RLF - campus - D`Youville College
advertisement

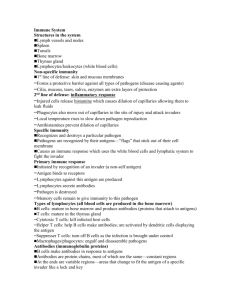
D’YOUVILLE COLLEGE PMD 604 - ANATOMY, PHYSIOLOGY, PATHOLOGY II Lecture 5: Immune system & blood groups G & H chapters 34, 35 & Robbins chapter 5 1. Body Defenses: • nonspecific immunity – innate immunity: skin, mucous membranes (e.g., lungs, GI tract), and external secretions (e.g., saliva, tears) represent barriers to entry of microbes - phagocytes, natural killer cells (NK cells) - acute inflammations, fever & antimicrobial chemicals obstruct spread of infections • specific immunity – acquired (adaptive) immunity: delivered by lymphocytes - specific for offending agent; has capacity for recognition - responds to specific macromolecular markers of foreign cells or organisms (antigens), which present specific identifying features (epitopes) that elicit specific responses - specific immunity exhibits tolerance of ‘self’ - includes two patterns: antibody-mediated (AMI or humoral) response is delivered by B-lymphocytes - cell-mediated (CMI) response is delivered by T-lymphocytes - AMI & CMI operate collaboratively with each other and with nonspecific defenses (figs. 5 – 1, 5 – 2 & ppts. 1 & 2) - specific immunity produces slow, weak initial response, but mounts stronger response upon encounters that follow initial exposure (learning) (fig. 34 – 3 & ppt. 3) 2. Lymphocytes: • T-lymphocytes: progenitors of cell-mediated immunity and facilitators of antibody-mediated immunity (humoral immunity) - two well understood types: helper T-cells (TH) & cytotoxic T- cells (CTLs) - originate in bone marrow; mature in thymus (primary lymphoid organ) • B-lymphocytes: progenitors of antibody-mediated immunity assisted by helper T-cells (TH) - originate & mature in bone marrow (primary lymphoid organ) • NK cells: ‘natural killer cells’ - large granulated lymphocytes that respond to antibody-coated infective agents or to virus-infected or tumor cells (ppt. 4) PMD 604, lec 5 3. - p. 2 - Lymphoid Tissues and Lymphocyte Traffic: • primary lymphoid tissues: - red bone marrow - repository of stem cells for formation of all types of formed elements of the blood; site for development of immunocompetence & selfrecognition for B-lymphocytes - thymus gland - site for development of immunocompetence & selfrecognition for T-lymphocytes • secondary (peripheral) lymphoid tissues: spleen, regional lymph nodes, & gastrointestinal lymphoid depots (tonsils, Peyer’s patches, & vermiform appendix) + free lymphocytes scattered in various body tissues • lymphocyte traffic - lymphocytes produced in bone marrow develop further in marrow (Bcells) or migrate via bloodstream to thymus gland for further development (T-cells) - competent cells from marrow and thymus circulate in bloodstream to populate secondary lymphoid tissues (fig. 34 – 1 & ppt. 5) - guarantees strategic location for encounters with antigens; antigenactivated lymphocytes linger in lymphoid depots and freely circulate in blood 4. Maturation of Lymphocytes: • lymphocyte clones: both T and B cells bear surface receptors (T cell receptors or antibodies on B cells) - receptors on one type of B or T cell are unique and all cells of a given type constitute a clone; lymphocyte population of the body consists of a billion or more clones, each with its own unique receptor - clones are produced in maturation process & represent recognition capability for virtually all possible antigens that may be encountered • screening of lymphocyte clones: in the immature immune system, lymphocyte screening (B-cells in bone marrow, T-cells in thymus gland), eliminates (by apoptosis) clones that may attack self - T cells or B cells that have undergone maturation and join the lymphocyte traffic will be immunocompetent as well as self-tolerant - until they have had their first encounter (sensitization) with the antigenic determinant for which they bear specific receptors, they are considered naive • antigens - complex molecules on the surface of microbes as well as normal body cells; most antigens will have a number of immunogenic features, called antigenic determinants (epitopes), so may stimulate several lymphocyte clones • self-antigens are displayed on the surfaces of normal body cells and are known as MHC (major histocompatibility complex) proteins; also known as HLA (human leukocyte antigens) in humans PMD 604, lec 5 - p. 3 - - serve as presenters of antigens on surface of infected cells or on antigenpresenting cells (APC) - class I MHC proteins are expressed by all cells and interact with cytotoxic T cells (CTL) expressing CD8 receptor proteins; presentation of endogenous foreign antigen may indicate virus infection or carcinogenic state (tumor cell) - class II MHC proteins are expressed only by antigen presenting cells and interact with helper T cells (TH) expressing CD4 receptor proteins; exogenous foreign antigens are recognized this way PMD 604, lec 5 5. - p. 4 - Antibody-Mediated Immunity (AMI): • antibodies (fig. 34 – 4 & ppt. 6) – Y-shaped protein molecules that are products of and receptors for B cells; circulate in plasma as immunoglobulins - Fc fragment (constant fragment = stalk of Y) binds to surfaces of defensive cells (e.g. B lymphocytes, phagocytes, mast cells, NK cells) - has different properties for different classes of immunoglobulin - FAB fragments (variable fragments = branches of Y) bind to unique epitope of antigens - antigen-antibody binding (immune complex formation) results in: - neutralization of toxins, agglutination (clumping) of cell-bound antigens, precipitation of soluble antigens, complement fixation --> promotes phagocytosis (opsonization), inflammation (stimulation of mast cells, chemotaxis), and lysis of offending cells (by activated complement and activated NK cells) (fig. 34 – 5 & ppts. 7 & 8) • immunoglobulins (ppt. 9) –constitute fraction of plasma proteins and include five categories – IgA (often a dimer – found in external secretions) - IgD (poorly understood) - IgM (pentamer - ppt. 10) delivers initial response (mainly to bacterial infections), followed by IgG (commonest); both are complement-fixing antibodies - IgE (involved in parasitic infections and in allergies), binds (via Fc component) to mast cells to promote anti-allergen & anti-parasitic reactions • sensitization (fig. 5 – 5 & ppt. 11): - antigen-presenting cells (APC) are cells that have phagocytosed antigen (macrophages, B cells, dendritic cells) (ppt. 12) - antigens are presented on surface in association with MHC markers (ppt. 13) - T cells of appropriate clone are activated by antigen recognition (clonal selection) and stimulated to proliferate a population (clonal expansion) of active helper cells as well as ‘memory’ cells (fig. 5 – 6 & ppt. 14) - B cells activated by antigen binding proliferate a population of plasma cells (secrete specific antibodies) as well as ‘memory’ cells; antibody titer (specific for activating antigen) becomes elevated (fig. 5 – 7 & ppts. 15 & 16) - clonal expansion (plasma & memory cell formation) can be undertaken by B cells with or without the intervention of helper T cells, however, B cell activation is facilitated by lymphokines from activated T helper cells 6. Cell-Mediated Immunity: • TH cells interact with antigen presenting cells and undergo clonal expansion (fig. 5 – 6 & ppt. 14) - these helper cells facilitate clonal expansion of several other cell types specific for the antigen, i.e. same clone (cytotoxic T cells, NK cells), and activate macrophages through release of lymphokines (interleukins) (fig. 34 – 8 & ppts. 17 & 18) PMD 604, lec 5 7. - p. 5 - Blood Groups: • red blood cell antigens: hundreds of antigens (not HLA) have been identified on red cells; however, two main classes invoke immune responses of clinical significance: A & B of the A-B-O system & D (Rh factor) of the Rh+/Rh- system • ABO system (table 35 – 1): - individuals with A antigen (agglutinogen A) are type A (genotype AO or AA) & recognize B agglutinogen as foreign and make antibodies (anti-B agglutinins) against it - individuals with B antigen (agglutinogen B) are type B (genotype BO or BB) & recognize A agglutinogen as foreign and make antibodies (anti-A agglutinins) against it - individuals with both antigens are type AB (genotype AB) & recognize neither A agglutinogen nor B agglutinogen as foreign and make no antibodies against them - individuals with neither antigen are type O (genotype OO) & recognize A agglutinogen & B agglutinogen as foreign and make antibodies (anti-A & anti-B agglutinins) against them - testing blood group can be achieved by obtaining blood sera containing anti-A (from type B individual) or containing anti-B (from type A individual); incompatibilities produce agglutination (clumping of red cells) (table 35 –2) • Rh system - individuals with D antigen (Rh factor) are type Rh+ (genotype Dd or DD) & do not make antibodies - individuals with no D antigen are type Rh- (genotype dd) & recognize Rh factor as foreign and make antibodies (anti-D agglutinins) against it • transfusion reaction: agglutination of incompatible donor cells - agglutinated cells can block blood vessels (embolization) & eventually undergo hemolysis releasing toxic substances that may cause circulatory shock &/or kidney failure 8. Active and Passive Immunization: • vaccination: active immunization with sensitizing dose of antigen - vaccines are prepared from dead microorganisms, weakened microorganisms (attenuated), or inactivated exotoxins of microorganisms - administration of vaccine elicits primary immune response so that subsequent natural exposure to the antigen will vigorously and rapidly dispatch the offending agent; an otherwise dangerous or lethal first encounter can be avoided • antiserum administration: passive immunization with donor antibodies or manufactured antibodies (monoclonal antibodies) - temporary protection from infective organisms, e.g. inoculations for travelers to exotic locations PMD 604, lec 5 - p. 6 - - protection during immune system’s development of sensitization to an infection, e.g. rabies shots - prevention of sensitization to Rh incompatibility between mother and fetus (ppt. 19)