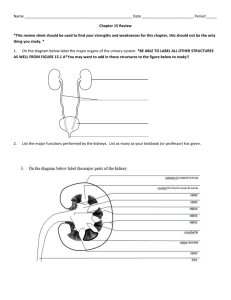
Urinary System
advertisement

Urinary System The urinary system consists of: a pair of kidneys, which remove substances from blood, form urine, and help regulate certain metabolic processes a pair of tubular ureters, which transport urine from the kidneys a saclike urinary bladder, which stores urine a tubular urethra, which conveys urine to the outside of the body. Blood enters the kidney via the renal artery, which is a branch of the aorta. The blood leaves the kidney in the renal vein, which joins the inferior vena cava. Kidneys The kidneys are bean-shaped organs, each about the size of a tightly clenched fist. They lie on the posterior abdominal wall behind the peritoneum and on either side of the vertebral column near the lateral borders of the psoas muscles. The superior pole of each kidney is protected by the rib cage, and the right kidney is slightly lower than the left because of the presence of the liver superior to it. Each kidney measures about 11 cm long, 5 cm wide, and 3 cm thick and weighs about 130 g. A fibrous connective tissue layer, called the renal capsule, encloses each kidney, and around the renal capsule is a dense deposit of adipose tissue, the renal fat pad, which protects the kidney from mechanical shock. The kidneys and surrounding adipose tissue are anchored to the abdominal wall by a thin layer of connective tissue, the renal fascia. The outer portion of the kidney is the renal cortex. The medulla lies deep to the cortex. The innermost portion is the renal pelvis, which collects the urine and passes it to the ureter. Each kidney lobe contains about 1.2 million functional units called nephrons. The nephron is the functional unit of the vertebrate kidney. Each human kidney has about one million of these tiny structures. Nephrons are the urine-producing unit in each kidney. Each nephron consists of a renal corpuscle; where plasma is filled from the glomerulus and is collected in the glomerular capsule and a renal tubule surrounded by blood vessels. The renal tubule is a duct that leads the filtrate away from the glomerular capsule. The renal tubule is divided into sections; the proximal convoluted tubule, the nephron loop (Loop of Henle), and the distal convoluted tubule. Several nephrons empty into one collecting duct. Cells of the nephron wall process the material filtered from the blood, returning valuable substances to the bloodstream and collecting additional wastes for excretion The renal artery branches until each nephron has an afferent arteriole leading to it. This afferent arteriole leads to a convoluted capillary called the glomerulus. The efferent arteriole leads away from the glomerulus to a second capillary bed, the peritubular capillaries. Venous circulation leads away from the nephron. Urine Formation Urine is formed through a combination of four basic processes: 1) glomerular filtration, 2) tubular reabsorption, 3) tubular secretion, and 4) water conservation. Blood is under high pressure in the glomerulus; thus, plasma (except for plasma proteins) moves into the glomerular capsule. This fluid is called filtrate. As the filtrate moves along the tubules, it is referred to as tubular fluid. Most of the water and many other molecules are reabsorbed into the blood, while some substances are secreted into the tubular fluid. Once the fluid moves into the collecting, duct it is called urine. While in the collecting duct, additional water is removed from the urine, concentrating the wastes. Although about 45 gallons of filtrate is produced daily, most of the water is reabsorbed; if not, we would quickly die of dehydration. The conservation of water is largely due to the long loop of the nephron, which establishes a concentration gradient in the kidney tissue. Water can leave the collecting duct by osmosis and return to the bloodstream in the surrounding peritubular capillaries. Net Filtration Pressure Filtration pressure across the filtration membrane is equal to the blood hydrostatic pressure (BHP) minus the colloid osmotic pressure (COP) in the glomerular capillary and minus the capsular pressure (CP). Glomerular Filtration Autoregulation of Glomerular Filtration Rate (GFR) GFR must be precisely controlled. The kidneys are able to maintain a relatively stable GFR in spite of changes in blood pressure; however, it is not able to compensate for extreme blood pressure variations. The Renin-Angiotensin-Aldosterone Mechanism Decreased blood pressure is detected by the kidney, resulting in increased renin secretion. The result is vasoconstriction, increased water reabsorption, and decreased urine volume. These changes function to maintain blood pressure. Tubular Reabsorption & Secretion The proximal convoluted tubule (PCT), primarily functions in tubular reabsorption. The PCT reabsorb about 65% of the glomerular filtrate. The concentration of Na+ in the tubular fluid is high compared to that in epithelial cells of the PCT. Sodium is thus reabsorbed by both simple diffusion and facilitated diffusion. Sodium carriers will also cotransport glucose and amino acids, thus allowing for the reabsorption of glucose and amino acids. As sodium ions are reabsorbed into the interstitium and then into the blood, an osmotic gradient forms, allowing for the reabsorption of water as well. The permeability of the wall of the collecting duct varies under the influence of antidiuretic hormone (ADH). ADH is released by the posterior pituitary in response to increased osmotic pressure (decreased water or increased solutes in blood). ADH increases the wall’s permeability to water so that more water leaves the collecting duct and returns to the bloodstream. If the osmotic pressure of the blood decreases, ADH is not released and water stays in the collecting duct, leaves as part of the urine. Neurons in the hypothalamus produce ADH, which the posterior pituitary releases in response to a decreasing water concentration in blood or a decrease in blood volume. When ADH reaches the kidney, it increases the permeability of the epithelial linings of the distal convoluted tubule and collecting duct to water, and water moves rapidly out of these segments, eventually into the blood, by osmosis (water is reabsorbed). Consequently, urine volume falls, and urine concentrates soluble wastes and other substances in minimal water. Concentrated urine minimizes loss of body fluids when dehydration is likely. If body fluids become too dilute, ADH secretion decreases. In the absence of ADH, the epithelial linings of the distal segment and collecting duct become less permeable to water, less water is reabsorbed, and urine is more dilute, excreting the excess water. Urine Concentration One of the primary functions of the kidney is better understood at the level of the nephron. In forming urine, the nephron functions to remove metabolic wastes from blood while regulating the volume and composition of body fluids. Urine formation begins in the renal corpuscle, where blood passing through the glomerulus is filtered. Filtrates include water, ions, and other solutes, which are filtered out of the blood and into the capsular space to begin urine formation. Urine passes into the proximal convoluted tubule, then into the nephron loop. The nephron concentrates urine by the process of the countercurrent multiplication system. The countercurrent multiplication system is basically the means by which water and sodium are extracted from the filtrate as it passes through the tubules toward the collecting ducts. This system is called countercurrent, because of the dynamics set up by the hairpin turn of the loop of Henle. The direction of flow in the descending limb of the loop is opposite from the direction of flow in the ascending limb. By flowing in opposite directions in such close proximity, a unique interaction occurs. The loop of Henle dips from the cortex of the kidney into the medulla, and is surrounded by medullary interstitial fluid. The countercurrent multiplication system is responsible for not only elevating the concentration of urine in the loop, but more importantly, it elevates the concentration of the interstitial fluid as well. To explain the countercurrent multiplication system, we must first imagine the loop filled with a stationary column of glomerular fluid, which includes water, salt, and urea. At first, the concentration of the glomerular fluid and the surrounding interstitial fluid will be equal at an osmolarity of 300 milliosmoles. Within the walls of the thick segment of the ascending limb, special pumps extract salt (NaCl) from the fluid and transport it to the interstitium. The two areas no longer have an equal osmotic pressure and a gradient has been established. Within the thick segment, the concentration is at 200 milliosmoles, whereas in the medullary tissue, the concentration is at 400 milliosmoles. Over time, a net diffusion of salt into the descending limb and a net diffusion of water out of the descending limb result in a balance in osmolarity between the descending limb and the surrounding interstitium. Because the thick segment is still actively pumping out salt, the osmolarity of the ascending limb is still 200 milliosmoles and the interstitium and descending limb are balanced at 400. Salt accumulates in the medulla while water is drawn out of the fluid in the descending limb. Water is removed by the vasa recta, which are capillaries that surround the loops. In real life, operation of this gradient occurs while the fluid is flowing. Fluid flowing in from the proximal tubule and out to the distal tubule along with the constant pumping of salt into the medulla contributes to the "multiplication" of this gradient. As fluid follows the path of the loop, an increasing amount of water is extracted as it reaches the bottom and an increasing amount of salt is pumped out as the fluid reaches the top. The more salt pumped out, the higher the concentration in the medulla. The higher the concentration in the medulla, the more water is extracted. Eventually, the levels of osmotic pressure are equal horizontally, with the highest value being at the tip of the loop. This level is at 1,400 milliosmoles/liter, which is also the value of the maximal osmolarity of excreted urine. As you can see, fluid becomes more concentrated as it rounds the loop but it immediately becomes re-diluted as it reaches the top. Final concentration of the fluid occurs in the collecting ducts, as it must travel back through the concentrated interstitium of the medulla on its way to the calyces. Urine is concentrated even further in the collecting ducts. The collecting duct must transport urine back through the concentration gradient formed by the nephron loop. The walls of the collecting duct are permeable to water but not to salt, therefore an increasing amount of water is drawn out by osmosis as the fluid travels though the gradient. The gradient provides the force for the concentration of urine, but the rate is determined by the amount of anti-diuretic hormone (ADH) in the blood. An increase in ADH in the blood causes the collecting ducts to become more permeable to water. Less urine is secreted and it is more concentrated. A decrease in ADH results in a decrease in water removed, thus a larger volume of more dilute urine is excreted. Urine Elimination Male Urinary Bladder (a) Coronal section. (b) Posterior view.