URGENT COMMUNICATION - RED CELL HbS- UNITS
advertisement
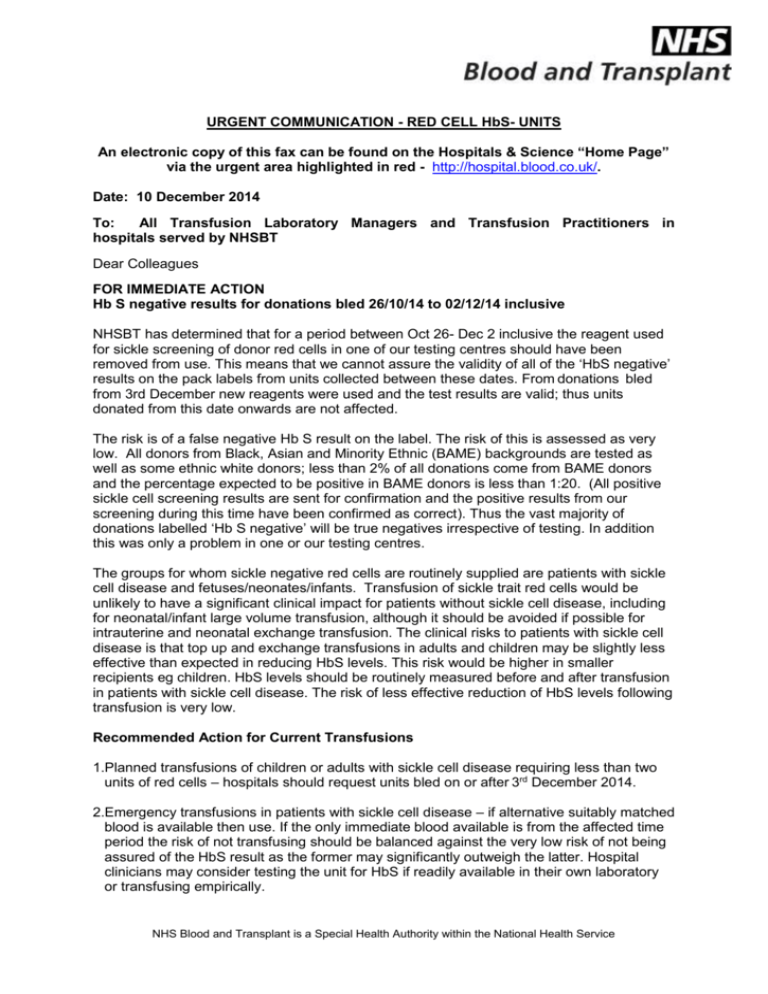
URGENT COMMUNICATION - RED CELL HbS- UNITS An electronic copy of this fax can be found on the Hospitals & Science “Home Page” via the urgent area highlighted in red - http://hospital.blood.co.uk/. Date: 10 December 2014 To: All Transfusion Laboratory Managers and Transfusion Practitioners in hospitals served by NHSBT Dear Colleagues FOR IMMEDIATE ACTION Hb S negative results for donations bled 26/10/14 to 02/12/14 inclusive NHSBT has determined that for a period between Oct 26- Dec 2 inclusive the reagent used for sickle screening of donor red cells in one of our testing centres should have been removed from use. This means that we cannot assure the validity of all of the ‘HbS negative’ results on the pack labels from units collected between these dates. From donations bled from 3rd December new reagents were used and the test results are valid; thus units donated from this date onwards are not affected. The risk is of a false negative Hb S result on the label. The risk of this is assessed as very low. All donors from Black, Asian and Minority Ethnic (BAME) backgrounds are tested as well as some ethnic white donors; less than 2% of all donations come from BAME donors and the percentage expected to be positive in BAME donors is less than 1:20. (All positive sickle cell screening results are sent for confirmation and the positive results from our screening during this time have been confirmed as correct). Thus the vast majority of donations labelled ‘Hb S negative’ will be true negatives irrespective of testing. In addition this was only a problem in one or our testing centres. The groups for whom sickle negative red cells are routinely supplied are patients with sickle cell disease and fetuses/neonates/infants. Transfusion of sickle trait red cells would be unlikely to have a significant clinical impact for patients without sickle cell disease, including for neonatal/infant large volume transfusion, although it should be avoided if possible for intrauterine and neonatal exchange transfusion. The clinical risks to patients with sickle cell disease is that top up and exchange transfusions in adults and children may be slightly less effective than expected in reducing HbS levels. This risk would be higher in smaller recipients eg children. HbS levels should be routinely measured before and after transfusion in patients with sickle cell disease. The risk of less effective reduction of HbS levels following transfusion is very low. Recommended Action for Current Transfusions 1.Planned transfusions of children or adults with sickle cell disease requiring less than two units of red cells – hospitals should request units bled on or after 3rd December 2014. 2.Emergency transfusions in patients with sickle cell disease – if alternative suitably matched blood is available then use. If the only immediate blood available is from the affected time period the risk of not transfusing should be balanced against the very low risk of not being assured of the HbS result as the former may significantly outweigh the latter. Hospital clinicians may consider testing the unit for HbS if readily available in their own laboratory or transfusing empirically. NHS Blood and Transplant is a Special Health Authority within the National Health Service 3.Fetal/neonatal/infant large volume transfusions, including neonatal exchange transfusions, are recommended to be with units within 5 days of donation. Units of this age will now have been bled on or after 3rd December 2014 so will be unaffected. For urgent/emergency large volume transfusion of neonates and infants, if the only available units are from the affected time period, the risk of not transfusing should be balanced against the very low risk of not being assured of the HbS result as for emergency transfusion of patients with sickle cell disease above. 4. All other clinical situations – no action required NHSBT will be confirming whether any units for intrauterine or neonatal exchange transfusion could have been affected and will inform the relevant hospitals if so. Any clinician requiring further advice should contact NHSBT consultants who are available 24 hours via Hospital Services. If you have any queries please contact an NHSBT Consultant, Customer Service Manager or Hospital Services Manager. Alternatively please contact the Customer Service Response Desk on 0208 201 3107 between 08:30 to 16:30, Monday to Friday. Please notify your Consultant with responsibility for the transfusion laboratory of this communication. Yours sincerely Teresa Allen Assistant Director – Customer Services email: teresa.allen@nhsbt.nhs.uk Dr Kate Pendry Clinical Director – Patients email: kate.pendry@nhsbt.nhs.uk NHS Blood and Transplant is a Special Health Authority within the National Health Service