Pharmacology 7 – Neuromuscular Blocking Drugs
advertisement

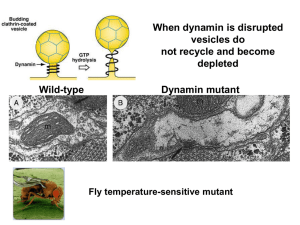
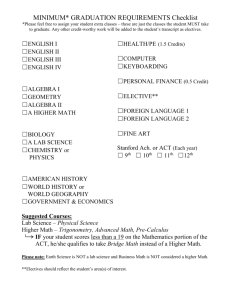
Pharmacology 7 – Neuromuscular Blocking Drugs Anil Chopra 1. 2. 3. 4. 5. 6. 7. What is the neurotransmitter at the skeletal neuromuscular junction and on which receptor type does it act? Define the nature of the antagonism of tubocurarine on the effects of acetylcholine (ACh) at the motor end-plate. Draw a log dose-response curve showing the response of skeletal muscle to increasing concentrations of ACh. How would the shape of this curve be altered in the presence of tubocurarine? Why is tubocurarine not effective if given orally and why does it not act centrally? By what route is tubocurarine administered, what is its duration of action, and how is it eliminated from the body? Why are tubocurarine-like drugs used in surgery and how may their actions be reversed? The major unwanted effects of tubocurarine include a reduction in blood pressure, bronchospasm, tachycardia and apnoea. Explain how these effects arise. The autonomic and Somatic Nervous Systems Parasympathe tic arises in cranial and sacral regions ANS Sympathet ic - arises in thoracic and lumbar regions ACh ACh ACh ACh NA Adrenal medulla A (and NA) released into bloodstream Somatic nervous system Motor neurone ACh = acetylcholine A = adrenaline (epinephrine) NA = noradrenaline (norepinephrine) - Effector organ Effector organ ACh ACh Effector organ Effector organ e.g. sweat gland ACh Skeletal muscle In the somatic nervous system, ACh is released at the neuromuscular junction. There are no ganglia Neuromuscular blocking drugs act here. (5) nAChR - different to ganglionic nAChR (nicotinic Acetylcholine receptor). Have a different structure and morphology. These are opened by both nicotine and acetylcholine and are inotropic (ion channels). The Nicotinic ACh Receptor: 5 sub-units – 2xα, β, γ, and δ Binding of ACh causes a conformational change that allows Na+ influx ACh binds to α-subunits – therefore 2xACh molecules are required for channel to open, one for each α-subunit Strictly cation channels – some Ca2+ also flows in, and some K+ flows out when open as well as bulk inward Na+ flow Stages of Neuromuscular Transmission: 1. Synthesis of ACh in the nerve end 2. Arrival of action potential 3. Influx of Ca2+ through voltage gated channels 4. ACh released into synaptic cleft via endocytosis 5. ACh binds to receptors on post synaptic membrane (Type 1 nicotinic receptors (Type-1 ion channel linked)). This causes Na+ influx into skeletal end-plate leading to a graded end-plate potential 6. ACh comes into contact with AChEsterase which breaks ACH down into choline and acetic acid in 1-2 msecs. The acetic acid is absorbed by the blood stream and removed 7. Choline uptake into the pre-synaptic nerve terminal so it can be used again to generate ACh At the postsynaptic neurone, there are 2 types of drug that can act: NON-DEPOLARISING (COMPETITIVE ANTAGONISTS): Names These block the nAChR: - Tubocurarine - Pancuronium Usage - Neuromuscular blocking Mode of Action Tubocurarine is a competitive neuromuscular blocker that binds to and antagonises nicotinic acetylcholine receptors on the postsynaptic nerve terminal stopping depolarisation. They can bind to receptors but are not flexible enough to allow channel opening. It is used in surgery to stop reflex actions. • Naturally occuring 4° ammonium compound (alkaloid) found in s. american plant (arrow poison) • Range of synthetic drugs now available. • 70-80% of the receptors need to be blocked in order for the drug to have effect. • There is a graded block i.e. different proportions of fibres are blocked. • It causes flaccid paralysis of: • extrinsic eye muscles (double vision) • small muscles of face, limbs, pharynx • respiratory muscles – hence patients should be on ventilators. epp Side Effects and Pharmacokinetics N.B. • They DO NOT affect consciousness • They do NOT affect pain sensation • ALWAYS ASSIST RESPIRATION (until drug inactive or antagonised). The actions of non-depolarising blockers can be reversed by anticholinesterases. E.g. neostigmine (+ atropine) - Should be administered i.v. Does not cross blood brain barrier, or placenta. Onset is 2-3 minutes and effects last from 40-60 minutes. It is not metabolised. It is excreted via the bile (30%) and urine (70%). Side effects include: o Histamine release due to ganglion block. o Hypotension o Can result in tachycardias. o Histamine release can lead to bronchospasm. o Excessive brochial and salivary excretions. DEPOLARISING (AGONISTS): Name - suxamethonium (a.k.a. succinylcholine) Usage Used for muscle relaxation in operations and to facilitate artificial respiration Mode of action » Binds to and excites the postsynaptic nAChR for a long period of time (mins vs msec for ACh) » Eventually action potentials cannot be generated because the voltage sensitive Na channels have been inactivated causing flaccid paralysis Side effects and Pharmacokinetics » Initial spasms due to binding to receptors causing post-operative pain » Muscarinic receptor activation causing bradycardia (prevented by administering atropine). » Potassium release from muscle causes elevated potassium levels » Some people with Myasthenia Gravis – and auto-immune disease that causes loss of function of ACh receptors the drug has no effect » People with poor AchEsterase function the block may last for hours » Duration of action is around 4 mins before it is hydrolysed by AChEsterase » Only drug used clinically