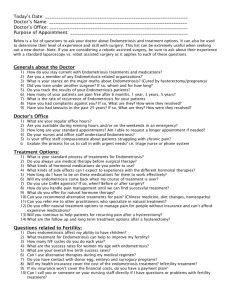
treatment of pelvic pain
advertisement

In the name of God Endometriosis symptoms of endometriosis • pelvic pain, • infertility, • pelvic mass Treatment options • • • • • • • • • ●Expectant management ●Analgesia ●Hormonal medical therapy •Estrogen-progestin oral contraceptives, cyclic or continuous •Gonadotropin-releasing hormone (GnRH) agonists •Progestins, given by an oral, parenteral, or intrauterine route •Danazol •Aromatase inhibitors ●Surgical intervention, which may be conservative (retain uterus and ovarian tissue) or definitive (removal of the uterus and possibly the ovaries) • ●Combination therapy in which medical therapy is given before and/or after surgery • Laparoscopy is the gold standard for establishing the diagnosis of endometriosis, and provides an opportunity for conservative surgical treatment. • Therapeutic intervention is desirable at the time of diagnosis to ablate or excise implants and adhesions, thus potentially preventing or delaying • expectant management is considered primarily for two groups of patients: • women with no or minimal symptoms • perimenopausal women TREATMENT OF PELVIC PAIN • empiric medical therapy prior to establishing a definitive diagnosis by laparoscopy • medical interventions neither enhance fertility nor diminish endometriomas or adhesions • Therefore, women with suspected endometriomas and advanced stages of disease, or infertility, are more appropriately managed surgically. • • • • • • Analgesics Estrogen-progestin oral contraceptives GnRH agonists Progestins Danazol Aromatase inhibitors Surgical management • Surgery may be indicated for management of endometriosis that cannot be treated with medical therapy or to provide a definitive diagnosis. INDICATIONS • Surgery allows both diagnosis and management for women with known or suspected endometriosis. Indications for surgery include: • ●Failure of medical therapy to ameliorate symptoms • ●Women who decline or have contraindications to medical therapy • ●Need for a definitive diagnosis of endometriosis – • ●Exclude malignancy in an adnexal mass – Endometriotic implants may develop into an ovarian cyst (endometrioma). • ●Treatment of infertility in selected women • ●Obstruction of the urinary tract or bowel. • Making a definitive diagnosis requires surgery to visualize and/or biopsy lesions. • Women with mild symptoms suggestive of endometriosis are often treated empirically with firstline therapies (eg, nonsteroidal anti-inflammatory drugs [NSAIDs], estrogen-progestin contraceptives). • If such therapy is unsuccessful, a definitive diagnosis may be preferred prior to treating with therapies that are difficult to tolerate and/or have potential adverse effects (eg, gonadotropin-releasing hormone [GnRH] agonists). • Historically, a diagnostic laparoscopy to evaluate for endometriosis was a standard part of the evaluation of infertility. • However, current practice varies. • Some experts advise that women with infertility and symptoms suggestive of endometriosis undergo laparoscopy prior to other treatments, while others do not perform laparoscopy and treat these patients in the same stepwise manner as other women (ovulation induction with intrauterine insemination followed by in vitro fertilization [IVF]). • In some cases, women are not able to undergo ovulation induction or IVF, and laparoscopy should be performed. CONTRAINDICATIONS • Relative contraindications to surgical management of endometriosis include: • ●Incomplete evaluation of the patient’s pain – Etiologies that do not require surgical evaluation or treatment should be excluded prior to surgery (primary dysmenorrhea, interstitial cystitis/bladder pain syndrome, irritable bowel syndrome). • ●Repeated surgeries for endometriosis without sustained relief. • ●Women who are approaching menopause SURGICAL PLANNING • Conservative surgery: initial surgical treatment for most wome • Definitive surgery consists of hysterectomy combined with bilateral salpingooophorectomy • Conservative surgery is the first-line option for most women planning surgical treatment of endometriosis. • We suggest hysterectomy rather than conservative surgery ONLY for women with persistent bothersome symptoms of endometriosis who do not plan future childbearing and who have both failed medical therapy and at least one conservative treatment procedure. • Definitive surgery is also reasonable for women who have additional indications for hysterectomy. • ●For women undergoing hysterectomy for treatment of endometriosis, we suggest bilateral salpingo-oophorectomy ONLY for those who value decreasing the risk of reoperation more than avoiding the risks of premature menopause. • In general, a preference for oophorectomy is more likely as a woman approaches menopause. • Oophorectomy is also reasonable for women with extensive disease involving the ovaries. • Laparoscopy is performed for the great majority of conservative procedures for treatment of endometriosis, regardless of the severity of disease. • The laparoscopic approach allows for greater visualization using lens magnification, faster patient recovery, and likely less pain and morbidity than larger abdominal incisions PREOPERATIVE EVALUATION AND PREPARATION • Suspicion of deep infiltrating lesions or extrapelvic disease • Deeply infiltrating endometriosis (DIE) refers to lesions that penetrate to a depth of 5 mm or more. • These are frequently multifocal and may involve the uterosacral ligaments, retrocervical space, bowel, ureteral and/or bladder • Involvement of these structures or severe pelvic adhesive disease may require more extensive surgery. • One study found that deep infiltrating endometriosis occurred without disease at other sites in only 6.5 percent of patients DIE • If is suspected based on symptomatology (eg, dysuria, dyschezia, hematochezia) and/or physical examination (eg, uterosacral ligament tenderness with dense nodules, non-mobile uterus), the preoperative evaluation should include appropriate additional testing. • This includes evaluation of the urinary or gastrointestinal tract. • Extensive pelvic adhesions are difficult to diagnose with imaging. • However, magnetic resonance imaging (MRI) or rectal sonography may suggest an obliterated pelvic cul-de-sac • Using transvaginal ultrasonography, one can look for the “sliding sign” when placing the probe in the posterior fornix to see if the anterior rectal wall glides smoothly over the retro-cervix [32]. • If there is no such sliding observed, then there is a high probability of obliteration of the culde-sac by endometriosis. Evaluation of the urinary and gastrointestinal tracts is discussed • superficial endometriotic implants, • ovarian endometriomas, • deep pelvic nodules • Lesions that may be confused with endometriosis on visual examination include endosalpingiosis, • mesothelial hyperplasia, • hemosiderin deposition, • hemangiomas, • adrenal rests, • inflammatory changes, • splenosis, and reactions to oil-based radiographic dyes Classification of extent of disease • American Society for Reproductive Medicine (ASRM) classification system • The classification system has a poor correlation with pregnancy outcome or pain • ecord the clinical score to provide a measure of comparison of the extent of disease between the initial and subsequent surgeries and to plan ahead for any subsequent operative procedure. • Ablation – Destruction of lesions by laser vaporization , electrosurgical fulguration, or ultrasonic cutting and coagulation. • ●Excision – Removal of lesions, typically with laparoscopic scissors • Adhesiolysis • Surgical management of DIE requires specialized skills to adequately remove extensive disease. The goal is to re-establish normal anatomy. It is vital to administer postoperative suppressive therapy to try to prevent recurrence • Rate of recurrence was higher for women with more severe disease Postoperative medical therapy • • • • • Conservative surgical treatment generally does not obliterate the disease burden and provide subsequent, life-long pain relief. Symptom recurrence requiring reoperation is common and worsens with time: 21.5 percent at two years and 40 to 50 percent after five years We recommend postoperative medical suppressive therapy for most women treated surgically for endometriosis. Several randomized trials have reported postoperative hormonal therapy increased the duration of pain relief and delayed recurrence of disease Two randomized trials have found that postoperative insertion of the levonorgestrel-releasing intrauterine device (LNG IUD) results in decreased dysmenorrhea compared with expectant management • The options for postoperative medical therapy are the same as for medical therapy alone. • Typically, first-line therapy is estrogen-progestin contraceptives or oral progestins alone, both of which are easy to tolerate and cost-effective. • Another option is a LNG IUD. • If these options are not effective, patients may be treated with other hormonal agents (eg, gonadotropin-releasing hormone [GnRH] agonists), although these are associated with more adverse effects. • Treatment may be initiated immediately after surgery