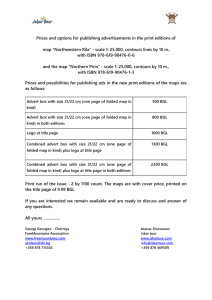
table width="0" cellpadding="0" cellspacing="0" border="0"
advertisement

INVESTIGATION MEMORANDUM Office of Inspector General, Licensing Division Public Information Minnesota Statutes, section 626.557, subdivision 1 states, “The legislature declares that the public policy of this state is to protect adults who, because of physical or mental disability or dependency on institutional services, are particularly vulnerable to maltreatment.” Re Dat por e t Iss Nu ued mb : er: Sep 201 tem 541 ber 33 11, 201 5 Na Dis me pos anditio Ad n: dre Inc ss onc of lusi Fac ve ilit y Inv esti gat ed: Inte grit y Liv ing Opt ion s 108 01 Mis siss ippi Blv d. N W Co on Rap ids, MN 554 33 Integrity Living Options Report 20154133 Page 2 Inte grit y Liv ing Opt ion s, Inc. 112 1 Jac kso n St. NE Ste. 100 Mi nne apo lis, MN 554 13 License Number and Program Type: 1072687-H_CRS (Home and Community Based Services-Community Residential Setting) 1072676-HCBS (Home and Community-Based Services) Investigator(s): Mindy Fleming Minnesota Department of Human Services Office of Inspector General Licensing Division PO Box 64242 Saint Paul, Minnesota 55164-0242 Suspected Maltreatment Reported: It was reported that when emergency medical services were called for a vulnerable adult (VA), a facility staff person (P1) was unable to provide paramedics with the VA’s medical history. It was also reported that the VA was unkempt, and was wearing a month old hospital bracelet. Date of Incident(s): July 3, 2015 Nature of Alleged Maltreatment Pursuant to Minnesota Statutes, section 626.557, subdivision 9c, Integrity Living Options Report 20154133 Page 3 paragraph (b), and Minnesota Statutes, section 626.5572, subdivision 15, and subdivision 17, paragraph (a): The failure or omission by a caregiver to supply a vulnerable adult with care or services, including but not limited to food, clothing, shelter, health care, or supervision which is reasonable and necessary to obtain or maintain the vulnerable adult's physical or mental health or safety, considering the physical and mental capacity or dysfunction of the vulnerable adult and which is not the result of an accident or therapeutic conduct. Summary of Findings: Pertinent information was obtained during a site visit conducted on August 10, 2015; from documentation at the facility, the VA’s day program, and medical records; and through five interviews conducted with community providers (CP1-CP2) and facility staff persons (P1-P3). The VA’s diagnoses included a brain injury due to encephalopathy and type I diabetes. The VA’s blood glucose levels (BGL) could be “erratic,” and the VA did not always follow his/her recommended diabetic diet. The VA’s Coordinated Service and Support Plan (CSSP) stated that the VA required assistance monitoring his/her blood glucose levels and insulin regimen. The VA was also monitored by his/her primary care physician, psychiatrist, endocrinologist, and neurologist. The VA’s Individual Services and Supports Plan (ISSP) stated that the VA had a history of hospitalizations due to his/her fluctuating BGLs. The VA was in a diabetic coma in 2005 and was placed on life support, but recovered. In May 2015, the VA had a choking incident and required cardio pulmonary resuscitation (CPR). Following that incident, the VA experienced continued difficulty swallowing and “drastic” weight loss. The VA was admitted to the hospital and a feeding tube was placed. The VA no longer ate solid food, and communicated through “grunts” and shaking his/her head. The VA was his/her own guardian. The VA was on a sliding scale insulin regimen (sliding scale refers to the progressive increase in the pre-meal or nighttime insulin dose, based on pre-defined blood glucose ranges). Staff persons were to check the VA’s BGL before meals and administer the appropriate dosage of insulin based on his/her current level. If the VA’s BGL was 450 milligrams per decilitre (mg/dL) or higher, staff persons were to call a physician. According to the VA’s documented routine cares, the VA could not use toothpaste or mouthwash due to his/her difficulty with swallowing. Staff persons were to assist the VA in dipping a toothbrush in water to clean his/her teeth and mouth twice daily. The facility’s General Event Report (GER) stated that on July 3, 2015, a staff person (determined to be P1) checked the VA’s BGL around 7 p.m. and it was 491 mg/dL. P1 “followed protocol and administered 10 units of Novolog and 7 units of Levimir.” P1 also administered 200 milliliters (ml) of water through the VA’s feeding tube. P1 called the physician’s office and spoke with the on-call nurse who directed P1 to call 9-1-1. When paramedics arrived and re-checked the VA’s BGL, it was 420 mg/dL. The paramedics were “concerned” because the VA’s glucometer was not showing the correct time and date, “but the readings [were] accurate.” The VA was transported to the emergency room. CP1 and an Allina Medical Transportation Prehospital Care Report provided the following information: Emergency medical services (EMS) arrived at the facility around 8 p.m. on July 3, 2015. Paramedics checked the VA’s BGL approximately 45 minutes after P1 administered his/her insulin and it was reduced to 420 mg/dL. P1 was unable to provide paramedics with a list of the VA’s recent BGLs “due to a change in record keeping.” Integrity Living Options Report 20154133 Page 4 The VA did not like to be touched and “growl[ed]” and pulled away from paramedics. CP1 stated that upon the VA’s arrival at the hospital, P1 was asked to provide information about the VA’s recent BGLs. P1 was unable to “access medical records” because s/he did not know how to use the new electronic documentation system the facility implemented. CP1 stated that when the VA arrived at the hospital, his/her face was “caked in feeding tube substance,” and s/he was wearing a hospital bracelet from May 2015. The VA also had “bloody drool” on his/her mouth. P1-P3 provided the following information: P1 stated that the VA only got “shakes” through his/her feeding tube and they should not make the VA’s BGL rise so high, but when P1 spoke with the on-call nurse at the VA’s endocrinology clinic, s/he stated that because the VA was a “fragile diabetic” his/her BGL could be “up and down like that.” P1 stated that when the paramedics asked to see the VA’s recent entries on the VA’s glucometer, it was not working because it needed a battery. When P1 replaced the battery, the glucometer displayed the VA’s recent BGLs but with the wrong date and time stamps. The facility’s medical professional attempted to fix the time and date problem on the glucometer the day before, but could not. Due to this, staff persons documented the date and time the VA’s BGL was checked, and the result in the VA’s electronic record. P1 was able to complete basic functions in the VA’s electronic documentation system, but was unable to “pull up” a report of the VA’s recent BGLs because the switch to the electronic documentation system was recent and this was the first time that P1 actually used it. P1 told paramedics that s/he would call the hospital to provide the information after s/he was able to access it. P1 called a supervisory staff person (P3) to find out how to access the information. P3 stated that s/he told P1 that the hospital would want information about the VA’s medical history and that P1 should call them. P1 was in “panic mode” so P3 decided to go to the facility. When P3 arrived s/he asked P1 if P1 called the hospital and P1 stated that s/he called but hung up because s/he was on hold too long. P3 stated that was “not okay” so s/he called the hospital and provided them with information. P3 felt s/he “cleared up a lot” of information for the hospital. When P3 checked the VA’s glucometer, P3 noticed that P1 had two different glucometers sitting out. P1 told P3 that s/he had two out because one was not working and needed a battery. P3 stated that the VA would sometimes “play” with the glucometer and take the batteries out and staff persons just needed to put the battery back in when using it. P3 also stated that a medical professional from the home health agency recently tried to correct the time and date issue on the glucometer but was unsuccessful so staff persons were documenting the information in the electronic record. P3 thought that P1 was unable to retrieve the VA’s medical history from the electronic record because P1 “panicked.” P2 and P3 each stated that staff persons were trained on how to use the new system, and P3 walked P1 through it again after the incident. P2 also thought that P1 “panicked” and did not remember how to “run the report.” P1 told the paramedics that s/he did not know how to get the VA’s information and “left it at that,” which is why the hospital was concerned. P2 stated that P1 was only employed at the facility for about one month when the incident occurred. P1 worked for the facility two years prior, but the VA’s condition changed “quite a bit” during that time and Integrity Living Options Report 20154133 Page 5 P1 was retrained to work with the VA. P1-P3 acknowledged that the VA had poor dental health. P3 stated that the VA was diagnosed with chronic periodontal disease. P2 stated that this was ongoing and began because the VA did not like to brush his/her teeth and when staff persons would try to assist him/her, s/he would have “major behaviors.” P2 stated that the VA’s dental health was an ongoing “struggle” and the VA’s team was aware of it. P1 and P3 provided consistent information that the VA saw a dentist, and that the VA had an appointment on August 4, 2015, to discuss having all of his/her teeth removed. The VA’s family members would make the final decision about the VA’s dental care. P1 stated that the VA struggled with drooling and was prescribed a medication to lessen the problem. P2 and P3 provided consistent information that the VA sometimes refused to change into clean clothes or shower. P2 stated additionally that staff persons prompted the VA to complete these tasks. P1 and P3 each acknowledged that the VA wore a hospital bracelet from his/her last admission over one month ago. P3 stated that s/he tried to cut it off or have the VA cut it off “15 times,” but the VA refused. P1 and P3 each stated that when they tried to remove the bracelet the VA yelled and became upset. CP2 provided the following information: CP2 stated that the VA used to attend day programming, but the VA was no longer able to attend because the staff persons at the day program could not provide the level of care that the VA needed to manage his/her issues with eating and BGL fluctuations. CP2 stated that day program staff persons had to make “a lot” of calls to 9-1-1 when the VA’s blood sugars “spiked” or “bottomed out.” The VA often had “drool” on his/her shirt and “bad breath.” CP2 stated that the VA did not like to be touched, and would not let staff persons assist him/her in cleaning up. The facility’s policies and procedures regarding Health Services Coordination stated that staff persons would assist with or coordinate medical, dental, and other health service appointments. All staff persons interviewed received training on the Reporting of Maltreatment of Vulnerable Adults Act prior to the incident. Conclusion: On July 3, 2015, P1 called 9-1-1 when the VA’s BGL was 491 mg/dL. When paramedics arrived, P1 was unable to provide them with the VA’s medical history because s/he did not know how to access the information on the facility’s new electronic documentation system. The VA’s glucometer also provided inaccurate information related to the dates and times that the VA’s BGLs were checked. When the VA arrived at the hospital, s/he appeared unkempt and had a month old hospital bracelet on. P1 and P3 each stated that the VA’s glucometer did not report accurate date and time stamps, but the BGLs stored in it were correct. P1 and P3 stated additionally that a medical professional attempted to fix the issue but could not, so staff persons alternatively documented the date, time, and result of all BGL checks in the VA’s electronic record. Although P2 and P3 each stated that P1 received training on the new electronic documentation system prior to the incident, P1 stated that the day of the incident was his/her first time using the system. P1 could not provide paramedics with the requested information, but told them that s/he would call the hospital with the information Integrity Living Options Report 20154133 Page 6 when s/he was able to access it. P1 called P3 for assistance and P3 ultimately provided the needed information to the hospital. Although P1 was unable to provide necessary medical information to emergency medical personnel during the incident and did not effectively communicate the reason s/he was unable, given that the information was provided by P3, that P1 did follow the facility’s protocol by consulting with a physician and obtaining emergency medical services for the VA, and that the delay in providing the information did not prevent the VA from receiving needed care, there was not a preponderance of the evidence whether there was a failure to provide the VA with care or services that were reasonable and necessary. P1-P3 acknowledged that the VA had poor dental health. P1 and P3 provided consistent information that the VA received dental care and that the VA and the VA’s family members were involved in making decisions about the VA’s treatment options. P1 stated that the VA struggled additionally with drooling and was prescribed a medication to lessen the problem. P2 and P3 provided consistent information that the VA sometimes refused to change into clean clothes or shower, but that staff persons prompted him/her to complete these tasks. P1 and P3 each acknowledged that the VA wore a hospital bracelet from his/her last admission over one month ago, but stated that the VA refused to take it off despite staff persons’ attempts. Given the above, there was not a preponderance of the evidence whether there was a failure to provide the VA with care or services that were reasonable and necessary. It was not determined whether neglect occurred (the failure or omission by a caregiver to supply a vulnerable adult with care or services, including but not limited to food, clothing, shelter, health care, or supervision which is reasonable and necessary to obtain or maintain the vulnerable adult's physical or mental health or safety, considering the physical and mental capacity or dysfunction of the vulnerable adult and which is not the result of an accident or therapeutic conduct). Action Taken by Facility: The facility completed an internal review and found that their policies and procedures were accurate and followed by staff persons. The facility determined that there was no need for corrective action. Action Taken by Department of Human Services, Office of Inspector General: During the course of the investigation it was determined that the facility did not comply with background study requirements. On September 11, 2015, the facility was issued a $200 fine for the background study violation. The Order to Forfeit a Fine is subject to appeal.