Obesity - Big Birthas
advertisement

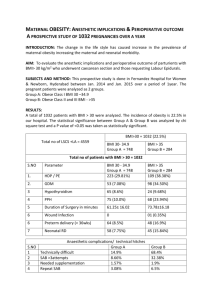
MATERNITY SERVICES GUIDELINE OBESITY Version Authors Date of first issue Version Date of version issue Ratified by Date ratified Review date Version information Obesity Guideline Version 3 February 2012 Louvain Shaw Midwife, Helen Joyce Midwife. October 2009 3 February 2012 Obs & Gynae Clinical Governance Forum 10th February 2012 February 2015 Updated in line with clinical practice Page 1 of 12 Contents Section Page 1. Guideline Flow chart 3 2. Introduction & Definitions 3 3. Management 4 4. Antenatal 5 5. Intrapartum 5 6. Anaesthetic risks associated with obesity 6 7. Postnatal 7 8. Monitoring Compliance with the guideline 8 9. Links with 8 10. References 8 Appendix 1 Equipment available 9 Appendix 2 Guideline for use of equipment for overweight patients 10 Appendix 3 Monitoring Compliancy 11 Obesity Guideline Version 3 February 2012 Page 2 of 12 1. Guideline Flowchart (refer to full guideline for further information) Booking appointment: All pregnant women must have an accurate measurement of height and weight taken (preferably, before 12 weeks) and BMI calculated. Women with a BMI ≥ 30 and above: Should be given the patient information leaflet on obesity (raised BMI and lifestyle changes) Vitamin D 10mcg/day supplement ( prescribed by GP) Glucose Tolerance Test, arranged through Antenatal clinic at their 20 wk scan appointment. All women with a BMI ≥ 30 consider presentation USS on admission for labouring women and before IOL. They also need to be re- weighed again at 36 weeks. All women with a BMI≥30 should be recommended to have active management of the third stage of labour. Women with a BMI ≥ 35 Women with a BMI ≥ 35 must be booked consultant care and should have antenatal consultation with an obstetric consultant to discuss possible intrapartum complications, the discussion must be documented in the health record. These women are not suitable for midwifery led care and should be advised to deliver in hospital Women with BMI ≥40 Women with BMI ≥40 at booking should be referred to the Lead Obstetric Anaesthetist irrespective of the planned mode of delivery. This is done by the consultant unit team at 20 wks scan appointment. The duty anaesthetist should also be aware of all women with a BMI ≥40 admitted to the maternity unit. The duty anaesthetist should be notified immediately of all women with a BMI ≥ 40 who are admitted in labour. All women in labour with a BMI ≥ 40 and above must have a grey cannula (16 gauge) sited together with a FBC and group and save sent to lab. In women with a BMI ≥ 40, a fetal scalp electrode should be applied to record the fetal heart rate if unable to obtain a good external CTG trace. BMI of 40 and above, regardless of their mode of delivery require Fragmin for 7 days. Patients at particularly high risk may need a 6- 8 week course of Fragmin. Obesity Guideline Version 3 February 2012 Page 3 of 12 2. Introduction & definition Obesity is defined by the World Health Organisation (WHO) (1998) and the National Institutes of Health (1998) as a Body Mass Index (BMI) of ≥30. Body Mass Index (BMI) is an index of weight-for-height. It is calculated by the weight in kilograms divided by the square of the height in metres (kg/m2) The prevalence of obesity in pregnancy is on the rise and it is becoming increasingly more urgent to have guidelines and strategies in place to be able to give care to this group of women. The role of this guideline is to outline the appropriate management strategies to minimise the clinical risk to this group of women. In the last CEMACH (2007) report obesity alone was identified as a risk factor for maternal death, following the finding that 35% of all mothers who died were obese. It was recommended that women with a BMI ≥ 35 at first contact are unsuited for midwife led care and that they should deliver in a consultant unit with appropriate emergency facilities. In order to make the pregnancy safer for obese women it should be acknowledged that they represent a “high risk pregnancy” 1. Management Pregnancy risks associated with obesity: Obesity is a recognised risk factor for a range of antenatal, intrapartum and postnatal complications with maternal BMI ≥ 30 being a recognised risk factor for: Hypertension and pre-eclampsia Gestational diabetes Difficulty with physical examinations Thromboembolic disease Fetal macrosomia Difficulty in monitoring fetal heart rate Prolonged labour Increased rate of LSCS Difficult operative procedures Risks associated with anaesthesia Wound infections Shoulder dystocia Maternal Death Failure to progress in labour 4. Antenatal: 1. All pregnant women must have an accurate measurement of height and weight taken at their booking visit (preferably, before 12 weeks) and BMI Obesity Guideline Version 3 February 2012 Page 4 of 12 calculated. They also need to be re- weighed again at 36 weeks. This should be carried out by a healthcare professional using appropriate equipment. These measurements must be clearly documented in the women’s hand held notes and electronic patient information system. Self reported weights and height should not be used as substitutes. 2. Blood pressure readings must be recorded using an appropriately sized cuff. 3. Women with a BMI ≥ 30 and above should be given the patient information leaflet on ‘Raised BMI and Lifestyle Changes’ Women should be given the opportunity to discuss this information. 4. Women with BMI ≥30 at booking should have a Glucose Tolerance Test (GTT), arranged through Antenatal clinic at their 20 wk scan appointment. At the GTT appointment consideration will be given regarding midwifery led care or consultant led care. Women with a BMI ≥30 at booking are not currently booked for Consultant led care due to resources. 5. Women with a BMI ≥ 35 must be referred to a consultant obstetrician for Consultant led care. These women are not suitable for midwifery led care and should be advised to deliver in hospital with appropriate neonatal services. 6. Risks of pregnancy complications and morbidity should be discussed and recorded in the woman’s notes. Women with a BMI ≥ 35 must be booked consultant care and should have antenatal consultation with an obstetric consultant to discuss possible intrapartum complications, the discussion must be documented in the health record. 7. Women with BMI ≥40 at booking should be referred to the Lead Obstetric Anaesthetist irrespective of the planned mode of delivery, so that potential difficulties with venous access, regional or general anaesthesia can be identified. This is done by consultant unit team at 20 wks scan appointment or at subsequent appointment when a letter is sent to request the mother for an anaesthetic review. An individualised management plan should be written in the woman’s maternity notes and any specialised equipment identified. Dietary advice should be given and referral to dietician offered. 8. Venous thromboembolism Risk Assessment form to be completed at booking and on each admission to hospital. 5. Intrapartum: 1. All women with a BMI ≥ 30 consider presentation USS on admission for labouring women and before IOL. 2. All women in labour with a BMI ≥ 40 and above must have a grey cannula (16 gauge) sited together with a FBC and Group and Save sent to lab. 3. Administer oral Ranitidine 150 mg / 6 hourly, in labour. Consumption of food should be avoided, clear fluids only. Obesity Guideline Version 3 February 2012 Page 5 of 12 4. In women with a BMI ≥ 40, a fetal scalp electrode should be applied to record the fetal heart rate if unable to obtain a good external CTG trace. 5. All women with a BMI≥30 should be recommended to have active management of the third stage of labour. 6. All staff must follow the Trust Manual Handling policy, consider transferring and positioning. 7. A manual handling risk assessment on admission must be completed and reassess throughout labour and recorded 2 hourly in the maternity in patient notes. 8. Suitable equipment such as large BP cuffs are available in all care settings including the community. Large chairs, wheelchairs are available throughout the Trust for further information refer to Bariatric Guidelines in the Manual Handling Resource Pack or contact one of the Manual Handling Link Midwives. Also see (Appendix 1) Maximum Load Weight of Equipment and (Appendix 2) Guideline for use of equipment for overweight patients. This equipment will be assessed annually by the Manual Handling Link Midwives. 6. Anaesthetic risks associated with obesity: Practical: Transferring and Positioning Practical procedures such as IV access, regional anaesthesia, intubation, mask ventilation Special equipment needed such as stronger beds and tables Monitoring Associated conditions: Diabetes Sleep apnoea Hypertension Gastro-oesophageal Reflux The duty anaesthetist should also be aware of all women with a BMI ≥40 admitted to the maternity unit, as they may have additional risks and potential difficulties. The duty anaesthetist should be notified immediately of all women with a BMI ≥ 40 who are admitted in labour. A consultant anaesthetist (Specialty Trainee year 6 and above) should be informed and available for the care of women with a BMI ≥40 during labour and delivery, including attending any operative vaginal or abdominal delivery advising what analgesia or anaesthetic should be used. If a delivery plan is available the duty anaesthetist should follow it. If it is not they should assess the woman paying particular attention to: Airway assessment Any history or suspicion of obstructive sleep apnoea Any coexisting disease Obesity Guideline Version 3 February 2012 Page 6 of 12 A multidisciplinary delivery plan should be formed considering the obstetric risk in light of high BMI and any additional anaesthetic concerns. Extra care should be taken to avoid lying a women flat as aorta compression is exacerbated. This must never be under estimated. The high risks of a general anaesthetic in this group coupled with the likelihood of difficulty with regional anaesthesia mean that siting an epidural early in labour, when there is no urgency and calling of a 2nd anaesthetist if necessary, seems the prudent and safest choice. This should be explained to the woman, who should have had this discussed antenatally. Once an epidural is sited the anaesthetist must ensure it is working well and continues to work well in case it needs to be topped for a theatre procedure later. If theatre is needed a general anaesthetic should be avoided if at all possible. A senior anaesthetist should be involved. Extra monitoring may be required (e.g. arterial line as non-invasive cuffs tend to misread) and HDU care may well be needed post operatively. Good analgesia is essential but opiates will exacerbate sleep apnoea and reduce mobility postoperatively. Other points for consideration Sitting up for pre-oxygenation and intubation Ensuring adequate suxamethonium is given Inducing and siting regional anaesthesia in theatre so that she doesn’t have to be moved on the table Sitting her up before extubation Getting extra people into theatre to help with positioning 7. Postnatal: 1. Early mobilisation 2. Particular risks are concealed PPH, Obstructive Sleep Apnoea difficulties measuring BP, DVT, slow mobilisation and wound infection 3. Consider use of HDU facilities post delivery due to risks of respiratory and cardiovascular complications. 4. Refer to physiotherapists, as indicated. 5. Postnatal VTE risk assessment completed and appropriate Fragmin should be prescribed doses appropriate for maternal weight. Refer to thrombo prophylaxis guideline. 6. BMI of 40 and above, regardless of their mode of delivery require Fragmin for 7 days. Women at particularly high risk may need a 6- 8 week course of Fragmin. 7. Dietary advice should be given and referral to dietician offered. 8. It is also recommend for future pregnancies that women receive prepregnancy counselling and folic acid supplementation. Obesity Guideline Version 3 February 2012 Page 7 of 12 8. Monitoring Compliance: See Appendix 1 This will be monitored as part of the Annual Audit Programme. The lead person will be responsible for completion of the monitoring process by means of an audit, development of an action plan, any subsequent actions and their dissemination. Process for monitoring e.g. audit Audit Lead Responsible Naomi Inman Frequency of monitoring Responsible Lead / Committee for review of results and development of action plan Annually – according to Annual Audit plan Obs & Gynae Clinical Governance Forum Labour Ward Forum & Obstetric Risk Group Responsible Lead / Committee for monitoring of action plan Obs & Gynae Clinical Governance Forum 9. Links with: Bariatric Guidelines in the Manual Handling Resource Pack Pregnancy and Obesity Patient Information Leaflet Home Birth guideline Thrombo-prophylaxis guideline Antenatal Day Services guideline 10. References: M Dresner, J Broklesby, J Bamber: Audit of the influence of BMI on the performance of epidural analgesia in labour and the subsequent mode of delivery. BJOG. Vol113. Issue10. ROCOG (2010) Joint Guideline: Management of Women with Obesity in Pregnancy London Centre for Maternal and Child Enquiries (CMACE). Maternal obesity in the UK: Findings from a national project. London: CMACE, 2010. U Krishnamoorthy, CMH Schram, Sr Hill: Maternal obesity in pregnancy: is it time for meaningful research to inform preventive and management strategies? BJOG. Vol 113 Issue 10. Lewis, G (Ed) 2007: The Confidential Enquiry into Maternal and Child Health (CEMACH). ‘Saving Mothers’ Lives: Reviewing Maternal Deaths to Make Motherhood Safer-2003-2005’. The Seventh Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. London: CEMACH. National Institute for Health and Clinical Excellence (NICE) 2008: Clinical guideline 62: Antenatal care: Routine care for the healthy pregnant woman. London Richens Y,(2008) Tackling maternal obesity: Suggestions for midwives. British Journal of Midwifery: vol16: 1p 14-18. CKH Yu, TG Teoh, S Robinson: Obesity in pregnancy. BJOG Vol113, issue 10. Obesity Guideline Version 3 February 2012 Page 8 of 12 Appendix 1 Equipment available Ward Area Ward G2/G3 Labour Ward Equipment available Kings Fund Bed Huntleigh Profile Bed-Centura Huntleigh Profile Bed 480 Wide Bedside Chair Hill Rom Affinity Delivery Bed Theatre table- Room 15 Maximum Weight 180 kgs 250 kgs 267 kgs 225 kgs 227 kgs 225 kgs table not to be moved > 135 kgs 225 kgs table not to be moved > 135 kgs 225 kgs 160 kgs 180 kgs 225 kgs 180 kgs 180 kgs 225 kgs 180 kgs 180 kgs 225 kgs Theatre table- Operating Theatre Antenatal Clinic Antenatal Day Unit Triage Unit All Areas Wide Bedside Chair Parker Knoll Recliner Chair Theatre Trolley Wide Waiting Room Chairs Examination Couch Kings Fund Bed Wide Waiting Room Chair Examination Couch Kings Fund Bed Wide Waiting Room Chair Wheelchair – Bradfern X-ray Wheelchair Heavy duty wheelchairs available from main porters 134 kgs Maximum Load Weight of Equipment See Manual Handling Bariatric Flowchart for Trust equipment availability Further information available from the Manual Handling Resource Folder Obesity Guideline Version 3 February 2012 Page 9 of 12 Appendix 2 GUIDELINES FOR USE OF EQUIPMENT FOR OVERWEIGHT PATIENTS <114kg (18st) 114kg – 180kg (18-28st) >180kg (28st) Standard equipment may be used Profiling bed or prima pink foam mattress (on some ward beds) (kings fund bed may be used) Heavy-weight Profiling bed (up to 267kg) Heavy duty chair (on G2) Heavy duty chair (on G2) Arrange with porter for a heavy- duty wheelchair if required. Wheelchair may be available from OT Arrange with porter for a heavy-duty wheelchair if required Wheelchair may be available from OT Equipment co-ordinator available on Bleep 300 for access to Trust heavy duty equipment Remember weight now, not booking weight. 36/40 weight may need checking on admission if close to the upper weight limit. Scales on G3 weigh up to 190kg, may use 2 scales if required. Scales on G1 weigh up to 200kg Liko Gantry scales weigh up to 317kg – phone works (ext 5566) will need requisition. Refer to guidelines for very heavy patients/bariatric patients. Refer to pool guidelines re: exclusion criteria. Obesity Guideline Version 3 February 2012 Page 10 of 12 Appendix 3 Monitoring Compliance In order to monitor compliance with this guideline, this guideline will be monitored as follows: Minimum requirements a) The calculation and recording of the body mass index (BMI) for all women b) The calculation of the body mass index(BMI) and recording of the BMI in the electronic patient information system c) That all women with a BMI≥30 should be advised to book for maternity team based care d) That all women with ≥35 should be advised to deliver in an obstetric led unit e) An agreed BMI at which women must be offered an antenatal assessment with an obstetric anaesthetist Guideline Statement Evidence All pregnant women must have an accurate measurement of height and weight taken at their booking visit and BMI calculated. They also need to be re- weighed again at 36 weeks. These measurements must be clearly documented in the patient notes. Notes audit These measurements must be clearly documented in the women’s hand held notes and electronic patient information system. Notes audit At the GTT appointment consideration will be given regarding midwifery led care or consultant led care. Women with a BMI ≥30 at booking are not currently booked for Consultant led care due to resources. Notes audit. Women with a BMI ≥ 35 must be referred to a consultant obstetrician for Consultant led care. These women are not suitable for midwifery led care and should be advised to deliver in hospital with appropriate neonatal services. Notes audit Women with BMI ≥40 at booking should be referred to the Lead Obstetric Anaesthetist irrespective of the planned mode of delivery. Notes audit. Obesity Guideline Version 3 February 2012 Page 11 of 12 CNST standards 3.10 3.10 3.10 3.10 3.10 f) That an obstetric anaesthetic management plan for labour and delivery should be discussed with the woman and documented in the health record. g) That all women with a BMI ≥30should have an antenatal consultation with an obstetric consultant to discuss possible intrapartum complications, the discussion must be documented in the health record h) The requirement to assess the availability of suitable equipment in all care settings for women with a high BMI An individualised management plan should be written in the woman’s maternity notes and any specialised equipment identified. Notes audit. 3.10 At the GTT appointment consideration will be given regarding midwifery led care or consultant led care. Women with a BMI ≥30 at booking are not currently booked for Consultant led care due to resources. Notes audit. 3.10 A clear plan of care should be written in the patient maternity notes and any specialised equipment identified. Suitable equipment e.g. large chairs, wheelchairs are available throughout the Trust for further information refers to Bariatric Guidelines in the Manual Handling Resource Pack or contact one of the Manual Handling link midwives or Trust equipment co-ordinator. Also see (Appendix 1) Maximum Load Weight of Equipment and (Appendix 2) Guideline for use of equipment for overweight patients. This equipment will be assessed annually by the Manual Handling Link Midwives. Obesity Guideline Version 3 February 2012 Page 12 of 12 Notes audit. 3.10