Pulmonary Infections
advertisement

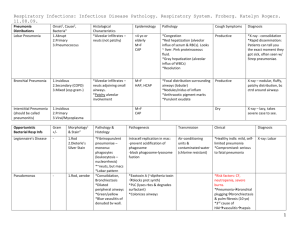
Pulmonary Infections Disease Respiratory Tract Infections Overview - More frequent than infection in other organ - Account for the largest number of work days lost in the general population - Majority URTIs caused by viruses - Lung infections, such as pneumonia, lung abscesses and TB rank among the major immediate causes of death Pneumonia - Any acute inflammation of the lung parenchyma Etiology: - Bacteria - Viruses - Chemical irritants Pathogenesis Respiratory tract - Inhalation of aerosols – usual mode - Aspiration of secretions containing pathogenic organisms that have colonized the oropharynx - Hematogenous spreadfrom extrapulmonary Nosocomial infections – hospital acquired - Acquired resistance to antibiotics - Invasive procedures and contamination of instruments, e.g. intubation - Ventilation Impairment of defense mechanisms - Loss or suppression of the cough reflex aspiration of gastric contents – coma , anesthesia - Damage to the mucociliary apparatus o Smoking, viral infections, genetic (immotile cilia syndrome), inhalation of hot or corrosive gases - Interference with alveolar macrophages o Smoking, alcohol, anoxia, O2 toxicity - Pulmonary congestion and edema o CHF - Accumulation of secretions o Bronchial obstruction, cystic fibrosis - Lowered resistance of the host o Immunodeficiency o Unusually virulent infections o Chronic diseases: Diabetes, malnourishment, alcoholism o Leukopenia o Immunosuppression Types - Lobar Pneumonia: Affects an entire lobe - Bronchopneumonia: Scattered foci - Interstitial: Alveolar interstitium Course Most patients recover with antibiotic therapy < 10% succumb due to: - A complication - Meningitis, empyema, endocarditis, pericarditis - Predisposing condition - Debility - Alcoholism ©2010 Mark Tuttle Clinical The Pneumonia Syndromes Community-Acquired Acute Pneumonia Chronic Pneumonia - Nocardia - Actinomyces - Granulomatous: Mycobacterium tuberculosis and atypical mycobacteria, Histoplasma capsulatum, Coccidioides immitis, Blastomyces dermatitidis Necrotizing Pneumonia and Lung Community-Acquired Atypical Pneumonia Abscess - Mycoplasma pneumoniae - Anerobic bacteria (extremely - Chlamydia spp. (C. pneumoniae, C. psittaci, C. common), with or without mixed trachomatis) aerobic infection - Coxiella burnetti (Q fever) - Viruses: respiratory syncytial virus, parainfluenza - Staphylococcus aureus, Klebsiella virus (children); influenza A and B (adults); pneumoniae, Streptococcus pyogenes, adenovirus (military recruits); SARS (Severe acute and type 3 pneumococcus (uncommon) respiratory syndrome) virus Pneumonia in the Immunocompromised Nosocomial Pneumonia - Cytomegalovarus - Gram-negative rods belonging to - Pneumocystis carinii Enterobacteriaceae (Klebsiella spp., Serratia - Mycobaterium avium-intracullulare marcescens, Escherichia coli) and Pseudomonas - Invasive aspergillosis spp. - Staphylococcus aureas (usually penicillin-resistant) - Invasive candidiasis - “Usual” bacterial, viral, and fungal Aspiration Pneumonia organisms (listed above) - Anaerobic oral flora (Bacteriodes, Prevotella, - Streptococcus pneumoniae Haemophilus influenzae Moraxella catarrhalis Staphylococcus aureus Legionella pneumophilia Enterobacteriaceae (Klebsiella pneumoniae) and Pseudomonas spp. Fusobacterium, Peptostrepococcus), admixed with aerobic bacteria (Streptococcus pneumoniae, Staphylococcus aureus, Haemophilas influenzae, and Pseudomonas aeroginosa) Symptoms - Malaise, fever, productive cough - Fibrinosuppurative pleuritis – friction rub - Dyspnea, hypoxia and cyanosis - X-ray o Lobar pneumonia – radiopaque lobe o Bronchopneumonia- focal opacities Complications - Abscesses: Localized suppurative necrosis o Right sided abscesses most often seen in aspiration pneumoniae o Type 3 pneumococci or Klebsiella infections - Pleural Involvement: Empyema Labs - Gram stain, culture of sputum - Rapid urine antigen test Legionella - Current Jelly Sputum Klebsiella - Chest x-ray, CBC - Blood cultures - Blood gases if significant hypoxemia - Bacterial Dissemination o Heart valves, pericardium, brain, kidneys, spleen or joints - Organization o Converting part of the lung into solid o Fibrosis, scarring Disease Lobar Pneumonia Pathogenesis - Affects a large area or the entire lobe of a lung - Degree of involvement depends upon: o Virulence of the organism Heavy contamination by virulent organisms may cause lobar pneumonia in healthy individuals o Vulnerability of the host Organisms of low virulence may affect predisposed individuals - Extensive exudation in the lung allows spread through the pores of Kohn - No alveolar injury - Less common today due to antibiotics - Stop progression of lung consolidation Etiology - Streptococcus pneumoniae in 90-95 % - Generally types 1, 2, 3 and 7 - Type 3 cause a virulent form of pneumonia - Other organisms: o Klebsiella pneumoniae, staphylococci, streptococci, H. influenzae; gram negative organisms Pseudomonas and Proteus Clinical 1. Congestion First 4 – 12 hrs - Heavy, wet, red - Vascular engorgement, intra-alveolar fluid - Few neutrophils, numerous bacteria 2. Red hepatization Next 48 hrs - Firm, red, airless with a liver like consistency - Massive confluent exudate with red cells, neutrophils and fibrin 3. Gray hepatization 3 to 8 days - Grayish brown, dry - Progressive disintegration of red cells - Persistence of fibrinopurulent exudate 4. Resolution 7 to 11 days - Progressive enzymatic digestion o Granular semi-fluid debris ingested by macrophages or coughed up Labs/Histology Red Hepatization Gray Hepatization Microscopic Bronchopneumonia Aspiration pneumonia Common organisms: - Staphylococcus, streptococcus, Pseudomonas, H. influenzae, pneumococci, Klebsiella and other gram negative coliform bacteria - Gross - Lesions 3-4 cm in diameter, slightly elevated, dry, granular, gray red to yellow, poorly demarcated, patchy - Usually an extension of bronchitis of bronchiolitis - Generally multilobar; frequently bilateral and basal Microscopic - Suppurative, neutrophil rich exudate that fills the bronchi, bronchioles and extends directly into adjacent alveolar spaces - Necrosis may be present in more virulent organisms - Exudate may resolve or organize - Inhalation of foreign material, usually food, drink, vomit or Types secretions - Partially chemical pneumonitis from irritating gastric acid and partially bacterial - Aspiration may occur with unconsciousness, repeated from oral flora vomiting, and abnormal gag & swallowing reflexes - Typically >1 organism isolated with aerobes > anaerobes Disease Atypical Pneumonia (Community Acquired) Pathogenesis - Most common– Mycoplasma pneumonia - Viruses: o Immunocompetent individuals -influenza viruses type A and B, respiratory syncytial virus, adenovirus, SARS virus, etc. o Immunocompromised – CMV, herpes - Chlamydia – Psittacosis (Ornithosis): transmitted by inhalation of dried excreta of infected birds - Rickettsia – Q fever due to Coxiella burnetti: Transmitted by : o Inhalation of dust particles w/ the organism o Drinking unpasteurized milk from infected o Working with infected cattle or sheep o Unknown Signs & Symptoms - Acute Febrile Respiratory disease - Patchy inflammation of alveolar septa and interstitium - No exudate Serology: cold agglutinis present (mycoplasma) Complication: cold autoimmune hemolytic anem Fungal - Some pathogenic, while others are opportunistic infections of the - Spectrum of colonization and disease; host lung response influenced by immune status - Characteristic geographic (endemic) regions Severe Acute Respiratory Distress Syndrome (SARS) - First: 2002 in Guandong Province of China - 2-10 days incubation - Corona virus - Often necrotizing pneumonia fulminant course frequent death Clinical Labs/Histology - Pneumonia in the immunocompromised CMV “Owl Eyes” - Mostly due to opportunistic infections - Often more than one agent is involved - Diffuse Infiltrates: o Cytomegalovirus o Pneumocystis carinii (esp. in AIDS) o Drug reaction - Focal Infiltrates: o Gram negative rods o Staphylococcus aureus Pneumocystis carnii (H&E stain) o Aspergillus o Candida Gross - Patchy or may involve entire lobes, bilateral or unilateral - Red-blue, congested, subcrepitant - Pleura smooth, pleural involvement infrequent Microscopic Depends severity - Interstitial inflammation - Predominant pattern - Alveolar septae widened by edema and chronic inflammatory cells –lymphocytes, macrophages and occasional plasma cells. Neutrophils may be present in the acute phase - Alveoli free of exudate - Diffuse alveolar damage (DAD) - Changes similar to ARDS Pneumocystis Carnii (GMS stain) - Coccidiodomycosis - Aspergillus Aspergilloma - Cryptococcus neoformans Immunocompromised hosts - Mucormycosis (association with diabetes) - Dry cough Diagnosis - Malaise - PCR - Myalgias - Antibodies to virus - Fever Morphology - Diffuse alveolar damage - Multinucleated giant cells - Corona viruses can be seen within pneumocytes by EM Disease Lung Abscess Local suppurative process in the lung characterized by necrosis of lung tissue Pathogenesis Source: Bacteria - Anerobic organisms like oral cavity flora ~ 60% - Aerobic and anaerobic streptococci, S. aureus; gram negative organisms Aspiration of infective material - Most common cause - Associated with conditions in which cough reflex is depressed, such as: o Debilitation o Alcoholism, acute o Coma o Anesthesia Antecedent primary bacterial infection - Postpneumonia – S. aureus, K. pneumoniae and type 3 pneumococcus - Fungal infections - Bronchiectasis Septic embolism - Systemic veins or from right side of heart Neoplasia –obstruction ~ 10-15% of cases Miscellaneous - Direct penetration of the lung - Spread from neighboring organ - Hematogenous seeding Idiopathic –primary cryptogenic lung abscess Clinical Course - Fever, productive cough- copious amounts of sputum, generally foul smelling, purulent or sanguineous - Clubbing of fingers and toes - Diagnosis suspected based on clinical signs and symptoms - Confirmed by X-ray and bronchoscopy - Important to rule out cancer present in 10-15% Resolution: w/antibiotics no sequelae Complications - Extension of infection into the pleural cavity - Septic emboli brain abscess or meningitis Gross: - Size – variable - Aspiration more common in right lung, generally single (more vertical right bronchus) - Pneumonia or bronchiectasis multiple, basal and diffusely scattered - Septic emboli, hematogenous spread multiple and affect any region - Cavity, filled with suppurative debris - When communicating with an air space, partly drained and may show air-fluid level - Saprophytic infections may be superimposed resulting in gangrene of the lung - In chronic infections, fibroblastic proliferation produces a fibrotic wall Labs/Histology Microscopic - Cardinal histologic change – Suppurative destruction of the parenchyma within the central area of cavitation Disease Pulmonary Tuberculosis Pathogenesis - Relatively uncommon cause of death in the United States - On the rise in the last decade – AIDS - Emergence of highly drug-resistant strains - Causative organism – Mycobacterium tuberculosis - After HIV, TB is the leading infectious cause of death in the world. Clinical - Three forms: o Primary pulmonary TB o Secondary (reactivation) pulmonary TB o Progressive pulmonary TB Cavitary fibrocaseous TB Miliary TB - Tuberculous bronchopneumonia Labs/Histology Secondary TB Gross - ~ located in apex of one or both lungs - Usually < 3.0 cm Microscopic: - Coalescent caseating granulomas - Outcome: Heal spontaneously or with therapy fibrocalcific nodule Primary TB - Infection of an individual Progressive pulmonary TB (Cavitary Fibrocaseous) lacking a previous contact - Erosion of a lesion into a bronchiole cavity - Primary pulmonary focus Ghon - Apical cavitary fibrocaseous TB focus - Advanced fibrocaseous TB - Subpleural: just above / below the Miliary TB interlobar fissure between the upper - Infection gains access to the bloodstream and and lower lobes lymphatics and disseminates - Primary focus + regional lymph node - Disseminated pulmonary spread: TB gains entry into the pulmonary arteries involvement Ghon complex Disseminated systemic spread: TB gains entry - Asymptomatic fibrosis and into the pulmonary veins or lymphovascular calcification Miliary TB may be seen in either Primary or - Progression to miliary TB Secondary tuberculosis Tuberculous Bronchopneumonia Secondary TB - Previously sensitized - In highly susceptible, highly sensitized individuals - Reactivation – 5-10% o Apex or posterior segments of the - Rapid spread of infection – “galloping consumption”; bronchopneumonia or lobar upper lobe, of one or both lungs pneumonia - Reinfection - less common - Granulomas may not be seen; Acid fast bacilli present Miliary TB Ghon Complex (primary TB) Granuloma Acid-fast bacili