Cardio110-ExercisePhysI
advertisement

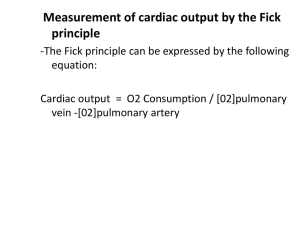
Cardio #110 Mon, 02/10/03, 9am Dr. Smith Jennifer Uxer for Milena Patel Page 1 of 4 Exercise Physiology I I. Introduction Dr. Smith will send out an e-mail with what we need to know for the respiration part of Friday’s exam. It will include acid-base, oxygen dissociation curve, oxygen transport, respiratory changes in intrathorasic pressure, especially in the valsalva maneuver. Review the content (i.e. contractilitiy, P – V loops) from last week’s exam. This week’s lectures are to give lots of applications. He’ll have additional practice questions. Take the previous practice questions (from last week) and put them into exercise scenarios. II. Challenges to Cardiovascular Function Why the body responds—control and distribution of cardiac output A. Increased need for delivery of oxygen—fundamental need Occurs where there’s increased metabolism. Profound vascular vasodilation at maximal exercise in skeletal muscle can cause a 90% decrease in vascular resistance. This is GREATER than the systemic resistance—ALWAYS. Regional resistance is still greater than systemic resistance (even at maximal exercise)! (Think resistances in parallel.) NOTE: All of what is discussed relates to Dynamic or endurance (Aerobic) forms of exercise. B. Redistribution of blood volume (Q) Coronary resistance drops; flow increases 2 – 3x at maximal exercise. Increase in generalized sympathetic activity during exercise. Vasodilation occurs because local metabolic activity overcomes the sympathetics. Skin—depends on the thermal load. At exercise onset, resistance is increased or not changed—no thermal load. Once there’s a thermal load, it’s decreased, and thus increased blood flow. Splanchnic and renal—resistance increases, flow decreases—no local control to override the sympathetics. Brain—no change Skeletal muscle—biggest increase in flow. If skeletal muscle accounted for 1 L/min of cardiac output at rest, then during exercise, 14L/min of the 15L/min increase in total cardiac output would go to the skeletal muscle. Tremendous decrease in vascular resistance and increase in blood flow. C. Heat dissipation III. Responses to Exercise A. Oxygen Cardio #110 Mon, 02/10/03, 9am Dr. Smith Jennifer Uxer for Milena Patel Page 2 of 4 1. VO2 = Oxygen consumption of the whole body = oxygen uptake = cardiac output * oxygen extraction 2. Oxygen extraction = A – V O2 difference If oxygen extraction = 0, then AO2 = V O2. No oxygen is consumed. Can have situations with high cardiac output and low O2 extraction. Increase in both O2 extraction and cardiac output in exercise. 3. VO2max = Qmax * A – V O2 difference max Everyone has a maximal O2 consumption--#1 definer of your fitness level. As work increases, O2 consumption will plateau at some point. Increasing the workload further will NOT increase O2 consumption. Anaerobic metabolism helps out at this point to allow you to exercise a little harder. VO2 isn’t measured clinically. Workload is measured because there’s a linear relationship between the 2 until the maximum point. B. Cardiac Output Same principle as oxygen uptake response. There’s a linear relationship between workload and cardiac activity until a max workload where cardiac output plateaus. CO tends to be main limiting factor of VO2max in a normal, healthy individual. Because the CO plateaus, lungs are not suggested as the limiting factor. More about this later. Related to Oxygen Consumption—as plot CO vs O2 consumption, you reach a max O2 consumption. There’s a linear relationship between the 2 and both achieve a maximum (no plateau relative to each other). C. Venous Return There’s a linear relationship between workload and venous return until a max workload where venous return plateaus. Related to Oxygen Consumption—as plot VR vs O2 consumption, you reach a max O2 consumption. There’s a linear relationship between the 2 and both achieve a maximum (no plateau relative to each other). Ways to increase venous return/cardiac output during exercise: 1. Skeletal muscle pump--#1 method. Important in pumping blood back to the heart in the standing position. Increase the skeletal muscle pump work with the amount of work you do—the greater the force & frequency of contraction. Sometimes referred to as the 2nd heart. 2. Vasodilation—decrease SVR, increase flow, increase VR 3. Venoconstriction increases with sympathetic activity. 4. Decrease in venous compliance caused by the venoconstriction. Veins then function more as a conduit to send blood back to the heart instead of acting as storage (as they normally do). Remember from last week. No increase in blood volume; compressing veins mobilizes more blood. Cardio #110 Mon, 02/10/03, 9am Dr. Smith Jennifer Uxer for Milena Patel Page 3 of 4 5. Respiratory pump—creates a greater negative pressure establishing a transient gradient, increasing VR. Least contribution compared to others. D. Stroke Volume SV increases as workload increases up to a point. Then, it acts as a curvelinear function that’s difficult to predict—varies between people. THIS IS DIFFERENT FROM THE OTHER CURVES—THAT IT PLATEAUS BEFORE MAX. Increasing contractility increases stroke volume. Increase heart rate, decreases filling time, decreases stroke volume—this causes some degree of plateau-ing. This isn’t at max exercise. Stroke volume plateaus at about 50 – 60% of the max workload. Afterload affects SV….reduced afterload contributes to increased SV. Contractility affects SV---increased.. Vasodilation occurs in arterioles where there’s sympathetic innervation. Compliance of larger arteries isn’t changed. Venous compliance is affected by sympathetics due to its innervation. Increase stiffness along the length, decrease compliance. E. Heart Rate O2 consumption achieves a maximum & HR achieves a maximum. If HR plotted against workload, it looks like CO. It rises to a maximum and plateaus. Everyone has a max HR that varies between people. Ballpark HR = 220 – age. Its response is due to changes in sympathetic and parasympathetic activity. At rest, parasympathetics predominate up to a HR of about 100 – 110 bpm. The increase is due to withdrawal of the parasympathetics. Above 110 bpm, sympathetics drive the HR. Fluctuations in parasympathetic system are the primary HR controller in a healthy system—exept at high exercise workloads. Sympathetic system is a stress response. Tends to be high in diseased states—stresses to the system. Plays role in progression of many cardiovascular diseases. When you Stop exercising: HR drops quickly. Most of initial decrease is return of parasympathetic nerve system. As it continues, see a progressive decrease in sympathetic nerve activity also. F. Cardiac Function as increasing sympathetic activity. Increase preload a little bit. Increase contractility—for a given preload, you have an increase in stroke volume. Decreased afterload because of systemic vasodilation. SVR decreased. Increased stroke volume—contribution by lower afterload. Increased ejection fraction—crude marker of contractility. As contractility increases, ESV decreases, and ejection fraction increases. Cardio #110 Mon, 02/10/03, 9am Dr. Smith Jennifer Uxer for Milena Patel Page 4 of 4 Increase in contractility changes the cardiac function curve. A decrease in venous compliance is seen, shifting mean circulatory filling pressure. The slope of the VR curve is steeper—evidence in change of the SVR. Steep slope = low resistance. More blood flow and get a much higher VR. Preload is increased slightly. Higher VR & CO Left shift due to increase in cantractility Steeper slope CO and VR at rest Preload at rest MCFP