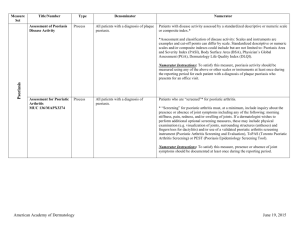
EULAR_transcript_200..
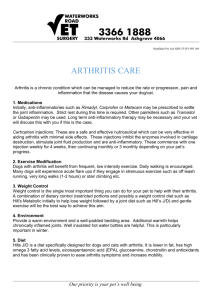
advertisement

GRAPPA June 8, 2005 Philip Mease: Hello. Could people please have a seat? I. Philip Mease: Introduction Thank you very much for attending the GRAPPA meeting at EULAR 2005. For the sake of keeping on schedule today, we have a very busy agenda. We are going to move right along. We are taking things, in a sense, a bit out of order, in that one of the committee reports, the committee led by Desiree van der Heijde, having to do with x-ray assessment in PsA, will come first because of other obligations that Desiree and Robert Landewe and John Sharp have, all of whom could be here for this part of the discussion and so that will finish up sharply at 1:30. I just have a few introductory comments to make. This is today’s agenda. We will try to stick with it as closely as possible on time. First, going over radiology assessment, then very importantly, a CASPAR update since we are now having data emerging from Philip Helliwell and Will Taylor’s study. Then, a fairly long period of time for a treatment guideline discussion to be led by Artie Kavanaugh and Chris Ritchlin. We will then have a break, and hopefully, some food at the break. From 3:45 on, we will be having a series of committee reports, beginning with research committee, then quality of life and participation, the interesting study that Alberto Cauli is leading having to do with global assessment, and then Dominique Baeten will give a review on discussions that have been going on regarding standardization of tissue histology and immunohistochemistry, since Oliver Fitzgerald could not be here. I will update the group on plans for a World Congress of psoriasis and psoriatic arthritis, which is being held in Stockholm, May 31-June 2, 2006. I will give you details about that. Henning Boehncke from Germany will be giving a review of subjects from the dermatology world. We will conclude the committee reports with discussions about the publications committee and then close. For this meeting and this year’s support for EULAR, we gratefully acknowledge the following companies: Abbott, Amgen, Aventis, Biogen-Idec, Centocor, Novartis, Schering-Plough, and Wyeth. This is the membership of GRAPPA: there are 174 members currently. This gives you a spread of where people are from and the different background they have. There is a predominance of people from Europe, Australia, and New Zealand. Then, North American representation is about one-third. And these are the number of dermatologists and these are the number of rheumatologists in the group. Robin, I am not quite sure what “other” represents, but we can talk about that later (laughter in audience). These are the countries that are represented in GRAPPA. These are some examples of the work projects that are underway and we will be hearing reports from a number of these today. Also, I think, most of you hopefully have seen the Annals of Rheumatic Disease supplement that came out in March 2005 published by Annals of Rheumatic Disease, which is free to download online if you do not have a copy, and in my presentation of the publications committee, I will give you that Web site. This is my last slide for the introduction. There has been a flurry of recent email exchanges. I apologize for those of you who speak German in the group, but I was particularly taken with this word from Josef Smolen’s last email. He introduced this word in the conversation and said that in German, it means “little diseases,” and the context was seeding ideas that grow into major projects and new learnings. Now, can someone who speaks German, Frank, do you want to make a comment on how this is used in German? Frank Behrens: . (from audience) Philip Mease: Oh, okay. I hardly would consider psoriatic arthritis that, but I kind of like the way I interpreted the term instead, so, sort of like the way Heidegger could make up new words, I like this word. Okay. So, Desiree, let us get you up here. II. Desiree van der Heijde: Radiology Committee Report I would like to apologize that I am unable to stay longer this afternoon, but at 2:00 the conference starts, and we are giving the first session, so it was not really my choice to be there in the first session. I would like to give you now an update on where we are with radiology scoring methods. We have formed a group of people who are interested in scoring x-rays of psoriatic arthritis and we will try to come up with some results that we can present at the next OMERACT meeting in May 2006. Just to remind you, there are four methods that have been described to be used in psoriatic arthritis. It is the modified Steinbrocker that was developed in Dafna’s group in Toronto. There is the score developed by the group in Ratingen, also formatted to score psoriatic arthritis. Then you have the method from John Sharp, which was adjusted to be used in psoriatic arthritis. My own modification is also adjusted for PsA. And they were all originally developed for rheumatoid arthritis and they were all tested and validated in rheumatoid arthritis. Then, later on, they were adjusted for use in psoriatic arthritis. One of the things that was adjusted was the testing of the DIPs of the hands, as a scoring site, as we all know, that involvement of the DIPs is important in psoriatic arthritis. There are several specific features in radiographs for psoriatic arthritis, so it is involvement of the DIPs and also the PIPs, and that is often in an asymmetric way and frequently in a ray pattern. So you see, DIP, PIP, also for example, MCP of the fourth digit, and not of the other digits. It can also be that you have just involvement of the wrist in one case, but in some cases, it is really symmetrical in a similar way to rheumatoid arthritis. Also, the features are different. So there is a combination of destruction and proliferation: destruction that leads to widening, osteolysis, and “pencil in cup” phenomenon, and the proliferation leads to proliferation of the shaft, usually of the metacarpal and tarsal, it can be close to the joints, and can also lead to ankylosis. And it can be a combination of all these different features at the same time in the same patient. If you compare which features are being scored in the four different methods, it all includes the films of hands and feet. The modified Steinbrocker is a global score, so it is taking all the damage, the proliferation, into account into one score, and the others are scoring specific features. The Ratingen score has a separate score for damage and for proliferation. So for a damage score, and a proliferation score, the original Sharp is including erosions and joint space narrowing and the van der Heijde modifications also erosions, joint space narrowing, but also taking malalignment into count, in the form of luxation and subluxation. The ranges are up to 160 for the modified Steinbrocker, up to 528 for the modified Sharp. These are the different aspects that we try to answer at the OMERACT meeting. For the four different methods, what is the truth? Does it measure what it should measure? Is it really an assessment of damage? Is it related to, for example, mortality or loss of function, or other aspects of outcome? We will focus mainly, on discrimination, and that means is it a reliable method? If it is repeated twice by the same observer or by two different observers, do you get the same results? Is it able to discriminate between groups of patients with severe disease and mild disease? But also, within patients, is it able to detect change over time, so sensitivity to change? And of course, feasibility is an important aspect. Several of the data are already available. I have shown that in a previous GRAPPA meeting, but still, a lot of these things need to be sorted out. Two of the methods have been applied in clinical trials and they have proven sensitive to change over relatively short periods of time. After 24 weeks, there was already significant difference between treatment groups and it was also seen after 52 weeks. It was also clear from those trial results that the addition of the DIPs did not help a lot in discrimination between the two treatment arms. So if you analyze the results without including the DIPs, you will see similar results. Also, the trial duration was too short to pick up change in “pencil in cup,” tuft resorption, periostitis, osteolysis. So all those features had been scored separately, but they did not add to the sensitivity to change because in that short period of time, we do not see those changes. It does not mean that these are not important, but it might be that you do not need them for a clinical trial to evaluate treatment efficacy. The plan for OMERACT 8 is that we score the radiographs of the Impact One trial by the four different methods. The Impact One trial is a trial where patients have been treated with infliximab or placebo. All the persons who are involved in the development of the various methods are also involved in this scoring exercise. We will focus on the test-retest reliability and the sensitivity to change and by applying the scoring methods, we also get information on feasibility. This plan is already there for over a year, but we have one big issue and that is that we do not get the films. And so it might be worth that GRAPPA could help us to really get the films so that we can start the project now because everyone is eager to start it and we really want to do it, but so far, we did not succeed in getting the films although they have been promised many, many times. This is what we would like to do for OMERACT 8 and I think we can do it, when we have the films, we really have nice results to show how these four different methods relate to each other. Thank you. Philip Mease: Why don’t you remain there, Desiree. John, do you and Robert want to come up? John, do you mind joining us up here? John Sharp: Carry on. Desiree van der Heijde: The results of the Impact Two trial will be presented on Friday morning, so then we can see the results of, again, one of the scoring methods. Philip Mease: So, Desiree, what is the process of getting the films, and maybe you can guide us through what the issues there are. Desiree van der Heijde: It is an investigator-driven study and so the people who did the study have to go back to the sites and ask for formal approval that we can use the films for this purpose. Philip Mease: Oh, so each of the sites has the films. It is not in the hands of the center. Desiree van der Heijde: No, in the meantime, the films have been digitized because they have been scored in a digitized way, so as soon as we have the permission to use them, we could start negotiating that we get the digitized images. Philip Mease: So it is in the hands of the individual investigators and not the company that sponsored this study. Desiree van der Heijde: No. It has nothing to do with sponsorship. Artie can help, I think. John Sharp? Artie Kavanaugh?: It is a study that, as everyone knows, Christian and I and several other people initiated, so we have the x-rays, as Desiree has said, and they have been digitized and we are trying to collect the second year, as possible, from some of the sites, and we can certainly talk about what to do with the films. Obviously, we did not want to have them distributed as a CD when you come in the door. We want to have a good plan and to know what to do with the data from them, but they are a very valuable resource and we have the clinical data and of course, sensitivity to change because it was as part of the clinical study. It is available, and we can talk. Philip Mease: Let us figure it out now. How should we go about helping in this process? What do you think? John Sharp: I am confused. Philip Mease: Getting the permission from the various—. John Sharp: No, we have the permission to use them. We will just talk about what to do with the actual x-rays. Philip Mease: Is there adequate support for the budget, financially? John Sharp: No. Desiree van der Heijde: No. There is no financial support so far. Philip Mease: What was the intent, in that regard? Desiree van der Heijde: Well, what do you have to offer? (laughter) John Sharp: All offers will be duly reviewed. Philip Mease: I am just curious, because I did not see it in the research proposals. Desiree van der Heijde: No, so far, the people who were involved to score the films said okay, we can do it as a research project. The problem might be in having the system to be able to score the films. Dafna Gladman: We have actually tried to negotiate some support from one of the companies that sponsored the trial. Even though we , what is necessary is to develop a reading system, a digitized reading system for the methods other than the modifications and that will require some doing. John Sharp: And there was support for the digitization process and in a weird testament to the state of clinical research, that cost more than actually doing the entire study itself, which we did as an investigator study, and mostly did it on the cheap, on the very cheap. That has been paid for, and they are digitized, and the clinical information is available. As you go forward, though, the time and resources are something we have to see about acquiring to really do it right. Philip Mease: Okay. So that is worthy of discussion. What are the pros and cons of getting other projects that are out there, that have x-rays? What are the hurdles of supplementing what you do with the Impact One with x-rays from other projects? Desiree van der Heijde: I think the only hurdle is the time involvement of the readers, in fact, if you could get access to more trials, then you have more data and we can base our conclusions on more data. So, I think most people would be interested, John and Dafna, to do that. Dafna Gladman: It might be worthwhile to try to get the set of x-rays from another trial that had a six month placebo arm because the sensitivity to change may be more noticeable the longer a placebo is available. But it is going to be the same hurdle—getting the digitized pictures and getting a digitized mechanism to read the x-rays for these methods other than the one that the xrays were read in in the first place. Desiree van der Heijde: But I think we can overcome that. We can make a data entry program to enter that in a separate computer as where you read the films. It is mainly to get the films, to have the images available. Robert Landewé: I think an important issue with regard to the choice of the databases, actually not the issue of expanding the number of patients, but careful selection of trial with patients that actually show signal, so sensitivity to change is a very important discriminatory aspect in terms of the OMERACT filter, and it should be able to judge the sensitivity to change. You can only do that if you have a sufficient number of patients that actually show signals, so that is an important criterion, I think, and that is a more important criterion than actually expanding the entire set of patients or trials. Desiree van der Heijde: So far, we have just selected Impact One because the films have been promised for a long time, so we knew we could get those. But if there are other trials available, then we would be more than happy to use also those films. (Unidentified): But what Robert said, Impact One had a hundred patients. What percentage do you expect, in terms of patients, and is that sufficient to make ? Desiree van der Heijde: Yes, because it has been shown as one of the methods that it was able to discriminate between placebo and infliximab. So if then— (Unidentified): But if it is made on only a very small minority of patients who show progress— Robert Landewé: That is not too important in this regard. Obviously for a clinical trial result and for discrimination between treatment arms, you need a sufficiently large group to show a difference, but in this regard, it is far more important to have the entire range of possible scores available so you can test the validity of the entire range. You can even do that with 20-30 patients, for example, instead of 150 as long as it is not 19 patients with zero scores and only one or two with positive scores. That is actually what I mean. So you are not limited to the entire database. You can easily make a selection. We did ankylosing spondylitis, for example, with a selection of a trial which included only how many pictures? Desiree van der Heijde: 20 patients, 4 time points. But here the interest is in comparing the four methods and then the Impact One is really a good trial and could be sufficient. Siegfried? Siegfried Wassenberg: As far as I know, the results of the Impact One trial did not show any difference between the trials. . Desiree van der Heijde: There was a change in the trial, but there was a positive change in a small number of patients, but there was a negative change in a larger proportion of patients so there is a change in the trial. Robert Landewé: Apart from that, I think you confuse discrimination with sensitivity to change. Sensitivity to change only says something about whether or not you can pick up the signal in relation to the level of noise. So sensitivity to change means signal to noise ratio. You only need a group in which you are sure that there is in this term, progression. If you want to know whether there is sufficient discrimination, so whether a method is able to discriminate between active treatment and for example, placebo, then you need the entire trial which should be sufficiently powered to actually demonstrate that change. So that is a subtle difference. Philip Mease: Do you think that you will be able to present this at OMERACT? I do not know about the time line here, so what do you think? Desiree van der Heijde: That really depends on when we get the films. If we get the films, let us say, early autumn, then it must really be possible to do that, yes. Robert Landewé: What we learned from AS was really the rate-limiting step was obtaining the x-rays and being able to present them to the readers. After that, it was three weeks of work and the entire exercise was finished. But obtaining the films and making them feasible to readers so they actually could start was the most important part. Philip Mease: How long does the analysis take? Desiree van der Heijde: It will take a bit longer here for 100 patients, but the analysis will be the shortest part. So if we have the results in three weeks’ time, it will take about three weeks, and we can present the data. Philip Mease: Let us say, for example, that you determine that adding the DIPs really made no difference at all, then might an example of a recommendation going forward then, just simply to be using the standard and not modified forms? Would you make it tentative and say we need to simply continue to try to observe more and thus include the DIPs? Desiree van der Heijde: I think that is dependent on the purpose of the use of the method. If you want to include it in a short-term clinical trial, that might be the conclusion: that you do not need the DIPs, that you do not need the score for osteolysis, “pencil in cup,” etc. But for face validity and for long-term studies, you really need those. So it might be that we come up with two different conclusions. This is best for clinical trials, this is the best one for observational studies, correlation with physical function, etc. Philip Mease: Other questions or comments? Will Taylor: This is not much useful for the sensitivity to change, Christian, but the CASPAR project has a lot of digitalized images, as well, of about 500 patients, so in terms of doing testretest reliability study, that is a source that is available, too. Desiree van der Heijde: Mm-hmm. And they all have the diagnosis of psoriatic arthritis? Will Taylor: Yes. Desiree van der Heijde: Those 500 have the diagnosis? Philip Mease: Right. There are 535 or so PsA patients and a similar number of control rheumatic disease patients. (Unidentified): Yes, but not all with digitized images. About half to two-thirds have. (Unidentified): No, but if you have two-thirds of the cases and you have the possibility to select on the level of damage, then it is worth the effort to see whether it is possible. Desiree van der Heijde: This will give you information on the truth aspect, so that you could correlate the level of damage is the physical function what I believe you also have and the clinical disease activity so that will be a different aspect of the OMERACT filter, that can be very useful to add that and that could also answer the question of when and in which situation do you want to include the DIPs and the “pencil in cup,” etc. So it could be very useful to discuss that. It is a very good suggestion. (Unidentified): . (comment from audience) Mark Weinberg: Desiree, I am not sure about the autumn time frame, but there will be data presented on Friday from the Abbott study with adalimumab which is 300 patients with films that are digitized. So we should talk. That might be able to be added to that set you want to look at. Desiree van der Heijde: Wonderful. Thank you. Philip Mease: Boy, you did not realize how much additional films you might have your hands on. Desiree van der Heijde: Great! I think we start next week! Philip Mease: Thank you very much. Desiree van der Heijde: You are welcome. (applause) Philip Mease: So, just a couple of housekeeping details. Doug, apparently there is food en route and there are refreshments out there, so if people want to go a little bit at a time to get refreshments, that is fine, but the food is coming shortly. So let us go to the next. One other comment to make is that in order to record this effectively and have a transcript for posting on the GRAPPA web site, it would be helpful if you can think to walk over to the microphone to make comments, ask questions. Do not be shy about going to the microphone. Unfortunately, we do not have a sophisticated microphone system as we have had in other meetings. So the next section will be the CASPAR review led by both Will Taylor and Philip Helliwell. Philip, why don’t you come on up here and sit at the front table just so that it is more efficient that way? III. Will Taylor: CASPAR Update Philip, did you want to start, or should I just crack on? Philip Helliwell: You might as well crack on, then. Will Taylor: It is really nice to be able to finally present the results of the CASPAR study. I will be presenting the results of the study to the main meeting on Friday morning. But as you will see, there is quite a bit of important discussion before we finally perhaps understand what the results mean and so that discussion would be very nice to incorporate into the final presentation on Friday. I am really doing this on behalf of many of you who are in this audience, the CASPAR collaborators: 30 rheumatologists in 13 different countries. The starting point for the study was that there was really no agreed classification criteria for distinguishing between psoriatic arthritis and non-psoriatic arthritis and although there have been seven different proposals for classification criteria, none had been adequately validated. It is important to emphasize that when I am talking about classification criteria, I am talking about the criteria that distinguishes between psoriatic arthritis and non-psoriatic arthritis, particularly distinguishing between groups of patients with these diseases rather than making the diagnosis in an individual patient. Although classification criteria are quite useful rules of thumb or for teaching purposes, they are really designed for groups of patients rather than individuals. The second point is that in psoriatic arthritis in particular, there is a bit of confusion between what classification means in the sense that it can also refer to sub-group classification within the disease of psoriatic arthritis. I am not talking about that, but the data within CASPAR can be analyzed with that question in mind and Philip might want to talk about that. My presentation is primarily about diagnosis. These are the seven classification criteria. I do not really have time to go into the details of each one. I just make the point that although there are quite a lot of similarities between the criteria, there are also quite a lot of differences. For instance, the presence of radiological features in some criteria but not others; whether psoriasis itself has to be present or whether a family history of psoriasis would suffice is also different amongst the criteria. There is one criterion that requires HLA analysis. I have attempted to summarize in quite a busy slide, some of these issues. I am not sure that is particularly legible. Some of the criteria are very complex; some are very simple. In 2001, the CASPAR group got together, principally at a meeting at the ILAR conference in Toronto, although it had initially been set up by a group of European investigators in psoriatic arthritis during 2000, but it later on expanded to encompass a worldwide perspective. So the aim of the project was two-fold. Firstly, to directly compare the test performance characteristics of the existing criteria, and then to see, secondly, whether a new criteria that could be developed directly from the data would be more accurate than existing criteria. And when I am talking about test performance characteristics, I am really talking about sensitivity and specificity. The design of the study really reflected what our main purpose for these criteria would be, which is essentially, to form a case definition for enrollment in clinical trials or intervention studies so that we enrolled consecutive patients who had a clinic diagnosis of psoriatic arthritis and consecutive patients with other inflammatory arthritides. So the control patients were patients with inflammatory arthritis. There were not normals. There were not patients with other diseases. There were not patients with other skin diseases. They were patients with inflammatory arthritis and that is quite important when we think about how the criteria could be applied in the future. We made a sample size calculation based on a correlated Chi square statistic to distinguish two percentage points between the specificity of two competing criteria and we used the gold standard of diagnosis, being the physician’s diagnosis in the clinic. As I will show later, we validated that gold standard against a couple of external criteria. The data were collected over a two year period between February 2002 and March of last year. We collected quite a lot of data on patients - over 50 clinical, laboratory, and radiologic variables. We measured anti-CCP in many of the patients and HLA analysis is to be performed at some stage. Although we have extracted DNA, we do not have the results of that particular test at this time. X-rays, as you have heard before, were mostly digitized, but if not, were sent as hard copies and read blindly by two readers in tandem, one of whom was a musculoskeletal radiologist. The gold standard of diagnosis was validated in two ways. The first way was to use a data quality committee to examine a random selection of case records to check that the diagnosis was correct. The second way was to use a statistical modeling technique called latent class analysis. Then we derived new criteria using two quite different statistical methods. Classification and regression tree methods and logistical regression. So there were 588 patients with psoriatic arthritis and 536 control patients. About 70% of the controls had rheumatoid arthritis and you can see the other diseases there: ankylosing spondylitis, undifferentiated arthritis, connective tissue diseases, and some others. But most of that cohort, 70% were rheumatoid arthritis. The age was a little younger in the psoriatic arthritis cohort and more of the psoriatic arthritis cohort was male, which is what you would expect from the demographic of that particular disease. 4.6% of the psoriatic arthritis group were rheumatoid factor positive, compared to 57% of the controls. CCP antibodies were found in 7.6% of psoriatic arthritis patients. The psoriatic arthritis patients had relatively mild skin disease; the median PASI score there was only 2.15. This is the main slide to show how the different classification criteria compare and what I have shown here in the yellow bars is the portion of patients who were unable to be classified, usually because of missing data. You can see that this is really a problem for the Fournie criteria because this criteria relies upon HLA analysis as part of the method. Because HLA levels were not available, 32% of patients could not be classified by that method. In the blue bars is the sensitivity and you can see that all the criteria are pretty sensitive, apart from the ESSG and the Bennett criteria. And in the purple bars or the red bars, is the specificity. All the criteria were generally very specific, above 90%. And then I have shown a single index of discrimination called the diagnostic odds ratio which is a means of combining the sensitivity and specificity into a single index. That is plotted along this scale, a log scale and you can see that the best combination of sensitivity and specificity as expressed by the diagnostic odds ratio is the Vasey criteria. Now the next thing we had to do was to see whether any differences in sensitivity or specificity were statistically significant and to do this, we performed a conditional logistic regression analysis, essentially to demonstrate the odds of true positives amongst cases or false positives amongst controls. So this slide shows the comparison of specificity, reference criteria being the Vasey and Espinosa criteria, which has an odds ratio of one and along here is the odds ratio for the false positive rate. So the criteria that have an odds ratio of greater than one show a worse specificity than the Vasey and Espinosa criteria. Those criteria that had an odds ratio of less than one has a better specificity. So we can see that the Bennett criteria was more specific than Vasey and Espinosa whereas the McGonagle and ESSG criteria had a worse specificity and the Gladman criteria and the Moll and Wright criteria were statistically the same. We did that amongst cases of psoriatic arthritis to demonstrate sensitivity. This time, the way that the odds ratios work are reversed so that better sensitivity is now above the line and worse sensitivity is below the line and you can see that in reference to Vasey and Espinosa, all the other criteria have a worse sensitivity apart from McGonagle, which was statistically the same. So, at this stage, it seemed that the Vasey and Espinosa criteria indeed had the best combination of sensitivity and specificity and was better than the others. We then looked at whether we could really trust that the criterion standard, the gold standard of physician diagnosis, and the first way was using data quality control methods, so 1% of the case record forms were randomly selected and examined by a data committee and only one control was reclassified as psoriatic arthritis by that examination. The second approach to validate the gold standard was to use a statistical modeling technique called latent class analysis. Now, this approach is mathematically a little difficult to comprehend, I have to say, but essentially, it assumes that each of the methods, each of the criteria, the six or seven criteria, classify patients into psoriatic arthritis or non-psoriatic arthritis with different degrees of error. The distribution of how those criteria agree with each other can be used to develop a model of clusters. So it is kind of a form of cluster analysis using the distribution of the results from the different criteria. So, using that modeling approach, it was possible to re-classify all of the subjects in the study, and there was very high agreement between the statistical model and the physician’s diagnosis with a kappa of 0.96. We were able to determine the sensitivity and specificity of each of the criteria based on that statistical model or the way the model classified the patient and essentially, it shows a fairly similar pattern. Although the numbers are not identical, the pattern of sensitivity and specificity is very similar to how a clinical diagnosis is used. Since the Vasey and Espinosa seemed to come out the best, I thought it would be important to examine what the content of the Vasey and Espinosa criteria are in a bit more detail. There needed to be a mandatory involvement of psoriasis, either skin or nail disease, plus one other feature, either in the peripheral pattern group or a spinal pattern group. So you can see that you could have radiological features and that would be enough, or clinical features would be enough to classify a patient as psoriatic arthritis. The next thing we wanted to do was to see if we could derive a better classification criteria and the first statistical approach to identify useful items that would contribute to that criteria was this approach called classification and regression tree, or CART analysis. This is being used in other classification problems, particularly the rheumatoid arthritis original classification paper produced an alternative to the traditional RA classification criteria using this CART approach. Basically, it splits the data into progressively purer and purer groups using the best discriminating variables in a sort of iterative way, building a very large tree, until the groups can be split no longer and then tree is progressively pruned back by the software until there is a balance between the complexity of the tree and the accuracy of the tree. Now in the event with the CART analysis, there are only two variables that were selected as being important for the diagnosis: basically the presence of psoriasis: history of psoriasis or current psoriasis. And those two variables together have a specificity of 96.8% and a sensitivity of 96.1%. Now one of the other things that CART analysis can do is to look at what would happen if those variables were missing, for whatever reason, and so it specifies surrogate variables that could used in place of the presence or absence of psoriasis if for some hypothetical reason, that data was not available. Those are the variables that the algorithms selected: nail dystrophy, family history, dactylitis, and rheumatoid factor being negative. Philip Mease: Family history of psoriasis or psoriatic arthritis? Will Taylor: Psoriasis. So the definition was a second-degree relative. Dafna Gladman: The patients all had an inflammatory arthritis? Will Taylor: Correct. Dafna Gladman: So, it is an inflammatory arthritis in the presence of psoriasis? Will Taylor: Yes. The second way that we looked at which variables were important in discriminating between psoriatic arthritis and non-psoriatic arthritis was logistic regression which looks at the independent contribution of variables. There were 26 clinical and laboratory variables and 18 different radiologic variables in this analysis and only these ones shown were selected as being independently predictive or independently discriminating between psoriatic arthritis and non-psoriatic arthritis. So, again, rheumatoid factor-negative, dactylitis, either current dactylitis or history of dactylitis, history of psoriasis, family history of psoriasis, current psoriasis, and one radiologic feature which was juxtaarticular and new bone formation. What the table shows is the univariate analysis, so just looking at the raw sensitivity and specificity of each of those items, and then in the multivariate logistic regression, it shows the odds ratios for each of those variables. So, that actually overlapped quite a lot with the CART analysis, which was reassuring. We had two quite different statistical techniques basically telling us the same variables were important in the diagnosis of psoriatic arthritis. So we decided to combine those variables in a fairly simple way. Basically, using these eight items as defined here, just adding them together. We did not use any kind of weighting that might have been suggested by the odds ratios from the logistic regression analysis mainly because we felt the numerical value of the odds ratio is likely to be very sample-specific, and so to get around that, we simply combined these variables together in a simple way by just adding them together. We then performed a ROC analysis or a received or operating characteristic curve which basically plots the false-positive rate or one minus specificity against the true positive rate or the sensitivity by the number of items that were present. You can see that this is a very accurate approach. The area under the curve gives an idea of the discriminating power of the classification set. A perfect diagnostic test, for instance, would follow a curve that goes up and across and you see most diagnostic tests need to have that kind of curve like this. So an area under the curve of one is the perfect test. This area under the curve was 0.99. We selected a cut point here which were three or more of those items being present and that gave a sensitivity of 93% and a specificity of nearly 99%. We could have selected that cut point, which is two or more items; that would have been a more sensitive test, but a less specific one. (Unidentified): Can I ask you what you used as your rheumatoid factor-negative cut-off? (from audience) Will Taylor: The rheumatoid factors were done locally by each clinic and so we did not actually request what the titer was. It was just dependent on what the local laboratory used as their cut-off for positivity. Philip Helliwell: But we did say not Rose-Waaler or latex so preferably some other test such as ELISA or nephelometry. (from audience) (Unidentified): And it gives you a latex positive, then you are CCP-positive, the same thinking. (from audience) Philip Helliwell: They probably all correlate. We are not presenting that data, but they more or less are. Will Taylor: We actually found a lot more psoriatic arthritis patients being CCP-positive than were a rheumatoid factor-positive. So 7.6% were CCP-positive versus 4.6%, so nearly twice, and that was using a cut-off of 20 units for the CCP test. You will see that the criteria here are written, and the items within the criteria are written in a kind of a dependent way so that you cannot score for history of psoriasis if current psoriasis is present and you cannot score for family history of psoriasis if current psoriasis or history of psoriasis is present. Similarly, for dactylitis, you cannot get two for having current dactylitis and a past history of dactylitis. So this is the final version of the CASPAR criteria. Bear it in mind that all the patients had inflammatory arthritis; that was the first mandatory criteria that they had to have inflammatory musculoskeletal disease with three or more of the following. In conclusion, the CASPAR study is a relatively robust design. We had a large sample that could distinguish quite small differences in specificity and sensitivity between competing criteria. We had 13 centers which would tend to reduce any kind of diagnostic bias that might be present in one or two centers. Subjects were unselected consecutive clinic attendees. We validated the gold standard of diagnosis. We examined a large number of potential items that could contribute to the diagnosis of psoriatic arthritis, and we used a convergence between different statistical approaches rather than relying on just one. But it is important to note that the control population in this study does limit where the results can be applied. We cannot really apply the criteria to early disease, for instance, because only 4% of patients or so had disease duration of less than 12 months and the mean disease duration was around 12 or 13 years. We also cannot apply the criteria to non-rheumatic disease populations, so for general epidemiology in a community population or in a dermatology clinic, for instance, further studies need to be done to see what the specificity of these criteria would be in those populations. We do think that the CASPAR criteria are simple, they are highly specific, they are derived from observed patient data, and we feel that these could represent a new standard for case definition for the context of clinical trials. (applause) Philip Mease: Wonderful, Will. We are open for questions now. Paul (?): One to begin with—in the U.K., actually, it is quite useful not to have too strict criteria for psoriatic arthritis. There is an enormous number of people now who seem to have psoriasis and rheumatoid that we like to include in that group rather than psoriatics because of the lack of availability of funding for anti-TNF therapy. My serious point was actually to do with HLA typing. I think it is quite a good time to bring it up and you mentioned that one of these studies has used HLA criteria for the classification and I wondered whether there is a general feeling in the room about what the most useful HLA typing to be done. Clearly, you have not got a homogenous population in this CASPAR study, ethnically, so there are issues about what one should do in relation to HLA typing. What one feels are the most important things to do, whether, indeed, it is actually an essential thing to do, and I would be interested in general thoughts on that. Will Taylor: My feeling is that very limited HLA analysis would be important so that we can properly evaluate the Fournie criteria. Essentially, we could not really do justice to the Fournie criteria in this analysis. And the item within the Fournie criteria is B16 or 17, so it is a very simple class to analyze. Now, if you wanted to use the data for any further kind of genetic studies, then that is a different issue. Perhaps you would like to address that, Philip? Philip Helliwell: No, I just wanted to add that my particular interest in doing HLA studies in this group was to try and look at the purity of our sample of polyarticular psoriatics, as many of you have heard me rattle on about this before, that I believe that maybe we have been overdiagnosing psoriatic arthritis because of the way that the subgroups have changed since Moll and Wright originally described it. So my particular interest here is just to look at the HLA typing in the particular subgroups to make sure we were getting pure subgroups of psoriatic arthritis and not mixing them with rheumatoid. I think there are lots of other possibilities and Paul and I have already discussed them. I know that Dafna wants to say something here. Dafna Gladman: My comment is that there are a number of HLA alleles that are associated with psoriasis and psoriatic arthritis and I think to look at this population and not look at those alleles that are known to be associated would be kind of a waste of time. Once you are putting it, I do not know exactly how you are doing it, but if you are putting it on a— Paul (?): The problem is, you have not got an ethnically matched, control group, necessarily, to judge the frequency of alleles against. Dafna Gladman: That is correct, except that your control group in general, comes from the same area where the patients came from, so my 40 psoriatic arthritis patients would be compared with 40 patients with non-psoriatic arthritis who came from the same area. So I think that in terms of the prevalence of different alleles, it may be kind of a wash-out if you find the alleles that are associated with psoriasis and psoriatic arthritis. I agree that in the Fournie criteria, they were looking at antigens, not alleles. They were looking at B27, B16, B17. Well, now you are going to have to look at B38, B39, you going to have to look at B57 and 58— Paul (?): The problem with B38 and B39 is that you only actually have a chance at finding a massive population because the effect is so weak. The genetic effects associated with B38 and B39 have never been really proven, simply because we have not done the studies in many hundreds of patients that are required to do it beyond any reasonable doubt. Dafna Gladman: One of the problems is, it depends on the population you are selecting, you know. In some populations, it is B38, and in others it is B39. But certainly B57 and B58 is associated with psoriasis and psoriatic arthritis. The other thing that I think is relevant is CW6 which has come up as important, and it may very well be that CW12 may be associated with psoriatic arthritis as well. Now, in terms of DR4, we have actually shown that DR4 in psoriatic arthritis, therefore, is similar to rheumatoid arthritis, but it not necessarily the same DR4 allele. In rheumatoid arthritis, the majority are O41, O44. In psoriatic arthritis, there is increased frequency of O42, at least in the Canadian cohort. So I do not know if one wants to go into that kind of detail. If you wanted to respond to Philip’s question as to whether or not these are rheumatoids— Paul (?): That does also, actually, beg the question in an emigrant population as to whether there is a big population stratification phase. It is possible and that may be a Jewish influence. Dafna Gladman: The O42? Paul (?): Yeah. Dafna Gladman: Could be, but I do not think so. Philip Mease: Let us see. There are three hands—one at the mic and then two hands raised, Hans, at the mic? Hans Zmierczak: If you look at HLA, you have to be very careful with the control groups. It is not sufficient to look only at the HLA pattern in an area of patients and controls, it is also important to look at patients with psoriasis without psoriatic arthritis. This is one of the problems of the past, that that has not been done. So you need this psoriatic control group without arthritis. Philip Mease: That is an excellent, excellent question. Philip, what is your thought about that? Philip Helliwell: I would not disagree with Hans has said, but I am really keen that we do not spend the whole of our discussion time on what HLA testing we are going to do in this group because I do not think that in the end of the day, it will come to view to the new criteria. I would really be interested to hear any comments on the proposed criteria that we have put out there. I think we may have one of you now. (Unidentified): No, no, it is just that I agree. I think that genetics is a completely separate issue and I do not think it is going to contribute to the work that you have done and I have to congratulate both of you for a fantastic effort, really, in coming up with these criteria. It is really quite a major achievement, I think. My question related to, if you have had a chance of looking, getting back to the rheumatoid factor and anti-CCP, my concern was relying on physicians’ gold standard for diagnosing of psoriatic arthritis and wondered whether those patients had a chance to go back and see whether the physician was wrong and they are patients with an inflammatory arthritis coincident psoriasis but have other features of just the rheumatoid. Have you looked at— Will Taylor: Yeah, we have had a look at the CCP-positive psoriatics, and quite a large proportion of them, I cannot remember the exact numbers, but a large proportion of them have other characteristic features of psoriatic arthritis like dactylitis and the radiological features in the same kind of proportion as the CCP-negative psoriatic arthritis patients. Philip Helliwell: Yeah, I have spent the last three weeks trying to get some meaningful data out of this set that regards this polyarticular psoriatic subgroup, and any way I look at it, or divide it up, they all look psoriatic, true-bill psoriatics. None of them, well, maybe a handful, look as though they may be rheumatoid. The CCP-positivity just tells us that they group with the nonpolypsoriatics. It has been helpful and illuminating, I think. Philip Mease: One quick point there is that I recently was asked to review a paper from a pure psoriasis group which showed elevated frequency of CCP and it also could be that there are different forms of CCP present, that there are different reactivities or different forms of filigrin that it is reacting to that might distinguish from psoriasis CCP from rheumatoid factor CCP which may be pertinent here in terms of the positive CCP that we are seeing in this group. Will Taylor: You might be interested in this curve which looked at the different titers of CCP to see whether the cut-off was different, perhaps, in psoriatic arthritis. We plotted again false positive rate against sensitivity with the different titers of CCP defining positivity. This is the conventional manufacturer’s guide, greater than 20 units that gave us the sensitivity of 54% and specificity of 92% for negative test. If we increase the level of CCP required to make a positive diagnosis, you still get, it does not improve the specificity by that much. So increasing the rigor of the CCP test does not help a great deal, either. Philip Mease: Doug. Doug Veale: Question actually—the fact that the rheumatoid factor negative has made it, if you like, as a classification criteria, suggests that there is a difference between the rheumatoid factor positive people and the anti-CCP positive people, is that right? Will Taylor: Yeah. Well, it means that firstly, not as many of the control patients were CCP positive, rather more were rheumatoid factor positive, and less of the psoriatics were rheumatoid factor negative than were CCP negative. Doug Veale: Oh, I was just trying to work out what it is telling us that there are less rheumatoid factor positive than anti-CCP positive and that rheumatoid factor negative is a discriminating criteria. Will Taylor: That is correct. Doug Veale: What is that telling us about the patients who were rheumatoid factor positive? Will Taylor: I am sorry. I did not understand that question. Doug Veale: There was 4.6% of patients who were rheumatoid factor positive. So what do we know about them? What is it telling us that there is a difference between rheumatoid factor positive and the anti-CCP positive and that rheumatoid factor negative still makes it as a criterion for the actual classification? Will Taylor: I think it is telling us that CCP in psoriatic arthritis is not as useful a test as it has been made out to be for diagnosing rheumatoid arthritis. Doug Veale: And what is it telling us about the rheumatoid factor positive patients? Will Taylor: Well again, we looked at those patients and they were fairly typical psoriatic arthritis as well and the baseline frequency of rheumatoid factor is not a million miles away from 4%. Philip Helliwell: We have asked ourselves the same questions, I think. Perhaps not exactly the same ways you have just put it. But there is no way that I convinced myself yet that these patients are any different based on their serology. Doug Veale: Do not get me wrong. I like what I see in a sense that it confirms a lot of what we have been doing for a long time. I have a slight problem in this, while I would accept the rheumatoid factor negative as being a criterion, I have always believed it, and I can see the sense in what you are presenting. But then how do you square that with the fact that there was 4% rheumatoid factor positive. Will Taylor: Well, it is not mandatory. If we go back to the criteria, you only need three. Doug Veale: Yes. Sure. It is only one. Will Taylor: And only one of those is rheumatoid factor negative, so it is perfectly possible to have— Philip Helliwell: So all your patients could be rheumatoid factor positive and still actually meet the criteria. Will Taylor: And as you say, the criteria kind of feel intuitively right. For instance, it is possible not to have psoriasis present to make a diagnosis based on this criteria as long as you have a family history or if you have very characteristic radiological signs. And also, kind of highlights the importance of dactylitis in the mix which, I think we would agree, is a very typical feature of psoriatic arthritis. Philip Helliwell: I thought perhaps there would have been more discussion about the stems to these criteria. In fact, the criteria for admission to this study was inflammatory arthritis, but 21 of our psoriatic cases did not have any peripheral joint involvement. (Unidentified): How many? (from audience) Philip Helliwell: 21 out of 588. (Unidentified): At the moment ? (from audience) Philip Helliwell: Ever. (Unidentified): Ever. That is quite a small number. You would expect more, really. Philip Helliwell: So that is why we are including enthesial. So if you have got enthesial pain, you can get in on that basis. (Unidentified): If you are going look at the stems, we looked at a group of 100 or so peripheral psoriatic arthritis diagnosed by our less good criteria and 30% of those had asymptomatic, often, evidence of sacroiliitis on MRI scanning, for example, and one could imagine that that might be a useful diagnostic addition. Because I do not think you see that in rheumatoid, for example. Will Taylor: I think that including MRI is something kind of beyond the scope of this criteria. I think to include MRI specifically, is asking a bit too much of a simple straightforward classification criteria. By all means, in the individual patient, MRI can be very useful. But I want to, again, underline the importance of the issue, discriminating between groups of patients and making an individual patient’s diagnosis. Philip Mease: Front mic, and then I wanted to mention both to Dominique and Kurt de Vlan, who have sat down again, do not give up. If you have comments to make, please so. So, front mic— Morton Scheinberg: How high was the elevated frequency of your pure psoriasis patients on the paper that you were reviewing? Philip Mease: I cannot remember that actual number. It was in the teens, as I recall. But the point that was made in the paper is that you have got the antigen generating elements in the epidermis, and so not to forget the epidermis in this regard. Morton Scheinberg: You would consider close to 10% in elevation of frequency? Philip Mease: It was in that order, I just cannot remember the exact number. And these were patients who, theoretically, did not have psoriatic arthritis, although one of my criticisms of the paper was that there was no rheumatologist involved in reviewing the patients. Morton Scheinberg: On the CCP issue, there are two scenarios that one would have to apply for interpretation. The time that you are doing the CCP assay, and how long does the patient have the disease. If you do this in a rheumatoid, well-known population, you go for 95-98% specificity. But you will get an 80% sensitivity. If you are doing this on an earlier , you will get 20% sensitivity and you will get a very high specificity. So it depends on the timing. So applying this to psoriatic arthritis is very helpful and if you get something like 20-25% or something, that is meaningful. If you get below 10%, some JRAs also have below 10%, so one has to be careful with the timing that you are using this and how to interpret this. We published a paper less than two years ago in the Annals of Internal Medicine. We got almost 90% of rheumatoid patients that were anti-CCP positive. But those are those patients with a mean disease duration of over 10 years. Everybody knew they had rheumatoid arthritis. So that is not how you have to use the test. So putting that on the criteria may be very helpful. Philip Mease: Kurt. Kurt de Vlam: Can you exclude any selection bias on the rheumatoid factor because patients were selected on expert opinion basis? Some of us can use rheumatoid factor or negativity as a kind of diagnostic feature. Will Taylor: Well, looking at the rate of psoriasis amongst the control patients, for instance, is a kind of marker for selection bias, perhaps, in the controls. There were about 2% of the control patients with psoriasis. So that would be kind of in the same ballpark as the population frequency of psoriasis, which would suggest that the controls were not being selected. For the cases, I guess all we can really rely on is the two validation steps for validating the diagnostic gold standard. Several of the classification criteria that we used to model the clusters do not include rheumatoid factor as a necessary criterion, so I guess that is the only way I can answer your question, Kurt. Philip Mease: Herman. Herman Mielants: Well, first of all, I want to congratulate you for your work. It is excellent work. There is still the main problem I have with this criteria is definition of inflammatory musculoskeletal disease. Will Taylor: Yes. Herman Mielants: What does it mean? Arthritis, or arthralgia? For the spine, do you use the Calin criteria, or not the Calin? In ASAS we are renewing the definition of inflammatory spinal disease. It has to be a definition. Will Taylor: I think you are right, Herman. There is a lot of uncertainty in my mind how we defined this initial mandatory criteria. I think the data can tell us this because it was a precondition for entry that patients had inflammatory arthritis. So, it may be more sensible to have an initial criterion that just simply says, inflammatory arthritis. That may then exclude patients with enthesial only or spinal only symptoms. In many ways, I feel that because the remainder of the criteria are very specific, I think that it does not matter so much that the entry into the application of the criteria be very broad and keeping it kind of vague and ill-defined may not necessarily be a bad thing. I am very interested to hear what others say. Herman Mielants: The patients with psoriasis and has osteoarthritic back pain in inflammatory periods, would he be classified— Philip Helliwell: Well, he has only got two of the three criteria. He only has two there, so he would not be classified as psoriatic arthritis. Will Taylor: The patient only has one. If you have inflammatory back pain, that gets you in. But then you have got to have three. If they have only got psoriasis as one of those three, then they do not have psoriatic arthritis. Dafna Gladman: Well, they might have a negative rheumatoid factor. Will Taylor: Okay, if they have a negative rheumatoid factor, then they have two. So they still do not have three. Philip Helliwell: It is worth saying that these are not diagnostic criteria; they are classifications. I have thought long and hard about this after Will came up with it, and I am sure he is right. This reflects what was included in the study, that patients that were included in the study, both those with and those without peripheral joint involvement and spinal involvement. So I think Will is right in putting that first. Philip Mease: Let us have room for—. How many people are still having comments? One, two three, four, it looks like. Let us make brief comments and we will try to draw this to a close in about four or five minutes. Daniel Aletaha: My comment is really a minor comment and a rather cosmetic comment. I have the feeling that items one, two and three can give you only one point in your criteria, and the same thing with current dactylitis and history of dactylitis. So if you would combine them in one item, then your criteria would go down to five items and I think that would be an aspect to make them even more simple and if you present them, people would like them more. Will Taylor: Yeah, I think that is a really interesting point. In fact, I did that, but having fewer items meant that they were less discriminating. So the actual test performance was less good when you had fewer items. Having only five items rather than eight items actually made it less discriminating. Daniel Aletaha: My main point is you could say item one is current or past psoriasis or family history of psoriasis. And it would give you one if one of these is true, and it still can give you one if you have all three. Will Taylor: Yes, I understand that. Daniel Aletaha: I am not sure that this is affecting your discriminating power. Will Taylor: Yes, it did. Dafna Gladman: Once you have generated your list from your analysis, the rest is, like he said, cosmetic. It is just a matter of presentation. Will Taylor: In fact, it was more than cosmetic because when I actually tested that approach by having a shorter list, same number of items within the list, but presented in a different way, actually less discriminating. Philip Helliwell: You would have had to score two out of five. Will Taylor: Yes, because you cannot get kind of two and a half. Proton Rahman: I just had a question about the family history. So I certainly agree for it to be there, I am just wondering how good would patients be about a family history of psoriasis and whether we can actually get a little more specific if you look for a family history under the age of 40 since those are the ones that are more familial and are likely to have a family history? Will Taylor: That is a nice research question, but the data cannot answer that question because we did not collect enough information about what the family history meant. Alberto Cauli: Just a simple example: if you have got a patient with inflammatory oligoarticular arthritis, psoriasis, and seronegativity for the rheumatoid factor, is does not fulfill CASPAR criteria? Only arthritis, psoriasis, and negative rheumatoid factor. Will Taylor: That is correct. Alberto Cauli: That is a bit strange, isn’t it? Will Taylor: Not really, I mean, it makes it extremely specific criteria. Alberto Cauli: Oligoarticular— Philip Mease: You have got to take an x-ray, keep looking. Alberto Cauli: Okay. (applause) Dafna Gladman: While Philip is getting ready there, I wanted once again to thank Philip Helliwell and Will Taylor for getting together the CASPAR group. You have to realize how many people were involved. You saw the list of the countries—how many people were involved in this, and to put this all together was a mammoth exercise, so thanks once again. Philip Mease: My congratulations, too. It was a huge enterprise. Thanks. And I expect we will hear more about this as this is looked at more carefully over time. One housekeeping detail is that these slides from the whole afternoon will be available on the GRAPPA intranet site. I notice that some people are taking pictures, so after the EULAR meeting, these will be available. If any of you do not have a password into the intranet site or know how to get into the site, ask Robin Shapiro, who is our executive director for that information and she will get you signed up for it. So next is the discussion about treatment guidelines led by Artie Kavanaugh and Chris Ritchlin, which should be a rich discussion based on the evidence of the email traffic over the last several months. IV. Artie Kavanaugh, Chris Ritchlin: Treatment Guidelines Update / Consensus Discussion Artie Kavanaugh: All right. As we are getting our materials all ready, as Philip has said, it was a very active discussion, so I am thinking that we will have a very good and a very useful discussion at the end of our presentation. What we would like to do is to catch up. Again, what we are trying to do is to come up with GRAPPA treatment guidelines. We will catch up on the process that we had gone through to date, and some of this we talked about at the ACR meetings, and we talked about it last year at EULAR, to present a little bit of the data. If you will bear with us, we are going to show you snapshots, different people had been involved in doing different projects to look at the actual data as far as what evidence is there. Because we wanted the guidelines to be as evidence-based as possible, what evidence was there out there, and you will see and definitely recognize the good contributions by all of the GRAPPA members who volunteered to undertake this. But we will go through that kind of quickly, and afterwards, we will have these slides available, and the papers we will try to get available as quickly as we can from the individual contributors who did this to be able to share with the larger group and to review those. But let us not get tied down with arguing the points of the data, except if it is something very specific because then, I think, we will have to get to the more difficult part, and that is: how do we bring these together? How do we synthesize these into treatment guidelines? So, with that as a start, Chris and I will go back and forth, sharing the chair for this. Just to remember what we are trying to do: to develop guidelines based upon the best scientific evidence. I think one of the things that we will see and we had sort of known beforehand, but now having rigorously gone through the exercise of really extracting all the data, there are many, many gaps. There is a lot information that is not there; something, again, that we need to talk about as a group. What are guidelines? Systematically developed statements to assist practitioners and patient decisions about appropriate healthcare for specific clinical circumstances. So some of these slides are old—we had shown these last year, but just to refresh and catch us up and really begin the discussion, issues of course that you heard about in the CASPAR presentation, that the disease can be heterogeneous, the course can be clinically variable. Obviously the great work from CASPAR is going to be very relevant as you just heard especially for subsetting, to get to issues of prognosis. Psoriatic arthritis is multifaceted and one of the things that we are going to struggle with today and as we put these guidelines together is how best to synthesize distinct levels of involvement in distinct parts of the body. Last year, one of the things that we got consensus on was about the extrapolation from other areas. To very briefly recap the voting that we had at the ACR, most people felt it was acceptable in the absence of specific evidence that spoke to psoriatic arthritis, to extrapolate from similar conditions, specifically in terms of the spondylitic involvement, enthesopathy, and dactylitis, and for skin in terms of psoriasis. So that was generally agreed upon and was, I think, a strong consensus, that if there is nothing specific in psoriatic arthritis, we could, for example, use data in psoriasis to speak to that facet of the disease. Of course, we need to do more with the outcome measures, not just we heard a lot about the xrays, but also for the work in signs and symptoms and the measures that we will use to measure these. And, of course, we know that a lot of the interest in this is driven by the fact that we have newer therapeutics. That is partly why there is such excitement, and also part of our challenge as we think about the data that we have today, we do have to come up with useful guidelines. I think the GRAPPA guidelines should be as scientifically based as possible, and then the question is, how far do we want to go in terms of extrapolating as we get to synthesizing the different facets of disease? Some questions, and these are the things we will have to wrestle with: what do we do when the state of the art outstrips peer-reviewed published literature? And I think also at the ACR last year, there was consensus that if something was presented at a scientific meeting, a large, for example, double-blind placebo-controlled trial, that we should have that as evidence that we could be willing to incorporate, knowing that it may not get into the published literature for some months. What do we do when older studies do not have the quality of newer studies? That issue came up a lot. Various diagnostic criteria, we decided, pretty much largely ignore them, and to take diagnosis of psoriatic arthritis in these studies as they were defined by the authors of those studies. There are certainly areas where there is no data. There have not been studies. Where this is going to come up, we will see, in one area, the use of methotrexate in the skin. Relative paucity of data that speaks to something useful that we could incorporate. Of course, the absence of head-to-head trials, we have tried to get around that by the use of effect sizes, but that is not always perfect. Again, what do we do with areas where there is not so much data, like the use of methotrexate for some of the manifestations. It has become a de facto standard, but there is really small data sets that speak to that. This is where we are today, then. This is where we have been in the past. We will show you the process. But what do we do with expert opinion, and how do we use expert opinion to synthesize these different aspects of psoriatic arthritis? The skin, the peripheral joints, the dactylitis, the enthesitis, the spinal involvement; how do we make those into a single guideline? I think we saw that on the emails that went around, that what we do as clinicians is really take all these different facets and make out judgment using the different levels of activity, the different amounts of severity and damage, in these different facets, and we synthesize that. So that is our task today. How do we put that on paper in a way that is evidence-based as best we can? Again, these are older slides, and this is what was done. We determined the areas of interest. The questions we kept very simple. And any time you do this sort of exercise, you need specific questions from which you are going to use the data to get those answers and what we wanted was the effect of a given therapy on the clinical manifestations. Signs and symptoms, quality of life, functional status, structural integrity, what is the effect size. And then the flip side, safety. What is the effect of a given therapy as regards safety, what is the effect size of that? Systematic literature review, as you will see from the people who volunteered to do this, the data was excerpted from this. As we go all the way along, key areas that we need data in the future, key areas for research, were identified. And where we are today is, we need to assemble this into a unifying guideline. So, hopefully this slide looks familiar. This is how we dissected this and Chris put this together. The different facets of disease and I really like this because I think this really summarizes what we do when we see a patient with psoriatic arthritis in the clinic. All of us, we say in our minds, “How much arthritis do they have? How about the skin and nail involvement? What about the axial disease, if they have that? What about dactylitis, if they have it? What about enthesitis?” Now, each of these, of course, has a menu of choices, and this is not hard and fast. These are just things that were commonly used and commonly identified and put in these different lists. In our way, what we are doing as we evaluate patients is to evaluate all the different facets and then we combine them, begin on a level of treatment, and then reassess. So how do we take this cartoon and really flesh it out with that with specifics of therapies to make recommendations as specific as we can? For the literature search, just these were the methods that we went through. Again, these are things that we talked about last year, so we will go through this quickly so that we can get to the important discussions. We tried, as far as possible, to follow where rigorous procedures had been set up for the formulation of guidelines. We tried to follow those all the way along. For example, this is the system, how you do a systematic review. And these are the guidelines we had all of the individual contributors go through, just a rigorous process. Again, in the interest of time, we will go through these quickly, but that is what we wanted to get, as complete a review of the relevant literature as possible. Scoring was done. So the articles were then systematically analyzed. The evidence was accumulated, and these are the different levels of evidence. This is, again, a very standard way of assessing these and grading them. Level One evidence: when there is randomized controlled trials. Level Two from control trials without randomization or other well-designed studies. Level Three from non-experimental studies. Level Four: expert opinion. That then gives you levels of recommendation: Grade A, when you have category one evidence. Grade B for category two, etc. As you will see, there are many areas where we do not have good scientific evidence, and that is what we would like to do today is to begin the groundwork, how we formulate an approach that takes in as much evidence as we can possibly use, but needs to get at the key areas that clinicians are also going to want to know. As people went through they determined effect size by which you can see the results with the treatment as compared to a comparison with placebo or to another medication, as a way to give a standard in the absence of head-to-head trials to give us some means of assessment for how large a clinical effect might be. We try very hard to stick with published guidelines on doing guidelines, and these are, I think, some of the things that are the challenges as we go through this today. In the process that we are all involved right now, do we get all the important options and outcomes or did we specify them, did we have an explicit and sensible process to combine the evidence? I think that is really the challenge for us today, is combining all the different aspects of disease into a treatment guideline as best we can. And then for the guidelines again, things that we will see, we will try to follow all the way along so the clinicians will be able to say, “Yes, these GRAPPA psoriatic arthritis guidelines will help me care for my patients.” What we will do now is go through the different facets, and you see them divided here: peripheral arthritis was tackled by Enrique Soriano and Neil McHugh; they did a bang-up job and went through a very large, luckily, a very good and large amount of data. I think we will get good information from that. Peter Nash did axial involvement, the skin involvement in terms that we divided the skin into data related to biologics, remember, because we are including psoriasis as well, studies that just looked at psoriasis, and Wolf-Henning Boehncke did that, and did, again, there is a very good amount of information so we have nice results there. Skin, in terms of synthetics, methotrexate, leflunomide, cyclosporin—boy, that is a tough area. I think that is going to generate some discussion because there is just not a whole lot of good data out there, and I think there are important gaps that we are going to need to talk about. Enthesitis, Chris did a great job of organizing this and going through the process in the best way, and dactylitis, Philip Helliwell. In these two areas, not so much data and not a lot of data with a large variety of therapies, so that is also going to be a challenge. As we go through these, remember these will be on the Web site so you can see, and I do not want to minimize the amount of work done. We are just going to kind of show it to give you a little bit of a flavor. For example, this is peripheral arthritis. This is what Enrique and Neil did, and just see, looking at these different therapies: sulfasalazine, methotrexate, cyclosporin, leflunomide, gold, injectable or oral, azathioprine, etanercept, and infliximab. And they went through and did a said yeoman’s work, evidence of symptomatic control and effect size, evidence of x-ray, toxicity issue, and then a recommendation. We will eventually have all these so everyone can look at the articles, but just to give you, I think there is a good amount of data that speaks to peripheral arthritis and, as you can even see, looking at the effect size, and they did a nice job of coming up with values that they said that either showed a small effect or a very large effect. There are still some issues remaining with peripheral arthritis. Of course, we need to incorporate the newer data on infliximab and adalimumab, the methotrexate/methotrexate cyclosporin study that was just published in the Annals, methotrexate study that is underway. So obviously, as we have new data, we need to put this in. It is going to be very important to keep it up to date. Even though I impose on them because they did such an incredible job, but one aspect that we did not fold into there was functional status, and I think that is going to be key. And then the question, and this one is going to be open for discussion, what do we do with toxicity? What do we do, do we rate it low, medium, high? Do we need a number needed to harm for specific avenues of toxicity? It is going to be very tough and in some ways very hard to excerpt from the literature because, as all of us know, it is not necessarily complete as regards toxicity. As we will go through, and I think everyone in this room has certainly read these, the British Society of Rheumatology published guidelines with Neil and many of his collaborators, and they wrestled with some of the same issues, but I do not know if we will come to those same results. They were, of course, driven by the exigency of the limited availability of TNF inhibitors and how to make regulations where they would not necessarily be used, and I think that is going to be open for discussion—do we follow their model in some ways, and I think we will in some ways, and maybe in other ways go beyond that. The skin and synthetics, this was done by Bruce Strober and some of his colleagues in New York, and boy, this one is a tough one. You look at the studies that are out there: there are two placebo controlled studies for cyclosporin with actually some data, two studies where it is compared with methotrexate, not including the one that just published in the ARD; leflunomide, one placebo controlled study where it has good data; sulfasalazine, similarly below that. Boy, there is just not enough, not really very good data, even with methotrexate. There are two well designed studies comparing it with cyclosporin, but there is a real dearth of information that will let us speak to what do we do for skin involvement. It is a big issue, I think this is a tough issue. There are many, many gaps in the data, efficacy wise and toxicity wise. Dactylitis, Philip did a great job, a very thorough job. As you see, there is not so much, not a ton of data, but there is some with traditional agents—sulfasalazine, leflunomide; some data with infliximab as well. And you can get a sense of the effect size of the different treatments, so we have some data for this, though not as complete about some of the traditional DMARDs. Let me turn this over to Chris, who is going to bring us back with the remaining aspects and then we will get into the discussion also. Chris Ritchlin: Artie, I just love it when you quote Donna Rumsfeld: “Absence of evidence is not evidence of absence.” Ahem, anyway. Yes, as already mentioned, each of these sections are manuscript, so they are very detailed and talk about the methods, and give more detail about effect sizes, etc., and these will be on the Web. So, this is just to give you a taste, as already mentioned, and to get some feedback from you as to how we should go forward in trying to assemble these guidelines. So with that in mind, I am going to talk about axial disease is. Is that okay, Peter, can I talk about yours? Just to move it along. Peter did axial disease, and I am going to move right through here to his caveats, which he has: inadequate studies, there is inadequate studies in psoriatic arthritis/axial disease, there is unvalidated outcome measures as we see with many of these areas we have been talking about. And using ankylosing spondylitis criteria may not be appropriate, such as tailoring others in the BASDAI studies. And you cannot assume that the BASDAI Baths Meyer are minimally clinically significant; differences comparable on AS and PsA with axial disease. And, again, these are general themes that we talked about at the last meeting here. So, let us get to some specific interventions: physiotherapy, there is evidence A, level A, that supervised group physician therapy is effective. For NSAID symptom and sign relief, evidence is grade A, and continuous NSAID usage may reduce radiologic progression, level of evidence A. Dafna Gladman: This is for ankylosing spondylitis? Chris Ritchlin: This is for ankylosing spondylitis, right. So, most of the evidence for axial disease if not all is in ankylosing spondylitis, and we have to decide how much we are going to borrow until we have our own data in axial disease. Correct, Peter? Okay. So, corticosteroid injections, intraarticular level of evidence C, fluoroscopic or CT guided sacroiliac joint injection, level of evidence A. And for intravenous pulse methylprednisolone for three days, 1 gram for three days, level of evidence B. Bisphosphonates, _____________ IV 16 mg monthly, we are all aware of that from the Canadian group up in Edmonton, 60% responders, 40% BASDAI decrease, 50%, and here the level of evidence is A. For sulfasalazine, the benefits of peripheral arthritis, level of evidence A, no axial benefit, level of evidence A. Methotrexate benefit peripheral arthritis, level of evidence A, benefit in axial disease level of evidence A, 1B. And no evidence of benefit: antimalarials, gold salts, Azathioprine, level of evidence D for penicillamine. Small, one year open study of thalidomide shows significant benefits, so therefore that is level B, and no benefits from either leflunomide or cyclosporin. In anti-TNS and axials, psoriatic arthritis, in the etanercept trials, 4% spinal arthropathy, no difference in response. Infliximab or adalimumab: at this time we have no data. Etanercept and infliximab improve symptoms, signs, function, quality of life, radiologic progression, we have level of evidence A for this. Using the ASA consensus disease definitions, contraindications and assessment of disease activity and response. Okay, so I am going to move on to this, and I am going to talk, we are moving quickly because we want to get your feedback and be able to have some interaction on this. I am going to talk about enthesitis and because I have a large table I did not really want to project this, so I am just going to hand this out for your reference as I am talking about this, because I am summarizing here for you all. So, from my review, and I will wait until they hand this out, it will just take a second here. From my review, NSAIDs, physiotherapy and corticosteroid injections, improving enthesial symptoms and psoriatic arthritis and spondyloarthropathy level 4, grade D. Azulfidine is not effective for treatment of enthesitis and psoriatic arthritis, level 1B. It is not effective. Methalamine is effective for the treatment of enthesitis and spondyloarthropathy, level 3, grade C. Infliximab is effective for the treatment of enthesitis and psoriatic arthritis, level 1B, grade A. Etanercept is effective for the treatment of enthesitis and spondyloarthropathy, level 1B, grade A. So, notice, there is a differentiation here between spondyloarthropathy and psoriatic arthritis. And as I get to the caveats, you will see why. In the comments, these recommendations should be viewed with caution, however, because the underlying data is incomplete and in many cases severely flawed. And you are going to hear that throughout this review’s presentations. There are several different outcome measures we used in these studies and examiner’s review, and none of these outcome measures have really been validated. They are listed actually, the outcome measures for each study, in your table. With the exception of Azulfidine, large control trials examine the effect of traditional DMARDs on enthesitis have not been carried out. And thirdly, most of the studies, and this was a particularly big problem in his work, thinking about study design, we really ought to keep this in mind, they did not state how many patients in the total population actually had enthesitis. So you could not tease that out, and this often could have resulted in an overestimation of the effect size. I am going to move on to biologics in psoriasis, and this is Henning’s work as well. I hope you all had a chance to see his superb review in the New England Journal of Medicine about a month ago on psoriasis. If you have not, it is really phenomenal. So, for the various agents we are all very familiar with, alefacept, efalizumab, the T-cell modulators, and then the anti-TNF agents, etanercept, infliximab, adalimumab, his reviews showed that the evidence for efficacy was 1B. These were all grade A. But he makes the point throughout his systematic review that there may be an underestimation of psoriasis in the psoriatic arthritis trials due to the fact that many of these patients had very mild psoriasis. And one needs to keep that in mind. So those are the other three areas. Therefore, we have covered the five areas and now I am going to move on to a very controversial area. Now I have to use some background here. The whole idea of “the grid.” The idea of the grid, actually of putting together in the Latin square was Artie’s, and Artie was going to send it around to all of you and have you fill in the blanks, and Robert and I sort of shrieked and said “Oh my God, they are not going to want to do that right before you, we just cannot do that.” So I said, “Well, you know, we really need to generate some discussion in this area and this is something that is so important,” so I decided to fill in the grid, sort of off the cuff. And what happened was a tremendous overwhelming thundering response, which we were very pleased about and I am sure has generated a lot of strong emotions and feelings. So please take that grid with the idea that it was put forth to generate this discussion and help us along in this very challenging process. Do we have the grid here? Okay, here is the grid. I am not going to read through it, but I will leave it up here for a minute or two for people to view it who have not had a chance to. Again, we have divided it into peripheral arthritis, skin, enthesitis, dactylitis, and spine into mild, moderate and severe categories for each in trying just to get some kind of sense of where you might think patients in these areas might be. Artie Kavanaugh: And the goal is to see, I mean you have seen the evidence, and I think this crowd is mostly very familiar with the evidence, to take that and especially to say how do you then go forward to, say, what should treatment guidelines be. So this is just a straw man to say that what we would like to do, and one possibility is that if someone has active skin that is very severely active, active joints, peripheral, then I think most of us would know what to do. The questions are going to be if they have skin that is a little bad, dactylitis that is moderately severe, and then to fill in the definition. So today we are not going to wrestle about whether it is 10% or 11% body surface area. We would like to, though, get opinions and buy-in about whether we can do something like this to get at our original goal on the other side, to really now synthesize all these different facets of disease, consider all them as we have treatment guidelines. Chris Ritchlin: Artie, Robin tells me a lot of people have never seen this because it went around the Steering Committee and many cannot read it back there, so I am going to just walk you through it, if you do not mind. For mild peripheral arthritis, 1-3 tender and/or swollen joints, no erosive disease on plane films, function not significantly impaired. Skin would be less than 3% body surface area; we took this from a dermatologist. No enthesitis, no dactylitis, no signs or symptoms of spinal inflammation, a normal Schober score, a normal AP pelvis film. For moderate, we had 5+ tender points, normal x-rays, but oligoarticular/polyarticular disease that interferes with normal function or less than five tender, swollen joints, but with erosions or joint space narrowing on x-ray. For skin, between 3-10% body surface area, again from the dermatologist. For enthesitis, 1-3 enthesial sites, for dactylitis, 1-3, and spine, inflammatory back pain with a normal AP pelvis film. For severe, five tender, swollen joints with evidence of joint damage on exam, arthritis mutilans, oligoarticular/polyarticular disease that limits activities of daily living. Then again, the skin greater than 10% body surface area, enthesitis greater than three sites, enthesial involvement in a foot that prevents ambulation, tendon rupture. Greater than three inflamed digits for dactylitis, evidence of ankylosis in the dactylary joint. Lastly, symptomatic inflammatory back pain with radiographic changes on plane films. So this is what went out. Yes? Paul (?): I think there is always a slight problem in putting our synthesis of what constitutes mild, moderate and severe. Just to give you a bit of background on that, we call mild all osteogenesis imperfecta, mild because it does not kill you. Whereas, the severe form is lethal in utero. But actually when you talk to people who have mild osteogenesis imperfecta, they tell you it is not mild at all. Now, the reason I say that is that in your mild group there, you have individuals who have 1-3 tender or swollen joints, but I do not quite see how you classify two patients that I have had to treat who are both surgeons who have one or two swollen joints, but whose careers are subsequently threatened. Where do they fit in that? Chris Ritchlin: I think you hit it right on the head of the nail, that implicit in our mild/moderate/severe and not arguing about specifics, but implicit is that there are different levels that you would treat differently. Now, you might say now with osteogenesis imperfecta, you might say everyone is going to get this treatment, so mild/moderate/severe does not matter, but I think tacit to this is there are some people who you are not going to give a TNF inhibitor to because their disease is too mild, but you are exactly right. The two, for those people who did not see the e-mails, and I do not know, how many people saw the e-mail exchanges? Did a lot of people? Okay, they were great. But I think there were a couple of recurrent themes in there. Dafna Gladman: But just to respond to Paul, if you go back to the slide— Chris Ritchlin: I really do not want to, Dafna. Dafna Gladman: You lost it? Chris Ritchlin: Do I have to? Dafna Gladman: Go back to here. You see, if you look at the moderate under normal x-rays, but oligoarticular or polyarticular disease that interferes with normal function. Now, that addresses your surgeon. Chris Ritchlin: But not for mild, not for mild. Dafna Gladman: No, no, but that is why you have to read the whole thing, the whole score. Peter Nash: Let us look at it this way, is it worth taking five features to make it mild/moderate/severe, or to take each feature and treat it if it is mild/moderate/severe, which is what . So if you go back to the model with the grid that we have been going over, that is how you treat people. You attack it that way. That way, anyone who is mildly axial you would start at the top and work your way down and it does not matter about the other four features, because with the five features at once, might make the treatment. Philip Mease: Can I make a suggestion that Chris have a chance to review the e-mail responses that he got and bring it further along and then open it up for discussion. Chris Ritchlin: Right, exactly, and here they are. Here are comments that were common themes, and I could not put them all up here or we would be here for the rest of the day because it really generated a great amount of enthusiasm, very brilliant discussions. The first comment was, signs and symptoms of disease activity at present had to be distinguished from signs of residual damage of the past. That was a very common comment. Secondly, a composition severity score for psoriatic arthritis and peripheral arthritis, skin, enthesitis, dactylitis and spine should be avoided for treatment purposes as every item on its own, which is what Peter is talking about, can be severe enough to start or intensify treatment. Outcomes are different, and the most appropriate treatment can be different for each item. Third, a severity of score for PsA has to be oriented to its aim: treatment, trial, quantification and physical damage or other aim. Fourth, a severity score for PsA should not, at least not exclusively, rely on numbers of peripheral joints or numbers of digits with dactylitis, but on the functional consequences of the joint or digit involvement, a point well made right here at the beginning. Fifth, a severity score for skin involvement for treatment decisions next to the total area should take into account the location of the lesions. Sixth, treatment decisions considering the spine can be adopted from ankylosing spondylitis. Seventh, we must consider function, i.e. link, the number of inflamed joints to function of those joints and function of the individual, more importantly. Other comments have derm generates skin boxes, we did those and it is based on dermatologic criteria. And what is the rationale for looking at BSA? Beware, can of worms, circular approach, consensus should be limited to the Steering Committee. Separate process, again, this is really a common theme, activity from outcome, accumulation of process. Define what you are treating, symptoms vs. prevention of damage. Please do not build rigid guidelines. Combine disease activity score with a disability score. So these were sort of three common themes that ran in response to our little test table there, and I think can we now open it up and have people? Artie Kavanaugh: You want to leave the table up? Chris Ritchlin: Sure, would be happy to. Artie Kavanaugh: And the way the room is situated, it is a little bit tough, but please everyone come to the microphones because we want to record the comments, and if you want to stand up at the microphone and just take turns speaking, that would be great, but please come up to the microphone for your comments. Will Taylor: I just say how important it is not to make them rigid because even though we put them out there not to be anything, regulatory authorities will grab these and rigidly make you can or not a valuable treatment as a result of them. Artie Kavanaugh: I think that is absolutely a fair comment and Alice Gottlieb is not here, but what she often says in a circumstance like this is that for skin psoriasis, if there is no data that the biologic agent needs to be used after traditional DMARD, then it should be available for people with severity up to the patient and doctor, that you can go with the biologic agent instead of going to a disease modifying drug. Now, the BSR when they wrestled with this, obviously came up with the fact that you should use DMARDs first in PsA patients, but again they ended up, I think, being more rigid. (Unidentified): ___________________. (from audience) Artie Kavanaugh: Good point. Philip Helliwell: Patients are pretty savvy, actually, and they pretty soon learn that if they’ve got to score high, they squeak louder when you press their joints. (laughter) Alberto Cauli: Well, actually, the last sentence in the severe box oligo- or polyarticular disease, limits activity of daily living, allow you to treat almost everybody if you feel it needs. For example, the joint, because if you decide it is limiting the daily activities, that is in the severe box. Artie Kavanaugh: Can you think of a way that we can incorporate that and be true to the data and yet not have it so that every single person can get every single therapy for whom it might not be— Alberto Cauli: No, it is the physician who believes it may be the right options. Like in this case, of this sort, the physician just does his job. Artie Kavanaugh: That was another theme that was in the emails—patient preference, which we do not specifically include. Obviously, we included, as you say, tenderness. We included it in functional status indirectly. But what about patient preference? Does that allow you to move one box, if your doctor thinks you are moderate, but you think that you are severe, is that fair enough? Does that move you a box? That is what we want to try to get input about. How to synthesize this beast into something that actually makes sense on paper. Alberto Cauli: I think that also the BSR guidelines, that is, importance in the patient’s opinion. In two sentences, they underline that the responsive treatment is to be discussed with the patient and also the treatment, in two difference sentences. Artie Kavanaugh: That is it. That is absolutely right. (Unidentified): I think Paul is treating too many mice. (laughter) (Unidentified): It is a very important point, though, what you have just raised, and that is the patient preference because patients do actually come in and say, “Look, I have heard about this treatment and this is what I want.” It illustrates one question that we cannot answer and that is, the prediction of how a patient’s disease is going to go. Even though the patient may have mild disease, what we consider mild disease, even though if it is an MTP joint, they may not be able to walk, and they may still only have one joint involved. They may have only one spinal joint involved, and it can actually destroy their lives, in terms of quality of life. What we define as being mild disease, or mild, moderate, severe, really, I do not think, comes into this at all. Artie Kavanaugh: Well, actually, Eric Ruderman and Ken Gordon put together something which looks similar in a way, and Eric, I would like to get your thoughts on that. They have the square, where it arthritis— Eric Ruderman: We try to look at it from the skin and the joint perspective, looking at it as a rheumatologist and a dermatologist, and we sort of box it into four boxes, looking at mild skin disease and severe skin disease, and then mild arthritis and severe arthritis where it was a simpler approach. It got at the idea that we may end up adding treatments for two different options and come up with a third option. That was what we were driving at—that skin disease may drive the therapy in some cases, and in some cases, the joint disease may drive the therapy and sometimes you have to take them both into account because you come up with yet a third choice, that skin disease that may require light-box therapy, and joints that could be okay with sulfasalazine, maybe the best answer is actually methotrexate because you hit both, and that is the way we looked at it. Philip Helliwell: What one way of looking at it is to say that skin is just another site. So this disease can effect lots of different sites. It can effect the joints, the skin. Chris Ritchlin: But how do we get that down on paper? Philip Helliwell: The other thing we have got to take into account is actually the effect on the patient. Chris Ritchlin: That is right. Philip Helliwell: Because it is okay for us to say mild, moderate, severe, but it is the patient’s definition of mild, moderate, severe that is absolutely critical. Dafna Gladman: But following up on that point, it is easy to deal with a patient who actually complains and wants to be treated. But on the other side of the coin, you have these patients who say “I am doing fine, I do not need anything,” and that is where the five or more joints come in because there are now a number of studies: the Neills-Dennis study, there are a couple of studies from Spain, and our own studies show that if you have five or more inflamed joints when you first present, your chances of going on to progress both clinical and radiological damage are much higher. (Unidentified): Well, your studies were the first to show that if you had two knees involved and a high ESR, that was the very first study that showed prediction of outcome. Dafna Gladman: The point I am making is, that we can talk about oligoarticular disease in the face of impaired function, but I think you need to think about polyarticular disease in the absence of impaired function as an important predictor of bad outcome and therefore, those patients should be offered good therapy early on in the course of their disease. How the therapy changes the course is another thing that we need to study. I mean, hopefully, what we are seeing with the biologics currently will actually hold true and prevent further progression of disease. Likewise, if you already have an erosion, your prognosis is worse than if you do not have an erosion when you first present. So the idea here is not to actually incorporate severity and activity, the idea is to say, when you have active inflammation, but you already have some damage, you are already a sitting duck and therefore you should be treated with big guns a lot earlier and a lot more aggressively than perhaps the next person who has a few active joints without any evidence of damage, without any evidence of impaired function, and that is the kind of thing that the grid is actually trying to address. Philip Helliwell: I am just not comfortable with the mild, moderate, severe, and I just wonder whether if we had data—first line treatment has really got to be a biologic agent, and what is the information for that? Chris Ritchlin: Start with a therapy, and then say, “What will be—“ Philip Helliwell: Spinal disease, structural damage, skin disease body surface area greater than 10% and then below that you have got the next category, maybe you tried a DMARD, maybe you have tried a— Chris Ritchlin: Yeah, and then you could actually grade the DMARDs within that category. That might be a better way. Philip Mease: One quick question for Eric: in the square concept, which I think is a useful one, I am actually thinking of a cube, in my mind, with a third dimension being always what is the felt impact by the patient. Eric Ruderman: I think is what we kind of did. And maybe think of it instead of dividing it into mild, moderate, severe activity, maybe impact is sort of a better term because that encompasses what the patient is and it may better get at what Dafna is saying because you could think about it as potential impact as well. Maybe that is a better way of dividing it is sort of what is the impact on them right now and what is the potential given their state right now, the potential impact in the future in terms of disability and function. Philip Mease: Both disability as well as the embarrassment issue of the skin. Eric Ruderman: Yeah, embarrassment issue. So, the impact was sort of implicit in how we did the square because we looked at mild or more severe arthritis, it was not just active right now, but arthritis that had already evidence that it was going to be a larger problem down the road. Artie Kavanaugh: Something else that there were comments about is that as you see on the grid there, there are mostly activity and somebody early on, I think it was actually Josef, who said, “All the things on there should be things that you reverse. You treat things that are going to reverse.” So do you say activity, but as Dafna has said, you want to add prognostic variables because not only are you relieving signs and symptoms, but you want to prevent progression, so that is why there is a mixture of things on there. Not all of which are activity, but somehow I think that is something that we need to incorporate too, that we want to control activity, and certainly you are going to treat to control something that can be reversed, but we have to keep in the back of our mind things that are prognostically important, I think Doug just pointed that out as well. (Unidentified): Most of my points have just been made by Dafna and by Doug, but I think disease severity is a compass of all damage and activity, reversible versus irreversible components and for treatment guidelines, obviously, activity is important. As Dafna has made the point, you need to incorporate those prognostic markers of severity that are going to actually dictate your treatment as well. If these are around treatment guidelines, then I congratulate you. I think it has created a lot of comments and focused our minds and gives us a way forward. But I think you can argue several of the points on that grid, and I would appreciate, for instance, you can get someone with a complete normal spine with no symptoms at all, and have mild spine disease. What is the next step forward? How does one validate this? Because obviously, you would need to look at it from a patient’s perspective and functional sort of studies as well. I congratulate your thought-provoking grid. Paul (?): Two points, if I may: the first is, well, I have never treated a mouse in my life. (laughter) This business of severity is clearly something which has been looked at very carefully. We perhaps are guilty, sometimes, of not allowing the patient enough say in how severe they are, but what we have got to be able to do if we accept that the patient is going to have a big input into deciding which of these boxes they go into, is have very, very good and probably strict criteria for judging their improvement over the next three to six months. You have got to have some sort of contract in a world where there are a million starving in Africa, it is not right that you pour money down the drain in people who probably should not be on these treatments. And that is the downside. The other thing I wanted to say was in regard to spine disease. I personally feel that MRI is a very useful potential adjunct in people who have got spinal disease that may very well be inflammatory, particularly where the CRP is not up. If you have got a raised CRP and you have got inflammatory-sounding spinal disease, fine. Treat. But I think in those who have normal CRPs, which is quite common, then I think MRI is an extremely useful adjunct to assessing whether there is inflammation currently present. It is about 250 pounds to do a sequence of the whole spine and the sacroiliac joints and you can then have something objective that you can follow up three to four months later. (Unidentified): Agreed. Philip Mease: Middle mic. (Unidentified): Can I just comment about that point? About the MRI because we have just looked at out clinical experience using the algorithm that was published in Annals and MRI actually may not be necessary in a substantial number of patients. I take your point, Paul, it is very good if it is positive, it is a very good test. But it may not be necessary if you have got enough clinical criteria. You can actually show that these patients do have active, inflammatory spinal disease. And the other side of that coin is that a patient did come up to me after 25 years, very, very advanced spinal disease, and I was saying, look this guy should not have treatment because he is N-stage and he sort of convinced me, so I said, “Look, we will try it for three months.” And this guy could not touch his knees and then after three months, he could touch his toes. So what we believe is sort of N-stage, these patients actually test our beliefs. (Unidentified): I agree with you, but _________________. (from audience) Chris Ritchlin: It is also done when your outcome at three months gives you the answer. That goes back to his outcome. (Unidentified): Artie, one point bothers me with this grid. You define mild peripheral arthritis, you define mild skin disease, but you do not define mild enthesitis, dactylitis, or spine disease. So do we really want to imply that any form of enthesitis, any form of dactylitis, is already moderate? Are there any mild forms of dactylitis or enthesitis? Artie Kavanaugh: Well, by the way you question, I think I would agree. I think there should be something in the box. There can be some that are so mild that you would probably not use anything beyond a nonsteroidal. (Unidentified): Mild enthesitis? Artie Kavanaugh: Is that fair enough? Philip Mease: Remember this was just the first grid. That was an example of the attack that— Artie Kavanaugh: That is a good point. What do other people feel? In the dactylitis and enthesitis, is there mild? (Unidentified): Dactylitis, not yes or no. Dactylitis can be between zero and one. That is absolutely. Often, very mild dactylitis where you do not need treatment changes. Then it depends on where you have dactylitis. If it is on a little toe, does not mind too much. If it is on your fingers that you need every day to play violin or to operate, it is another question. So the number does not tell us much. And it does not depend on the numbers. It depends more on the location of the lesion, the location of the problem, because this has an impact on the consequences later on. The little toe does not have as much consequences. Also, two or three small toes do not have the consequences of one finger. Artie Kavanaugh: So you would throw the numbers out completely of the dactylitis? (Unidentified): Completely. Dactylitis and peripheral arthritis also. It does not depend on the numbers. Artie Kavanaugh: So mild has to, okay. I see a lot of heads shaking. Not everyone came up to the mic, but mild needs to have something. There is mild dactylitis and enthesitis. (Unidentified): There is another great problem. So if you treat anything, does not matter if it is psoriatic arthritis or something else, you have to know what you want to treat. If you want to treat residual damage, your treatment will be much different than from active inflammation. So if someone cannot walk any more, you better give him a wheelchair, than biologicals. So it is absolutely necessary to be clear what should be treated. Psoriatic arthritis goes on and off and patients who have only one period of greater signs and symptoms, and then they go down again and have a pretty good life. You cannot, you have to put this in mind, too. Philip Mease: Good. Okay. Daniel Aletaha: Arthur, I would hear on the site some comments about the few cases that are being reported of exacerbation of psoriasis on biological treatment. One of those reported on last month on— Artie Kavanaugh: So you would that in the toxicity. Daniel Aletaha: How do we deal with this? Artie Kavanaugh: I would think of it as a toxicity and that is a tough one. I mean, I think that is something that we would have to list. How do we frame that, and we can get some numbers for the prevalence, but as far as how serious it might be, I do not know. What do you think? Daniel Aletaha: You have to stop the medication. You do it, you rechallenge, it shows up again. You have to put it on toxicity side. Even if you have to try to stop the medication. Philip Helliwell: Could I respond to that directly? Two out of the first nine patients we treated with biologics with ankylosing spondylitis, actually, did not have psoriasis, but they developed a very severe palmoplantar pustulosis. They had excellent results with their spinal disease, but the skin problems were terrible. They did not go away, they were in studies, we kept them going for four months in both cases and both patients came off. One of them was treated with retinoids, and the other one is about to be treated with retinoids. The patient who was treated with retinoids has eventually done quite satisfactorily. But it was a really nasty eruption. Philip Mease: I have a question that I would like Henning’s comment on this as well as Artie and Chris’. So, in the spine, in the absence of data in PsA, you are including the evidence from the ankylosing spondylitis trials? And so, theoretically, will have some caveat about that, that it is extrapolation. Yet in the skin, you respectfully restricted your comments to the skin data from the PsA trials whereas there is this rich database from psoriasis. My feeling is that if we are going to accept data from ankylosing spondylitis, we should fully accept the psoriasis database as well. Wolf-Henning Boehncke: Just briefly, in this list of evidences, the idea was to really point out that the biologics are unestimated with regard to their potency in treating the skin changes because you have relatively mild to moderate skin disease so it cannot clear as well as in the psoriasis trial. Philip Mease: So that is where I think you should bring in the full psoriasis database for this. Wolf-Henning Boehncke: So the efficacy on skin is much better as it looks from the psoriatic arthritis side. With regard to flare-ups and cutaneous adverse events, it is really a problem when you treat joint involvement because then you really have to decide as the physician whether you think that what you see in the skin is still acceptable given the beneficial effects on the other sites involved. Whereas as a dermatologist reading just psoriasis, we clearly tend to stop the treatment and switch that patient to another biologic because we have the option to move away from TNF alpha-blockers. So that would be our natural reaction to that. However, the other comment is true that there is a considerable number of patients who will eventually improve. I think there is a lot of unknowns regarding those flare-ups and changes in the clinical picture. It is really completely unexpected, but it is a reality that under the treatment of TNF alphas, you see postules popping up. And nothing in the world can explain. In this situation, we as dermatologists, we tend to switch to a non-TNF alpha-blocker. I think to be on the safe side, the general suggestion would be whenever you can, you should stop the biologic in case of a flare-up, and at least for a limited time, treat the skin in a different way. The contraindications to classic therapies may be relative, after all, you need to control most of the time, a short-term and acute event. So we are not talking about 8 weeks, 10 weeks, 12 weeks of cyclosporin or methotrexate. Artie Kavanaugh: Just to answer on our behalf, part of extrapolating from other conditions was felt to be more of a rescue if there was no data. In PsA, there is some data on the efficacy of the skin. Philip Mease: But not adequate. Artie Kavanaugh: Yeah. Not as adequate as one would like, but there is data. And so, since that is the disease itself, that was the original idea, that if there was no evidence, we would look for the other conditions, like for the synthetics, like for the spine. If people think it should be opened up— Chris Ritchlin: Well, the data with the skin, Artie, is the same condition. It is not extrapolating from another condition. It is the same disease. It is a little different feel than the AS. Dafna Gladman: The only thing is that psoriasis studies tend to deal with patients with moderate to severe psoriasis, the ones who do not have arthritis. Whereas in the psoriatic arthritis, you actually get mild to moderate psoriasis. Philip Mease: And the assessment tools are just not good enough in mild disease, so you are not getting an adequate assessment in the PsA trials alone. Chris Ritchlin: I wanted to comment back on the dactylitis/enthesitis issue. I think maybe one of the ways to deal with it is rather than leaving them in the grid as their own things, is using a modifier. Set up a grid or set up guidelines that look at skin and peripheral and actual arthritis and then use the presence of dactylitis or enthesitis that is sufficiently enough to be an issue for that patient that may change your therapy somewhat if it is present rather than looking at it as a separate piece on the grid as a possibility. Artie Kavanaugh: Somebody can correct me if I am wrong, that dactylitis counts as a joint in the peripheral. Is that how it is folded in? Dafna Gladman: We have actually shown that dactylitis predicts worsening of radiographic changes. So the digits that have dactylitis have much more radiographic regression than digits that do not have dactylitis. So again, in terms of prognosis, dactylitis is a significant feature. Daniel Aletaha (?): Do I understand that the recommendation that if the joint’s response was very good, that we should continue on the biologicals and try to treat psoriasis by a classical way? Is that the recommendation? Artie Kavanaugh: Once we get the agreement on how to initiate treatment, that is going to be a key issue, assessing treatment at the appropriate evaluation time and then what to do with residual disease. I think, boy that is going to be a tough one. I am thinking that the evidence for that is going to be very lacking and you will end up with opinions. I think in the case you are saying, yeah, you treat the skin, you treat the joints and the joints get much better, but the skin is still very active? Is that what you are saying? Daniel Aletaha: The case I reported in ANR last month, we did not have at the time, CTLA or MRA or did not have the picture it has now. So the patient was on the aggressive treatment of RA and we did not have where to go. Now probably, one of the recommendations that we try the other forms of therapy if psoriasis is becoming a limiting factor. (Unidentified): Can I just pick up the point about taking out the quantitative assessment on peripheral joint involvement, because I am just a little bit wary of that. Undoubtedly, the point has been well made that obviously some of the arthritis may have severe functional consequences for that individual and they need to be treated accordingly. But as Dafna was alluding to, certainly patients with more joints involved, patients who are severe get more severe and that is an excellent prognostic marker. So you really do want to have some type of quantitative assessment of the degree of peripheral joint involvement. I do not think you can abandon that completely. It might be slightly different from what you listed there, but I think it still needs to be included. Philip Helliwell: Can you hear me? outcome in psoriatic arthritis, then I think a lot of the problems that we are discussing here will resolve themselves. As example, with the dactylitis instrument that we developing, that Paul Healy is working on, we will have patient-derived data as well as the dactylitis instrument data to guide us in terms of severity of this particular feature. And as a numerical index, we will be able to give you numerical bounds within which you can call it, this feature mild, moderate, or severe and that could apply to each of these other features that you have listed on this grid. As I said to Artie right at the beginning, the way to do this is prospectively, and he said, “Well, we cannot afford it; it will take too long.” But I think we have got to start thinking in those terms. We have to start developing instruments first and then apply it to a group of patients, just as the ASAS group has done. Artie Kavanaugh: I think that is a great point and that would be certainly the perfect way to do it. I think it will be good and I think there is work going on to develop instruments to do that. Of course, an issue that is going to raise, though, is that if dactylitis instruments are available in 2006, then only studies done in 2006 and later will incorporate that, so we still be left with a gap in our scientific evidence to say how does this compare, especially against older therapies which would not have used that instrument because it was not available at the time the study was conducted. Chris Ritchlin: Okay. Great discussion. Any other comments? What we are going to do, is Artie and I are going to take all the transcripts from what we have heard today and we are going to revise what we have got here and we are going to send it out to you all and we want feedback. We will put together something that we think is going to be effective and something that we have some consensus on, and that is going to happen pretty quickly. Please continue the input you have been giving us so that we can develop this and move it along pretty quickly. Philip Mease: Tremendous, you guys. Thanks very, very much. Applause. So, we now have a break. There are refreshments outside. If you could come back in 15 minutes promptly, Dafna Gladman will be leading committee reports. Break Philip Mease: Thank you very much for rejoining us now. The continuation of the meeting will include individual committee reports and one of the foci of the committee reports is aiming toward OMERACT in mid-May 2006 in Malta. So, we are similar to the previous OMERACT meeting where PsA had a workshop in California. We are going to be attempting to support as many people who want to come to that meeting who are members of GRAPPA as can. What we are going to be doing is individually working with you, so if you have any potential option of having your flight and/or registration to OMERACT paid for, in any way that you can, either from your institution or a potential sponsorship from a pharmaceutical company, we are going to be encouraging you to take advantage of that. But then, GRAPPA will be there to help support you in the process. Vibeke, do you want to add a comment here? Vibeke Strand: What about the flyers for OMERACT? Philip Mease: Do you want to pass them out? Yeah, okay great. So, with that on hand, Dafna will be taking over at this point. V. Dafna Gladman: Committee Reports/Feedback Measurement What I am going to do in the next very few minutes is just summarize where we have been since the OMERACT meetings that we have participated in. One thing I would like to mention is that the OMERACT participation has actually allowed us to focus some of our activities in a way that we might not have been able to do if we did not have this timetable at hand. This is OMERACT 7 PsA workshop result. This was the research agenda, and I see Doug is wondering about the word, “Focus,” (laughter) but before we had these items to focus on, we had nothing. We had a sea of disease. So now, at least, we have some items in a research agenda that we have really been focusing on. As you can see, the number of items is actually quite large. In order to address this research agenda, we have actually developed some research committees which we will get to in a minute. Philip and I have taken the opportunity to propose a module for OMERACT 8 and it has been accepted and the key domains for which we hope to have updated information include: joint assessment, spine disease, enthesitis and dactylitis, imaging modalities, histologic and immunohistochemical markers, quality of life function and participation, and skin assessment. Of course, the skin assessment, we are actually leaving to the dermatologists, but we hope that by next May or maybe April, there will be some further progress with regards to other skin instruments. In terms of our approach, as you recall, last year at this meeting, we identified committees and we identified members of GRAPPA responsible for the individual committees. As you can see for peripheral joint assessment, these are the individuals that were responsible and I am going to introduce some information on where we are with peripheral joint assessment. Alberto Cauli was kind enough to take on the global assessment and the question of whether the skin, the joints, or both should be together. Philip Helliwell has been looking at dactylitis and enthesitis; I think he has concentrated more on dactylitis, but he has got that, too. Philip Mease, Will Taylor, and Doug Veale have taken on quality of life participation; we are going to hear about that. Ignacio Levari, with the help of Philip Helliwell, are responsible for spinal assessment and we have already heard from the committee on treatment guidelines. We are going to hear about immunohistology from the small meeting that took place a couple of months ago. We have heard from Desiree about the imaging. I do not have anything to report about economic impact, but hopefully by the next meeting, we will have something to report. So, just to remind you, OMERACT stands for Outcome Measures in Rheumatology Clinical Trials. OMERACT was established at a conference in Maasstricht in 1992 and it is structured as an informal international network of clinicians and investigators in the field of rheumatology. The process involves achieving consensus on outcome measures and it is based on the OMERACT filter, which you have seen earlier in Desiree’s talk, where truth reflects face content, construct, and criterion validity, and basically addresses the question, “Does the measure address what it was meant to in an unbiased and relevant way?” And so in terms of face content and validity, it has to make sense, whatever we are measuring has to make sense and it has to be measuring what we think it does. So an actively inflamed joint count has to measure the degree of inflammation in psoriatic arthritis. Whatever we use as a measure of skin assessment, it has to measure the degree of the inflammation and severity of the skin involvement. Likewise, the measure has to have a discriminating capacity. It has to be reliable, in the sense that two people doing it separately, one person doing it repeatedly, we should get the same kind of result, and the measure has to be sensitive to change over time. It has to be an ability to measure a change between one visit and the next, and of course between drug and placebo. And so, does it discriminate between situations of interest? Last, for the OMERACT filter, it has to be feasible. It has to be a measure that can be applied pragmatically, given financial and interpretation constraints, in longitudinal observational studies, and in randomized controlled trials. And that is one of the reasons why one shies away from doing or expecting to have an MRI for diagnostic or classification purposes because it is not practical measure to be done in every single area that is represented here in terms of practice. So, it has to be practical. The question that I ask is, “What measurements should be included in the assessment of peripheral joints in patients with psoriatic arthritis?” Last year, at this time, we decided that we were going to look at 68 tender, 66 swollen joints for entry to clinical trials and for assessment in longitudinal cohorts. You really need 68, 66 swollen joints for calculation of the ACR 20/50/70 as well as the psoriatic arthritis response criteria. Now, when you are looking at ACR 20/50/70, or the PsARC they both include joint counts, they include patient and physician global assessment. The ACR responses also include an ESR or CRP. And so the question that arises is, “Should the ACR or the PsARC be considered a primary outcome measure? Should they both be considered outcome measures? Or should there be a new response measure developed specifically for psoriatic arthritis?” And this is similar to what Will Taylor and Philip Helliwell did with the CASPAR, saying that since none of the classification criteria was actually developed specifically for psoriatic arthritis, they tried to evaluate the sensitivity and specificity of all of them, and then generated from the data that was collected, a set of criteria which is sort of in-between all the sets that we have seen. The question is, “Should we actually develop a new response measure in psoriatic arthritis?” So I leave that as a question. Let me finish what I wanted to say. What I wanted to show you is, how do the ACR and PsARC function in the trials that we have seen today? So this is a summary of the new therapies in psoriatic arthritis, meaning specifically, the biologics. You can see that the numbers by the agents are the phase of the trial, so it is 2 Phase 2, 3 Phase 3, and so on. You have the number of patients that were included in the trial, ACR 20, ACR 50, ACR 70 in the treated and the placebo patients and the PsARC treated and placebo. I highlighted in yellow, for each of the trials, what was the primary response criterion. So, for the etanercept 2 which was Philip Mease’ trial, the primary response was the PsARC and you can see that it functioned very well, as did the ACR 20/50/70. For the infliximab, the IMPACT trial, the ACR 20 was the primary response, but you can see the PsARC functioned very well as well. The etanercept multicentral trial, again, the ACR 20 was the primary response, but again, the PsARC functioned very well. The leflunomide trial, the PsARC was the primary response. The ACR 20 did not function quite as well as the biologics, but it certainly was statistically significant. The onercept trial only reported on its primary outcome, which is the PsARC, and notice that placebo response was very high here. The infliximab Impact 2 trial, again used ACR 20, but they did not include the PsARC response at all, so we cannot actually compare this response here. Efalizumab used ACR 20 and turned out to be a negative trial. Adalimumab used ACR 20, but also shows a very good PsARC response, and the alefacept trial used ACR 20 and again, was a pretty good response, but no PsARC results. So, just looking at the clinical trials that have already been completed, you can see that either the ACR 20 or the PsARC response is a pretty good outcome measures in differentiated drug treated/placebo treated patients. The PsARC has a slightly higher placebo response than the ACR 20, but just to remind you, the PsARC requires a 30% improvement in swollen tender joint count, and in the physician and patient responses, there has to be an improvement by one category on a category rating scale. Paul (?): I wonder, could you tell us what onercept’s Dafna Gladman: Oh, right, okay. So, if the efalizumab you heard before, there were a number of T-cell agents that are used in psoriasis, and some of them have been tested for psoriatic arthritis, so onercept is a T-cell receptor which, unlike etanercept it is P55. Efalizumab is CD11A antibody, and alefacept is an LFA3 receptor. So, these are both T-cell agents. The rest, except for leflunomide are anti-TNF agents. So the point I am making then, is, that both the ACR 20 and the PsARC have functioned very well in the trials that we have performed so far in psoriatic arthritis. (Unidentified): I see people trying to write down the numbers, and it is very hard to do that. I just want to remind everybody that all of these slides will be posted on the intranet, probably Monday or Tuesday of next week. Dafna Gladman: I can see why they want to write it down. It takes quite a bit of time to make these tables, and a lot of sources, as you can see at the bottom. (Unidentified): So, all of these things will be in the library section, which is where all the slides from all of the meetings, as well as the transcripts are. I just wanted to save people the time. Dafna Gladman: I just want to tell you that if anybody is using these slides, please give credit to the person that produced them (laughter). I know you are going to use them. Anyway, so the idea is, here is a proposal for measurements for clinical trial. So, obviously, we all know about the peripheral joint count, the dactylitis, at the moment, what we have looked at is the number of digits with dactylitis, and the level of tenderness and/or swelling. This is what has been included in some of the trials. Obviously, when Philip Helliwell has validated his new measures, we will have to make sure that it is feasible to include in clinical trials because it does take a little bit of time. But if it does work better than doing a count or a look, then it may very well be something we want to incorporate. But as was mentioned earlier, the things that are not currently validated will not be included in clinical trials until after they have been validated. There is a tendency to include things in clinical trials that are not validated and that might be fine, but they are not actually valid for the study in which they were done. They actually become validated for the next study that will be done. The enthesitis score in a number of centers, and certainly in our SPARK reliability study of measurements in psoriatic arthritis, we used four sites for enthesitis and these were the Achilles insertion, the plantar fascia insertion, the shoulder, and the knee. But of course, the MASES includes thirteen sites. Again, it is going to be included in one of the upcoming trials and hopefully will be tested in a validation trial that we are trying to put together in the very near future. So, again, the question is, how this should be measured. The spinal assessment, there is no point talking about it at the moment because there is a study that is going to be done. We could do what we did in the treatment guidelines; we could borrow the measurements that are used in ankylosing spondylitis, and we may end up actually doing that if we prove that those measures are as reliable in psoriatic arthritis as they are in ankylosing spondylitis. The problem is, we already know from a study that Will Taylor has done and a study that we did in Toronto, that the BASDAI and BASFI do not quite differentiate patients with psoriatic arthritis with and without spinal involvement and they do not work as well in patients with psoriatic arthritis. Partly, this has to do with the fact that patients with psoriatic arthritis are not quite as tender and really do not perceive as much pain as patients with ankylosing spondylitis or rheumatoid arthritis, for that matter. So that still remains to be done. At the moment, we are using the PASI score, or a target lesion score, which is sort of a PASI limited to the 1-2 cm lesion, but again, I await my dermatology colleagues to come up with a better measure, particularly for the extent of psoriasis that we have among our patients with psoriatic arthritis. The patient and physician global, you are going to hear about, so I will not say any more about that. At the moment, the HAQ and the SF-36 have been included in psoriatic arthritis trials and they have both been validated in psoriatic arthritis. Now, there are new measures; there is the PsA Quality of Life measure that Doug Veale’s group has produced. That needs to be validated in clinical trials for sensitivity to change. We know that these two do respond within six months. They do give us enough of a change within six months, and we know that among patients that are followed that are not on trials that are followed, probably do not respond as well to whatever they are on, there is very little change. And the fatigue scales that have been incorporate—there is a fatigue severity scale (FSS) that we have used in Toronto that again, has been validated in psoriatic arthritis. There is the FACIT which has been used in a number of studies with rheumatoid arthritis and a number of studies with psoriatic arthritis and in fact, my medical student who started two days ago in my absence is actually doing a study this summer comparing the FSS to the FACIT so that we can see if they can be used interchangeably, or if one gives us more information than the other. So, just before we go into the committee reports, are there are any comments or suggestions as to how we should proceed with the selection of what instruments would be the appropriate ones? (Unidentified): I have a clarification comment. PsARC was included in IMPACT 2 study and actually performed quite well. Dafna Gladman: But it has not been reported upon. (Unidentified): It has been reported in several presentations. But anyway— Dafna Gladman: It is not in any of the published abstracts or papers that I have seen so far. So you may need to go back and make sure that it is there. (Unidentified): Okay. I would like to make the point that it performed very well also. 77% of patients responded to infliximab versus 20% to placebo. Dafna Gladman: Can I quote you? This is the IMPACT 2? Philip Mease: So is it written in any of the abstracts or papers? (Unidentified): I think it is in the paper that is on Web sites. Philip Mease: Okay. So that is the paper that is theoretically going to be published in the next month or two. (Unidentified): Right. Dafna Gladman: Well, if it is already on the site, I can certainly put it in. I just did not have it. I should have had it. I did not have it. So, proposed measurements: Philip Mease: Now, Dafna, can you make any comments about, in just two minutes, on how you would propose that we as a group go about validating in areas that we are not already projected to do so? Dafna Gladman: One of the proposals that we actually have on the table is to actually have a validation study. The best way that I know of to validate, at least reliability, is to get a bunch of investigators together, to get a bunch of patients together, in what is known as a Latin square design, so it is like a round robin, where all the investigators, all the examiners get to see all the patients and get to perform the examinations of interest and then there is specific statistical analysis, actually in a NOVA, that is done, and you then appreciate the effect of the patient, the effect of the order of the examination, and the effect of the examiner on the variation that occurs. You can actually show that the examiners are doing things in a similar way and you can then say, “Okay, this particular examination is reliable.” We have done that in lupus using the systemic lupus international collaborating clinic group very effectively to look at SLEDAI, SLAM and BILAG which are three activity measures for lupus and showed that they are actually very highly correlated with each other, and therefore any one of those could be used in a clinical trial. So, that is the reliability part. In terms of sensitivity to change, what you would have to do is take individuals that are followed at regular intervals. Now, that can be done in a trial over six months, or in a longitudinal clinic over six to twelve months, and see what the measurements give you. We know, for example, in lupus, we have shown that the SLEDAI actually is sensitive to change, and we can actually determine the value that correlates with a flare. So, a similar approach can be taken here. The fact that we have these results in clinical trials, in clinical trials, we only get the beginning and the end of the trial. But we could look at what happens in individual visits within the trial and evaluate the differences between drug-treated and placebo-treated patients. Philip Mease: Vibeke? Vibeke Strand: I just wanted to say, to refer back to what you have done in lupus, that is actually right, except that unfortunately, in some of the clinical trials, most of which have failed, they have not performed as well as they did in longitudinal observational studies and those validations. And I think that is because of the difficulty with lupus. But, to avoid having this kind of a problem also with psoriasis and psoriatic arthritis, it would obviously be very helpful to do both, as you said. And to try to get databases from the clinical trials and to try look at the validity of these, their sensitivity and their repeatability within the trial. Also, going forward, if there are new instruments that can be introduced into a Phase 2 study and validated that way, and then subsequently be applied in a Phase 3, and since hopefully we are going to have more new products, I think that is something that should be done in parallel to what you have suggested with the observational cohort. Because, I think it was difficult even with just RA to start with that and to move them into RFCTs and in lupus, we are really faced with a very difficult disease process. So here, it would be nice to be able to do both and I think that the resources are available. Doug Veale: Could I just ask a question and maybe Vibeke would comment on this and that is whether in terms of looking at a measurement value and whether it is discriminant value is actually good or not. Are you better actually looking at a group of responders or a group of nonresponders? Or are you better looking at a group of responders in the placebo-controlled study? Vibeke Strand: Well, it depends, obviously, but I think that one of the reasons that it would be nice to do these in the context of a clinical trial is that we could look at responders by the definition but we could also look at the therapies, by difference of controlled versus active. And that is what has been missing for us, obviously, in lupus. It is going to missing anyway, in the longitudinal observational cohort because all patients are ostensibly trying to be treated to their maximum benefit, so change may not be as evident. Whereas, clearly, in a trial, you may see some change over a shorter period of time that would be clearer. I am just saying that I think we need both, and I think is exactly what we should be aiming for. Regulatory agencies do, in fact, recognize that certain measures will have to be actually validated in an earlier study to be applied to a subsequent study. Dafna Gladman: One of the things that is important, actually, in the clinical trial, is at least the measure should be reliable in the sense that if people from different centers are doing it, that they are doing it in the same way, because one of the problems in the studies where there has not been a response is that there is so much noise from the different people doing it that you cannot see the forest for the trees and so the reliability is important to start with, and the sensitivity to change and the responsiveness can then be derived from clinical trials. Doug Veale: Which actually brings me to my second point which is, what we mean by validation. I have read two reviews of quality of life, which I know we are going to come on to, whereby the PsA QOL has been, if you like, labeled as being “not yet validated.” Certain instruments are validated in terms of their derivation. So for instance, reliability, face validity, content validity, test re-test—all of these things, if you take the example of the PsA QOL, has been actually published. That data is available published. What I think is meant is that it has not been used in a clinical trial. Dafna Gladman: It is sensitivity to change. Doug Veale: That is different. That is different. Sensitivity to change is being looked at, but not in a clinical trial. So, I think we need to be just a little bit careful when we use the word, “validation,” as exactly what we mean. Because some instruments have been validated very carefully, but they have not been used in a clinical trial and there is a difference. Vibeke Strand: I think that is incredibly important, because for instance, measures in lupus have been well-validated and yet do not function well, or are not discriminant in a clinical trial. Now, that is probably not a problem with the measure, necessarily, but we cannot be looking at ten or fifteen failed therapies over the last two decades and not think that perhaps there are some issues about also trying to validate these instruments within a clinical trial. I think the double-edged approach that Dafna has been recommending, and that Doug, you were just talking about, is the way to go, and we obviously can say something has been validated for its reliability, or for its sensitivity to change in longitudinal observational studies, but then it requires similar type of validation in an RCT. Dafna Gladman: We are running out of time, so I think we are going to move on. Since you have not helped me sort out which of the instruments we should use, we are going to move on. Maybe you will get an opportunity to discuss it on the GRAPPA page, and we are going to ask Philip Helliwell to come and give us the results of the research committee deliberation. A. Philip Helliwell Research Committee Well, despite the fact that GRAPPA stands for the Group for the Research and Assessment of Psoriasis and Psoriatic Arthritis, as a group, we did not have a mechanism or a budget to support any research. So it came as something of a surprise to us, I suppose, in early this year, when we received an application for research funding. There was some talk about this at the Steering Committee at the time, and I would not say animated discussion, but the result was that I was elected chairman of the newly formed Research Committee to tackle this issue. I have already said those first two points, haven’t I? So, it was left to me to work out how to do this and I decided that I would like to try and involve people outside the Steering Committee because there were some criticisms that erupted from that point of view. But because the research application wanted a fairly quick decision in terms of getting the research done, we would have to ask for proposals to the whole group with a fairly short closing date. The group identified $50,000 as the budget for this particular round. So, as I was saying, I was trying to involve people outside the Steering Committee, and I also wanted people who had experience in this area and also were likely to respond quickly. Obviously, that is important when you have such short deadlines. I also wanted to include dermatologists and rheumatologists. So, apart from myself, Peter Nash and Eric Ruderman agreed to sit as rheumatologists and Richard Langley from Canada and Alan Menter from Texas as the dermatologists. We had this short call time as I have told you and to our amazement, we received eleven proposals, total funding $266,000 so clearly that far exceeded the budget we had and really, knocked it out of it. At the Steering Committee discussion, it was decided that we should sort these proposals. The original thought that I had had was, okay, well, we have done this sort of on the hoof and we might as well just share the funding out. But it was suggested that we try and grade them. So we set up a grading system and there was a filter question which was, “Is the project relevant to the GRAPPA aims as identified in the Annals supplement which came out earlier this year?” And then, each proposal was scored on three dimensions: firstly, significance and innovation, and the grading 0-7, with seven being better; scientific quality, same grading system; and ability and track record of the applicants. So each of these eleven proposals were sent out to members of the committee. Since I was one of the applicants, I did not include myself in the initial scores, but I will show you that it probably did not make any difference anyway. So I could not have been accused of bias. These are the scores, the aggregate scores. Remember that the three dimensions graded up to seven, so 21 is the top score. You can see that there are probably four or five proposals that scored better than the rest, there is another group and then two or three at the end. I initially thought, well, maybe we could look at the top three. In fact, there are top four because there is a first, second, and joint third. You will see how we came to our recommendations. I must emphasize this point, that really all the Research Committee is doing is recommending to the Steering Committee. We are not suggesting this is actually what should be done. We are just making recommendations as we were asked to do. These are the scores. On the right, with my scores added, and you can see that it probably did not make any difference at all to the final places. Very little difference, anyway. So we were all fairly coherent in our appraisal of these proposals. The winner was a proposal from Italy, Ennio Lubrano and colleagues, and was designed to look at the validity of two instruments for assessing the radiological progression in psoriatic arthritis. And this group requested $10,000. The second application was from Vienna, appropriately enough, and in fact, this application had some similarities to the original application we received that started the whole process off. It was a two-part study, part A being qualitative to identify the domains of items that are important to patients with this disease, and part B a quantitative study that would take this forward and do some validation. That study requested $49,512. (laughter) I think talking to Josef earlier on today, there was a little bit of misunderstanding when we put the call out, because he thought the call was for proposals up to $50,000 each, so this just fits nicely under that $50,000 mark. (laughter) You have all done this, haven’t you? So the joint third was the proposal from Leeds and remember, Will, as Dafna pointed out, we are in OMERACT mode at the moment, and these first really do fit into the work that we want to do towards the OMERACT next year. And our study was the validation of our dactylitis instrument using MRI to aid the validation process, and we were asking for $26,500. The joint third was a purely psoriatic application from Henning looking at the impact of psoriasis on coronary artery calcification. In retrospect, if you remember the graph, there were really five that were on equal footing, separated from the rest. So we looked at the next application, which was from Leeds and Belgium, looking at activated molecular signaling in mesenchymal stem cells. Again, this is not really an OMERACT orientated application, but was felt to score very highly in this round. So we had some electronic discussion about these proposals and the solution to how we could share out the $50,000 and the solution we came up with that we are going to suggest is that we fully fund the first application, as befits the application that came first, and then to part from the next four, as they all received similar scores. We felt if we could argue that the study from Vienna was a two-part study, and we could fund the first part, and they could come back after that and look for funding for the second part, that then we could probably give each of the next four studies $10,000 that would set them well on their way to completion. So that is the research committee’s recommendations for the distribution of this pot of money that has been allocated this year. Philip Mease: Thank you, Philip. One of the issues to be discussed, perhaps, is the close overlap between Will Taylor’s project which he had initiated in collaboration with Professor Stucki and in relation to the WHO project and the one from Vienna. If there is some way of helping to marry these projects and have collaboration in this regard, so if we could have some commentary on that, and in particular, this concept that we were sort of being seen as a beta-site for this development of a participation questionnaire within that WHO project and to present to OMERACT. Will Taylor: It feels slightly odd, actually, to be in this position, to be the initiator of the whole process and end up kind of the loser. (laughter) It was not really until I looked at the report of the Research Committee of the other applicants. When I saw the Vienna proposal, and in fact, there is a lot of overlap between that project and the one that I proposed. In addition to that, the first part of that project, which is a qualitative focus group study, is almost identical to a focus group study that I have already got funding for, separately outside out GRAPPA. So, it would seem that part A of that project would not necessarily need to be done, and perhaps we could work together on the part B. I have happened to meet with Tanya Stam, who is the first applicant and she is quite keen to look at that. Philip Mease: Part of my interest in asking is because Will had already reached out to a number of centers in a various places, rheumatology centers and dermatology centers including ours, so we were all lined up to do this project. We would have self-interest in having this continued collaboration at an international level potentially, as opposed to involved in such a project. Will Taylor: Well, I cannot really answer that without discussing the project in more detail with the Vienna group, who are not here. Philip Mease: So, Philip, in terms of moving this—oh. (Unidentified): I am a co-author on this project, so Tanya Stam has had a major input in this. But I think the prospective cohort study we were proposing, which is part B, I guess, had an important aspect, which I today heard a lot of controversy about. To include the patient perspective, to include patient reported outcomes into the meaning of our measures. So what we are simply suggesting was to look at patients at two time points, first time point when they get a change in treatment in any way, and then ask them on the second occasion, “Are you better, are you worse,” major, minor worse, major minor better, and relate it back to extensive assessment at both time points. The other part, and I think that would be great to have a cooperation, and the other part is actually the more costly part, in having the focus groups and the qualitative study, and it would be great to have a cooperation in this part, and I am sure that Tanya Stam would agree to do that. Philip Mease: It would be great if we could hear back about the progress you make in terms of bringing the two together. If there was any way of bringing in the network that Will originally developed which included some key thought leaders in the dermatology realm, I think that would be very important for both the weight or authority of whatever comes out. Philip Helliwell: It was clear to the research committee that, how shall I put this delicately, that all the projects, or certainly the top scoring ones that we looked at, probably already had other sources of funding, and if they hadn’t, their project was not any good coming to us for aid because of the way it was all set up in an ad-hock fashion. We thought, therefore, we could be rather magnanimous and equitable in our recommendations about the distribution of funds. If that is any help. Philip Mease: Why don’t you go ahead? Thank you, Philip. Dafna Gladman: Thanks. Obviously, the Steering Committee will make the final decision, and that will be on the web. So the next committee that is going to be reporting for us is the Quality of Life/Participation, and Philip and Will, I do not know which one of you is going to present. Philip Mease: I will go ahead and make a few introductory comments and then turn it over to Will. Will, are you prepared to step forward? Okay. So, basically, there are a number of quality of life and function measures that are being used in trials. These will be brought together and analyzed for the purpose of the OMERACT meeting. One other part of this is that we are beginning the process of determining MCID values for some of these instruments. For example, there has been a proposal that the MCID for HAQ be ascertained as 0.3 as opposed to the 0.22 in rheumatoid arthritis based on a, if you will, pilot study that was done with the Phase 3 etanercept data. What would be useful would be to use data from other clinical trials to verify whether or not this is a reasonable number or not. I bring that up as an example of furthering what is clinically relevant to patients in the realm of quality of life and function. But Will has been very involved with helping with this business of bringing this participation project forward. So, Will, if you want to take over. B. Will Taylor Quality of Life/Participation Will Taylor: I am going to present the findings of a study that you all and others have been very helpful in, which is a Delphi exercise to help determine a core set of ICF items. ICF stands for International Classification of Functioning, Disability, and Health, which is a world health organization framework and classification system for understanding how diseases affect people. It is a very important framework and it is very useful, I think, for the whole outcome initiative we are doing in psoriatic arthritis, to do this within the ICF framework. This is, to remind you, Gerold Stucki is going to be chairing or involved with a much larger presentation about the ICF within the EULAR meeting, but this is a model of the ICF. We came in with this part of the picture, participation, which was identified as a gap in the measurement of outcome at the last OMERACT meeting. This gap is not unique to psoriatic arthritis. Participation is not really measured adequately in any disease condition or rheumatic disease. But is a nice way of conceptualizing assessment and outcome. The ICD, or the International Classification of Disease, with how that disease affects people in the context of their environment and personal factors such as how they cope with things. The ICF is enormous. There are 1400 items within the International Classification. So to apply that to any individual person is not feasible. So there has been a proposal from Gerold Stucki’s group in Munich to develop core sets or items within the ICF that are more relevant to particular disease conditions, so to develop disease-specific core sets. The process by which that happens looks at a number of preliminary studies to gather data from patients themselves by applying the ICF to individual patients and that was the study I had applied for funding from GRAPPA and could be combined with the Vienna study. The expert opinion about what items from the ICF are relevant for people with a particular condition, which is the Delphi exercise I will be talking about now, a literature review of which measures have been used in outcome studies in psoriatic arthritis already, and then mapping these measures to the ICF, and then patient opinion, using qualitative methods: which items within the ICF are relevant to patients when you ask them directly in a focus group format. All that information gets considered at a consensus conference, and that produces the final list of ICF items which could be considered a core set that should be measured in all patients with the disease of interest. There is a second phase which involves a validation. So it is quite a big process. As I say, we have the Delphi exercise for psoriatic arthritis. We have a similar process going on for psoriasis, but it is a few months behind, but that will be completed at some stage. Then, the literature review certainly for psoriatic arthritis is complete, and it is ongoing, really, for psoriasis. The focus groups, we have funding for studies in psoriasis and psoriatic arthritis, so this is the part that we are missing here. So, just to report on the Delphi exercise, this was an email-based survey to 37 health professionals: rheumatologists, dermatologists, rehab physicians, some occupational therapists, physiotherapists, so we got a broad spectrum of health professional opinion. It was not just confined to rheumatologists. In the first round, we asked people to nominate areas of life that they thought relevant to people with psoriatic arthritis in a free text kind of way. Those areas were then mapped to specific categories within the ICF which were then rated on a scale of 1-9 as important or not in the next couple of rounds. We used a method of calculating agreement or disagreement that the Rand Corporation and the UCLA developed where a score of less than one means agreement. Within the ICF, activities and participation are not distinguished. There is a chapter within the ICF entitled “Activities and Participation,” and so both of those areas I am going to be talking about now. It is possible when you look at the items themselves to work out which one would be more likely to be linked or categorized as an “activity” and which as a “participation.” Just to remind you, how the WHO considers participation as sort of a societal level activity. So, work, and we already heard how important that is to an individual person, but other life activities such as being a parent, or being involved in a sport or other hobbies. Whereas, activities are much more at a person level, such as tying shoelaces or being able to walk, that kind of thing. So the example that Paul gave earlier today, the surgeon with a single digit, may have very high scores on activity level questionnaires but be very impaired when it comes to participation level questionnaire, if one existed. There were a very large number of items that were suggested by the first round. 83 areas within this activity and participation. Of those, when they were rated, 41 got a median score of 7 to 9, which basically meant that there was agreement that these were important. In the third round, I asked people to rank the other items, and a further two were agreed to be relevant, but there were 39 that were rated as neutral. That means that they had a median score of 4 to 6. So neither irrelevant or very relevant. Of those 39, there were 26 items that scored at a median of 6, which essentially means that they were more relevant than not. That gave 72 items. So, a lot. I do not know whether this is particularly easy to see. The items shaded in purple here at the ones that there was agreement as being relevant. The other ones here, not shaded, were the ones agreed with a median rating of 6, so probably relevant, but not absolutely sure. I will give you a minute to look at those. They pretty much cover the spectrum of human life. Then, I took out, because we are particularly interested in participation here, I took out from those the items that one could consider as being a participation item rather than a simple activity. So these are the ones that were definitely agreed as being relevant, and those were the ones that scored a median of 6. Now it is relevant to mention at this point, that at the OMERACT meeting in 2006, there is two relevant special interest groups in addition to the psoriatic arthritis. One is, the ICF framework itself is going to be introduced to OMERACT by Gerold Stucki and his group for the first time. The second one is a group led by Clare Bombardier regarding work productivity as one of the components of participation. You can see that certainly employment features in the items that one would consider as participation, but it is certainly not the only one and I just wanted to highlight that. So we have an excessive number of items to be a core set, and I will give an example here. There are 32 items from the RA core set which has already been developed. We need the patient’s perspective, we need to refine the number of items, but it may be that we would be able to use that list of participation items that we had already identified to develop a measurement questionnaire. Thank you. Dafna Gladman: Any comments, questions to Will? Okay. We are going to move on, then. You had a question? (Unidentified): (from audience) Will Taylor: The ICF is supposed to be a worldwide system, so that in third world countries, for instance, transportation may not necessarily be motorized. You can use bicycles. So it is attempting to measure the whole spectrum of humanity. Dafna Gladman: Okay. So we are going to move on to the next committee report. Alberto Cauli is going to talk to us about the proposed study of PGA VAS. C. Alberto Cauli PGA/VAS Good afternoon. Today I will summarize a protocol designed to study the use of visual analog scale in patients and physician perception of disease in psoriatic arthritis. This item has been raised because VASs are a popular tool in the assessment of chronic arthritis. Let me underline a few examples. A VAS on general health status is included in VAS 28, and in psoriatic arthritis response criteria we find improvement in patients’ and physician’s global assessment. Furthermore, ACR 20/50/70 response also include patient and physician global assessment. It is therefore clear this is an important issue. Given the fact that psoriatic arthritis is a complex disease that affects both joints and skin and very often these patients has got a psychological involvement, a question has arisen: are patients’ Global, joint and Skin disease evaluated by means of VAS a reliable tool to easily define disease status or, conversely, they are not, and therefore we should not employ them in clinical trials and even in routine outpatient clinics? Although doctors are not supposed to be psychologically involved, the same question arises also for them. This item was included in the 2004 GRAPPA research agenda. In previous GRAPPA meetings, it has been decided to differentiate global joint and skin questionnaire for patients and for physicians. In Berlin we decided altogether to perform a proper study. One recommendation was to keep it simple and easy to perform. The protocol was discussed all together in San Antonio, and then via email; in particular with Professor Gladman who is chairing the assessment committee This is the list of the participating colleagues. First of all, I would like to thank all of them for joining this project. In the list, there are four dermatologists. Philip correctly underlined that four perhaps is a low number. This is true, but my feeling is that we do not need to be 50% rheumatologists and 50% dermatologists. We really need to have 100% of patients correctly evaluated both on the joint and skin aspect. For doing that, I strongly encourage all of you to look for the help of your local colleague, a dermatologist if you are a rheumatologist, or a rheumatologist if you are a dermatologist in your town so we will have precise and reliable data on both aspects of skin and joints. The main aim of this project is to test if global joints and skin disease evaluation by means of VAS are reliable in psoriatic arthritis. Furthermore, to define the different impact of specific joints and skin areas, to define the impact of dactylitis and enthesitis, differences in PsA subsets, job, disease duration, because people may get used to disease. And furthermore, to provide data in answering this question: patient perception of disease should be taken into account when proposing treatment guidelines or reinbursement policies? And furthermore, to help us in defining when a physician considers PsA disease mild, moderate, or severe. We have had this discussion today and in the past week by email on this subject. Let us see the questionnaires. We have decided all together that this questionnaires will be translated into the local language by the participating physicians. Each question will be in a different form in a random order of administration. Let’s read them: Global. In all the ways in which your PSORIASIS and ARTHRITIS, as a whole, affects you, how would you rate the way you felt over the past week?, from excellent to poor in a ten centimeter scale. Joints: in all the ways your arthritis affects you, over the past week, how would you rate the way you felt over the past week? From not at all to severely. Skin: in all the ways psoriasis affects you, how would you rate the way you felt over the past week? From excellent to poor. These are the questionnaires for physicians: Global: How would you rate global skin and joint disease in this patient? From quiet to very severe. How would you rate joint disease in this PsA patient? From quiet to very severe. And how would you rate psoriasis in this psoriatic arthritis patient? From quiet to very severe. The protocol inclusion criteria is very simple. Any consecutive PsA patient, regardless disease activity, treatment, or disease subset, may be included. Many colleagues have underlined the need to have severe cutaneous involvement in some patient, and I agree completely with that. But I recommend to include consecutive patients to avoid bias. And before seeing the CRF, let us see the timetable. On study entry, we have demographic, medical history, objective evaluation, and of course, the questionnaires. Week One: repeat questionnaire, plus objective evaluation in order to determine the reliability of the instrument. And Week Twelve as in Week One. In twelve weeks, we may be able to see differences in the skin and joint activity, so twelve weeks has been chosen as an interval. This is the first part of the CRF that has to be filled at first visit, Week One, Week Zero. You can write in the boxes on your computer. If one patient has got peripheral and axial involvement, both boxes have to be marked. Onset of psoriasis, onset of arthritis, family history because people may get used to red skin or swollen joints, medical history. Yes, any disease that may influence VAS is important. Criteria for fibromyalgia, psychological involvement, these are factors that may influence the answers of the patients. Job and current treatment. These are the questionnaires for the doctors. You can sign in the boxes Week 0-1-12. ESR and CRP, and do not forget to report any change in treatment. Changing treatment is welcome, but it has to be reported. Joint count out of 68 tender and 66 swollen, presence of dactylitis or enthesitis. I will need to have the form back. Do not send me the score, because we will analyze the different impact of the different areas. Face, genitals, hands, buttocks, intergluteal or feet. These questions are not part of PASI, but they are important sites, so we will evaluate the area involved. And these are the patient questionnaires, as you can see in different forms, to be randomly administered. In this page, you can see the empty box, in case you feel the need to underline some characteristic of the patient. And there is a grid where you can summarize the various score of the patients and doctor’s global joints and skin disease. Do not send me the questionnaire, please, but simply the score. I suggest you to print out the CRF to fill the boxes and administer the questionnaire in the clinic in front of the patient, and then you have got two options: my favorite one is to fill the electronic forms on your PC and then send them by email. Remember, that each patient is one file. Second option is to make a copy and send them as they are by ordinary mail or courier, but always remember to keep a copy. The data will be statistically analyzed as appropriate and hopefully we can have these outcomes. We will better understand how patients and physicians perceive the disease and the impact of the different clinical manifestations and specific variables. Perhaps the results may even affect our approach to treatment. Thank you. (applause) Philip Mease: I am going to jump in. I would like Henning to make a comment if he would. I remain concerned that we are not going to get enough severe psoriasis patients. I know in my clinic, we will not, to really do this right. So I am wondering if there is a way, and what your thought is, Henning, whether or not you think this needs to be expanded and include more dermatologists or can we rely on us to really weave in our dermatology colleagues to help us participate in this? Wolf-Henning Boehncke: I agree that from the way the patient is choosing the physician, rheumatologist or dermatologist that is likely that there is a strong bias toward mild to, at the maximum, moderate skin involvement. I mean, the way Frank Behrens would do it, he would ask us to send him all our patients, and those that have joint involvement will be included. So I think this question needs to be answered on an individual basis. The question is, do you have dermatologists who would refer patients with moderate to severe disease so that you get to see them? If that is not the case, in the majority of the centers that you plan to include, I would agree that it is a good idea to ask a few dermatologists to feed in a few patients with moderate to severe skin involvement. Philip Mease: Might one way to do this be to proportion, partly based on PASI, the patients that are being entered? Alberto Cauli: No. Actually we do not have any entry criteria for PASI. Philip Mease: I understand, but again, I am concerned that we are going to get a bunch of people with PASIs of 6 and it will be okay for us, from a certain point of view, but I am not sure it will be bought in dermatology. Wolf-Henning Boehncke: I do not know how many academic centers with a hospital basically close by, would be on that list. With regard to Frankfurt, no doubt we will see moderate to severe skin involvement, too. But I simply am not familiar with everybody on that list. I would say if there is a fair amount, say, some 30% of the people who are closely cooperating with dermatologists, I think that is fair enough to get started. The reality is, that the vast majority of patients do suffer from relatively mild psoriasis, anyway. (Unidentified): I think it is very important to the PASI scoring system . It is very important information for us regarding skin data for arthritis because there is difference . . (from audience) psoriatic Alberto Cauli: Yes, and also I recommend that the same person score the PASI at the various phases. Not to change observer. Dafna Gladman: Last comment there? (Unidentified): One of the things you have got in there, is whether there is any psychological assessment that might influence your visual analog scales and I just wonder why you do not put in the patient’s assessment of where they feel they are on an anxiety and depression scale as a visual analog scale as well? That might be quite an interesting thing to correlate with your results. Alberto Cauli: So you mean, to ask the patient. Well, there are two boxes about that for the physician (Unidentified): Yes, but those are for the physician, really. Why not graded? Alberto Cauli: Well, that comes from the medical history. The physician may talk about that with the patient. (Unidentified): You could grade it, but not to a hundred. Alberto Cauli: It is difficult to grade the level of anxiety. Peter Nash: Just a very quick practical point. Desiree van der Heijde should talk to you about visual analog scales because the ASAS group found instead of a line, which does not reproduce very well, difficult to measure, takes a lot of work, she has a 1-10 in numbers along the line. Much easier to work on and for the patient to fill out. So you should ask ASAS about that. Alberto Cauli: I am open to make alteration if the majority feels that it is better. Peter Nash: They just found that to analyze and then follow them to the patient to put, instead of a cross on the line, which they always get wrong. Philip Mease: Peter, the problem is, so that is a Likert scale, but we need to do something. Dafna Gladman: No, it is not Likert scale, it is a categorical visual analog scale. So the Likert scale is when it goes from mild to moderate to severe. This is called a categorical rating scale. Vibeke Strand: I have done a lot of work comparing those, if I could just comment. Dafna Gladman: And the bottom line is? Vibeke Strand: Well, in fact, if you go back to this in RA, but it has also been shown in several other diseases, the Likerts are actually not as sensitive to change as the visual analog scale. But it has been largely believed that if you put numbers by it, then people simply remember the number and you do not see change, either. The one time that there has been a very good correlation with change is the way Guyatt has recommended the “thermometer”, which is actually a vertical scale, which has numbers on it. That has worked out quite well also when trying to look at MCID and utilities. So what we might want to try and do here is to look at the difference between a VAS that can have two anchors but should not have numbers, versus the “thermometer” about a question that would be vertical. Philip Mease: I think that is actually a good idea. My concern is that we have got an anchor in what is being done in clinical trials. Vibeke Strand: It is pretty well accepted in clinical trials, pain questions, fatigue questions, global disease, etc., do much better with VAS. But I do think that there is quite a bit of room for looking at a Guyat type of scale for those questions, too. Dafna Gladman: The problem is that we would be trying to validate two things at the same time without really having a gold standard. The question here is whether a global versus an individual disease component. So if you are now going to introduce yet another measure, another way to measure it, which has not been validated, we are going to have great difficulty. Viveke Strand: I think you would have to say that the VAS’s are generally validated and have been in most conditions. So I think you could use those as your “gold standard” and just look for test-retest variability as well as increased sensitivity to change. Sue Oliver: Just another point. If you want something that is already well-recognized and used, it is the hospital anxiety and depression scale, if you are really looking to see if there are patients who are going to have a high level of anxiety and depression, if you like, that may have factors on the visual analog scale. Alberto Cauli: That would take a lot of time to fill it out. Sue Oliver: No, they are very, very quick. Alberto Cauli: Very quick? Sue Oliver: Yeah. Dafna Gladman: So maybe you could send it to him. (Unidentified): And I have also a comment on doctor’s VAS. I think, just a suggestion, instead of the term “quiet,” “quiet skin” or “quiet joints,” I would use “none,” since “quiet” may imply some mild disease activity. Dafna Gladman: Yes, actually, that is a good point. And the other point was in your patient questionnaires, there was a difference in the wording between the global, the joints, and the skin. They all have to have the same wording. Philip Mease: I agree. You have got the joints as being slightly different than the other two, and I think they all should be worded the same. Alberto Cauli: Okay. No problem. Dafna Gladman: Thank you very much. I hope that people who cooperate with this study, because if we do it on time, we will certainly have a very important component for the OMERACT meeting, and as you can see from the amount of information that is collected, there is more than the VAS that can be derived from this study. So, we will move on, because we are running out of time, and we will ask Dominique Baeten to give us some information on the synovitis measurement which, by the way, is another feature that we really want to include in the OMERACT studies that we are doing. D. Dominique Baeten Tissue Histology Thank you, Dafna. Before starting, just to say that there was a special work group on synovitis that we had a meeting in San Antonio. We had a meeting in Dublin. I was not at the meeting in Dublin, and the people were at the meeting in Dublin could not make it here. So the data I will present to you are not really from this Psaim group, but this Psaim group is gathering again on Friday and we will come up with a proposal for a new study. So this is ongoing. The data I will present to you are essentially from our group in Ghent and also from the synovitis study group and the data are essentially the work of Elli Kruithof and Leen De Rycke. So I will touch on two aspects. The one is when you look at peripheral synovitis in psoriatic arthritis; is this really different from other spondyloarthropathies subtypes? And this was already discussed, I think, in Annals of Rheumatic Disease issue of April and so we went back to our data on synovial histopathology to see if we really have biological data to see that these diseases are different, or rather similar. Previously, we indicated that there are some differences between spondyloarthropathy and RA. And so the next step was to look within spondyloarthropathy if we could find some differences between the different sub-groups. And these are the groups that were studied by Elli Kruithof. An RA control group of 52 patients and a psoriatic arthritis group of 22 patients, and I have to say that all these psoriatic arthritis patients who filled the criteria for spondyloarthropathy. So these were essentially all oligoarticular patients. And then, non-psoriatic spondyloarthropathy being undifferentiated or AS, all with peripheral joint assessment. As you can see, the psoriatic and non-psoriatic group are quite similar. What we did was to take synovial biopsy by needle arthroscopy from an inflamed joint in all these patients and score both the histology and immunohistochemistry for a number of cellular markers, adhesion molecules, and others. So quite extensive analysis. But first, when you compare the whole group of spondyloarthropathy with RA, what we found was essentially what we found previously in the other studies. If you have some differences, for instance, in higher lining layer thickness in RA, also more dendritic cells, CD83, also more intracellular citrullinated proteins, and other specific marker Mab 12A in RA. In spondyloarthropathy as a whole, you see much more pronounced vascularity, more polymorphic nuclear cells, more CD163 positive macrophages which is a mature macrophage subset. Now, this was to essentially validate that we found the same as the previous study and that the technique is reproducible and so the next step was within these 50 SpA patients, to split up between psoriatic and non-psoriatic. This just summarizes this. Basically what we found is that the difference that we found between spondyloarthropathy and RA, we found this also between AS/undifferentiated SpA and RA, or between psoriatic and RA. So the same differences when you split up in sub-groups. On the other hand, when you compare AS with psoriatic arthritis we found no difference at all in this study. So, apparently, no difference between what I call SpA subtypes. Now one relevant question was, of course, all the psoriatic arthritis are oligoarticular. What about the polyarticular that did not fulfil the criteria for spondyloarthropathy? And this was the second part of the study; comparing 28 oligoarticular versus 17 polyarticular. The cut-off was 5 swollen joints. These are the patient characteristics, and to make a long story short, in fact we see no difference at all for those markers that discriminate between RA and spondyloarthropathy. Also, including some markers like E-selecting and CD68 that were reported previous by Doug Veale comparing psoriatic and RA. Of interest, also, the two last markers, intracellular citrullinated proteins and Mab 12A are markers that we report to be very specific for RA, and you do not find these markers in polyarticular psoriatic arthritis in this study. Now this is one study. We did several other studies where we looked at spondyloarthropathy as a whole, but also did the subtype analysis for psoriatic arthritis and other subtypes, MRPs, which are molecules secreted by macrophages, MMPs, and inhibitors of MMPs, toll-like receptors, also response to infliximab and response to etanercept and we did not see in these studies any difference between psoriatic and other subtypes. So we think the conclusion of this part is that we do not say that there is no difference, but at least, we have no evidence of any difference at this point. I think if we are analyzing larger cohorts, using more sensitive techniques, maybe we will find some difference. But of course, then the question is, what is the biological relevance of these differences? But I think more important, there are certainly other pathophysiological mediators that are of interest to study, and I think of the work that Chris did, for instance, on mediators of cartilage and bone destruction, osteoclasts, and others. So I think this is more a plea to try to build up more biological data to get back when we go to our patients and to see if we can go to pathophysiological rather than a phenotypical approach when we think of psoriatic and other associated diseases. (Unidentified): Does disease duration, or the amount of acuteness in that joint affect the histological appearance significantly? Dominique Baeten: Yes. I come back that in the second part, so there is a clear correlation between the histology and the severity. This is the disease activity at the moment of assessment. I come back on that issue. (Unidentified): What about duration of disease? Have you had a joint for ten years compared to six months? Dominique Baeten: No. If you look for duration of disease, for all these markers I showed you, there was no difference. If you have a swollen knee joint, or if you have active inflammation of the joint at the time of the biopsy. (Unidentified):And have you looked at all at vitronectin receptor and TRAP staining? Dominique Baeten: We are doing that, so I think Chris Ritchlin has some data on psoriatic arthritis. Now we are looking also in other SpA subtypes. So I think this is one of the ways we should proceed. (Unidentified): It would be very interesting to look at that and try correlate it with severity. Dafna Gladman: Chris? Chris Ritchlin: Dominique, absolutely gorgeous work. I have been quoting it for a long time now. One of the questions is Fassbender, in the forum of pathologists had written that he had really never seen the invasion of synovium into cartilage in psoriatic arthritis that you see in rheumatoid. We have not found that to be true and I wondered about your thoughts, number one. And number two, in your polyarthritic group, was this an erosive sub-group? I did not get a chance to read all the variables up there. Did they have erosions on x-rays? Dominique Baeten: Yes, they had erosions. And as to the invasiveness, of course we are taking the results from needle arthroscopy, so we are just taking biopsies of synovial tissue. We have no idea of cartilage and bone. But at least, what you see when you are doing arthroscopy on the patient is that we clearly have pannus growing over the cartilage and you see this also in spondyloarthropathy. So that suggests, at least, that there may be invasion also in these diseases. Chris Ritchlin: And the last follow-up to that, did you see any of the nodular kind of lymphocytes that you tend to see in RA in any of your specimens? Dominique Baeten: I am sorry? Chris Ritchlin: Nodular array of lymphoid follicular appearance of lymphocytes that you sometimes in RA synovium? Dominique Baeten: Yes, we see it in psoriatic and in other spondyloarthropathies. It is much more frequent in RA and we are now setting up a study in which we look at a large cohort of more than 200 samples, 100 are RA and 100 are spondyloarthropathy, at specific markers of these aggregates, looking at chemokines, specific dendritic cells, etc. so this is ongoing. Chris Ritchlin: Thank you. (Unidentified): Have you looked for regulatory T-cells in both disease groups for a CD25 high positive cells? Dominique Baeten: No, because therefore you have to double-stain, and is much more difficult to do in a large group. (Unidentified): This is very interesting to see is there any difference between these two groups? Dominique Baeten: Yes, in fact we are waiting for better markers to do immunohistochemistry assay. Philip Mease: To get at more at the lytic type changes that are seen in PsA, and weaving in the work that Chris has been doing, how do you propose to add markers in that regard? Chris has used both tissue markers as well as markers from blood samples, and so— (Unidentified): ______________________? Dominique Baeten: We have done it with the MMPs now. We are doing, for the moment, looking at osteoclast and osteoclast markers that Chris used, and we are taking in these patients’ synovial biopsies and doing stainings, and the same patients, we are taking peripheral blood as did Chris and we look at spontaneous osteoclast formation. So this study is ongoing. And we have another study started just now looking more at fibroblasts.—(end of tape. Some dialogue cut out) Philip Mease: precursors yet. You are just in the process. Dominique Baeten: Yes, I have preliminary data, so the first test that we did was on blood that had been frozen. And on frozen PBMC, we see no difference, but we are now struggling with the problem that we think that there is an artefact when you compare frozen versus fresh PBMC. So we are doing all the experiments again with fresh PBMC. So this is ongoing. Dafna Gladman: Thank you very much. This is quite fascinating. Nobody has done longitudinal studies yet on synovial tissue? Dominique Baeten: I do not know if we have time or not. I have some data on disease activity and treatment on these pages. Dafna Gladman: I do not think we have time now. Maybe after. We really should finish what we have now. Dominique Baeten: For those who are interested, this data will be shown tomorrow in the synovitis study group at 12. (applause) Dafna Gladman: Okay. Thanks a lot. I wonder if I should have Henning actually give his skin presentation first. E. Wolf-Henning Boehncke Reporting from Dermatology Actually, I was asked to focus on quality of life assessment, and time permitting, I can throw in a few additional remarks there. There is not, really, so many remarkable things going on with regard to measuring QOL in psoriasis. So where are we? I mean, there is lots and lots of instruments out there that I use to measure quality of life or aspects of this. By far, the most frequently used, obviously, is the DLQI and then there are others, a lot of others. You have seen data like this in similar studies. Perhaps this is the most frequently cited study when it comes to measuring disease severity. This is using the SF-36 with regard to mental impact of disease and comparing it to other entities and the physical impact. So that is obviously well recognized and there are numerous studies out there that cover this aspect of psoriasis. The next point, really, is when we focus on psoriasis in its own right, and not compare it to other diseases, what is the kind of data we can generate with quality of life instruments? With regard to these instruments, one can say that it is really very robust findings. Those instruments really indicate improvement when the disease is treated effectively and the best examples are the data that have been generated in the context of huge trials using biologics and treating psoriasis. This is one example of a major trial using Enbrel for treating psoriasis and you can see that the improvement of quality of life, which in this case is measured again with the DLQI, is rapid and significant. There has been a long discussion going on whether what you measure there really correlates with the objective clinical course. There have been recent abstracts at least, and some publications already, that come up with answers and I have put two citations on here. One says, particularly the DLQI demonstrated the ability to detect small but meaningful changes in clinical status over time. That has been published in 2003. More recently, there have been longitudinal studies, two, that actually asked, “What is the correlation between DLQI and PASI?” It is relatively clear from this cited poster here and there are numerous other posters using other biologics, that there is actually a parallel improvement of DLQI and PASI and that is true for treatment and retreatment. So these two follow each other quite well. That has been discussed on whether DLQI really is somehow related to PASI to the objective disease severity. When it comes to actually the practical implications of using the DLQI, we have a big “but” here. This point was raised previously, and that is, if you know how to play this, you know where you put your marks in order to earn yourself the treatment you want. We are talking about a lot of money over the years. And so far, that is an unsolved problem. Actually, this morning we were sitting together and we were looking at data that were generated in a Delphi process where dermatologists were asked to define moderate to severe psoriasis. Quality of life, interestingly enough, was not way up on that list because dermatologists are rather skeptical. I mean, we understand that it is bad to have these skin changes, but we also seem to understand that our patients are good actors every once in a while and they know how to receive the kind of treatment they want. So perhaps, it is not too surprising that dermatologists do not like quality of life assessment when it comes to grading disease severity. They also oppose the idea of following the patient’s perspective. So one of the items asked “What influence should patient’s opinion have on your treatment decision?” And it was also very low. I will forward those results because I think they matter in the skin boxes which we have seen on the grid previously. Maybe a better way of measuring quality of life is really the participation, and I am really looking forward to seeing the results in Will Taylor’s efforts to generate those because I think this is where the solution is. Since you called it the “Derm Perspective,” I should at least briefly mention skin assessment as something that I understand it, is actively pursued by the International Psoriasis Council, and I am in contact with who is basically coordinating these activities on skin assessment. I think the best strategy for me is to have my ear very close to Berlin, see what they do, and let GRAPPA know what they do because I do not think it is worthwhile doing the same thing in parallel. After all, this is an initiative that has been started by dermatologists. Although, I must confess, that I personally love GRAPPA because of the dynamics here and I am still not so sure whether they will be ready with something to show on the occasion of OMERACT 8 in Marta next year. Finally, there is a lot of guideline writing going on. Actually, I broke my arm on writing a guideline. To tell you the truth, it was slightly thereafter, on the occasion of meeting. We will have our guideline on the status of getting the consensus this weekend. So from here, I will travel to Berlin and we will have the consensus on, actually, the efficacy and safety aspects, and then they will go into the clearing phase. Maybe this is the point where I can also communicate this consensus toward GRAPPA because we then could perhaps make use of a more differentiated way of looking at the different classics established as well as biologic antipsoriatic therapies. At least, I will try to get their “okay” that GRAPPA can have a look at it and maybe adapt aspects of this. So this is all I have to say for now. Thank you very much for your attention. (applause) (Unidentified): Henning, I have a question for you. One of the things I have noticed in treating patients with psoriatic arthritis is that with the onset of newer agents, that the bar for psoriasis has gotten incredibly high with many individuals. For example, how the patient who has had horrible psoriasis, we treat him with an agent, the psoriasis gets tremendously better, but if he or she gets a little bit of a patch there, their quality of life is all of a sudden plummeted in ways that I would not have expected. How do you think about this and how do you adjust for this when you are trying to develop these kinds of measures for the skin? Wolf-Henning Boehncke: We see this progress from fighting how to control the disease somehow, to getting means of blowing it away. And actually, if we were ever allowed to use it on a continuous basis, we would keep our patients symptom-free with regard to the skin, that is for sure, and patients use this. So, I think this is more a political issue about treatment goals. What is a sufficient response? What would allow us to terminate treatment? I would say, we are in the midst of this process. Our patients definitely do not want to wait for the next rash of psoriasis occurring, but the treatments that would allow us to do so are simply very expensive. We may see a change in policy when your less expensive drugs get along. I am thinking about BG12 which may come with the price tag 30% of the price of a biologic and could be envisioned as a continuous therapy. The patients know that we could, basically we have the means, to keep them symptom-free, and that influences the level. Yes, are you satisfied with +/- 75 or are you more and more moving toward +/- 90 or really symptom-free. We have not answered the question yet, I would say. Paul (?): Just to comment. We run two combined clinics in Oxford, and the dermatologists that we work with hate the PASI. They loathe it. They think it is difficult to administer. They run a mile at the suggestion of using it. And that does not seem to be an unusual experience. Most dermatologists I speak to in Britain think it is horrible. I just think there should be some sort of mood going out from this meeting to the dermatologists to say, “Is there any way you can improve on the current, very unwieldy, difficult to administer, assessments?” I am sure it must possible to do it. Wolf-Henning Boehncke: Obviously, they are working on it. That is why BSA made it into the skin box, because BSA is a much easier way. On the other hand, it is tough to judge on treatment response, because psoriasis does not clear patch by patch. The thick, scaly patch loses scaliness and uses infiltration and slowly but surely gets less and less red. You do not see that when you measure or judge upon BSA. So, the answer is the PASI still is the most reliable read-out we have, but practically, nobody likes it and most people do not use it. So we basically, I think, in private practice, most people would use PGA. Paul (?): I was just thinking along the lines of dactylitis being an indicator of more progressive, severe disease is psoriatic arthritis. Maybe that is moving toward a single instrument one can use to assess severity. If there are other things that one can do in the skin like that, it would be useful. Wolf-Henning Boehncke: If you are only talking about mild, moderate, severe, what came out pretty nicely in this Delphi process was once somebody shows signs of joint involvement, immediately, this is the rocket shooting at patient from mild to at least moderate, if not severe, no matter what the PASI would say, or BSA or whatever. So in that regard, we are very pragmatic. But in regard to skin assessment tools, you are absolutely right—PASI is not loved at all. PGA is what most people would use outside of clinical studies. That is true. Dafna Gladman: Thank you very much. So we are actually catching up with ourselves, and Philip will finish the last two items on our agenda. First, reporting on the World Congress, and second, on the Publication Committee. Philip Mease: Thank you, Dafna. So, by the way, having sat in on a number of dermatology meetings where skin scoring systems are being debated, it is a fairly complex issue, Peter. F. Philip Mease World Congress (PsO/PsA) in Stockholm My purpose here is to talk about a meeting that has been proposed and is significantly underway in planning. The group that first brought this to us was the group from IFPA, which stands for International Federation of Psoriasis Associations. So these are directors of patient service leagues in different parts of the world. The key individuals are listed here: Lars Etarp and Bergita Rambe from Sweden, and Jan Mosbakken from Norway, and then Gail Zimmerman and Sheri Decker, both of whom are with the Psoriasis Foundation in North America. They approached Ken Gordon and I to discuss the possibility of having a combined physician meeting with patient service league organizations. Mark Ledball agreed to be the chair, and then the physician Steering Committee are listed here: several dermatologists and then Dafna as well. So the idea was to have something like the International Lupus Meeting, or to a certain extent, like the ACR, to the extent that it does things in coordination with the Allied Health Group or the Arthritis Foundation, or the Diabetes Meetings, where there are in parallel, physician meetings with scientific presentations, as well as a parallel set of sessions for patients and/or patient service league directing or representatives. We have an estimate of anywhere from 400 to 800 attending. We looked at variety of times that were possibilities and this one was settled on, both because of availability as well as trying not to conflict with other meetings, although I have to acknowledge, that when you think about OMERACT is, in the middle of May 2006, and when you think about when EULAR is, which fortunately, is more toward the end of June next year, it is going to be a little bit difficult, especially for those travelling from North American, or say, New Zealand and Australia. There were a lot of advantages to this time in terms of not conflicting with dermatology meetings, and another issue that came out that was a sensitive issue, is that the International Psoriasis Society has typically met in June of each year over the last several years, but next year, is not meeting. So the thought was, do this at a time when it is not in direct competition with that meeting and get a feeling for whether this might take off as an idea for every other year, or an every third year meeting. Key points were that it would be an opportunity to bring rheumatologists and dermatologists together as well as the allied health personnel, such as nurses, nurse practitioners, and so forth. The tentative agenda is, I have given you some ideas here, arrival late Tuesday, May 30, or early Wednesday, May 31. On Wednesday, have in the earlier morning, task force meetings. For example, if the histology/immunohistochemistry group wants to meet, or if there is a genetics group, etc, etc. Henning, you laugh. Wolf-Henning Boehncke: (laughter) Philip Mease: Oh, I see. And then the other is to have a conjoint meeting between GRAPPA and the International Psoriasis Council that Alan Menter is heading up between 11am-5pm, so as to have an opportunity to present to each other, somewhat like the way we are presenting and discussing today, followed by a reception dinner. Then Thursday, we would have the morning for genetics. Dafna, I forgot who was the dermatologist that had been assigned—oh, Jonathan Barker is assigned there. Have a mid-day industry symposium each day, partly for sponsorship purposes for the meeting, and then in the afternoon, have an immunobiology and pathophysiology session. The idea would be that in each session, there would be a dermatologist and a rheumatologist, each taking 20 or 30 minutes to do a brief overview of the field, and then to have invited abstracts, or submitted abstracts. What I mean by invited abstracts, for example, if Dominique could submit a review abstract on the kind of material that he has been developing over time, as an example of something. It does not have to be a discreet, new study. Whereas others might submit that. Then, the thing that the people in Sweden are so excited about is this notion that the king of Sweden has at least said that he will be present at the dinner reception in town hall. So, the draft flyer has this sort of benign-looking picture of the king of Sweden on it. Then on Friday, we would be, in the morning, having a session devoted to quality of life function and participation discussion with the two co-chairs being Peter Van de Kerkof and Will Taylor. Again, a mid-day industry symposium. Then, the afternoon was kind of a novel idea that Ken Gordon came up with which was to have a physician and a patient service league director from each continent present issues, problems, unique issues around psoriasis and psoriatic arthritis in their part of the world, and that could be a conjoint meeting between the physicians at the meeting as well as any patients that are meeting in a parallel set of sessions. That would be in the first portion of the afternoon. In the second portion of the afternoon, for GRAPPA and IPC representatives to present to the group, because many of them may not necessarily have arrived by Wednesday, something about what the groups are doing to sort of introduce themselves to more individuals who are attending the meeting. Then, again, have dinner. Saturday, the whole day is for a clinical session on clinical manifestations, disease assessment, and treatment, with treatment probably occupying most of the afternoon. Each day, by the way, the intent is to have a poster session in the early morning along with coffee and pastries. And then, Sunday departure. So that is an overview of how the meeting would go. There would be a parallel program for patient service leagues, allied health personnel, and patients. So that is the thought behind the meeting. Any questions, comments, criticisms, potshots at this whole idea? Vibeke? Vibeke Strand: I think it is a tremendous idea. Is it about two weeks after OMERACT? Philip Mease: It is. Vibeke Strand: So, people are going to take a month vacation in Europe? Philip Mease: Believe me, we knew this absolutely, and we also knew EULAR. Now, I am planning to fly home, work, and then come back to this. Vibeke Strand: And when is EULAR, again? Philip Mease: EULAR is around June 20 or so, so it is three weeks after this particular session. I apologize, but believe me, we looked at every other time of the year and it was awkward for one reason or another. Henning. Wolf-Henning Boehncke: I think it would be very important when announcing this to make clear what the uniqueness of this meeting is, because there are many, many activities in the field of psoriasis and psoriatic arthritis. I think this message must be spread that this is kind of a joint thing, and that there are some very unique sessions that are planned for that. So besides, the king of Sweden being there. (laughter) Otherwise, I think everybody would say okay, yet another psoriasis meeting and that is the danger I see. I know that very few Europeans like these international psoriasis meetings. Very few people travel to those. Philip Mease: That is why we put it in Sweden as opposed to, say, North America. Wolf-Henning Boehncke: Maybe, but, there are numerous unique features of that. So when that word spreads, I think everybody will be very curious. Philip Mease: Right. I agree with you. Some of the response among the psoriasis thought leaders has been that they are “meeting-ed out.” I think that there are fewer meetings in psoriatic arthritis although it ironic that it is falling at a time when we have several meetings in a row going on. Now, in terms of logistics, in terms of financing, we have not gotten there yet. We have acknowledge to people coming to OMERACT that we want to support them financially to do that. We have not gotten to that point in terms of GRAPPA supporting people for coming to this. This is a larger number of people that we talking about. So, as the time gets closer, we will have a better sense of that. These are the sponsors thus far that are committed to supporting the meeting and there will be a number of others that will be approached and getting on board, presumably. February 1, 2006 will be the deadline for the submission of abstracts. They are all going to go to a person at the National Psoriasis Foundation and then be distributed out to the different program chairs. G. Philip Mease Publications Committee As you can see, there are only a few slides. Publications Committee. This was the major product from the GRAPPA group over the course of the last couple of years. This was quite a project. A lot of time and effort by the various people who contributed as authors and by the editor group that reviewed the project and working with a writer/editor type person based in New York, as well as Robin Shapiro in helping give birth to this. Now this is available free by going online and downloading it from the Annals of Rheumatic Disease web site. In terms of the Publications Committee, the current composition is Dafna, Jerry Kreuger, and myself, Christian Antoni has recently stepped off the committee as he has gone into industry. Really, our major publication activities have been the birthing of the supplement and then an OMERACT workshop summary from the previous OMERACT session. So questions for us to address: should there be a fourth member to replace Christian? Might it be a European? Might it be a dermatologist? What should the rotation schedule be? Every two years, or other frequency? How many members at a time? So, one or more of us should step down? I mean, these are all open questions, and just to pepper your thoughts with some future publication projects—I suspect that there will be the whole PsA guidelines project that Artie and Chris are leading. That will be a major article. We will have an OMERACT module summary after the next OMERACT meeting. Committee projects probably are going to be deserving of their own manuscripts and the person leading that project will likely be lead author. Then, there will come up the question of who else might end up being authors. There are some questions around whether GRAPPA should be designated in the paper. Periodic review updates. I was mentioning this morning to someone about the GRAPPA supplement, and the first question they had was, “When are you going to do your follow-up?” I know. And if so, shall we continue using Annals of Rheumatic Disease? Should we do periodic review updates about the field in rheum or derm journals? One of the things that we have toyed with is the idea of trying to have a part-time writer/editor to assist people in writing projects. That might help increase the amount of writing activity going on. So, all of these things that have question marks, I invite commentary from people about this. Chris, go ahead and use the microphone. Chris Ritchlin: Regarding the whole structure of GRAPPA, Rob, do we have a committee that is in charge of doing that? Usually there is a committee that is in charge of setting up those kind of things. Membership. Is that something we should think about? I think we have to put together guidelines for this, and we want to get a lot of people involved in running GRAPPA and have more participation. Maybe we should create a membership committee to help structure that? Does that sound reasonable? Philip Mease: Uh-huh. (Unidentified): ? (from audience) Philip Mease: It has mainly been people stepping forward. Oh, in terms of Steering Committee. That arose some time ago and as Chris has just pointed out, we really do not have an internal structure for making changes in that. The way the ASAS working group evolved in this regard was that they had an initial Steering Committee, somewhat analogous to the way we have had it, and then ultimately after two or three years, they evolved into having an Executive Committee which has a very small number of people which helped make some of those recommendations. We could turn to them. But we actually do not have set guidelines in this regard. At the moment, we are trying to get a fairly equal amount of representation from both rheumatology and dermatology, so that is one principle that we have been trying to pursue. (Unidentified): . (from audience) Dafna Gladman: Maybe we can go back to the beginning when GRAPPA was first formed, there was sort of a committee that was established through CASPAR. CASPAR was the glue or the drop that started this, and then from CASPAR, there was a committee that was formed which was the basis of the Steering Committee that we have now, and then to this Steering Committee, we added more people both to represent both sides of the Atlantic as well as both derm and rheum. We are now at this situation where I think Christopher is quite right. We have grown a lot faster and matured a lot quicker than ASAS has done because it took them two to three years and it has taken us a little bit shorter to come to a point where we really do need to establish a better structure. The big difference between GRAPPA and ASAS is that GRAPPA has been inclusive, more inviting. We like the idea that we have a wider membership. We certainly prefer to continue to have this interaction between dermatologists and rheumatologists. Whereas, at the EULAR and at ACR, we tend to have primarily rheumatologists with very few dermatologists. It is the American Academy of Dermatologists and the European Academy of Dermatologists which Philip and I have attended for the last two years, there is a large cadre of dermatologists with a very small group, usually two or three, rheumatologists that have come. Although, at the AAD last year, we actually had a much larger representation of rheumatologists. Because of the fact that we are so large, it has been a lot more difficult to actually get the same people together every time so that we can go through some sort of a voting mechanism. Of course, it is not the end of the day. The majority of people are not here. So, the question is, how do we deal with moving on to some kind of a more structured format? Paul, you have a comment? Paul (?): Not directly related to committee structures, but related to much bigger issues that not only would relate to therapeutic research and clinical trials, but also into the basic disease mechanisms here. There are now efforts which are well established to look at the genetic basis, for example, of susceptibility to common diseases like diabetes and rheumatoid, ankylosing spondylitis, lots of infectious diseases using whole gene and association studies. It does seem to me that a grouping like GRAPPA has a real potential role to play in putting together the clinical material that could be put through this type of mechanism that now exists technically. It is an opportunity to, I mean it may not work, but it is a very novel approach which could be very exciting for us to get involved in. Dafna Gladman: Yes, certainly. I mean, we have not mentioned a Genetics Committee, but that is the next research item on the agenda. So, what has happened up until now, you can see, Philip has done a remarkable job together with Robin, of getting us the financial base, for the organization of this group. Together, we have made all of the decisions in terms of content and progress and so on. The committee structure arose through our meeting at EULAR last year and basically was the product of the OMERACT results. We said, “Okay, now we have to deal with these, but the two of us cannot do this.” So, we had people volunteer to pick a subject that was close to their hearts so that we could move on. The Publication Committee consisted of four people, and you can imagine for four people, you have seen the end result, but the four of us actually spent umpteen hours going through the various manuscripts and sending it back to the editor, and the editor had to send it back to the writers, and then we had to read it again and make sure it was the way we wanted this end product to look. This is a big commitment and I actually think that the Publication Committee should probably be a little bit larger so not everybody has to ready everything that goes through. So, just like in a Review Committee, not everybody reads all the applications to the same great detail. I would recommend that we increase the group to six. Again, keep our model of having derm and rheum, and international participation. Philip Mease: And then, any suggestions about the process of voting people on, and/or rotation off? How should that be determined? We are quite open. For example, I have no vested interest in staying on the committee. It was a lot of work, although I think it was worthwhile given the product of the first group’s efforts, but very happy to move along, and we need to have some orderly process of making the change and then getting new people on. Dafna Gladman: I would suggest that we put more people on and then we start getting off. I tell you, my biggest concern is, if we do not have people who actually continue this, it is going to fall apart which is why the Steering Committee, at the moment, has got appropriate representation from both Europe and international as well as North America, as well as derm versus rheum, and this committee has just started to work together just a few months ago. I think if we make any changes there, we are going to lose the momentum that has moved forward. So I would say, let us put more people on and let people start getting to work in the area, and then the three of us that are still left from the original two years ago can step back. But I think if we all step back, or even if one steps back now before other people start to put their teeth into it, we will not be able to appropriately move forward. (Unidentified): . (from audience) Dafna Gladman: Exactly. Absolutely. Philip Mease: Any ideas about how people who are interested, to put their names forward? I suppose that we could circulate emails. Dafna Gladman: How about the Web site? Yeah. When there is a note posted on the GRAPPA web site, you get an email. So, everybody will get an email that says there is a message on the web site and they have all the instructions on how to get on. And those people who do not have their proper ID, maybe Robin can put at the bottom, “If you do not have the proper ID, contact— “ Philip Mease: So let us say ten people say, “I would like to be on the Publications Committee.” Do you have a suggestion about how to move from there? Dafna Gladman: Well, for starters, we already said we need East, West, North, South, derm, rheum, so we start going through the list. Philip Mease: Do we, as an oligarchy, select them? Dafna Gladman: No, I think there is a Steering Committee. So we do not decide. We have a group of about ten people on a Steering Committee. So we already have a body for the time being that can help. Philip Mease: That begs the questions, too, then, how about the composition of the Steering Committee and how that should be refreshed. Dafna Gladman: That is something that needs to be decided, but I think, again, it needs to be decided with time. I do not think we need to do this today. We decide we are starting fresh with new executives—first of all, half the people are gone. Wolf-Henning Boehncke: I suggest to put this on the agenda for the Stockholm meeting because most likely, many GRAPPA people will attend there, and this is about the future, the mid to long-term future of GRAPPA. Until then, I think it has been a success story so far. So right now, we need more people on the Publication Committee and I think you should take the freedom to decide for now because so far, you have done a great job and basically people are trustful. If you are lucky enough that there are ten or twenty people, well, I do not know, maybe that would be great. Maybe you are not in that situation. If you are, I think it is fair to say, we will come up with an interim solution and we will try to really put an agenda together for 2006 for Stockholm to address a handful of key questions how GRAPPA shall develop in the future. We certainly cannot decide here and now. I doubt whether email discussions are the same thing as being physically together and I think the Stockholm concept has the potential to lure people from GRAPPA there so we are a considerable number of people to then really decide and constitute certain policies or so. Saying this, I wish you a nice evening. Philip Mease: Thank you, Henning. Thank you so much for being here. Will, you had raised your hand a moment ago. Did you have a comment to make? Will Taylor: Just to echo what Henning said, and to advance it a little bit more, it could be sensible to leave the Steering Committee to develop some kind of constitution that could be presented at the Stockholm meeting as a basis for something concrete to discuss. Philip Mease: For governance. Will Taylor: Yeah. Dafna Gladman: Sounds very reasonable to me. Philip Mease: If there are no other comments or questions or suggestions, consider the meeting adjourned. Thank you for being here. (applause)