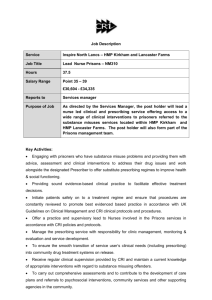
Psychosocial Interventions
advertisement

A Workforce Competency Framework for Newcastle’s Drug and Alcohol Treatment Providers 1 Contents Page Introduction 6 Section A: Psychosocial Interventions 7 A1. Competences to deliver Psychosocial Interventions 8 A1.1 A1.2 A1.3 A1.4 Generic Competences Basic Competences Specific (technical) Competences Metacompetences A2. Motivational Interventions A2.1 A2.2 A2.3 A2.4 A2.5 Generic competences Basic motivational interviewing competencies Specific motivational interviewing techniques Monitoring in motivational interviewing Metacompetences in motivational interviewing A3. Contingency Management A3.1 A3.2 A3.3 A3.4 Generic competences Basic contingency management competences Specific contingency management competences Metacompetences in contingency management A4. Family and social network interventions 9 12 14 A4.1 Treatments/Interventions involving family members A4.1.1 Working with family members (to engage relation in treatment A4.1.2 Joint involvement of family members (and their relatives in treatment) A4.2 Social Behaviour and Network Therapy A4.3 Competences for Behavioural Couples Therapy (BCT) A4.3.1 Generic Competences A4.3.2 Basic BCT competences A4.3.3 Specific BCT competences A4.3.4 Metacompetences in BCT A4.4 Competences for Community Reinforcement Approach (CRA) A5. Cognitive and behavioural based relapse prevention interventions (substance misuse focused) 16 A5.1 Competences for CBT-based guided self help interventions 2 A5.1.1 Generic Competences A5.1.2 Basic CBT competences A5.1.3 Metacompetences in CBT A6. Evidence Based psychological interventions for co-existing mental health problems A6.1 A6.2 A6.3 A6.4 A6.5 Generic competences Basic CBT competences Specific behavioural and cognitive therapy Problem specific competences Metacompetences in CBT for depression and anxiety 21 A6.5.1 Generic competences A6.5.2 CBT specific Metacompetences A7. Psychodynamic Therapy (substance use focused) 24 A7.1 Outline model for psychoanalytic/psychodynamic therapy competences A8. 12 Step Work 25 A9. Counselling – BACP Accredited 26 A9.1 Accreditation for individuals A9.2 Accreditation for services A10. Other Section B 33 Recovery Support Interventions 34 B1. Defining addiction and recovery 35 B2. Peer Support Involvement 36 B2.1 Volunteer Peer Meeting and Greeting B2.2 Informal Support or “Buddying” B2.3 Volunteer Peer Mentoring B3. Facilitated access to mutual aid 38 B3.1 Three essential steps for keyworkers facilitating access to mutual aid B4. Family support 39 B4.1 Drug sector partnership B4.2 Core competencies B4.3 Additional competencies B5. Parenting support 42 3 B5.1 Competences B5.1.1 Qualities and Experience B5.1.2 Skills B5.1.3 Knowledge B5.2 Parenting support programmes B6. Housing Support 44 B7. Employment Support 45 B8. Education and Training Support 46 B9. Supported work projects 47 B10. Recovery Checkups 48 B11. Behavioural based relapse prevention 49 B12. Evidence based mental health focused psychosocial interventions 50 B13. Complementary therapies 51 B13.1 Acupuncture B13.1.1 Competencies to deliver acupuncture B13.2 Reiki B13.2.1 Competencies to deliver reiki B13.3 Reflexology B13.3.1 Competencies to deliver reflexology B13.4 Yoga B13.4.1 Competencies to deliver yoga B14. Other Section C 54 Basis of Pharmacological interventions 55 C1. C1.1 C1.2 C1.3 C1.4 Prescribing Non-medical prescribing Independent prescribing Supplementary prescribing The regulators of non-medical prescribers 56 C2. The Prescribing Competency Framework 58 C2.1 C2.2 C2.3 C2.4 Domain A: The consultation (competencies) Domain B: Prescribing effectively (competencies) Domain C: Prescribing in context (competencies) Competencies for supplementary prescribers 4 C3. Competencies for doctors C3.1 Specialist doctors (3) C3.1.1 Supporting people to recover C3.1.2 Clinical leadership C3.2 Intermediate doctors (2) C3.2.1 Supporting people to recover C3.2.2 Clinical leadership C3.3 Generalist doctors (1) C3.3.1 Supporting people to recover C3.3.2 Clinical leadership C3.4 Competencies C3.5 Training C3.5.1 C3.5.2 C3.5.3 62 Specialist doctors Intermediate doctors Generalist doctors Appendices 65 Appendix 1: Competences to deliver cognitive and behavioural based relapse prevention interventions (substance misuse focused) Appendix 2: Competences needed to relate to people and carry out any form of psychosocial intervention Appendix 3: Parenting support programmes in Newcastle Appendix 4: Entry to education and employment support Appendix 5: The prescribing competency framework Domain A: The consultation Appendix 6: The prescribing competency framework Domain B: Prescribing effectively Appendix 7: The prescribing competency framework Domain C: Prescribing in context Appendix 8: Competencies for supplementary prescribers Appendix 9: The three levels of competency for doctors working with people using drugs and alcohol 5 Introduction The quality and effectiveness of service provision depends upon the ability of staff to deliver interventions and their managers to support them. A competent member of staff consistently applies relevant knowledge and skills to meet the standards of performance required. Competent staff benefit organisations and services, or in this case the treatment system by supporting it to achieve its aim of delivering effective interventions and by allowing the system to be assured of the quality of its services A treatment system which has competent staff also provides protection to its service users as they can be assured that staff are performing to an agreed level and are consistently demonstrating effective practice There are also benefits for staff within commissioned services within the treatment system; working within agreed national occupational standards and locally agreed standards means that they can clearly understand what the expected levels of performance are in their own and in other commissioned services within the system. The recent introduction of Dataset J has specifically defined a number of interventions relating to the treatment and recovery of users of drugs and alcohol under the headings pharmacological, psychosocial and recovery support This paper define the competences required from staff to safely and effectively deliver these interventions, as defined by Dataset J, using existing standards and requirements which might include NHS Knowledge and Skills Framework Drug and Alcohol National Occupational Standards Professional Standards and Codes of Ethics Supporting People Skills for Health NICE guidelines (2012) Royal College of Psychiatrists Royal College of General Practitioners National Treatment Agency for Substance Misuse Department of Health Action for Children 6 Section A Psychosocial Interventions 7 A1: Competences to deliver Psychosocial Interventions The competences required to effectively deliver psychosocial intervention can, according to the British Psychological Society (2010)1, be broken down into the following competences. A1.1 Generic Competences The competences needed to relate to people and to carry out any form of psychological intervention. A1.2 Basic Competences Basic intervention specific competences that are used in most sessions. A1.3 Specific (technical) competences Specific intervention competences that are employed in most sessions (usually associated with high intensity interventions). A1.4 Metacompetences Competences used by therapists to work across all levels and to adapt the intervention to the needs of each individual service users. These competences are abstract as they usually reflect the intentions of the person delivering the intervention and can be difficult to observe directly but can be inferred from the therapists actions. These four categories of competences have been applied throughout this section to describe the necessary competences for staff to deliver psychosocial interventions as defined by Dataset J. Routes to Recovery: Psychosocial Interventions for Drug Misuse – A framework and toolkit for implementing NICE recommended treatment interventions 1 8 A2. Motivational Interventions Dataset J definition: Motivational interventions aim to help service users resolve ambivalence for change, and increase intrinsic motivation for change and self-efficacy through a semi-directive style and may involve normative feedback on problems and progress. They may be focused on substance specific changes and/or on building recovery capital. Motivational interventions can be delivered in group or individual format and may involve the use of mapping tools. Motivational interventions require additional competences for the worker and delivery within a clinical governance framework including appropriate supervision. Motivational Interviewing and Motivational Enhancement Therapy are both forms of motivational interventions.2 A2.1 Generic competences Knowledge of drug misuse and mental health problems Establishing a positive relationship with the service user Establishing good relationships with relevant professionals Gathering background information Giving service users information about drug misuse A2.2 Basic motivational interviewing competencies An ability to: 2 Adopt an empathetic, non-confrontational, collaborative and non-judgmental approach Adopt an evocative tone throughout the intervention which draws out the service user’s ideas, feeling and wants Draw out, identify and discuss the service user’s intrinsic motivation for change Draw from the service user a distinction between how important it is for the service user to change and how confident they are they can maintain this change Respect the individual autonomy of the service user and responsibility for change Communicate to the service user a sense of safety and support Convey acceptance of the service user and to avoid confrontation or the use of persuasion Assist the service user in developing discrepancy between their current situation and future goals ‘Roll with the resistance’ and avoid direct confrontation of resistance Support and enhance a service user’s belief in their ability to carry out a specific activity Help the service user explore and resolve their ambivalence in favour of change Dataset J, November 2012 9 A knowledge of basic principles of stages of change (pre-contemplation; contemplation; preparation; action and maintenance). A2.3 Specific motivational interviewing techniques An ability to: Use affirmative statements to acknowledge service user efforts and strength Use open-ended questions Avoid the use of ‘traps’ including: question-answer traps; labelling traps; premature focus traps; talking side traps; blaming traps; and expert traps A knowledge of the levels of reflection including: repeating; re-phrasing; paraphrasing; and reflecting feeling An ability to use reflective listening through: Forming hypotheses about the meaning of service user statements Testing hypotheses by reflective statements to the service user Using different types of reflective statements including simple reflection, amplified reflection; double-sided reflection An ability to elicit ‘change talk’ in a collaborative manner through: Recognising, empathising and reflecting on desire, ability, reasons and need focused change statements Recognising and strengthening commitment language An ability to: Build rapport through identifying the service user’s concerns Centre discussion around the service user’s concerns and needs Reframe discussion positively Conclude a session with summaries and open-ended discussion on behaviour change Use decisional balance tools to facilitate the exploration of ambivalence Elicit discrepancy between current behaviour and future goals Elicit dissonance between beliefs and behaviours Enhance the service user’s perception of the importance for change and their confidence they can make this change Diffuse blame Invite service users in a non-confrontational manner to consider new perspectives Support self-efficacy via affirmation and positive reinforcement Offer specific information and advice, but only when solicited Elicit discussion of the benefits and drawbacks of changing problem behaviour Develop, in collaboration with the service user, a plan for behaviour change. A2.4 Monitoring in motivational interviewing An ability to identify the service user’s readiness for change, both from structured assessment and open-ended discussion through: 10 Using informal measures of change such as readiness, importance and confidence rulers and other basic measures of change Using key questions to assess readiness to change both to assess and facilitate readiness to change An ability to: Provide summaries during sessions to demonstrate understanding of the service user’s problem, structure the intervention and emphasise positive change focused service user statements Refer to, and elicit open-ended discussion from, assessment data Provide positive and constructive feedback and open-ended discussion on behaviour change during and at the end of sessions Make use of self-monitoring tools to reflect on and improve performance Make use of supervision, and the associated assessment and feedback A2.5 Metacompetences in motivational interviewing An ability to: Adapt motivational interviewing according to the setting in which it is provided Pace the rate of the intervention as relevant to service user needs Set agendas on an ongoing basis in order to clarify session topics and behaviour change targets Recognise service user need for motivational interviewing as it arises, and to deliver it opportunistically Elicit and be responsive to service user’s feedback Integrate motivational interviewing into routine assessment systems. 11 A3. Contingency Management Dataset J definition: Contingency management (CM) provides a system of reinforcement or incentives designed to motivate behaviour change and/or facilitate recovery. CM aims to make target behaviours (such as drug use) less attractive and alternative behaviours (such as abstinence) more attractive. CM requires additional competences for the worker and delivery within a clinical governance framework including appropriate supervision.3 The following competences for contingency management has been derived from Routes to Recovery: Psychosocial Interventions for Drug Misuse – A framework and toolkit for implementing NICE recommended treatment interventions, pp. 28-30 A3.1 Generic Knowledge of drug misuse and mental health problems Establishing a positive relationship with the service user Establishing good relationships with relevant professionals Gathering background information Giving service users information about drug misuse A3.2 Basic contingency management competences Knowledge of contingency management principles Structuring a contingency management programme Managing the relationship with a service user in a manner consistent with contingency management principles A3.3 Specific contingency management competences Drug testing for a contingency management programme Assessment for a contingency management programme Establishing a contingency management programme Delivering and monitoring contingency management programme Managing relationships with external agencies concerning contingency management Ending the intervention A3.4 Metacompetences in contingency management An ability to: 3 Judge the level and approach of contingency management intervention required Design a contingency management schedule in accordance with behavioural principles Dataset J, November 2012 12 Adapt a contingency management schedule to the characteristics and needs of individual service users including the nature of their drug misuse Adapt the contingency management intervention according to the setting in which it is delivered Identify barriers to effective intervention and to resolve these within the boundaries of the agreement with the service user and the overall objectives of the service setting Make use of supervision, assessment and feedback on performance as a contingency management therapist 13 A4. Family and social network interventions Dataset J definition: Family and social network interventions engage one or more of the client’s social network members who agree to support the client’s treatment and recovery. The interventions use specific psychosocial techniques which aim to increase family and social network support for change and decrease family and social support for continuing drug and/or alcohol use. These interventions may involve the use of mapping tools. They require additional competences for the worker and delivery within a clinical governance framework including appropriate supervision. Examples: Social behaviour network therapy (SBNT), Community Reinforcement Approach (CRA), Behavioural Couples Therapy (BCT) & formal Family Therapy4 A4.1 Treatments/interventions involving family members A4.1.1 Working with family members (to engage relation in treatment) Family intervention Community reinforcement and family training Unilateral family therapy Cooperative counselling A41.2 Joint involvement of family members (and their relatives in treatment) Conjoint family group therapy Behavioural couples therapy Family therapy Network therapy Social behaviour and network therapy A4.2 Social Behaviour and network therapy No competences currently available (Skills Consortium) A4.3 Competences for Behavioural Couples Therapy (BCT)5 A4.3.1 Generic competences Knowledge of drug misuse and mental health problems Engaging service users Establishing good relationships with relevant professionals 4 Dataset J, November 2012 Routes to Recovery: Psychosocial Interventions for Drug Misuse – A framework and toolkit for implementing NICE recommended treatment interventions, pp. 32-34 5 14 Dealing with the emotional content of sessions Gathering background information Giving service users information about drug misuse A4.3.2 Knowledge of family approaches to drug misuse and mental health problems Assessment of couples with drug misuse problems Knowledge and rationale of BCT A4.3.3 Basic BCT competences Specific BCT competences Establishing the therapeutic approach in BCT Monitoring of treatment progress in BCT Monitoring of drug and alcohol misuse and associated risks in BCT Ensuring effective delivery of BCT Relapse prevention A4.3.4 Metacompetences in BCT Ability to: Adapt sessions responsively in relation to service user feedback Implement BCT in a manner consonant with its underlying philosophy Select and skilfully apply the most appropriate BCT intervention techniques Structure sessions and maintain appropriate pacing Identify and manage obstacles to treatment participation and goals both in and out of session Identify and respond appropriately to non-substance related problems which may interfere with BCT or present increased risks for the couple, their family or the wider social network A4.4 Competences for Community Reinforcement Approach (CRA) No competences currently available (Skills Consortium) but Dr Robert Myers, the recognised expert in this field states that a successful CRA therapist must have sound, fundamental counselling skills. In addition, supportiveness, empathy, and a genuinely caring attitude are key to establishing the consumer-therapist relationship. CRA also requires that the therapist be directive, energetic, and engaging. (Bob Myers) Attendance at CRA course facilitated by Dr Myers (lead in this field) 15 A5. Cognitive and behavioural based relapse prevention interventions (substance misuse focused) Dataset J definition: Cognitive and behavioural based relapse prevention interventions develop the service users’ abilities to recognise, avoid or cope with thoughts, feeling and situations that are triggers to substance use. They include a focus on coping with stress, boredom and relationship issues and the prevention of relapse through specific skills – e.g. drug refusal, craving management. They can be delivered in group or individual format and may involve the use of mapping tools. They require additional competences for the worker and delivery within a clinical governance framework including appropriate supervision. Examples: CBT based relapse prevention (which may include mindfulness and ‘third wave’ CBT), behavioural self control (alcohol)6 The following competences for CBT-based guided self help interventions have been derived from Routes to Recovery: Psychosocial Interventions for Drug Misuse – A framework and toolkit for implementing NICE recommended treatment interventions, pp. 35-36 A5.1 Generic competences Establishing a positive relationship with the service user An ability to: Develop an empathetic, warm and genuine relationship Communicate effectively through appropriate use of empathic statements, reflection, clarification, verbal and non-verbal behaviours. Establishing good relationships with relevant professionals An ability to: Communicate effectively with professionals about the nature of the service user’s difficulties, the intervention(s) offered and the resulting outcomes. Gathering background information An ability to: 6 Gain an overview of the service user’s current life situation, any specific stressors and level social support Elicit information regarding diagnosis, past history and present life situation Gather information relating to the impact of emotional distress including work, home, social and private leisure and close personal relationships. Dataset J, November 2012 16 Establishing a context for the service and providing rationale for the service user of the self-help model An ability to: Help the service user understand that the main purpose of the intervention is to facilitate the use of self-help material(s) Provide a rationale for guided self-help to service users in an encouraging and realistic manner Establish a context for the intervention, through clear explanation of the practitioner role Ensure that the service user understands the nature and the timing of sessions and the schedule of contacts Convey to the service user the service-user-led, collaborative nature of a selfhelp intervention. Giving service users specific information relevant to the intervention An ability to: Impart accurate information on the nature, course and frequency of the presenting problem Give the service user information about alternative available evidence-based psychological therapies treatment-choices, as set out in the agreed protocol for the delivery of guided self-help Give realistic information regarding outcomes and the prognosis for the service user’s condition relevant to the self-help interventions. Assessing the service user’s main problems using a semi-structured interview An ability to: Use open and closed question styles flexibly and responsively Phrase questions unambiguously Give the service user regular summaries during the interview Assess, using agreed protocols; risk to self, others and self neglect (distinguishing between thoughts, actions and plans) and establish preventative factors Gather information on current and past treatment (including relevant medical, psychological, social and pharmacological interventions) Gather relevant information on drug and alcohol use Identify the key problem(s) through appropriate information gathering relating to the impact of emotional distress including work, home, social and private leisure and close personal relationships Elicit information regarding diagnosis, past history and present life situation Gather information relating to the impact of emotional distress including work, home, social and private leisure and close personal relationships. 17 Establishing a context for the service and providing rationale for the service user of the self-help model An ability to: Help the service user understand that the main purpose of the intervention is to facilitate the use of self-help material(s) Provide a rationale for guided self-help to service users in an encouraging and realistic manner Establish a context for the intervention, through clear explanation of the practitioner role Ensure that the service user understands the nature and the timing of sessions and the schedule of contacts Gathering information using formal assessment methods An ability to: Administer and interpret formal measures of mental health (e.g. PHQ-9, CORE-OM, the BDI, problem and goal statements) Support the service user in the completion of formal measures of mental health and to support the service user in using these to monitor their progress Support the service user in use of formal measures of mental health to determine the content and pace of the intervention. Decision making regarding the appropriateness of the intervention An ability to: A5.2 Agree on the suitability of the self-help intervention for the service user Collaboratively negotiate and agree with a service user the next steps in contact including organisational and therapeutic arrangements Where necessary in conjunction with a supervisor, identify service users whose problems lie outside the scope of low-intensity interventions and when alternative interventions are require Recognise, where necessary in conjunction with a supervisor, when referral to another part of the service is appropriate. Basic CBT competences Socialising the service user to a CBT model An ability to: Communicate the essential components of a cognitive, and/or behaviourally based self-help programme Communicate the options available to a service user within a CBT based selfhelp programme 18 Agreeing the aims of the intervention An ability to: Summarise information gathered from the assessment into a concise problem summary which is shared and checked with the service user (which includes information on environmental and/or intrapersonal triggers, physiological, behavioural and cognitive components of the main problem and the broader impact of this problem on the service user’s functioning) Use the problem summary to agree intervention goals with the service user Negotiate and agree the specific components of a self-help CBT based intervention. Facilitating service user self-monitoring An ability to: Support self-monitoring through the use of service-user-completed diaries (including activity schedules, sleep and thought diaries) Review diary records with the service user, and to discuss any implications of these observations with the service user. Facilitating service user led interventions An ability to: Understand the use of appropriate self-help materials (including written materials) and self-monitoring materials, and support the service user in the use of relevant and effective materials Help the service user problem solve difficulties encountered in the use of written materials, and self-monitoring materials Help the service user think through the rationale for performing homework and related tasks, and to identify and problem solve any anticipated difficulties in carrying out tasks Communicate effectively about the delivery, implementation and monitoring of self-help interventions both in face-to-face contacts and in telephone contacts. Ending the intervention A5.3 An ability to negotiate an appropriate ending to the intervention, including discussion of relapse prevention. Metacompetences in CBT An ability to: Maintain a clear distinction between acting as a facilitator of self-help and taking on the more extensive role of a therapist 19 With service users who are not making progress or who show low motivation, to identify when to persist with the intervention and when to re-evaluate its appropriateness In the context of indicators of service user progress, maintain fidelity to the intervention model in the face of service user complexity Use supervision to identify gaps in knowledge and understanding, and reflect on and to learn from experience. Further information relating to these competencies are tabled at Appendix 1 7 7 Appendix 1 - Page 64 20 A6. Evidence –based psychological interventions for co-existing mental health problems Dataset J definition: NICE guidelines8 for mental health problems generally recommend a stepped care approach. Low intensity psychological intervention for co-existing mental health problems, include guided self-help or brief interventions for less severe common mental health problems. High intensity psychological therapies (such as cognitive behavioural therapy) are recommended for moderate and severe problems. Typically formulation-based and delivered by clinicians with specialist training and who are registered with a relevant professional / regulatory body. They can be delivered in group or individual format. Both low and high intensity interventions require additional competences for the worker and delivery within a clinical governance framework including appropriate supervision9 A6.1 Generic competences Knowledge and understanding of mental health problems Knowledge of, and ability to operate within, professional and ethical guidelines Knowledge of a model of therapy, and the ability to understand and employ the model in practice Ability to: Engage client Foster and maintain a good therapeutic alliance, and to grasp the client’s perspective and ‘world view’ Deal with emotional content of sessions Manage endings Undertake generic assessment (relevant history and identifying suitability for intervention) Make use of supervision. A6.2 Basic CBT competences Knowledge of: Basic principles of CBT and rationale for treatment Common cognitive biases relevant to CBT The role of safety-seeking behaviours Ability to: Explain and demonstrate rationale for CBT to client Routes to Recovery: Psychosocial Interventions for Drug Misuse – A framework and toolkit for implementing NICE recommended treatment interventions, pp. 40-41 8 9 Dataset J, November 2012 21 Agree goals for the intervention Ability to structure sessions: Sharing responsibility for session structure and content Adhering to an agreed agenda Planning and reviewing practice assignments (‘homework’) Using summaries and feedback to structure the session. Use measures and self monitoring to guide therapy and to monitor outcome Devise a maintenance cycle and use this to set targets Problem solving Ability to end therapy in a planned manner, and to plan for long-term maintenance of gains after treatment. A6.3 Specific behavioural and cognitive therapy Exposure techniques Applied relaxation and applied tension Activity monitoring and scheduling Guided discovery and Socratic questioning: Using thought records Identifying and working with safety behaviours Detecting, examining and helping client reality test automatic thoughts/images Eliciting key cognitions/images Identifying and helping client modify assumptions, attitudes and rules Identifying and helping client modify core beliefs Employing imagery techniques Planning and conducting behavioural experiments. Ability to: Develop formulation and use this to develop treatment plan/case conceptualisation Understand client’s inner world and response to therapy. A6.4 Problem-specific competences Specific phobias Social phobia – Heimberg; Clark Panic disorder (with or without agoraphobia) – Clark; Barlow Obsessive compulsive disorder (OCD) – Steketee; Kozac Generalised anxiety disorder (GAD) – Borkovec; Dugas and Ladouceur; Zinbarg, Craske and Barlow Post-traumatic stress disorder (PTSD) – Foa and Rothbaum; Resick; Ehlers Depression – high-intensity interventions: o cognitive therapy – Beck o behavioural activation – Jacobson. 22 A6.5 Depression – low-intensity interventions: o behavioural activation o guided CBT self help. Metacompetences in CBT for depression and anxiety A6.5.1 Generic Metacompetences: Capacity to: Use clinical judgment when implementing treatment models Adapt interventions in response to client feedback Use and respond to humour. A6.5.2 CBT specific Metacompetences: Capacity to: Implement CBT in a manner consonant with its underlying philosophy Formulate and to apply CBT models to the individual client Select and apply most appropriate BT and CBT method Structure sessions and maintain appropriate pacing Manage obstacles to CBT therapy. 23 A7. Psychodynamic therapy (substance use focused) Dataset J definition: A type of psychotherapy that draws on psychoanalytic theory to help people understand the developmental origins of emotional distress and behaviours such as substance misuse, by exploring unconscious motives, needs, and defences. Psychodynamic therapy requires additional competences for the worker and delivery within a clinical governance framework including appropriate supervision. Therapists should be registered with an appropriate professional/regulatory body.10 The competencies needed to carry out any form of psychoanalytical /psychodynamic therapy have been defined by Lemma, Roth and Pilling11. These are tabled at Appendix 2. 12 10 Dataset J, November 2012 11 ‘The competences required to deliver effective Psychoanalytic/ Psychodynamic Therapy’, Alessandra Lemma, Anthony D. Roth and Stephen Pilling, Research Department of Clinical, Educational and Health Psychology UCL available online at http://www.ucl.ac.uk/CORE 12 Appendix 2, page 65 24 A8. 12 Step Work Dataset J definition: A 12-step program or counselling intervention for recovery from addiction, compulsion, or other behavioural problems. Interventions are delivered within a clinical governance framework including appropriate supervision. The aim of a 12-step programme is to facilitate service users to complete some or all of the 12-steps. (American Psychological Association)13 Any service provider delivering any element of 12 step work should have knowledge understanding and application of the relevant steps as well as competencies relating to psychosocial interventions. See Section B Recovery Support Interventions – Facilitated access to Mutual Aid 13 Dataset J, November 2012 25 A9. Counselling – BACP Accredited Dataset J definition: A systematic process which gives individuals an opportunity to explore, discover and clarify ways of living more resourcefully, with a greater sense of well-being. This requires additional competences for the worker and delivery within a clinical governance framework including appropriate supervision14 A9.1 Accreditation for individuals - Process for BACP Counsellor/Psychotherapist Accreditation – September 201215 COUNSELLOR/PSYCHOTHERAPIST ACCREDITATION SCHEME STANDARD FOR ACCREDITATION ‘To demonstrate the capacity for independent, competent, ethical practice’ Individuals can apply for accreditation if they provide counselling or psychotherapy to individual people, couples, groups or families and can provide satisfactory evidence to meet all Criteria 1 to 9 CRITERIA FOR APPLICATION Eligibility Criteria 1-5 When individuals apply and throughout the assessment process, they must be: 1. A member of BACP 2. Covered by professional indemnity insurance When individuals submit their application they must be 3. Practising counselling or psychotherapy 4. Able to evidence their training and supervised practice: They must have undertaken training and supervised practice to meet one of the following criteria: EITHER: 4.1 14 They have been awarded a qualification from a BACP accredited training course Dataset J, November 2012 British Association for Counselling and Psychotherapy (2013) – Applying for accreditation available at http://www.bacp.co.uk/accreditation/ Accessed: January 2013 15 26 AND Have been in practice at least three years when they apply for accreditation Have at least 450 hours of supervised practice accumulated within three to six years (they do not have to be consecutive years) Of the 450 hours at least 150 of the hours of supervised practice must be after the successful completion of your BACP accredited course Have been supervised for at least 1½ hours per month throughout the period of practice submitted OR: 4.2 They have successfully completed and received an award for practitioner training that: Included at least 450 hours of tutor contact hours Was carried out over at least two years (part-time) or one year (full-time) Had a supervised placement as an integral part of the training Covered theory, skills, professional issues and personal development AND 5. Have been in practice at least three years when you apply for accreditation Have at least 450 hours of supervised practice accumulated within three to six years (they do not have to be consecutive years) Of the 450 hours at least 150 hours of supervised practice must be after you have successfully completed your practitioner training Have been supervised for at least 1½ hours per month throughout the period of practice submitted. Supervision They have an ongoing contract for counselling/psychotherapy supervision for a minimum of 1½ hours per month for each month in which practice is undertaken. Reflective Practice Criteria 6-9 6. Continuing Professional Development (CPD) 6.1 Describe a CPD activity, relevant to your area of practice that they have undertaken in the 12 months before applying for accreditation 6.2 Provide reason(s) for choosing the activity with reference to your practice 6.3 Show how the activity has influenced their practice 7. Self-awareness 7.1 7.2 Describe an experience or an activity which has contributed to your (their)own self-awareness Provide a reason(s) for choosing the experience or activity 27 7.3 8. Knowledge and understanding 8.1 8.2 8.3 9. Show how you (they) use this self-awareness in your(their) practice Describe a rationale for your client work with reference to the theory / theories that inform all your(their) practice. Describe the place of your (their) self-awareness within your (their) way of working Describe how issues of difference and equality impact upon the therapeutic relationship. Practice & Supervision In your(their) case material account for: 9.1 9.2 9.3 9.4 9.5 9.6 How your (their) practice is consistent with your(their) described way of working (in 8.1) How you(they) use your(their) self-awareness in the therapeutic relationship How your(their) practice demonstrates your(their) awareness of issues of difference and equality and the impact they have on your(their) counselling / psychotherapy relationships Use of the BACP Ethical Framework for Good Practice in Counselling and Psychotherapy and how supervision influences your (their) practice by: Describing the awareness you (they) have gained through reflection in and on supervision Showing how you (they) apply that awareness in your practice This is based around a set of criteria and quantitative requirements rather than a set of competencies. BACP is currently working on devising competencies for talking therapies but these are still in the early stages of development. There are a variety of accreditation fees in addition to annual membership fees. A9.2 Accreditation for services - BACP Service Accreditation Scheme16 The Service Accreditation Scheme (SAS) helps the public, and practitioners, identify services providing a high standard of counselling/psychotherapy. The scheme is open to services that meet the eligibility and operational criteria and agree to be bound by the scheme’s conditions. This includes services that are members in their own right, or that are part of an organisational member. In the latter case, the organisational member applies for accreditation and bears ultimate responsibility for that service. To achieve accreditation, the service must apply in the prescribed form and demonstrate that its procedures and practices meet all the criteria. 16 BACP Service Accreditation Scheme available at http://www.bacp.co.uk/accreditation/ Accessed: January 2013 28 On acceptance, an accredited service: Will receive a certificate of accreditation Will have its name listed as a BACP accredited service May advertise its service as a BACP accredited service (this can be included on official notepaper) Accreditation is awarded for a five-year period, during which the service is monitored by BACP’s quality assurance procedures. At the end of the period the service has to apply for renewal of its accredited status. Application fees are charged in accordance with BACP policy. PART I – CRITERIA FOR ACCREDITATION OF SERVICES The criteria are divided into two parts: Part A: Eligibility criteria Part B: Operational criteria Part A: Eligibility criteria These criteria must be met before an application is accepted for assessment under the operational criteria specified in Part B. Services making an application for accreditation must: Criterion 1 Be an organisational member of BACP and subject to its Ethical Framework for Good Practice in Counselling and Psychotherapy and Professional Conduct Procedure. If the service is part of an organisational member, it is the organisational member that will make the application for the accreditation of its counselling/psychotherapy service. Criterion 2 Provide a counselling/psychotherapy service. Criterion 3 Include at least three practitioners who undertake counselling/psychotherapy. Part B: Operational criteria Applicants should provide clear, concise and appropriate evidence of meeting all these criteria. Criterion 4 – Policy 4.1 Aims and Objectives A statement of aims and objectives, available to all staff and service users, must set out clearly: 29 4.2 The purpose of the services provided The type of counselling/psychotherapy offered The ethical framework adhered to The limits of confidentiality The context and contracting of the work (this includes payment for services, relationships with the host organisation (if relevant) and times of service availability). Publicity All service publicity material and pre-counselling information should comply with the Ethical Framework for Good Practice in Counselling and Psychotherapy and be readily available. 4.3 Staffing 4.3.1 A specified person must hold clinical responsibility for the service. They should be a member of an appropriate professional body, subject to its complaints procedure and accredited by or of equivalent standing with it. 4.3.2 A training and development policy should exist for all staff. 4.3.3 A clear selection procedure for counsellors/psychotherapists should exist 4.3.4 Recruitment panels for counsellors/psychotherapists in the service must include at least one qualified, experienced practitioner familiar with the work of the service. 4.4 Equal Opportunities The service should: 4.4.1 Be committed to equality of opportunity for its staff and for users of the service and comply with all relevant legislation. It must demonstrate a nondiscriminatory approach to staff and users, irrespective of age, colour, creed, culture, disability, education, ethnicity, gender, information, knowledge, mobility, money, nationality, race, religion, sexual orientation, social class, status, etc. 4.4.2 Define its target population and survey users using an equal opportunities questionnaire or similar procedure. 4.4.3 Recognise its accessibility limitations and publish a strategy for addressing this. 4.5 Evaluation and feedback 4.5.1 All aspects of the service’s work should be formally evaluated by users and staff on a regular basis that is at least annually. 4.5.2 Evaluation findings should be reviewed and appropriate changes made. 4.5.3 Annual feedback should be given to users and other stakeholders. 4.5.4 All feedback must maintain users’ anonymity. Criterion 5 – Management and administration 5.1 Service structure 30 5.1.1 There should be clearly defined and effective management and organisational structure, which includes a Head of Service who has knowledge and experience of the counselling field and who has overall responsibility for management of the service. 5.1.2 There should be clear lines of accountability/reporting. 5.1.3 Formal arrangements for financial accountability should be in place. 5.2 Community liaison Links with referral resources and specialist services in the community should exist. 5.3 Health and Safety 5.3.1 The service must comply with the current Health and Safety at Work Act and other relevant legislation. 5.3.2 Practitioners must be given training and best practice guidelines for potential dangerous and violent situations. 5.3.3 Specific training and guidelines should be provided for those that undertake home visits. 5.3.4 There should be procedures that help all staff identify and deal with clients at risk to themselves or others. 5.3.5 Procedures must exist on how to deal with critical incidents such as dangerous or violent behaviour. 5.3.6 All counsellors/psychotherapists (both voluntary and salaried) should be covered by Professional Indemnity and Public Liability insurance. 5.4 Administration 5.4.1 All records (whether paper or electronic) should be secure and confidential. 5.4.2 The service should comply with the current Data Protection Act and other relevant legislation. 5.4.3 Appointment systems, if used, must be private and confidential. 5.4.4 Ownership of, and access to, service user records should be specified. 5.5 Management 5.5.1 All service staff should have the opportunity to meet on a regular basis and to have access to suitable consultation and feedback. 5.5.2 Part-time, newly qualified practitioners and trainees must be supported by a permanent member of the counselling/psychotherapy staff, and training in the service systems and procedures must be given. 5.5.3 Demand on the service should be monitored and managed. 5.5.4 There should be systems to monitor and manage the quality of practitioners work. 5.5.5 Staff undertaking a variety of roles must make it clear to service users and colleagues which one they are in at any given time. 5.5.6 Grievance and disciplinary procedures must exist for all staff. 31 5.5.7 Formal links should exist for consultation and referral between counselling/ psychotherapy staff and medical and psychiatric services. Criterion 6 – Delivery 6.1 Accommodation Rooms used for counselling/psychotherapy purposes should be private and free from interruption, furnished appropriately and, when counselling is in process, used exclusively for that purpose. 6.2 Professional conduct 6.2.1 The service must be run in accordance with BACP’s Ethical Framework for Good Practice in Counselling and Psychotherapy. 6.2.2 Where counselling/psychotherapy is not appropriate, or the service does not have the appropriate skills, users must be referred to suitable agencies e.g. psychiatric services, GP. 6.2.3 Counsellors/psychotherapists should monitor and develop their professional work through regular supervision/consultation and continuing professional development (CPD). 6.2.4 All secretarial, administration and reception support staff should work in a manner that maintains confidentiality. Reception staff must be experienced and confident in working with those in distress. 6.2.5 An appropriate client/customer complaints procedure should be available. Organisations need to be a BACP member in order to be eligible to apply for accredited status and there are a variety of submission fees depending on whether the organisation is from the not-for-profit or commercial sectors. The fees cover the cost of assessment both of the initial application and the annual report which needs to be submitted during the 5 year accreditation term. At the end of 5 years, a new application needs to be submitted in order to maintain accreditation. 32 A10. Other Dataset J definition: An intervention based on established psychological models/ theories, that have an evidence base, and that is undertaken by a worker with the required competences with adequate supervision and clinical governance arrangements This category can only be used where an intervention is not covered by individual, or a combination of, categories above. It is anticipated that use of this category would be relatively uncommon. Competence will be dependent upon the specific intervention being delivered. 33 Section B Recovery Support Interventions 34 B1 Defining addiction and recovery Addiction is often referred to as the continued use of a mood altering substance or behavior despite adverse harmful consequences, or a neurological impairment leading to such behaviors. There are many definitions of recovery, and recovery means different things to different people. Essentially, it is defined by ‘voluntarily maintained lifestyle characterized by sobriety, personal health and citizenship’ or the ‘process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential’.17 However, addiction and dependence are referred to as ‘chronic relapsing conditions’ which mean that it can take some people a long time to recover and numerous attempts at treatment programmes before moving into recovery. Providing services for people affected by drugs or alcohol includes supporting complex and multiple needs, and requires a holistic response which is dependent on the individual and their situation. 17 Source: The Betty Ford Institute Consensus Panel. "What is recovery? A working definition from the Betty Ford Institute" Journal of Substance Abuse Treatment. 20 September 2007. 35 B2. Peer Support Involvement Dataset J definition: A supportive relationship where an individual who has direct or indirect experience of drug or alcohol problems may be specifically recruited on a paid or voluntary basis to provide support and guidance to peers. Peer support can also include less formal supportive arrangements where shared experience is the basis but generic support is the outcome (e.g. as a part of a social group). This may include mental health focused peer support where a service user has co-existing mental health problems. Where peer support programmes are available, staff should provide information on access to service users, and support access where service users express an interest in using this type of support18 The Scottish Drugs Forum suggest that peer support involvement has three main areas of work 19: volunteer peer meeting and greeting, informal support or buddying and volunteer peer mentoring B2.1 Volunteer Peer Meeting and Greeting This may be done by a volunteer current service user who knows and attends the service regularly whose role is to meet and welcome potential or new service users either at the first service visit or initial assessment, and where appropriate, show them around the service, explain basic health and safety and housekeeping procedures Photocopy the checklist and give a copy to the new service user and one for a service file specific to Service User Involvement At key work sessions, key worker can ask volunteer involved in Peer Meet and Greet how many welcome sessions they have done, how they feel, etc. This should be recorded in the service users file/care plan. B2.2 Informal Support or “Buddying” This may be done by a current service user who knows and uses the service regularly, whose role could either incorporate meet and greet with further responsibilities, or be a separate role altogether and who would introduce the new service user to the other service users and staff and agrees an arrangement whereby the “buddy” makes regular contact with the new service user until the new service user feels comfortable. 18 Dataset J, November 2012 Scottish Drugs Forum, Service user and peer support available at http://www.sdf.org.uk/userinvolvement/best-practice/ : Accessed: February 2013 19 36 B2.3 Volunteer Peer Mentoring This may be done by a service user who is in the final stages of their treatment programme, aftercare or who has left and would like to do some volunteering within the service. Their role again could incorporate both meet and greet and “buddying” with further responsibilities or could be a separate role altogether. This role would be a more formal one than the other two and would assist the development of other service users through offering support, advice and encouragement so the service user can draw on the experience of the volunteer peer mentor. 37 B3. Facilitated access to mutual aid Dataset J definition: Staff provide a service user with information about selfhelp groups. If a service user has expressed an interest in attending a mutual aid group, staff facilitate the person’s initial contact with the group, for example by making arrangements for them to meet a group member, arranging transport, accompanying him or her to the first session and dealing with any concerns. These groups may be based on 12-step principles such as Alcoholics Anonymous, Narcotics Anonymous and Cocaine Anonymous) or other approaches (such as SMART Recovery)20 B3.1 Three essential steps for key workers facilitating access to mutual aid 21 1. Introduce the topic of mutual aid into sessions with service users and promote the value of attending meetings 2. Help the service user to contact a current member of a mutual aid group who can accompany him/her to a meeting 3. Take an active interest in the service user’s attendance at, engagement with and experience of mutual aid groups. It requires keyworkers to be knowledgeable about mutual aid and to promote its value. Services also need to build contacts with local groups. Familiarity can be improved if staff 20 Read the information or watch the videos on the websites of each of the 12step and SMART Recovery mutual aid groups Become familiar with the key texts i.e. Alcoholics Anonymous’ The Big Book (Cocaine Anonymous also use this) and Narcotics Anonymous’ Basic Text Take a short course, such as SMART Recovery’s one-hour online introduction Talk to members of the mutual aid groups. All operate a public information service whose purpose is to talk to professionals about their work – their speakers are often members with substantial experience Learn from colleagues and clients. Many drug and alcohol services have staff and service users who attend mutual aid groups and who may be willing to share their knowledge and experience Attend an open meeting, where professionals are welcome. All the fellowships run these and all they ask is that you identify yourself as a professional before the meeting starts. Dataset J, November 2012 21 Helping clients to access and engage with mutual aid – Turning evidence into practice available at: http://www.nta.nhs.uk/r-Evidence%20and%20Guidance.aspx : Accessed: January 2013 38 B4. Family Support Dataset J definition: Worker has assessed the family support needs of the individual/family as part of a comprehensive assessment, or ongoing review of their treatment package. Agreed actions can include: arranging family support for the family in their own right or family support that includes the individual in treatment22 This work closely links to family and support network interventions (under Psychological interventions) and can be divided into three broad categories23 Interventions that work with family members to promote the entry and engagement of drug and or alcohol users into treatment The joint involvement of family members and the relatives using drugs and/or alcohol in the treatment of the user Interventions aimed to respond to the needs of family members affected by drug and alcohol problems in their own right The 5 Step family intervention in primary care model24 support/intervention model should be used when working with families and focuses on staff being able to do carry out the following: Listen non-judgementally Provide information Discuss ways of responding Explore sources of support Arrange further help if needed B4.1 Drug Sector Partnership Four national charities, Adfam, DrugScope, eATA and the Alliance – have formed the Drug Sector Partnership 25 to support community and voluntary sector organisations working in the drug and alcohol sector. The partnership suggest that there are core and additional competencies of a family practitioner working with families affected by drug or alcohol use. 22 Dataset J, November 2012 23 Copello, Vellemand and Templeton, 2005 24 Copello et al (2007) 'The 5-Step family intervention in primary care: I. Strengths and limitations according to family members', Drugs: education, prevention and policy, 14:1, 29 - 47 25 www.drugsectorpartnership.org.uk/ 39 B4.2 Core competencies SCDCPC311: SFHSS03: SCDLDSS6: ASTH416: Promote effective communication and information sharing Promote, monitor and maintain health, safety and security in the workplace Reflect on, develop and maintain your practice Develop practice which promotes choice, well-being and protection of all individuals B4.3 Additional competencies CCSCC17: SFHAB5: SFHAD1: SFHMH13: SFHMH6: Contribute to safeguarding children, young people and vulnerable adults Assess and act upon immediate risk of danger to substance users Raise awareness about substances, their use and effects Work with families, carers and individuals during times of crisis Assess the needs of carers and families of individuals with mental health needs These National Occupational Standards (NOS) have been taken from the 2009 Health and Social Care suite and Adfam and the Federation of Drug and Alcohol Professionals (FDAP) have jointly developed a competence-based certification for practitioners supporting families affected by drugs and alcohol. The new FDAP/Adfam Drug & Alcohol Family Worker Professional Certification is specifically designed for practitioners working with families affected by substance misuse, after consultation with the sector, and the development of a unique role profile. It will provide practitioners with a package of benefits, including: This certification is offered at the registration level. Practitioners will, as a minimum, require their employers to attest to their competence in each of the national occupational standards outlined in the Role Profile. Practitioners will be required to develop a portfolio of proof of competence which may be asked for by FDAP as part of random sampling and which will allow them to demonstrate continued professional development in order to re-accredit at the end of the 3 years. Recertification Certification is valid for three years. To be eligible for re-certification, a practitioner must provide up to date evidence of their on-going competence in the units concerned. 40 Professional standards As well as demonstrating their competence, to be certified as a Drug & Alcohol Family practitioners must also adhere to FDAP's Code of Practice26. 26 Available at: http://www.fdap.org.uk/code_of_practice.php Accessed: April 2012 41 B5. Parenting support Dataset J definition: Worker has assessed the family support needs of the individual as part of a comprehensive assessment, or ongoing review of their treatment package. Agreed actions can include a referral to an in-house parenting support worker where available, or to a local service which delivers parenting support27 B5.1 Competences to deliver parenting support 28 The person should have the ability to: Carry out a comprehensive substance misuse assessment - DANOS AF3 Contribute to protecting children, young people from danger, harm and abuse (HSC325) B5.1.2 Qualities and experience The person should be: Child focused Warm, respectful and sensitive Action focused Engage and build trust Support and challenge 5.1.3 Skills The person should have the following skills: Empowering and enabling families Communication skills Planning skills Decision making and problem solving skills Providing a flexible and non-prescriptive approach to delivery Engaging and working with other services Self awareness and self reflection Ability to interact positively with children and young people 5.1.4 Knowledge The person must have: Technical and professional expertise Awareness of equality and diversity issues 27 Dataset J, November 2012 ‘Skills framework for developing effective relationships with vulnerable parents to improve outcomes for children and young people (2011) available at: www.actionforchildren.org.uk/ 28 42 Understanding family context Knowledge of support available B5.2 Parenting Support Programmes There is a variety of parenting support programmes in Newcastle29 which are coordinated by Parent Early Intervention Programme (PEIP). Staff in commissioned services should have knowledge of and be able to appropriately signpost or refer clients to30 these programmes. 29 http://www.newcastle.gov.uk/education-and-learning/parental-support/parenting-supportprogrammes-newcastle 30 Appendix 3, page 74 43 B6. Housing Support Dataset J definition: The worker has assessed the housing needs of the individual as part of the comprehensive assessment, or on-going recovery care planning process, and has agreed goals that include specific housing support actions by the treatment service, and/or active referral to a housing agency for specialist housing support. Housing support covers a range of activities that either allows the individual to maintain their accommodation or to address an urgent housing need31 Staff in commissioned services should, as part of a client’s initial (comprehensive) assessment and ongoing review32: Assess housing related need at entry to treatment and review regularly Optimise treatment to improve someones stability and ability to satisfy a landlord of their ability to maintain a tenancy Provide advice, information and advocacy to ensure people in treatment are being paid appropriate benefits Provide training and support (or access to them) in the skills needed to maintain a household and tenancy including financial and debt management to ensure rent is paid Work with people to improve chances of employment Provide (often in partnership with others) second stage or other supported accommodation Work with other agencies to ensure people have the foundations for stability somewhere to live, an income, be free from excessive debt. In addition, staff in commissioned drug treatment services should 31 32 33 Understand the ‘Gateway’33, its operating policies and procedures and how it relates to their service/service users Have knowledge of the housing related services available within the city and what those services provide Have knowledge and understanding of the Drug Management Protocol Be able to effectively signpost or refer service users to appropriate agencies Dataset J, November 2012 Medications in Recovery – Re-orientating drug dependence treatment, Strang 2012 p.23 http://www.newcastle.gov.uk/housing/housing-advice/newcastle-gateway#whatisgateway 44 B7. Employment Support Dataset J definition: The worker has assessed the employment needs of the individual as part of the comprehensive assessment, or on-going recovery care planning process, and agreed goals that include specific specialised employment support actions by the treatment service, and/or active referral to an agency for specialist employment support. Where the individual is already a claimant with Jobcentre Plus or the Work Programme, the referral can include a three way meeting with the relevant advisor to discuss education/employment/training (ETE) needs. The referral can also be made directly to an ETE provider34 Staff in commissioned treatment services should be able to recognise the typical barriers to employment experienced by the client group and how these may be overcome by35 Recognising, appropriately referring and supporting individuals with substance misuse problems into JobCentre Plus using the joint working protocol 36 Understanding the vital role that employment plays in the clients recovery journey Understanding the vital role that JCP and the Work Programme play in supporting treatment and recovery (and vice versa) Knowledge and understanding of the local champions and contacts are across the agencies and their respective roles Knowledge and understanding of the operational protocols and client pathways for shared clients Staff in commissioned treatment services should have an awareness of the support available to clients under this heading37and be able to signpost and/or refer clients as appropriate 34 Dataset J, November 2012 Employment and Recovery, A good practice guide – (NTA, 2012) 36 Joint working protocol between Jobcentre Plus and Treatment Providers ( NTA, 2010) 37 Appendix 4, page 68 35 45 B8. Education and training support The worker has assessed the education and training related needs of the individual as part of the comprehensive assessment, or ongoing recovery care planning process and agreed goals that include specific specialised education & training support actions by the treatment service, and/or active referral to an agency for specialist education & training support. Where the individual is already a claimant with Jobcentre Plus or the Work Programme, the referral can include a 3 way meeting with the relevant advisor to discuss ETE needs. The referral can also be made directly to an ETE provider This is part of the ongoing welfare reforms38 and links to employment support Staff in commissioned services should be aware of the support available under this heading39 and be able to signpost and/or refer clients as appropriate Staff in commissioned treatment services should be able to recognise the typical barriers to education and training support experienced by the client group and how these may be overcome by Recognising, appropriately referring and supporting individuals with substance misuse problems into education and training support Understanding the vital role that education, training and support plays in the clients recovery journey Understanding the vital role that education and training support providers play in supporting treatment and recovery (and vice versa) Knowledge and understanding of local education and training support provision and contacts within that provision Staff in commissioned treatment services should have an awareness of the support available to clients under this heading40and be able to signpost and/or refer clients as appropriate 38 http://www.dwp.gov.uk/policy/welfare-reform/get-britain-working/ 39 Appendix 4, page 68 Appendix 4, page 68 40 46 B9. Supported work projects Dataset J definition: The worker has assessed the employment related needs of the individual as part of the comprehensive assessment, or ongoing recovery care planning process and agreed goals that include the referral to one of the following: a service providing appropriate paid employment positions where the employee receives significant on-going support to attend and perform duties; or an appropriate volunteer placement, including active referral to an agency which provides specialist support to find volunteer placements. Staff in commissioned services should be aware of those services providing appropriate paid employment positions where the employee receives significant ongoing support to attend and perform duties and where to refer clients to in order to find a volunteer placement and be able to signpost and/or refer clients as appropriate Staff in commissioned treatment services should be able to recognise the typical barriers to education and training support experienced by the client group and how these may be overcome by Recognising, appropriately referring and supporting individuals with substance misuse problems into supported work projects Understanding the vital role that supported work and volunteering plays in the clients recovery journey Understanding the supported work projects and agencies supporting volunteer placements play in supporting treatment and recovery (and vice versa) Knowledge and understanding of local supported work projects and agencies providing specialist support to find volunteer placements and the contacts within that provision Staff in commissioned treatment services should have an awareness of the support available to clients under this heading4142and be able to signpost and/or refer clients as appropriate. 41 42 Appendix 4, page 68 http://www.volunteercentrenewcastle.org.uk/index.php 47 B10. Recovery Check Ups Dataset J definitions: Following successful completion of formal substance misuse treatment there is an agreement for periodic contact between a service provider and the former participant in the structured treatment phase of support. The periodic contact is initiated by the service, and comprises a structured check-up on recovery progress and maintenance, checks for signs of lapses, sign posting to any appropriate further recovery services, and in the case of relapse (or marked risk of relapse) facilitates a prompt return to treatment services43 Recovery management check-ups should be provided as follows44 Regular phone calls to (or other contact with) people who have left structured treatment. At least once a quarter when someone has first left treatment and then no less than once a year for up to five years. (The duration and intensity of checkups for a particular individual will be based on their problem severity and recovery capital). AND should include the following 43 44 Assessment of how the person’s recovery is progressing Provision of feedback and support Provision of rapid access back into structured treatment, if needed (rapid reentry option) Dataset J, November 2012 Medications in Recovery, Re-orientating drug dependence treatment: Strang (2012) 48 B11. Behavioural based relapse prevention Dataset J definition: Evidence based psychosocial interventions [as described in Section 4. Psychosocial] that support on-going relapse prevention and recovery, delivered following successful completion of the formal phase of structured substance misuse treatment. These are interventions with a specific substance misuse focus and delivered within substance misuse services45 Actions should be in accordance with those detailed under psychosocial interventions 45 Dataset J, November 2012 49 B12. Evidence based mental health focused psychosocial interventions Dataset J definition: Evidence-based psychosocial interventions for common mental health problems [as described in Section 4. Psychosocial] that support continued recovery by focusing on improving psychological well-being that might otherwise increase the likelihood of relapse to substance use. These are delivered following successful completion of the formal phase of structured substance misuse treatment and may be delivered by services outside the substance misuse treatment system following an identification of need for further psychological treatment and a referral by substance misuse services 46. As detailed under psychosocial interventions 46 Dataset J, November 2012 50 B13. Complementary therapies as defined by Dataset J Complementary therapies aimed at promoting and maintaining change to substance use, for example through the use of therapies such as acupuncture and reflexology that are provided in the context of substance misuse specific recovery support 47 . B13.1 Acupuncture Staff in commissioned drug treatment services delivering this intervention should be members of the British Acupuncture Council (BAcC) BAcC members have completed a first-degree-level training or equivalent in traditional acupuncture including substantial elements of western anatomy, physiology and pathology ; will record all relevant details of clients health condition and their medical history before treatment commences; uses only pre-sterilised single-use needles which are safely disposed of after treatment; carries out treatment in accordance with exemplary professional standards developed by the British Acupuncture Council and detailed in the BAcC Codes of Safe Practice and of Professional Conduct; uses a treatment room and equipment (all) that conforms to standards laid out in the BAcC Code of Safe Practice and (in nearly all cases) has also been approved by local authority environmental health officers; has full medical malpractice and public/product liability insurance cover. B13.1.1 47 48 Competences for acupuncture (cross references with NHS Key skills framework) as defined by Skills for Health48, the sector skills council for health CH Ac1 Evaluate and process requests for acupuncture CH Ac3 Assess the client for acupuncture CH Ac4 Agree action with the client (Acupuncture) CH Ac5 Formulate the acupuncture treatment plan CH Ac6 Provide the acupuncture treatment CH Ac7 Advise the client on acupuncture related self care strategies CH Ac8 Evaluate the effectiveness of the acupuncture treatment and self care CH Ac9 Review the acupuncture and evaluate the care Dataset J, November 2012 www.skillsforhealth.org.uk/ 51 B13.2 Reiki Staff in commissioned drug treatment services, practising this therapy should be members of one of the regulatory bodies of this discipline. There are currently two Regulatory Bodies soliciting membership by practitioners of Reiki and other complementary therapies in the UK, the Complementary and Natural Healthcare Council and the UK Reiki Federation49 .Registrants will have to be insured and sign up to a CPD Policy (continuing professional development), disciplinary procedures and code of professional conduct and ethics. B13.2.1 Competences for Reiki as defined by Skills for Health50, the sector skills council for health CNH1 Explore and establish the clients needs for complementary and natural healthcare CNH2 Develop and agree plans for complementary and natural healthcare with clients CNH12 Provide Reiki to clients B13.3 Reflexology Staff in commissioned drug treatment services practising this therapy should be working to the nationally agreed standard and ensure that their practice reflects up to date information and policies B13.3.1 Competences for Reflexology as defined by Skills for Health51 , the sector skills council for health CNH11 Provide Reflexology to clients Users of this standard will need to ensure that practice reflects up to date information and policies. There is currently no legal regulation of reflexology in the UK. 49 http://www.reikifed.co.uk/reiki-regulation/regulatory-bodies www.skillsforhealth.org.uk/ 51 www.skillsforhealth.org.uk/ 50 52 B13.4 Yoga Staff in commissioned drug treatment services or staff commissioned to deliver this intervention should be registered with the Yoga Alliance UK52 whose aim is to maintain a register of teachers, trainers and schools and to set standards for yoga in the UK. B13.4.1 Competences for Yoga as defined by Skills for Health53 , the sector skills council for health CNH 14 Deliver Yoga Therapy to clients Users of this standard will need to ensure that practice reflects up to date information and policies. 52 http://www.yogaalliance.co.uk 53 www.skillsforhealth.org.uk/ 53 B14. Other Dataset J definition: A recognised recovery activity or support intended to promote and maintain a service user’s recovery capital, that is not captured by an individual, or combination of, categories above Competence will be dependent upon the specific intervention being delivered. 54 Section C Pharmacological intervention 55 C1. Prescribing Doctors, dentists and a defined range of other healthcare professionals (referred to collectively as non-medical prescribers) are able to prescribe. C1.1 Non medical prescribing Prescribing by specially trained nursed, optometrists, pharmacists, physiotherapists, podiatrists and radiographers, working within their clinical competence as either independent and/or supplementary prescribers C1.2 Independent prescribing Independent prescribing is prescribing by a practitioner, who is responsible and accountable for the assessment of patients with undiagnosed or diagnosed conditions and for decisions about the clinical management required, including prescribing. In practice, there are TWO distinct forms of non-medical independent prescriber. i) An independent prescriber may currently be a specially trained nurse, pharmacist or optometrist who can prescribe any licensed medicine within their clinical competence. Nurse and pharmacist independent prescribers can also prescribe unlicensed medicines and controlled drugs. ii) A community practitioner nurse prescriber (CPNP), for example district nurse, health visitor or school nurse, can independently prescribe from a limited formulary called the Nurse Prescribers’ Formulary for Community Practitioners, which can be found in the British National Formulary (BNF). C1.3 Supplementary prescribing Supplementary prescribing is a voluntary partnership between a doctor or dentist and a supplementary prescriber to prescribe within an agreed patient-specific clinical management plan (CMP) with the patient’s agreement. Nurses, optometrists, pharmacists, physiotherapists, podiatrists and radiographers may currently train as supplementary prescribers and once qualified may prescribe any medicine within their clinical competence, according to the CMP. C1.4 The regulators of non-medical prescribers Professional regulators are required to set standards of education, training, conduct and performance and approve education programmes that prepare healthcare professionals to prescribe. They record the qualification of prescriber on their register. The regulators are: Nursing and Midwifery Council (for nurses and midwives) General Pharmaceutical Council (for pharmacists) General Optical Council (for optometrists) Health Professions Council (for physiotherapists, podiatrists and radiographers) 56 All prescribing should be in line with the ‘single competency framework for all prescribers’ 54which underpins a prescribers personal responsibility for prescribing. It can also be used by any prescriber at any point in their career as well as by others to inform standards, develop education and inform guidance and advice. The single competency framework has three domains, each containing three dimensions of competency (nine in total). 54 NHS National Prescribing Centre (May 2012) 57 C2. The Prescribing Competency Framework The prescribing competency framework (below) has three domains, each containing three dimensions of competency (nine in total). Within the nine competency dimensions are statements describing the activities or outcomes prescribers should be able to demonstrate. C2.1 Domain A: The consultation C2.1.1 Competency 1: Knowledge Has up-to-date clinical, pharmacological and pharmaceutical knowledge relevant to own area of practice C2.1.2 Competency 2: Options Makes or reviews a diagnosis, generates management options for the patient and follows up management 58 C2.1.3 Competency 3: Shared decision making (with parents, caregivers or advocates where appropriate) Establishes a relationship based on trust and mutual respect. Recognises patients as partners in the consultation The statements underpinning each competency are tabled at Appendix 5 55 C2.2 Domain B: Prescribing Effectively C2.2.1 Competency 4: Safe Is aware of own limitations. Does not compromise patient safety C2.2.2 Competency 5: Professional Ensures prescribing practice is consistent with scope of practice, organisational, professional and regulatory standards, guidance and codes of conduct C2.2.3 Competency 6: Always improving Actively participates in the review and development of prescribing practice to optimise patient outcomes The statements underpinning each competency are tabled at Appendix 6 56 C2.3 Domain C: Prescribing in context C2.3.1 Competency 7: The healthcare system Understands and works within local and national policies, processes and systems that impact on prescribing practice. Sees how own prescribing impacts on the wider healthcare community C2.3.2 Competency 8: Information Knows how to access relevant information. Can use and apply information in practice C2.3.3 Competency 9: Self and others Works in partnership with colleagues for the benefit of patients. Is self aware and confident in own ability as a prescriber. The statements underpinning each competency are tabled at Appendix 7 57 C2.4 Competencies for supplementary prescribers 55 Appendix 5, page 72 Appendix 6, page 74 57 Appendix 7, page 75 56 59 Supplementary prescribers require the same common competencies as independent prescribers to ensure safe and effective prescribing within the scope of their practice. The competencies for supplementary prescribers are the same as those of independent prescribers however there are several modifications and additions that reflect the unique nature of a supplementary prescribing relationship. The modifications to the competency framework are tabled at Appendix 858 58 Appendix 8, page 76 60 C3. Competencies for doctors The Royal College of Psychiatrists and Royal College of General Practitioners have published guide CR173 for commissioners, providers and clinicians 59 which defines three levels of competency for doctors working with drug and alcohol users and the training those at each level need to undertake. They define the three levels as specialist doctor, intermediate doctor and generalist doctor C3.1 Specialist doctors(3) C3.1.1 Supporting people to recover Specialist doctors will be able to work with people with the most severe and complex needs. Working with them and with other doctors and professionals, they will be able to lead on planning and delivering support and medical treatment towards their recovery. Examples of particular roles include: C3.1.2 providing expert advice to other doctors on diagnosis, assessment and recovery care planning, for example on complex drug interactions, comorbid drug-related physical and mental health issues, and integration of psychosocial and medical treatment; accepting referrals of people with the most severe or complex needs; expert oversight of provision of psychosocial support, based on comprehensive knowledge of research evidence; leading introduction of innovative interventions to improve outcomes and quality of provision; complex prescribing, for example injectable opioid substitution treatments (which also requires a license for some treatments); providing liaison drug and alcohol services in acute medical and psychiatric settings and expert advice to courts; providing expert advice to accountable officers and responsible officers. Clinical leadership The clinical leadership of specialist drug and alcohol services, including inpatient facilities, is a key role for specialist doctors. They take responsibility for leading on all aspects of clinical governance and quality assurance in line with the requirements of the designated monitoring bodies, including clinical effectiveness and patient safety across services in their area. They act as advisors on commissioning and implementation of policy through their input into local structures. They also champion and lead research and innovation to develop new clinical guidance and service protocols, both at local and national level. They will be able to provide supervision, appraisal and training ‘Delivering quality care for drug and alcohol users: the roles and competencies for doctors’ (September, 2012) 59 61 to doctors at all levels of competency. C3.2 Intermediate doctors (2) C3.2.1 Supporting people to recover Intermediate-level doctors will be able to make a full assessment of strengths, risk, harm and urgency for people with more severe or complex needs, and to work with them to formulate, initiate and monitor medical care in support of their recovery goals. This includes both the delivery of psychosocial interventions and prescribing most pharmacological treatments, as well as advising on harm reduction. They will be able to work with people to help them address any mental health problems or other physical health issues, drawing on support and supervision from specialists as appropriate. They will be aware of local protocols on provision of care to people with a mental illness using drugs and alcohol, and will be able to ensure appropriate, coordinated care is provided by relevant services. C3.2.2 Clinical leadership Intermediate-level doctors will have the specialist expertise to be able to lead on aspects of clinical governance in drug and alcohol services, including clinical audit. They will be able to work in partnership with other agencies to ensure that there is a full range of recovery options available locally, including both abstinence-oriented and harm reduction interventions. They will be able to provide supervision and training to generalists, trainees and other healthcare professionals working in the field. They will be able to make a substantial contribution to service management, a substantial contribution to service management, including by advocating for service users and promoting their involvement. C3.3 Generalist doctors C3.3.1 Supporting people to recover All doctors supporting drug and alcohol users should be able to identify people whose use of drugs or alcohol may pose a risk to their own, or others’, health and well-being, including that of children, through safeguarding issues; make an assessment of their needs and risks; and correctly diagnose substance use disorders. They should be able to provide the person and their family/carers with advice and information to support and motivate them in pursuing recovery, referring them to more specialist services if necessary, as well as helping them manage their general mental and physical health in liaison with other professionals. They will be able to prescribe medication, including opioid substitution therapy, only in uncomplicated cases. 62 Psychiatrists working at generalist level will also be able to implement mental health legislation, and to lead on supporting their own patients who are using drugs or alcohol and also have a mental illness, referring to more specialist help when needed. C3.3.2 Clinical leadership Generalists will not usually be in a position to lead drug and alcohol services, although all doctors are expected to participate actively in clinical governance activities – for example, GPs participating in an annual audit of uptake of vaccinations for blood-borne viruses. C3.4 Competences There are three levels of competency for doctors working with people using drugs and alcohol at Generalist, Intermediate and Specialist levels60. These are tabled at Appendix 9 61 C3.5 Training C3.5.1 Specialist doctors All doctors working at specialist level should either: be listed on the GMC’s Specialist Register as a psychiatrist with an endorsement in substance misuse psychiatry, with the supervision and CPD requirements this entails; or have training, experience and supervision equivalent to this, as certified by the GMC through an appropriate Certificate of Eligibility for Specialist Registration (CESR; for details of CESR for psychiatrists or be listed on the GMC’s GP Register and have the following additional training and experience: all the RCGP certificates listed earlier, or equivalent CPD approved by the RCGP SMAH unit; and if possible, a Masters degree or Diploma in addictions; and experience, evidenced in a logbook/portfolio, of front-line specialist work at a senior level and for a substantial length of time, including managing complex cases, working autonomously where necessary and in line with up-to-date best practice; and experience in: medicines management; strategic leadership and management of other clinical staff; supervision, mentorship and appraisal of others; clinical leadership and professional standards; integrated and multi-agency working; local policy and guideline development, audit, risk and incident review and ‘Delivering quality care for drug and alcohol users: the roles and competencies of doctors’, pp. 2224 available at www.rcpsych.ac.uk 60 61 Appendix 9, page 77 63 appropriate ongoing CPD relevant to this field. C3.5.2 Intermediate doctors All doctors working at intermediate level should either: be listed as a GP on the GMC’s GP Register, and have completed the RCGP certificates in Harm Reduction, Health Recovery and Well Being, the Management of Drug Misuse, both Parts 1 and 2; and the RCGP Certificate in the Management of Alcohol Problems in Primary Care; and undertake a specialist peer-led appraisal at least every 2 years to supplement their annual appraisal as a GP; and undertake relevant annual CPD; or be listed on the GMC’s Specialist Register as a psychiatrist (but not necessarily with an endorsement in substance misuse), with the CPD and supervision requirements this entails; and have extensive experience of working with people using substances under the supervision of a consultant addictions psychiatrist. C3.5.3. Generalist doctors The various medical Royal Colleges and Faculties require different competencies of doctors training in their respective specialties. Colleges also provide various CPD opportunities – for example, the RCGP encourages all GPs to complete its certificates in harm reduction, alcohol management and drug use (Part 1). A project sponsored by the Academy of Medical Royal Colleges has identified a set of basic, core competencies for all doctors in supporting people using drugs and alcohol at generalist level, and these are now being embedded into the postgraduate curricula of the medical Royal Colleges62 This will help ensure that every opportunity is taken to provide people with information and motivation to pursue recovery, and reduce the risks of medical complications which can arise from a lack of recognition of patients’ drug and alcohol use. 62 Academy of Medical Royal Colleges & Royal College of Psychiatrists, 2012. 64 Appendices 65 Appendix 1: Competences to deliver cognitive and behavioural based relapse prevention interventions (substance misuse focused) 66 Appendix 2: Competences needed to relate to people and to carry out any form of psychological intervention 67 Appendix 3: Parenting support programmes in Newcastle Strengthening Families This programme is available via Byker Sands family centre and sees parents/carers working both separately and together focusing on; building nurturing skills, placing boundaries, reinforcing messages that all behaviour has consequences, developing positive relationships, enabling communication, supporting young people in developing skills to enable them to cope with stress and peer pressure Incredible Years School Age Incredible Years is available via Byker Sands family centre and supports the development of positive and nurturing parenting through; play praise effective limit setting use of ignoring and time out strategies The Parent Factor in ADHD The Parent Factor programme is for parents / carers who have a school aged child who has been diagnosed with Attention Deficit Hyperactive Disorder. It focuses on the specific parenting skills and knowledge that are required within this context. The programme has four main aims: To increase parents knowledge of ADHD and its treatment To give parents insight into how it feels to be a child with ADHD To give parents advice on how to promote a more positive relationship with their child To educate parents on strategies for effective behaviour management Triple P Triple P is a parenting and family support strategy that aims to prevent severe behavioural, emotional and developmental problems in children by enhancing the 68 knowledge, skills and confidence of parents. This programme incorporates sessions on causes of children’s behaviour problems, strategies for encouraging children’s development and strategies for managing misbehaviour. Active skills training methods used in the sessions include modelling, rehearsal, self-evaluation, and homework tasks. Several generalisation enhancement strategies are incorporated into the program to promote the transfer of parenting skills across settings, siblings and time. 69 Appendix 4: Entry to Education and Employment support The Work Programme Up to two years of tailored in and out of work support designed to help people into paid employment. Delivered by private companies, charities and the public sector. Providers have the freedom to include the services they feel will be most effective – this can include training, mentoring, work placements, supported job search etc. This is for people aged 18 and above who have been unemployed for 9-12 months or more, and most people on Employment Support Allowance (ESA) / Incapacity Benefit (IB). People facing serious disadvantage in the job market, including homeless people, people with histories of substance use and mild to moderate mental health problems can opt to join at the discretion of their Jobcentre Plus adviser after 3 months. Joining is mandatory for people on Job Seekers Allowance (JSA), and for people on ESA other than in the Support Group. Once on the Programme, continued participation is always mandatory and the provider can require customers to carry out mandatory tasks and activities and referral is by Jobcentre Plus only. The Youth Contract 18-24 This is a series of incentives and improved offers, rather than a stand-alone programme. Employers have a wage incentive of £2,275 for each person recruited from the Work Programme and staying in the job for at least 6 months. It also includes additional apprenticeship places, incentive payments for small and medium enterprises (SMEs) recruiting apprentices, additional Sector Based Work Academy and Work Experience places. This is for unemployed people aged 18-24 and referral is through a JobCentre Plus adviser Supported work projects The worker has assessed the employment related needs of the individual as part of the comprehensive assessment, or ongoing recovery care planning process and agreed goals that include the referral to one of the following: a service providing appropriate paid employment positions where the employee receives significant ongoing support to attend and perform duties; or an appropriate volunteer placement, including active referral to an agency which provides specialist support to find volunteer placements. Links to employment support/education and training support63 Staff in commissioned services should be aware of the following and be able to signpost and refer clients as appropriate using the joint working protocol64 Day One Prison Release 63 http://www.dwp.gov.uk/policy/welfare-reform/get-britain-working/ 64 Joint working protocol between Jobcentre Plus and Treatment Providers ( NTA, 2010) 70 Immediate access to the Work Programme, rather than at 3, 9 or 12 months. People released from a custodial sentence who make a claim for JSA will be mandated to the Work Programme immediately. Jobcentre Plus staff will be processing any claims prior to release. People who do not claim JSA before leaving prison but who do so within 13 weeks of leaving will also be mandated to the Work Programme. It is mandatory and the referral route is through Jobcentre Plus advisers, either in prison or following release.. New Enterprise Allowance Support for unemployed people to become self-employed. Consists of business advice and support, an interest-bearing loan of up to £1000 and a tapered allowance of £1274 over 6 months to help the transition to self-sufficiency. This is for people who have been claiming JSA for 6 months or longer. People who are on, or who are required to be on the Work Programme are ineligible. It is voluntary and the referral route is through JobCentre Plus advisers Work Choice 6-9 months of pre-employment support, plus longer-term in-work support. The Programme is designed to support people with disabilities into paid employment. Delivered by private companies, and the voluntary and public sectors, includes elements such as vocational training, CV building, job brokerage. This is for Disabled people with complex employment support needs for whom other DWP provision is not suitable and those who are in work but under threat of losing their job as a result of their disability. It is not mandatory and the referral route is through JobCentre Plus Disability Employment Advisers, voluntary sector organisations with Statutory Referral Organisation status, Work Programme providers. Voluntary Work Experience Up to 8 weeks unpaid work experience, expenses are met. Placement can be with private, voluntary or public sector organisations. Administered by Jobcentre Plus. This is for people aged 16 – 24 who have been unemployed for between 3 and 9 months. It is voluntary to join, continued participation is now voluntary as well, although a sanction may be applied if someone is asked to leave for gross misconduct. The referral route is through Jobcentre Plus advisers Mandatory Work Activity Up to 4 weeks of unpaid work, designed to instil the habits and routines of working life. The activity is being delivered by organisations from the private, voluntary and public sectors, and the work has to be of benefit to the community. This is for people on JSA, any age, at the discretion of Jobcentre Plus adviser. It is mandatory and ‘customers’ who fail to complete a placement without good cause will lose their Jobseeker’s Allowance for a minimum of 3 months. The referral route is through 71 Jobcentre Plus advisers Sector Based Work Academy Mix of pre-employment training and a work placement of up to 6 weeks, followed by a guaranteed interview. Whilst the interview is guaranteed, there is no requirement to have a job vacancy. Any external training is fully funded through the Skills Funding Agency and delivered by Further Education colleges and training providers. The training is QCF accredited. This is for people aged 18 or over claiming JSA or in the Employment Support Allowance/Work Related Activity Group (ESA WRAG group). It is voluntary to join, but there is a risk of sanction if the ‘customer’ leaves. The referral route is through Jobcentre Plus advisers. Work Trial Work Trial is a trial in an actual job vacancy that gives an opportunity for an employer to see how someone gets on in a post, and allows a jobseeker to show an employer that they are the right person to fill it. Benefits and expenses will be paid for the duration of the trial, which will generally not be longer than 15 working days. You may be able to arrange your own Work Trial with an employer, subject to your Jobcentre Plus adviser agreeing. Generally, this is for people on JSA for more than 6 months, but anyone interested is encouraged to discuss with their Jobcentre Plus adviser who will tell them if they are eligible or not. It is not mandatory and the referral route is through Jobcentre Plus advisers Employment on Trial A prior agreement with Jobcentre Plus that a customer leaving a new job of more than 16hrs per week between 4 and 12 weeks after starting will remain eligible for JSA, reducing the risk for people prepared to try out a new job but concerned about how it will work out. Generally, this is for people who have been unemployed for more than 13 weeks, but anyone interested is encouraged to talk to their Jobcentre Plus adviser who will tell them if they are eligible or not. It is not mandatory and the referral route is by prior agreement with Jobcentre Plus adviser Work together Jobcentre Plus aims, where appropriate, to encourage and support people into volunteering opportunities when doing so will help the individual to improve their skills, CV, confidence, gain references and so on. Anyone can be a volunteer, but anyone interested should speak to their Jobcentre Plus adviser who can provide advice and support as well as making sure that they are still available for work and that their welfare benefits are not at risk. It is not mandatory. Community Action Programme (currently under pilot) Up to 30 hours of unpaid work per week for up to 26 weeks. The work would normally be for community benefit and is likely to be with a local authority, charity or 72 social enterprise. Concurrent with the placement there will be provider-led job search and potential additional support of up to 10 hours per week. This is for the very longterm unemployed; typically people who have been through the Work Programme without finding employment and have thus been unemployed for a minimum of 2 years. It is mandatory and the referral route is through JobCentre Plus Newcastle Futures65 Newcastle Futures are able to support Newcastle residents of working age, not in employment (or those in employment of 15 hours or less). Refugees must have leave to remain or indefinite leave to remain and migrants must be in receipt of a benefit. We are not able to help customers who do not have access to public funds. All residents must be unemployed AND match one of the below criteria AND live within the Newcastle City Council boundaries: Criteria Newcastle residents of a specific postcode area* Lone Parent (with dependant child/children aged 16 years or under) Workless Families (supporting dependant child/children aged 16 years or under) Aged 16 to 24 Sickness Benefit (Incapacity and ESA) Claimant * To find out if your client lives in an area which is covered by the services or for information about outreach venues across the city of Newcastle, contact: Lesley Widdowson Newcastle Futures 1 Cathedral Square Cloth Market Newcastle NE1 1EE T: 0800 587 0478 (Freephone) E: info@newcastlefutures.co.uk 65 http://www.newcastlefutures.co.uk/ 73 Appendix 5: The prescribing competency framework Domain A: The consultation 74 75 Appendix 6: The prescribing competency framework Domain B: Prescribing Effectively 76 Appendix 7: The prescribing competency framework Domain C: Prescribing in context 77 Appendix 8: Competencies for supplementary prescribers 78 Appendix 9: The three levels of competency for doctors working with people using drugs and alcohol 1: 2: 3: Generalist Intermediate Specialist 1 2 3 Provide information and advice on harms and risks to people using drugs and alcohol, their families and carers X X x Work to reduce stigma faced by people who use drugs or alcohol X X X Provide advice on medical interventions and treatment to people using drugs and alcohol in support of their recovery needs and goals, and to reduce harm as appropriate X X Develop educational materials on drug and alcohol use to support prevention and recovery X X X X X X Supporting people to recover Advice and Information Identification and diagnosis Correctly identify people using drugs and alcohol and diagnose substance use disorders Provide support and advice to generalist doctors on identification of substance use disorders and appropriate referral pathways Provide support and advice to intermediate and generalist doctors on appropriate identification and diagnostic tools and strategies X X 79 Assessment and Recovery Care Planning 1 2 3 Carry out basic assessment of drug and alcohol use, associated strengths, harms, risks, urgency, and need for referral to more specialist services X X X Carry out risk assessment of suicide and harm to others, and assessment of psychiatric comorbidity, and need for further medical treatment and/or onward referral X X X Carry out comprehensive assessment of drug and alcohol use, associated strengths, harms, risks, urgency, and need for referral to more specialist service X X Work with people with less severe or complex needs to devise and initiate recovery care plan in collaboration with other professionals as appropriate X X Carry out comprehensive assessment of people with more severe or complex needs using drugs or alcohol, including strengths, risks, comorbidities, and need for interventions X Advise intermediate and generalist doctors on assessment and recovery care planning X Work with people with the most severe or complex needs to devise and initiate a recovery care plan, drawing on the full range of treatment models and settings, in collaboration with other professionals as appropriate X Providing support, care and medical treatment Support people using or recovering from drugs or alcohol use in caring for their general mental and physical health and well-being X X X Liaise with relevant professionals (including social care, criminal justice, housing, medical, psychiatric, employment professionals) Provide appropriate management of assisted withdrawal where facilities allow X X X 80 Providing support, care and medical treatment 1 2 3 Provide appropriate management of assisted withdrawal where facilities allow X X X Implement relevant mental health legislation for drug and alcohol users and lead on supporting people with more complex psychiatric comorbidity (psychiatrists only) X X X Provide appropriate support and interventions for families and carers of people using or recovering from drugs or alcohol use X X X Prescribe appropriately for people using or recovering from drugs or alcohol, including opioid substitute prescribing and provision of medications to prevent relapse X X X Address health needs and comorbidities of drug or alcohol users with more severe or complex needs, in collaboration with other professionals X X Arrange or provide appropriate psychosocial interventions for people using or recovering from drugs or alcohol X X Carry out, with the person receiving support, regular review of recovery care plans X X Lead on provision of support and medical treatment for people with the most severe and complex needs X Appropriately prescribe injectable opioid substitution treatments (if licensed) and other complex prescribing (e.g. innovative or off-label uses of medicines) X Provide liaison drug and alcohol services in acute medical and psychiatric settings X Provide expert, specialised support for vulnerable groups of drug and alcohol users, such as young people, homeless people and pregnant women X X 81 Providing support, care and medical treatment 1 2 Provide specialist interventions for new emerging drugs of misuse 3 X Clinical Leadership Clinical Governance and innovation Be aware of research and clinical guidelines on drugs and alcohol relevant to clinical role X X X Participate in research and clinical governance activities, including clinical audit X X X X X Lead on aspects of clinical governance, including clinical audit Provide leadership on all aspects of clinical governance, and take responsibility for ensuring they comply with various national standards X Lead on development of local clinical guidelines and protocols and contribute to national initiatives X Lead research and innovation in treating substance use disorders and supporting drug and alcohol users, to improve services and care X Supervision, appraisal and training Provide general training in treating substance use disorders and supporting people using drug and alcohol to generalist doctors and other staff X X 82 Supervision, appraisal and training 1 2 3 Provide training for medical undergraduates and postgraduates in treating substance use disorders and supporting people using drug and alcohol X X Provide training and supervision for medical trainees and staff in other disciplines66 in treating substance use disorders and supporting people using drugs and alcohol X X Supervision, support, training and advice to keyworkers on delivery of psychosocial interventions X Provide support, advice, supervision, mentoring and appraisal to intermediate and generalist doctors in treating substance use disorders and supporting people using drugs and alcohol X Provide supervision for non-medical prescribers X X Advise responsible officers on competency issues arising for doctors working with people using drugs and alcohol in the context of revalidation X Advise accountable officers on appropriate uses of relevant controlled drugs X Carry out specialist assessment of fitness to practise for the General Medical Council and other professional organisations, and expert assessment of people using drugs and alcohol in childcare or criminal proceedings X 66 Postgraduate medical training is subject to specific requirements relating to trainers, for example psychiatry trainees must be supervised by an appropriately qualified trainer in psychiatry 83 Service Development 1 2 3 Support service provision and development locally X X X Contribute to service management locally X X Champion service user involvement and provide advocacy for service users X X Manage specialist in-patient services for people using drugs or alcohol X Provide expert clinical advice on drug and alcohol use to commissioners and providers regarding appropriate service provision and development in line with research and national guidance X Provide expert clinical advice and advocacy on drug and alcohol matters to policy makers nationally X Support medical workforce development locally and nationally X 84