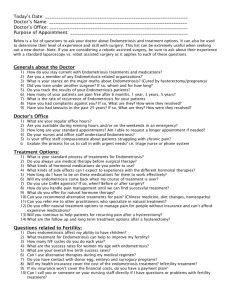
Endometriosis: A Mystery Tour for the Clinician and
advertisement

Endometriosis: A Mystery Tour for the Clinician and Patient W. Ledger, W. Schlaff* and D. Olive** Jessop Hospital for Women, Sheffield, United Kingdom *Department of Obstetrics and Gynaecology University of Colorado Health Sciences Centre, USA **Department of Obstetrics and Gynaecology, Yale University School of Medicine, USA Endometriosis is a chronic, recurring disease, often associated with infertility. It can affect women at any stage in their lives, but is most common in the reproductive years. Despite high incidence figures, the causes of endometriosis are still open to debate. In addition to uncertainty over pathogenesis of the disease, endometriosis is often misdiagnosed leading to delays in treatment, sometimes for several years. Such delay may result in disease progression, lack of symptom control and increasing incidence of infertility. Symptoms of endometriosis have been confused with conditions such as pelvic inflammatory disease, irritable bowel syndrome or even psychosomatic problems. By following a single case from first presentation, the chronic nature of endometriosis and the problems faced by patients and clinicians will be illustrated. Initial Presentation Mrs B, a 32-year old woman, presented with pelvic pain and dysmenorrhea suggestive of endometriosis. She was referred to a gynaecologist by her GP after several years of repeat visits to him for the same problem. Her GP had previously tried prescribing the continuous oral contraceptive pill (OCP) and a non-steroidal anti-inflammatory drug (mefenamic acid), neither of which proved effective. Analgesics and the OCP are often prescribed in these circumstances even though there is little robust data to support their use. Diagnosis At laparoscopy, widespread superficial endometriosis was visualized. Visible lesions were treated with electro-diathermy. Many physicians and some patients feel that laparoscopy is currently the only reliable way to confirm a diagnosis of endometriosis. The benefit of laparoscopy is that it permits a ‘see and treat’ approach, though the effectiveness of laparoscopy may be limited both by the nature of the disease and the surgeon’s skill. Management After initial improvement, her pain returned and she was given 6-months treatment with a gonadotrophin-releasing hormone agonist (GnRHa), Zoladex. She became pain free and amenorrhoeic, though she did experience hypoestrogenic side-effects such as hot flushes and night sweats. After some discussion, it was decided to continue treatment with Zoladex for a further 18 months with addback. The combination of GnRHa plus addback provided continued relief from her endometriosis symptoms and protected her from menopausal-like side-effects. The observation that endometriosis is rarely seen in hypoestrogenic post-menopausal women, led to the concept of treating the disease by inducing a pseudomenopausal state. Continued exposure to GnRHas leads to a hypogonadal state with decreased release and suppression of oestradiol from the ovaries. Use of GnRHas as a diagnostic test to determine whether pelvic pain is oestrogen-related, is also currently being evaluated for patients who continue to suffer pain when laparoscopy is unrevealing. Repeat therapy or extended periods of treatment with GnRHas have previously been limited due to their effects on bone mineral density (BMD). However, the loss of BMD does show a gradual return towards baseline following treatment discontinuation. By giving addback using an oestrogen/progestogen preparation with a GnRHa: • the impact of treatment on BMD loss is reduced • vasomotor symptoms such as hot flushes are relieved • efficacy of treatment on endometriosis symptoms is unaffected.1 Infertility Mrs B and her husband returned expressing their desire to start a family, so GnRHatreatment was stopped. Although her periods resumed, she was unable to conceive and after 6 months she was experiencing severe dysmenorrhea. She was treated with a GnRHa for 3 months and then commenced in vitro fertilization (IVF) while still down-regulated. IVF was successful and she later gave birth to a healthy son. Endometriosis is often diagnosed in women with infertility (20–68%) and infertility is a common sign of endometriosis.2 Controlled studies have shown that ablation of endometriosis laparoscopically partially improves fertility, by approximately 13% over 1 year.2 As laparoscopy is an important part of any infertility work up, ablation of any lesions seen during the procedure is suggested in order to improve fertility. Disease Recurrence Post-partum, Mrs B breast-fed for 6 months and was period free. When menstruation resumed, she again suffered pain and other symptoms. Ultrasound revealed severe disease with endometriomas present on both ovaries. Laparoscopically, bilateral ablation was performed on the endometriomas followed by a further 3 months with a GnRHa. With Mrs B’s desire for a second child, IVF was tried again. This was also successful, with the addition of a daughter to the family. Radical Surgery Following the birth of her second child her endometriosis recurred and she requested definitive treatment. She felt her family was complete and total abdominal hysterectomy with bilateral oophorectomy was agreed as the next course of action. She is now well and receiving hormone replacement therapy (HRT). Ovarian cystectomy, oophorectomy, hysterectomy and total hysterectomy are radical options which, while often curative, are unsuitable for women wishing to retain fertility. Following radical surgery involving oophorectomy, patients often require HRT. Conclusion The enigma that is endometriosis requires decision making at every stage by physician and patient alike. The complexities surrounding diagnosis, when to treat, sequence and combinations of treatment all add up to a truly mysterious disease. References .1PICKERSGILL A. GnRH agonists and add-back therapy: is there a perfect combination? Br J Obstet Gynaecol 105: 475–485, 1998. .2MARCOUX S, MAHEUX R, BֹRUB ֹS et al. Laparoscopic surgery in infertile women with minimal or mild endometriosis. NEJM 337(4): 217–222, 1997.