Anemia - Nutrition411
advertisement

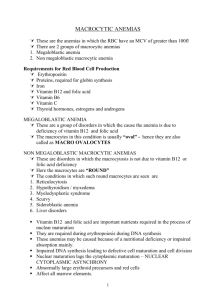
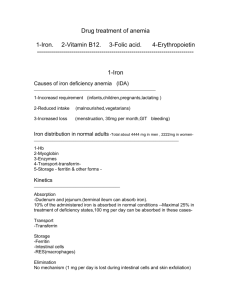
Anemia Folic acid deficiency anemia Folic acid deficiency anemia is generally caused by poor diet, intestinal malabsorption, renal dialysis, alcoholism, or pregnancy. It is a hyperchromic, macrocytic, megaloblastic anemia with signs and symptoms of: Weight loss Anorexia Malnutrition Smooth and sore red tongue Diarrhea Easy fatigue Lethargy Poor wound healing Coldness of extremities To differentiate between folic acid deficiency and B12 deficiency, the Schilling test, serum level of B12, and red blood cell folate tests are necessary. Note that serum levels of folic acid sometimes are misleading. Folate requirements increase with burns, hepatitis, infection, inflammatory diseases, cancer, pregnancy, lactation, surgery, and hemolytic anemias. Serum folate less than 3 nanograms (ng)/milliliter (mL), low red blood cell (RBC) folate, moderately elevated serum homocysteine levels, low RBC, decreased hemoglobin and hematocrit, increased macrocytic cells in a CBC, normal serum B12 levels, increased serum iron levels, increased mean cell volume (MCV), formiminoglutamic acid (FIGLU), normal methylmalonic acid, leukopenia, and the Schilling test to rule out vitamin B12 deficiency are useful for diagnosis of folic acid deficiency anemia. Folate deficiency is treated with 1 milligram (mg) of folic acid/day. High levels of folic acid can mask vitamin B12 deficiency. Vitamin C improves absorption of folic acid from food. Iron deficiency anemia Iron deficiency anemia is most commonly caused by inadequate intake, impaired erythropoiesis or absorption of iron, blood loss, or closely repeated pregnancies. In gastritis, treatment of H pylori can lead to recovery from iron deficiency anemia. Serum ferritin is useful in differentiating between iron deficiency anemia and anemia of chronic disease. Iron deficiency anemia can lead to: Impaired cognition Blue sclerae Koilonychia Decreased exercise tolerance Functional changes of the bowel Weakness Fatigue Vertigo Headache Irritability Heartburn Dysphagia Flatulence Abdominal pain Anorexia Glossitis Stomatitis Pallor Edema of the ankles Tingling of the extremities Heart palpitations The hemoglobin content of reticulocytes is a good indicator of iron deficiency in children. Changes in vitamins A, B12, C, and E, folic acid, and riboflavin status are linked to the development and control of iron deficiency anemia. If vitamin A deficiency is endemic, a single dose is often enough to correct iron deficiency in children. Riboflavin deficiency may account for a significant proportion of anemia. Patients with acute inflammation often present with altered levels of iron, total iron-binding capacity (TIBC), and serum ferretin. These tests thus lose their diagnostic value in some patient populations. Vitamin C improves absorption of iron from food, while excessive fiber, phytic acid, tannins, and polyphenols decrease absorption. Low serum iron, hemoglobin and hematocrit, decreased mean cell hemoglobin (MCH) and mean cell hematocrit (MCHC), decreased serum ferritin levels, decreased mean corpuscular volume (MCV), increased WBC/differential, increased TIBC, decreased transferrin saturation, increased red cell distribution width (RDW), decreased reticulocyte count, and the presence of small, microcytic hypochromic RBCs are useful for diagnosis of iron deficiency anemia. Elevated transferrin often indicates early iron deficiency, and it is the last lab value to normalize once the deficiency is corrected. Ferrous salts are the best treatment for iron deficiency anemia. It takes 4-30 days to note improvement after initiation of iron therapy. Vitamin B12 anemia Vitamin B12 anemia, a megaloblastic anemia, is treated with oral cyanocobalmin once weekly for 1 month. This anemia is more common among vegetarians and the elderly, and reduced intestinal absorption is the cause more often than insufficient diet. Low B12 serum levels do not identify all cases of deficiency. Serum methylmalonic acid level and homocysteine levels sometimes are useful. H pylori, atrophic gastritis with hyochlorhydria, and hidden blood loss can cause vitamin B12 anemia. B12 deficiency sometimes is masked by high intake of folic acid. Symptoms of vitamin B12 anemia include: Fatigue Flatulence Nausea and vomiting Diarrhea Upset stomach Constipation Anorexia and weight loss Pale waxy skin Tachycardia Cardiomegaly Achlorhydria Glossitis Recurring megaloblastic anemia Jaundice The Schilling test detects vitamin B12 absorption by measuring the amount of B12 excreted in the urine. A person with vitamin B12 anemia will excrete none. RBC, macrocytic/nucleated cells, increased lactic acid dehydrogenase (LDH), decreased Schilling test, increased gastrin, urinary increased methylmalonic acid, normal or increased serum folate, greatly increased serum homocysteine, decreased serum B12, and increased MCV, MCHC, and MCH can all help with the diagnosis of vitamin B12 anemia. Content adapted from Nutrition and Diagnosis Related Care. References and recommended readings Escott-Stump S. Nutrition and Diagnosis-Related Care. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002:496-503. Thompson C. Laboratory assessment. In: Charney P, Malone A, eds. ADA Pocket Guide to Nutrition Assessment. Chicago, IL: American Dietetic Association; 2004:110-117. Review Date 10/10 G-1394