fused basement membrane, and the filtration slits of the visceral layer of Bowman’s capsule, into the capsular space. What is the resulting fluid in the capsular space called? The fluid found in the capsular space is known as filtrate. How much is formed per day? Approximately 180 liters of filtrate are formed per day. This is some 60 times the entire blood plasma volume. What does it contain? In a healthy person filtrate contains everything in blood except formed elements and plasma proteins. 327 Name and give a brief description of the three structural adaptations that enhance glomerular filtration. glomerular capillaries are long -- The total length of the capillaries within the glomerulus is very high, yielding a very large surface area for filtration. filter is porous and thin -- The endothelial-capsular membrane, with its fenestrae, fused basement membrane, and filtration slits, is about 50 times more porous than regular capillaries. afferent vs efferent arteriole diameter -- Since the efferent arteriole has a smaller diameter than the afferent arteriole there is a damming effect in the glomerular capillaries causing glomerular blood hydrostatic pressure to be high. Describe the following pressures: glomerular blood hydrostatic -- Glomerular blood hydrostatic pressure (GBHP) (60 mm Hg) is the chief pressure of glomerular filtration. It is the pressure of blood within the glomerular capillaries pressing against the inside of the vessels. It is an outward force, trying to move fluid into the capsular space. capsular hydrostatic -- Capsular hydrostatic pressure (CHP) (15 mm Hg) is the pressure of filtrate in the capsular space pressing against the visceral layer of Bowman’s capsule. It is, therefore, an inward force, trying to move fluid into the glomerular blood. blood colloid osmotic -- Blood colloid osmotic pressure (BCOP) (27 mm Hg) is the osmotic pressure exerted by the trapped plasma proteins in the glomerular blood. It tends to cause water to move back into the glomerular blood. It is, therefore, an inward force. net filtration pressure -- The net filtration pressure (NFP) is determined as: NFP = = = = = GBHP- (CHP+BCOP) outward - inward 60 - (15+ 27) 60- 42 +18 mm Hg 328 The positive number means that the flow of fluid is into the capsular space. Normal capillaries have an NFP of +10 mm Hg on the arterial end. This higher NFP helps ensure that renal filtration occurs. filtration fraction -- The filtration fraction is the percentage of plasma entering the nephrons to become filtrate. It is normally about 10% per pass through the kidneys. cardiac output = 5,250 ml/min 25% goes to the kidneys = 1,250 ml/min filtration fraction = 10% Therefore, 125 ml/min filtrate formed. b. GLOMERULAR FILTRATION RATE Define glomerular filtration rate (GFR)? The glomerular filtration rate (GFR) is the amount of filtrate formed in all renal corpuscles in both kidneys per minute (125 ml/min). What factors determine the glomerular filtration rate? The GFR is directly related to the pressures that determine the net filtration pressure (NFP). Anything that alters the NFP will ultimately alter the GFR. c. REGULATION OF GFR Homeostasis of body fluids requires that the kidneys maintain a relatively constant GFR. What happens if the GFR is too high? Needed substances pass through the kidneys so quickly they are not reabsorbed and are lost into the urine. What if the GFR is too low? Nearly all filtrate is reabsorbed and waste products may not be properly excreted from the body. Glomerular blood flow depends on two factors. Name them. Glomerular blood flow depends on two factors: 1. systemic blood pressure 2. diameter of the afferent and efferent arterioles 329 List the three principle mechanisms that regulate these two factors. 1. 2. 3. renal autoregulation of GFR hormonal regulation of GFR neural regulation of GFR Describe the mechanisms by which renal autoregulation protects the GFR. Under normal conditions, macula densa cells secrete a vasoconstrictor substance that maintains a “normal” level of afferent arteriole vasoconstriction. When filtrate flow rate is low, macula densa cells secrete an inhibitor to the secretion of the vasoconstrictor. What is the result? As a result of removal of the vasoconstrictor, the afferent arterioles are allowed to vasodilate. Increased blood flow into the glomerular capillaries means increased GBHP, increased NFP, and increased GFR.. Name and describe the two hormonal mechanisms used to regulate the glomerular filtration rate. Hormonally, the renin-angiotensin-aldosterone system and atrial natriuretic peptide are used to regulate GFR. Renin, secreted by the juxtaglomerular cells of the juxtaglomerular apparatus in response to decreased blood pressure in the afferent arteriole, results in the formation of angiotensin II, which has four important functions. (1) It is a potent vasoconstrictor body-wide, thus increasing BP. In the efferent arteriole, this would cause increased GBHP and therefore increased NFP. (2) Angiotensin II stimulates thirst and thereby increases blood volume. This in turn increases systemic BHP. (3) Angiotensin II stimulates aldosterone secretion. Aldosterone stimulates increased reabsorption of Na+ and therefore increased reabsorption of water. This causes increased blood volume and therefore BHP. 330 (4) Angiotensin II stimulates anti-diuretic hormone (ADH) secretion. ADH stimulates increased water reabsorption, again raising blood volume and therefore BHP. The net result of these combined effects is increased systemic blood pressure, so that NFP is increased, and therefore, GFR is increased. From where is atrial natriuretic peptide secreted and why? How does ANP help regulate the glomerular filtration rate? ANP is secreted from the atrium of the heart in response to stretch caused by increased blood volume. ANP stimulates excretion of Na+, and therefore water, resulting in decreased blood volume. Decreased blood volume causes decreased BHP and therefore decreased NFP and decreased GFR. Describe the neural regulation of glomerular filtration rate. Based on blood pressure changes, sympathetic innervation to the afferent and efferent arterioles can be increased or decreased to change the GHBP and therefore alter the NFP and GFR. 2. TUBULAR REABSORPTION Define the concept of tubular reabsorption. How is it accomplished? Tubular reabsorption is the movement of water and selected solutes back into the blood of the peritubular capillaries and the vasa recta. Renal tubular epithelial cells use very discriminating processes that are dependent upon the body’s needs at the moment. In general, most of the body’s nutrients are retained while wastes are eliminated. What is tubular maximum (Tm)? Tm is the maximum amount of a solute that can be reabsorbed under any condition. 331 Discuss the active and passive transport mechanisms by which tubular reabsorption is accomplished. Tubular reabsorption is carried out through both active and passive transport mechanisms, primarily in the proximal tubule. Active transport involves the use of specific receptors (carrier molecules) found on the luminal surfaces of the tubular epithelial cells. When a substance in the filtrate binds to its specific receptor on the luminal surface of the cell, it is brought into the cell with the expenditure of energy, against its concentration gradient. Glucose and amino acids are 100% reabsorbed under normal conditions, since their active transport carriers are activated at all times. Other substances are actively transported only when their carrier systems have been activated by the endocrine system (ex: Na and K+ -- aldosterone, Ca -- parathyroid hormone). In passive transport, no energy is used when solutes simply diffuse into the tubular epithelial cells, either following their concentration gradient or their electrical gradient (ex: Cl, phosphate). Distinguish between obligatory and facultative reabsorption of water. In obligatory reabsorption, water follows reabsorbed solutes, primarily glucose and Na+, due to the osmotic gradients that are created between the filtrate and the intracellular fluid of the renal tubular cells. How is this type of reabsorption controlled? Since Na+ is the major extracellular cation, it has enormous effects on water movement. Its control by aldosterone, therefore, is a major control of water balance as well. In facultative reabsorption of water, the permeability of distal tubule and collecting duct cells to water is controlled directly by antidiuretic hormone (ADH). ADH is secreted from the hypothalamus during times of dehydration. What is the effect of ADH? ADH increases the number of water channels in the tubular cells, thus allowing water molecules to leave the filtrate and 332 enter the cells. This process is used to control the remaining 10% of water reabsorption and is the major controller of moment-to-moment needs in water balance. 3. TUBULAR SECRETION Define tubular secretion. The third process in urine formation is tubular secretion. In this process, renal tubular cells remove solutes from the blood and directly secrete them into the filtrate so that they will be excreted with the urine. What are its major functions? Tubular secretion has two principle effects: 1. to rid the body of substances that tend to accumulate in the body fluids (H+, NH3, K+, creatinine, some drugs); and 2. help control body pH How does it control body fluid pH? The body must tightly control pH at 7.35 - 7.45, despite the fact that a normal diet and normal metabolism promote the accumulation of hydrogen ions and therefore acidic conditions. To help raise body pH, renal tubule cells secrete H+ and ammonium (NH4) ions directly into the filtrate, so that they are lost in the urine. The ions are exchanged for Na+, so that Na+, and water, are reabsorbed. What is the relationship between tubular secretion and potassium? Potassium (K+) ions tend to accumulate in the body. In response to aldosterone, K+ ions are in exchange for Na+ ions, with water following. 4. SUMMARY OF NEPHRON FUNCTIONS a. Proximal tubule reabsorbs by osmosis -active transport -- simple diffusion -- water sodium ions glucose amino acids potassium ions chloride ions bicarbonate ions urea 333 secretes -- b. Loop of Henle reabsorbs by osmosis -active transport -- secretes -c. C. water sodium ions chloride ions urea potassium ions Collecting duct reabsorbs by osmosis -simple diffusion -- secretes -- water sodium ions potassium ions chloride ions urea Distal tubule reabsorbs by osmosis -active transport -- secretes -d. hydrogen ions ammonium ions urea creatinine water bicarbonate ions urea hydrogen ions URETERS 1. STRUCTURE 2. FUNCTION 3. PHYSIOLOGY Trace urine flow from the nephron to the outside of the body. From the collecting ducts urine is drained through papillary ducts into the minor calyces that drain into the major calyces that unite to form the renal pelvis. Urine then drains into the ureters. Using peristaltic movements, the ureters move urine to the urinary bladder, which stores the urine until it is expelled from the body via the urethra. Describe the ureters as follows: gross anatomy -- Each ureter is an extension of the renal pelvis of its respective kidney. It extends 10 - 12 inches, retroperitoneally, to enter the urinary bladder medially from its posterior aspect. 334 union with bladder -- There is no anatomical valve located at the junction of the ureter with the bladder. Instead, as the bladder fills with urine, pressure in the bladder wall compresses the ureteral openings and prevents reflux of urine into the ureters. histology -- Histologically, the ureters are lined with transitional epithelium, have longitudinal and circular layers of smooth muscle, and an outer adventitia that attaches the ureters to the overlying peritoneum. function -- The principle function of the ureters is to transport urine to the bladder. In addition to hydrostatic pressure, 1 - 5 peristaltic waves/minute pass down the ureters, moving the urine forward. D. URINARY BLADDER 1. STRUCTURE 2. FUNCTION 3. PHYSIOLOGY Describe the bladder as follows: gross anatomy -- The urinary bladder is a hollow muscular organ situated retroperitoneally in the pelvic cavity, posterior to the pubic symphysis. It is a freely movable organ held in place by folds of the peritoneum. When completely empty, it is collapsed. As it fills, it moves superiorly, rising into the abdominal cavity. male vs female -- In the male, the bladder is directed anterior to the rectum. In the female, it is anterior to the vagina and inferior to the uterus. epithelium -- Histologically, the urinary bladder is formed of the same three layers as the ureters (transitional epithelium, muscularis, and adventitia). The difference between the two is in the muscularis. detrusor muscle -- The muscularis of the bladder is collectively known as the detrusor muscle. It consists of three layers of smooth muscle (longitudinal, circular, and longitudinal) and works as a unit during the micturition reflex. 335 sphincters -- Around the opening of the urethra, the middle circular layer of smooth muscle is thickened to form the internal urethral sphincter. It is under unconscious (reflexive) control. The muscle of the pelvic diaphragm forms the external urethral sphincter where the urethra pierces through it. This muscle is consciously controlled. trigone -- In the floor of the bladder is a triangular area, the trigone, formed by the two urethral openings, and anteriorly by the opening into the urethra. What is micturition? Urine is expelled from the bladder by an act known as micturition (urination or voiding). This process occurs in response to a combination of involuntary and voluntary nerve impulses. Describe the micturition reflex. The average capacity of the bladder is 700 - 800ml. When urine volume is 200 - 400ml, stretch receptors in the bladder wall transmit impulses to the sacral spinal cord. By way of ascending tracts, these impulses initiate the conscious desire (cerebral cortex) to expel urine. In the sacral spinal cord itself, the micturition reflex is integrated. Parasympathetic outflow from the sacral spinal cord causes contraction of the detrusor muscle and relaxation of the internal urethral sphincter. At the same time, the cerebral cortex permits the voluntary relaxation of the external sphincter (this is a learned response), and urine is voided from the body. E. URETHRA 1. HISTOLOGY 2. PHYSIOLOGY What is the urethra? The urethra is a small tube leading from the floor of the bladder to the body exterior. Describe it as follows: epithelium -- The epithelium of the urethra is a blend of types. It begins as a continuation of the transitional epithelium of the bladder and ends as stratified squamous at its termination, 336 where it blends into the keratinized stratified squamous of the skin. female urethra -- In the female, the urethra lies directly posterior to the pubic symphysis, in front of the anterior wall of the vagina. It is about 1.5 cm long and opens to the exterior (external urethral orifice), between the clitoris and vaginal introitus. male urethra -- In the male, the urethra is about 8 inches long. Upon leaving the bladder it passes immediately into and through the prostate gland (prostatic urethra), then the pelvic diaphragm (membranous urethra), and finally the penis (penile urethra), ending at the external urethral orifice. function(s) -- Functionally, the urethra serves as the final passageway for urine from the body. In the male, it also serves as the duct through which semen is discharged to the exterior. 337