2010 Annual Report - University of Vermont
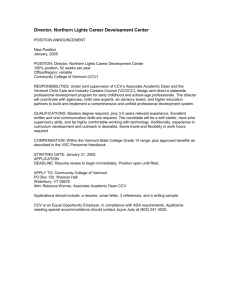
advertisement

FY 2010 Annual Report Department of Family Medicine Family Medicine Health Care Service Fletcher Allen Health Care 2 CHAIR’S MESSAGE 2010 There were many highlights for the Department of Family Medicine in 20092010. Dean Frederick Morin appointed Thomas Peterson, MD, as Professor and Chair of Family Medicine following a national search. Dr. Peterson brings longstanding experience as a clinician, educator, and organizational leader to the position. The department implemented our electronic health record (PRISM), and acquired a rural family practice and teaching site in Hinesburg, Vermont. This year marked our 34th Annual Family Medicine Review Course and 9th Annual Cultural Awareness Workshop. New faculty include Tavis Cowan, MD, and Nellie Wirsing, MD, who bring expertise in acute care and residency education. Department faculty with new roles include Alicia Jacobs, MD, Dan Weinstein, MD, and Dale Stafford, MD, as medical directors; Charlotte Reback, MD, directs the Generations Course, Candace Fraser, MD, the Third Year Clerkship, and Brian Flynn, ScD, is Interim Director of Research. Faculty and staff support the community through activities such as free clinics, wilderness rescue, boards and foundations service, and invited lectures on topics from lactation to palliative medicine. The Department has substantial achievement in medical student education through its third-year clerkship, elective offerings, course leadership, and advising programs. Our graduating students enter family medicine exceeding national trends and generate superlative reviews from residency programs. The department has written or co-written multiple educational innovation grants, every proposal funded or otherwise has led to enhancement. Our faculty have been recognized with national curriculum and teaching development leadership roles. Our residency program thrives with record applicant numbers, innovative curriculum, and commitment to rural and underserved health, patient- centered medical home development, and community medicine. Fifty percent of recent residency graduates elected to practice in Vermont—a program goal. Faculty scholarship is expanding with projects in farm worker care, breast and ovarian cancer screening, patient education using media and graphical decision aids, lactation education, behavioral motivation for self-care of chronic conditions, lead screening, and prevention of health professional fatigue and error. Family Medicine faculty receiving awards include Laura McCray, MD, as a Frymoyer Scholar, Michael Sirois, MD, as Faculty Teacher of the Year, and Melanie Lawrence, MD, and Kerry Crowley, MD, with UVM COM Alumni Awards. Thomas C. Peterson, MD Chair 3 THE MISSION ______________________________________________________________________________ The Department of Family Medicine and Family Medicine Health Care Service of Fletcher Allen strives to provide high quality, primary, and family-oriented care and to provide leadership in improving the health of the people and communities we serve. We do this through: High quality, innovative teaching programs for pre-doctoral, residency, continuing medical education learners, and encouraging the selection of Family Medicine careers Research and scholarship to advance the science of Primary Care and the specialty of Family Medicine Patient-centered quality care and service delivery, providing value to our patients Community service and outreach The Department is committed to continuous improvement of the quality of its programs, the development of its faculty, and the provision of its services. The Department will assure the efficient and cost-effective utilization of its resources and management of its programs and activities. The Department is committed to the development of excellent faculty who will serve as role models for learners, both in their specialty and their communities. http://www.med.uvm.edu/Familymedicine/ 4 FAMILY MEDICINE DEPARTMENT / HEALTH CARE SERVICE HIGHLIGHTS FOR FY2010 DEPARTMENT Tavis Cowan, MD, and James Ulager, MD, have joined our clinical faculty, Dr. Cowan at Walk-InCare and Dr. Ulager as medical director at the new Family Medicine site, Hinesburg Family Health. Among faculty accomplishments: Thomas Peterson, MD, was named one of the Best Doctors in America, 2009-2010; Michael Sirois, MD, was named Faculty Teacher of the Year; and Karen Richardson-Nassif, PhD, received the Outstanding Service Award from the Northeast Group on Educational Affairs in 2010. Dr. Candace Fraser took the reins of the clerkship in October and the transition has been extremely smooth. Dr. Thomas Peterson and resident Dr. Heather Stein, as part of the residency grant, attended a threepart conference in 2010 titled “Addressing the Health Needs of the Underserved,” presented by the University of California San Diego School of Medicine. The department is delighted to contribute to UVM’s overall excellence in primary care education. Our faculty teaches in the Family Medicine Clerkship and Acting Internship, Doctoring in Vermont, Doctoring Skills, Medical Student Leadership Groups, Palliative Care, and Health and Human Ecology electives. Counter to national trends, overall interest in family medicine is substantially increased, and nine members of the UVM COM 2010 graduating class matched in Family Medicine. Our family practice clinics participate in Vermont’s Blueprint for Health and seek qualification as Patient-Centered Medical Homes. All of our sites have implemented the electronic health record PRISM. Faculty scholarship projects include improving early detection and treatment of ovarian cancer in Vermont, assessment of program impact on trends in choice of practice in a rural state, seasonal and weather influences on bicycle commuting, and input on a mother/baby breastfeeding study. The department actively collaborates with the Palliative Care Service, VCHIP, the Vermont AHEC Program, and the Office of Health Promotion Research. The 36th Annual Family Medicine Review Course was held at the Sheraton Hotel and Conference Center in June. There were over 200 attendees on "Vermont Day". Anya Koutras, MD, directed this very successful CME program. The Department also organizes a Primary Care Sports Medicine Conference (led by Robert Luebbers, MD) and an Advanced Life Support in Obstetrics Conference (led by Anya Koutras, MD). Faculty presented their academic work at AAFP, STFM, North American Primary Care Research Group, Regional STFM meetings, and international educational conferences. The Department sponsored the Ninth Annual Cultural Competency Workshop at UVM under the leadership of Monica Romanko, MD. This year’s topic was “Crossing the Divide: Understanding the Impact of Culture and Diversity on Grieving and End of Life.” The Department continues to enjoy a close collaborative relationship with the Vermont Academy of Family Physicians. The FM clerkship will be expanding to 6 weeks beginning March 2011, thanks to the hard work of Drs. Candace Fraser and David Little. John King, MD, and Laura McCray, MD, Residency Director and Associate Residency Director respectively, presented a well-attended workshop titled “Competency-Based Criteria for Advancement: Setting Expectations to Create Success,” at the program directors’ workshop held June 6-8 in Kansas City. 5 RESIDENCY Our Residency Program has an outstanding reputation. Half of our recent graduates accepted practice positions in Vermont. Our entering residency class is top-notch; the Residency is excited to welcome UVM College of Medicine graduates Michelle Cangiano, Amy Savoy, and Elena Simon. Curriculum improvements include office procedural training, chronic care modules, and gynecologic training sites. Our HSRA Residency Training Grant for 2007-2010 continues to focus on health issues for Vermont’s farm workers and provides educational and clinical models for training. The Family Medicine Service has provided a popular and highly educational acting internship experience for students and has enhanced the quality of the program. Laura McCray, MD, has led the educational curriculum for the FMS. The program fully matched (6/6) in June 2010, with excellent residents from throughout the country, reflecting well on the curriculum, service, and recruiting changes implemented over the past years. There were 346 applicants to the Family Medicine residency program, a more than 34% increase from 2008-09. Resident Community and Prevention projects have continued to improve the health of the community and patient care at Milton Family Practice. Current projects include: development of a community garden to teach children about nutrition; Tar Wars, a smoking prevention program geared towards 4th and 5th graders; Helmets on Heads Program, a head safety program; published health-related articles; health-related posters displayed in patient exam rooms; presentations to high school students on health careers in collaboration with AHEC (Area Health Education Centers); ski helmet safety program to the Milton Ski and Ride Club co-sponsored by Community Health Improvement; and the mobile farm workers clinic. The Residency Teacher of the Year for 2010 was awarded to Michael Sirois, MD. The 2010 Community Teaching Award went to David Hobbs, MD; Michael Rappaport, MD; Jennifer Willingham, MD; Patti Fisher, MD; Paul Reiss, MD; and David Adams, MD. The 2009 Family Medicine Teaching Awards were presented to Hinesburg Family Health, Hinesburg, Vermont, and Family Medicine Associates, Springfield, Vermont. (Presented at the Review Course in June 2010) The 9th Annual Cultural Awareness Workshop, Crossing the Divide: Understanding the Impact of Culture and Diversity on Grieving and End of Life was held in June, with about 140 in attendance. This workshop was presented by the Residency Training in Primary Care Grant in conjunction with the Office of Multicultural Affairs. The course director was Monica Romanko, MD, Assistant Clinical Professor and Director of Program on Cultural Awareness. PRE-DOCTORAL PROGRAMS Doctoring Skills continues as a successful introduction to clinical skills. Family Medicine faculty includes Anya Koutras, MD, John Saia, MD, and Candace Fraser, MD. The course is co-directed by family medicine faculty member Cate Nicholas, EdD, MS. Doctoring Skills introduces first-year students to the physical exam, interviewing skills, and advanced skills training. The Family Medicine Clerkship continues as one of the highest-rated clerkships by students. Candace Fraser, MD, and Martha Seagrave, PA-C, continue their dedicated efforts to bring excellent training for the students. Anya Koutras, MD, serves as Director of the fourth-year and acting internship programs and helps support the advisee program. The Acting Internship in Family Medicine has received excellent evaluations from fourth-year students; we anticipate strong interest and participation from students over the coming year. 6 Three senior course selections are available. Charles Hulse, MD, PhD, developed and teaches a course in Ecosystem Change and Human Health, and Omar Khan, MD, designed and leads a seminar in Global Health. Both of these offerings have been extremely popular. Family Medicine also offers an Underserved Rotation where students work with underserved communities anywhere within the United States. Faculty members Karen Burke, MD, and Charlotte Reback, MD, are active teachers in the Medical Student Leadership Group course. RESEARCH AND QUALITY IMPROVEMENT PROJECTS Allyson Bolduc, Clinical Associate Professor; Rob Luebbers, Clinical Associate Professor; and Thomas Peterson, Professor and Chair, are working on an initial proposal entitled, “Improving Early Detection and Prevention of Ovarian Cancer in Vermont.” Hurowitz L, Flynn, Brian, Research Professor, Reardon M: Assessment of program impact on trends in choice of practice in a rural state. Peer-reviewed presentation to Sixth Annual American Association of Medical Colleges (AAMC) Physician Workforce Research Conference, Alexandria VA, May 2010. Flynn, Brian, Research Professor, Dana GS, Dorwaldt AL. Seasonal and weather influences on bicycle commuting: design and preliminary results of recruitment. Poster presented at the annual UVM Transportation Research Center Exposition, May 2010. King, John, Associate Professor; McCray, Laura, Clinical Assistant Professor: "Competency Based Advancement Criteria: Setting Expectations for Success." Family Medicine Program Directors Workshop, Kansas City, Missouri. June 4-6, 2010, workshop presentation. Seagrave, Martha, Research Associate Professor Author, Family Medicine Computer-Assisted Simulations for Educating Students (fmCASES) virtual patient case: 20. 28 year-old female with abdominal pain-Ms. Bell. Peer Reviewer, Family Medicine Computer-Assisted Simulations for Educating Students (fmCASES) virtual patient case: 6. 57-year-old female presents for diabetes care visit -Ms. Sanchez. Co-presenter “Case Description Papers - Utilizing a New Scoring Rubric” National Predoctoral Education Meeting of the Society of Teachers of Family Medicine, Jacksonville, FL. The Family Medicine Department is actively engaged in the Vermont Blueprint for Health. This project is a Vermont legislative directive through a grant to FAHC designed to explore how we can better manage chronic diseases in Vermont. Patient-care teams from each of the FAHC family medicine practices have been trained in and are actively pursuing micro-system practice improvements to enhance the care of their patients with chronic diseases like diabetes. CLINICAL Each of the clinical sites continued to be busy with over 107,674 total office visits in FY 2010. The Family Medicine Service expanded resident coverage for a larger portion of the community family physicians, providing quality interactions amongst them. Physician additions: At South Burlington Family Practice –Whitney Calkins, MD; at Milton Family Practice – Nellie Wirsing, MD. Hinesburg Family Health will become a family medicine clinical site this fall under the medical directorship of James Ulager, MD. 7 TABLE OF CONTENTS Page[s] EDUCATION Predoctoral Education ............................................................................... 9-11 Resident Education..................................................................................... 12-13 Continuing Medical Education.................................................................. 14 CLINICAL ACTIVITY Berlin Family Health ................................................................................. 15 Colchester Family Practice......................................................................... 15 Milton Family Practice .............................................................................. 16 South Burlington Family Practice ............................................................ 16 Walk-In Care Center ................................................................................. 17 GRANTS ............................................................................................................... 18-19 DEVELOPMENT /AWARDS.......................................................................... 19-20 PRESENTATIONS/PUBLICATIONS AND OTHER WRITINGS....... 20-21 SERVICE.............................................................................................................. 22 MAINE MEDICAL CENTER ........................................................................ 23-25 FORMAL PRESENTATIONS ........................................................................ 26-27 2009-10 TEACHING CONTRIBUTIONS .................................................... 28-31 COMMITTEE SERVICE ................................................................................. 32-34 FACULTY / PROVIDERS................................................................................ 35-38 RESIDENTS & 2010 GRADUATES ............................................................. 39 VERMONT PART-TIME FACULTY........................................................... 40-41 MAINE PART-TIME FACULTY................................................................... 41 STAFF..................................................................................................................... 42-44 8 PREDOCTORAL EDUCATION PREDOCTORAL EDUCATION TEAM Martha Seagrave, PA-C, BSN, is the Predoctoral Programs Director. Candace Fraser, MD, was selected to be the Family Medicine Clerkship Director beginning in October 2009, replacing David Little, MD. Kathryn Beaudry serves as the Predoctoral Education Coordinator. Anya Koutras, MD, leads the Advanced Integration programming and the FM Acting Internship. David Little, MD, co-led the Predoctoral Directors Institute, a national leadership program sponsored by the Society of Teachers of Family Medicine and serves on the STFM Education Committee. There was a successful continuation of the FOCUS curriculum, emphasizing programming to support and encourage care of underserved populations. Programming included brown bag sessions on rural and international health, panels and discussions on care of underserved populations, preceptorships in federally qualified health centers and other underserved settings, as well as student community projects. FOUNDATIONS LEVEL COURSES Family Medicine faculty teach throughout all the foundations level courses as guest lecturers in all core classes in addition to their roles as preceptors in Doctoring Skills and group leaders in Medical Student Learning Groups. They provide the clinical perspective in the basic science curriculum key to the goal of the Vermont Integrated Curriculum. DOCTORING SKILLS Doctoring Skills is a course which begins in the first semester, first year, and seeks to introduce each student to the basic skills of clinical medicine. It comprises a portion of the curriculum called “Human Structure and Function” during which students study gross and microscopic anatomy and the fundamentals of physiology as they learn and acquire the skills of performing a physical examination and building a coherent medical history. Students learn by working in small groups with standardized patients under the direct supervision of a physician preceptor in order to develop their professional interactive skills. This curriculum is directed by Dr. Cate Nicholas and Dr. Alan Rubin. Many of our Family Medicine faculty participate in the precepting for this course by providing highly experienced direct supervision of students while they learn and practice their clinical skills. DOCTORING IN VERMONT Doctoring in Vermont is a Foundations level course with both a spring (March-June) and fall (SeptemberDecember) session. Each session consists of four afternoons (total of 8 sessions for the course) spent in the office of an assigned community preceptor recruited from among the primary care physician community within a one-hour drive of Burlington. Students travel to their preceptor’s office and practice examination and interviewing skills under direct supervision. Students complete two “complete” history and physical examinations, one with their preceptor and one with a standardized patient at the campus Assessment Center, complete a clinical correlation presentation and maintain clinical logs. FM physicians comprise the majority of these community-based preceptors. 9 MEDICAL STUDENT LEADERSHIP GROUPS – I & II The Medical Student Leadership Groups (MSLG I and II), are designed to introduce and support the development of the capacities, attitudes, and behaviors critical to medical professionalism. This course focuses on the practice of leadership and professionalism in daily interactions with peers, mentors, colleagues, and families as the foundation of medical practice. FM clinicians and faculty participate as small group leaders and presenters for this course. STANDARDIZED PATIENT PROGRAM The Standardized Patient Program at the College of Medicine is directed by Dr. Cate Nicholas. This program provides students with physical exam training, medical interviewing skills, and evaluation with specific and thorough feedback on their application of skills and knowledge. This is done through the use of skilled and knowledgeable actors playing the roles of patients in predetermined clinical scenarios. This program showed significant foresight and is invaluable for the preparation of our students for clinical work and the newer clinical skills segment of the Boards. SENIOR STUDENT PROGRAMS IN FAMILY MEDICINE This advising program assists students in selecting and planning for residency training in Family Medicine. Students work with Dr. Anya Koutras and other Family Medicine faculty advisors. FAMILY MEDICINE CLERKSHIP This program, under the direction of Candace Fraser, MD, and Martha Seagrave, PA-C, is a required four-week office-based rotation in the Clerkship year. The responsibility for teaching the clerkship is shared with the Department of Family Medicine at the Maine Medical Center (Peggy Cyr, MD). Over one hundred and fifty part-time faculty in Vermont and Maine participate in the teaching at their offices. Programs include web-based learning modules on prevention, domestic violence, and musculoskeletal disorders. Our clerkship faculty also provides leadership and teaching for the Collaborative Bridge in Family Medicine / Internal Medicine/ Pediatrics, including a clinical performance assessment exercise. ACTING INTERNSHIP A one-month acting internship for fourth-year students led by Dr. Anya Koutras had a very successful year as part of the Family Medicine Inpatient Service. The service receives consistently high praise from the participating fourth-year students. Our Maine colleagues offer a similar AI at Maine Medical Center. Both programs include a directed learning experience with course competencies and basic science components. ADVANCED INTEGRATION Family Medicine now offers eight different fourth-year electives for students to choose from. In addition to the Acting Internships, we offer FM Preceptorships at our Milton Practice, and other Vermont and Maine outpatient practices. Students can also sign up for a month at a rural site working with a family doctor or an underserved rotation anywhere in the United States. Dr. Charles Hulse has created an extremely popular distance-learning course on Ecosystem Change and Human Health and Dr. Omar Khan returns to Vermont four times a year from his new home in Maryland to teach his Seminar in Global Health to our Vermont students. Twenty-eight students elected to participate in Dr. Khan’s Global Health elective and 38 students participated in Dr. Hulse’s Ecosystem Change elective. Students can also choose to do a supervised reading or research in the FM month. FAMILY MEDICINE INTEREST GROUP FMIG is a very active student-run organization which brings together students interested in Family Medicine under the leadership of a faculty advisor, Martha Seagrave, PA-C, and staff advisor Kathryn 10 Beaudry. The group is active within the medical school promoting Family Medicine. They host procedural workshops including injection, suturing, casting, and vital signs and are also involved in service projects within the community. Throughout the year, FMIG hosts brown-bag lunch discussions geared toward Family Medicine showcasing family physicians from throughout the state. In addition, student members participate at the statewide Vermont Academy of Family Physicians annual meeting and board meetings, regionally at the STFM regional meetings, and nationally at the National Congress for Residents and Students. The Department of Family Medicine hosts three events throughout the year for our Family Medicine students. During the month of February, we host a celebration for the students who have selected Family Medicine as their career choice. Partners are included as we celebrate the end of the clerkship year with our third-year students and the upcoming graduation of our fourth-year students. Shortly before graduation, we host a dinner meeting geared toward students who have selected Family Medicine as a career choice and who will soon begin the residency application process. Fourth-year students and residents are invited to share their experiences with the third-year students. During the month of September, we host a dinner meeting for our fourth-year Family Medicine students. This meeting focuses on the residency interview process. The members of the faculty as well as Family Medicine residents are available to provide information and to answer any questions. Our Maine colleagues also run an FMIG under the guidance of Dr. Peg Cyr. It has been active with faculty and current FM residents presenting on topics of interest to the students rotating in Maine. 11 RESIDENT EDUCATION John King, MD, MPH, is the Residency Program Director. Monica Romanko, MD, and Laura McCray, MD, are Associate Directors. Jennifer Wilson serves as Residency Coordinator assisted by Lise Vance, Education Coordinator. For 2009-2010, Sarah Davies, MD, and Mick Graham, MD, serve as Chief Residents in Family Medicine. Teaching is provided by eighteen full-time faculty members and many volunteer and part-time providers. RESIDENCY HIGHLIGHTS OF THE PAST YEAR INCLUDE The residency continues with the HRSA grant entitled "Family Medicine Residency Training in High Quality Accessible Rural Primary Health Care." This grant expands on quality improvement projects in Milton and provides experiential rural experiences including home and farm visits at Keeler Bay Family Practice in South Hero and NOTCH clinics in Franklin County, Vermont. The grant is complete in June 2010. Strong patient and financial numbers at Milton provided a model practice and population for resident education. Graduation of six residents in June 2010: three in Vermont—Norwich, Middlebury, and Berlin; one in Ontario, Canada; one to rural New York; and one to Louisiana. The 2009-2010 recruiting season showed an increased interest with a more than 34% increase in applications received from 2008-09 and 52% more applicants interviewed. The overall academic strength was higher as well. Dr. Omar Khan continues to direct the International Medicine didactic curriculum. Dr. John King, with Lise Vance’s assistance, is overseeing the Community Medicine Projects. The residents have been working on the following: Uninsured Farm Worker Health Care Youth Garden and School Nutrition Intimate Partner Violence Breastfeeding Education and Support Nutrition and Healthy Body Image for Girls on the Run participants Cooking and Nutritious meal planning for parents of kids K-2 at Milton Elementary School AED placement in the Milton Schools Tar Wars - smoking prevention program Helmets on Heads - head safety program Rural Health Modules presented during Education Sessions The Blueprint for Health local staff team is working with residents and focusing on quality improvement activities including patient education, message and prescription refills, immunizations, and chronic pain management. Dr. McCray continues to direct the education on the Family Medicine Service with the well-received "chalk talks" on Friday afternoons. The residency continues 1:1 TA sessions with residents and faculty members in order to increase accessibility and continuity among chronic care patients. 12 RESIDENT – AWARDS/PRESENTATIONS/CONFERENCES Sarah Davies, MD Alaska: Frontier Medicine - Triaging in a Remote Setting, including Adult, Pediatric, and OB Cases Craig Sillick, MD, and Meera Ramachandran, MD AED program implementation in schools / the Uninsured Farm Worker clinic Justin Karlitz-Grodin, MD Colorectal and Prostate Cancer Screening and Medical Malpractice Jessica Rouse, MD Annual 2009 STFM: Northeast Region Conference "Uninsured Farm Worker Clinic: Reducing Barriers to Care for Farm Workers in Northwestern Vermont" October 2009 Michael Graham, MD Attacking Obesity in Just 15 Minutes 13 CONTINUING MEDICAL EDUCATION VERMONT FAMILY MEDICINE REVIEW COURSES The 36th Annual Family Medicine Review Course was held at the Sheraton Hotel and Conference Center from June 8-11, 2010. There were over 200 attendees on "Vermont Day". The course faculty was drawn almost exclusively from Fletcher Allen Health Care / University of Vermont College of Medicine medical staff, once again highlighting the incredible depth of talent at our institution. The course serves a broad cross-section of regional and national physicians, nurse practitioners, physician assistants, residents and medical students with an emphasis on preparation for the Family Medicine Board Certification Exam. Dr. Anya Koutras served as course director and again enjoyed expert support from the Office of Continuing Medical Education at the College of Medicine. ADVANCED LIFE SUPPORT IN OBSTETRICS The department co-sponsored an ALSO provider course July 16 & 17, 2009, in Concord, New Hampshire. The two-day course is designed to review topics of importance in the management of childbirth emergencies with an emphasis on hands-on practical skills such as forceps and vacuum assisted delivery, delivery of malpresentation, monitory strip interpretation, shoulder dystocia, basic ultrasound, and counseling in the setting of birth crisis. This year there were participants from the New Hampshire Dartmouth Family Practice Residency, the University of Vermont Family Medicine Residency and the University of Vermont OB Residency. Several faculty from Vermont and New Hampshire served as instructors: Angela Yerdon McLeod, DO, Course Director; Patricia Glowa, MD, and Gail Fayre, MD, Dartmouth Medical School, Department of Community & Family Medicine; Steve Genereaux, MD, Advisory Faculty, Wells River Clinic; and Melisa Gibson, MD, University of Vermont Family Medicine Residency Program. ANNUAL CULTURAL AWARENESS WORKSHOP 2010 The Ninth Annual Cultural Awareness Workshop, Crossing the Divide: Understanding the Impact of Culture and Diversity on Grieving and End of Life was held June 2, 2010, with about 140 attendees present. The agenda was: Disparities at the End of Life: The Impact of Race, Culture, and Socioeconomics on Advance Directives and Access to Hospice and End of Life Care was presented by resident Debbie Lieber, MD; Funerary Customs and Religious Traditions in Asian and Buddhist Cultures by Cuong Mai, PhD, UVM Professor of Religion; Panel discussion: Religious and Cultural Perspectives on Illness and End of Life with resident moderator Meera Ramachandran, MD; and panelists Rabbi Ira Schiffer; Allan Ramsay, MD; Reverend Rick Neu; and Muhaideen Batah, from the Islamic Society of Vermont; Multicultural Perspectives on the Language of Grief and the Art of Consolation with Keynote speaker Sandra L. Bertman, PhD, FT. This workshop was presented by the Residency Training in Primary Care Grant in the Department of Family Medicine and the Office of Multicultural Affairs. The course director was Monica Romanko, MD, Assistant Clinical Professor, Department of Family Medicine, and Director of Program on Cultural Awareness. 14 CLINICAL ACTIVITY BERLIN FAMILY HEALTH (BFH) We particularly appreciated Dr. Tim Burdick’s involvement in preparing for PRISM. As site leader, I am grateful for the time and energy that all of our staff have expended to make the transition to electronic records. COLCHESTER FAMILY PRACTICE (CFP) Our dynamic practice group has matured even more in the past few years with a very steady group of multitalented physicians. Our group continues to deliver the full spectrum of Family Medicine including obstetrical care, gynecologic and orthopedic procedures, hospital coverage, nursing home care, and health care for all ages. Along with active clinical practices, our faculty providers have other leadership roles. Dr. Allan Ramsay continues his lead role as the Director of the Palliative Care team. Dr. Tom Peterson is the Interim Chair of Family Medicine. Dr. Anya Koutras is the Director of 4th year programs and is also a certified lactation consultant. Dr. Candace Fraser will transition to become the Family Medicine Clerkship Director and Dr. Alicia Jacobs will step up to the position of Medical Director. We continue to be a busy clinical office with our other clinicians being Dr. Marga Sproul, Joanne Hunt (ANP), Deborah Thompson (PA), Heather Holmes (PA), Nancy Morris (NP – per diem), and Dr. Stephanie Kehoe (per diem). Angela Paoli (LicSW) continues to provide mental health counseling for our patients. During some busy times, we have additional providers who also work per diem including Dr. John Saia. We continually pursue quality initiatives to ensure the highest quality of practice. In this regard, we are active participants in the state’s Blueprint for Health, Chronic Care initiative, primarily focusing on diabetes. We are keenly anticipating our newest transition which is the implementation of PRISM – our new Electronic Health Record. This year we have continued writing a monthly health article for the local papers, The Colchester Sun and The Essex Reporter. We are in the process of updating and further developing our website as well as making efforts to go green in our building. All of our clinicians share in the clinical teaching that we do at the office for all four years of medical school and for the nurse practitioner program. The MD’s are also extensively involved in teaching at UVM and in The Family Medicine Residency program (including Grand Rounds, didactics, Family Medicine hospital service, teaching attending at residents’ continuity clinics), doing service through committee work, and multiple leadership endeavors. Everyone also takes an active role in quality improvement projects and often participates in clinical research projects. We represent a very dynamic professional group of the highest standard. We are supported here at the office by a wonderful staff of nurses, medical assistants, practice support specialists, referral specialists, transcriptionists, health information management, and our dedicated site supervisor Donna Kaynor. 15 MILTON FAMILY PRACTICE (MFP) Milton Family Practice remains the home of the Family Medicine Residency Program at the University of Vermont College of Medicine. At present, 19 resident physicians have their clinical practices at Milton Family Practice. Drs. Sarah Davies and Mick Graham are the 2009-2010 chief residents. The department of Family Medicine did well in the Residency Matching Program and the 6 incoming residents will be a strong addition to the program. In addition to residency-focused education, first through fourth year medical students from the University of Vermont College of Medicine, as well as other schools of medicine, receive training in Family Medicine at the MFP clinical site. Milton Family Practice continues to grow and to provide quality health care to the people of Milton and the surrounding areas. We are excited that Milton Family Practice will now host a Pharmacist from the new Vermont campus of the Albany College of Pharmacy. Several pharmacy doctoral students will spend clinical time at Milton, and we expect a great deal of collaboration with our resident teaching program. A few changes in the last year are worth noting. Dr. Kevin Rodgers has returned from time away working for the Indian Health Service. He will continue here on a part-time basis as a regular Teaching Attending and as a proceduralist and non-continuity provider. Dr. Lewis Holmes, Dr. Liz Schneider, Dr. John Saia, Dr. Steve Mann, and Dr. Rachel DiSanto are per diem providers helping to fill in when needed. A Baird Pediatric Clinician, Manon Tenny, is replacing Ryan Mebust who is moving to Ohio where his wife is starting a psychiatry residency. Our newest proud mother, Dr. Melisa Gibson, will be returning to practice after a brief maternity leave. Nellie Wirsing, MD, is joining the staff in August. Milton Family Practice continues to be active in promoting a variety of community outreach and educational activities. Activities include the school-based Tar Wars, the Helmets on Heads programs, and many in-school teaching programs, as well as volunteering for H1N1 vaccination clinics, Respite Care activities, and VNA Adult program activities. We continue to collaborate with the State of Vermont on the Blueprint for Health and have been making many changes to improve the delivery and management of chronic care. A FAHC-wide change at Milton Family Practice is the adoption of PRISM, the Fletcher Allen Health Care electronic medical record. This is a major change in practice work flows, and we expect to see increasing advantages in the delivery of patient care. We are also excited to have achieved NCQA recognition status for Physician Practice Connections – Patient-Centered Medical Home (PPC-PCMH). We are Recognized as a Level 2, with 74.25 points out of 100 and just .75 points below a level 3 (the highest scoring). Milton Family Practice has worked very hard for this accomplishment, and we have hired a Medical Assistant to help with the next steps of further developing the Patient-Centered Medical Home. SOUTH BURLINGTON FAMILY PRACTICE (SBFP) South Burlington Family Practice has been serving the South Burlington community and surrounding areas since 1997. Dr. Norman Ward continues his practice there in addition to serving as Medical Director Case Management at FAHC. Dr. Robert Luebbers continues to serve as medical director for the site. Drs. Allyson Bolduc, Whitney Calkins, David Lisle, Laura McCray, Karen Burke, Caroline Slimovitch and Anne Pelkey, PA-C, continue their busy practices. Dr. Wendy Libby has also joined us as a per diem provider. Charleen Tuthill does an excellent job as our site supervisor. Also, several new nurses and staff have joined the practice and have contributed much to its success. Physical therapy and mental health continue to be offered on site. South Burlington Family Practice continues to strive toward providing the best medical care possible for its patients and the community. 16 WALK-IN CARE CENTER (WICC) In 2009, the Walk-In Care Center at the Fanny Allen Campus completed its 9th year under the leadership of the Family Medicine Health Care Service. We had yet another year of growing numbers of patients seeking care walk through our doors. With patients coming from as far away as Smuggler's Notch and Jay Peak in the winter and the islands in the summer, our urgent care practice is succeeding in its outreach to the greater community. At the same time, the clinic continues to serve the patients at our primary care practices by keeping the doors open to them during evening hours and weekends. Our “pre-operative clinic,” run by Elissa Close, FNP, has continued its success with clinics being full on most days. Our infusion center has been as busy as ever, with our dedicated nurses working to provide individualized care to this varied group of patients. To meet the needs of our growing clinic, our provider staff was expanded this year. Drs. Dan Weinstein, Charlotte Reback, Charles Schmitt, Vivian Esparza, Rachel Inker, and Marc Kutler were joined by Drs. Jean Anderson-Swayze and Rebecca Winokur, both graduates of our own residency program in Milton, and by Drs. Tavis Cowan and Steven Mann. Our mid-level staff grew with the addition of Jessica Sarinelli, PA, who came to us from New Jersey with experience in both pediatric and adult emergency medicine, Karen Hibbard, PA, and Kim Schmitt, PA. They joined the mid-level team of Betsy EllisKempner, NP; Anne Marie Gleeson, NP; and Tonya Howard, NP. Charlotte Reback remained as medical director while Christina Hamel stepped down as practice supervisor, being succeeded by Tammy Yohn. Joyce Guillemette continued to serve as our clinical nurse specialist. We are fortunate to have many very experienced nurses and front desk staff on our team. They all work extremely hard to make our clinic the successful open access practice that it is. Looking forward, with our ever-growing numbers, we are hoping to expand our staff and our exam space to allow for efficient and seamless care of the patients who seek our services. 17 GRANTS Calkins, Whitney, MD Academic Detailing-Evidence-Based Prescription Drug Education Program for Health Care Professionals. Co-investigator with Amanda Kennedy. 07/01/2009 – 06/30/2010, $300,000. Carey, Peggy, MD, and Thomas Peterson, MD Boston Children’s Hospital, Screening and Brief Advice will Reduce Teen Substance Abuse. Funded by: National Institutes of Health (NIH) and Children’s Hospital Boston - $241,919 (2004-2009) Cichoskikelly, Eileen, PhD University of Vermont College of Medicine Office of Admissions: Assessment and Advancement of Humanism in Medical School Admissions and Beyond. Arnold P. Gold Foundation Grant. 07/01/09 – 06/30/2011. Flynn, Brian, ScD Special Research Grant for Child Obesity and Nutrition. Co-investigator with J Harvey-Berino as PI. Cooperative State Research, Education, and Extension Service, U.S. Department of Agriculture, 9/039/11 Seasonal Impacts on Bicycle Transportation. Principal Investigator. UVM Transportation Research Center/USDOT, 07/01/07 – 06/30/11. Special Research Grant for Child Obesity and Nutrition. Co-investigator with J Harvey-Berino as PI. Cooperative State Research, Education, and Extension Service, U.S. Department of Agriculture, 9/039/09, $104,637. Geller, Berta, EdD Vermont Breast Cancer Surveillance System (VBCSS). This cooperative research project links data from all breast imaging procedures performed in Vermont with pathology data and cancer registry data to provide a general description of mammography quality, participation levels, and breast cancer patterns, in addition to providing feedback to radiologists and research opportunities for a variety of potential investigators. The VBCSS is part of a five-member national consortium funded by the National Cancer Institute. Two other studies have been funded using the VBCSS data. Factors Affecting Variability of Radiologists is a four-site study funded by NCI and AHRQ, and Assessing and Improving Mammography Interpretive Skills is a six-site study co-funded by NCIs Breast Stamp funds and the American Cancer Society. There are also several supplemental studies through the VBCSS. We have two studies using quantitative measurement of breast density, one on the general screened population to better understand the role that density plays in predicting the risk of breast cancer, the other, which is also collecting buccal and blood samples, and fresh and frozen tissue samples is trying to elucidate the micro-environment of breast density. We have also been comparing mammography performance between Vermont, an opportunistic screening program, and Norway, an organized screening program. Funded by: The National Cancer Institute renewed for two additional five years periods, August 2000 - July 2010. Total direct cost support for the first five years was $1,397,608, with an additional $1,845,531 for the second five years, and $1,222,499 for the third fiveyear period. Improving Breast Cancer Outcomes for Older Women Through Effective Use of Screening Mammography. Co-investigator with Pamela Vacek as principal investigator. We will study the relationship of co-morbidity, treatment and mortality to screening benefit using Medicare and VBCSS data. Susan Komen Foundation. September 2009- September 2011. $202,837. 18 GRANTS (continued) Accuracy of Breast Pathology and the Impact of Technology & Double Reading. Co-investigator working with principal investigators, Drs. Donald Weaver (UVM) and Joann Elmore (University of Washington). We will evaluate the extent of variability, its sources and its impact on women undergoing breast biopsy and also evaluate possible techniques to improve accuracy, such as digital transmission of slide images and double reading. National Cancer Institute, 09-14, $303,480. Comparative Effectiveness of Breast Imaging Strategies in Community Practice. Co-principal investigator. The overall goal of this project is to conduct comparative effectiveness research on breast cancer imaging modalities and strategies to inform evidence gaps on how to optimize breast cancer screening in community practice. ARRA Grand Opportunity grant, National Cancer Institute, 09-11, $280,793 Hulse, Charles, PhD, MD Vermont Statewide Public and Private Partnership to Improve Maternal and Child Health. CoInvestigator with Judith Shaw. 07/01/2009 – 09/30/2010. Kessler, Rodger, PhD R-24 AHRQ. Collaborative National Network Examining Comparative Effectiveness Trials CoInvestigator. Patient-Centered Medical Home Collaborative. A Survey of NCQA certified PCMH practices to determine response to mental health and substance abuse problems. Principal Investigator. R-13 AHRQ 1R13HS018318-01. Conference to develop a national agenda for Collaborative Behavioral Health in the Patient Centered Medical Home. Co-Principal investigator. 2009. King, John, MD, MPH Residency Training in Primary Care. Additional Investigators: Monica Romanko, MD; Michael Sirois, MD; David Little, MD. Family Medicine Residency Training in High Quality, Accessible Rural Primary Care Health: HRSA Primary Care Residency Training Grant. Funded by: Department of Health and Human Services, Health Resources and Services Administration (HRSA) - $436,171 (Year July 2007-June 2010) Seagrave, Martha, PA-C Student/Resident Experiences and Rotations in Community Health (SEARCH) Program, “VT SEARCH Program”, Health Resources and Services Administration (HRSA), 9/2009-8/2012, $500,000, co-investigator. _____________________________________________________________ DEVELOPMENT E.L. Brownell Fund: The market value reached $1,715,111 with a working balance of approximately $82,802. This has allowed us to continue developing family medicine through supporting salaries and purchasing new office equipment to meet our expanding needs. Daniel G. Fischer Fund: This fund has a market value of $17,587 with a working balance of approximately $850 to further develop the medical library at Milton Family Practice. ______________________________________________________________________________ 19 AWARDS 2010 Edward E. Friedman Award: Presented to the graduating fourth year student best exemplifying the ideals of Family Medicine - Presented to Amy Savoy MD. (May) 2010 John P. Fogarty Leadership Award: Presented to Justin Smith, MD and David Longstroth, MD (May) 2010 Resident Teacher of the Year Award: Presented to Michael Sirois, MD. (June) 2010 Faculty Appreciation Award: Chosen by residents and presented to Paul Rosenau, MD. (June) 2010 Community Teaching Award: David Hobbs, MD; Michael Rappaport, MD; Jennifer Willingham, MD; Patti Fisher, MD; Paul Reiss, MD; and David Adams, MD 2009 Family Medicine Teaching Awards: Presented to Hinesburg Family Health, Hinesburg, VT, and Family Medicine Associates, Springfield, Vermont. (Presented at the Review Course in June 2010) Thomas Peterson, MD, Best Doctors in America, 2009-2010 PRESENTATIONS, PUBLICATIONS, AND OTHER WRITTEN PRODUCTIVITY 1. Burdick T. Improvisation techniques for prehospital medicine. East Montpelier Rescue Service training. East Montpelier, VT. 2010. 2. Burdick T. Wilderness trauma: case studies from Vermont search and rescue operations. Vermont Emergency Medical Services Conference. Burlington, VT. 2010. 3. Burdick K and Burdick T. IUD counseling and insertion techniques. Family Medicine Board ReviewCourse. Burlington, VT. 2010. 4. Burdick T. (accepted). High altitude medicine. Wilderness Medical Society Community Education Series. Salt Lake City, UT. 5. Burdick T. (in press). Musculoskeletal injuries. Wilderness Medical Society Community Education Series. Salt Lake City, UT. 6. Burke Karen - Dartmouth COOP, 2/09 Farm Injuries "Aging Farmers and Their Injuries," Vermont Farm Health Task Force 8/09 7. Primary Care Follow-up Plans for Adolescents With Substance Use Problems, Areej Hassan, Sion Kim Harris, Lon Sherritt, Shari Van Hook, Traci Brooks, Carey Peggy, Robert Kossack, John Kulig and John R. Knight. Pediatrics 2009;124;144-150, 2009. 8. Adolescents’ Preferences for Substance Abuse Screening in Primary Care Practice, John R. Knight, MD, Sion K. Harris, PhD, Lon Sherritt, MPH, Shari Van Hook, MPH, Nobelani Lawrence, BS, Traci Brooks, MD, Carey Peggy, MD, Robert Kossack, MD, John Kulig, MD, MPH. Subst Abus 2007;28:107-117, 2009. 9. Prevalence of Adolescents At-Risk by Riding in Cars with Intoxicated “Parents”, Celeste R. Wilson MD1,2,3,4, Sharon Levy MPH, MD1,2,4, Lon Sherritt MPH1,2,4, Melissa A. Rappo BA1,2, Sion K. Harris PhD1,2,4, John R. Knight MD1,2,4 and the New England Partnership for Substance Abuse Research (NEPSAR), (NEPSAR Co-Authors: Traci Brooks MD, Suzanne Boulter MD, Carey Peggy MD, Robert Kossack MD, John W. Kulig MD MPH, Nancy Van Vranken MD) 1Center for Adolescent Substance Abuse Research, Children’s Hospital Boston (CHB); 2Division of Developmental Medicine, CHB; 3Division of General Pediatrics, CHB; Department of Pediatrics, Harvard Medical School. Supported by grant #R01 DA018848 from the National Institute on Drug Abuse. Other support from #K07 AA0132980 (JK; National Institute on Alcohol Abuse and Alcoholism) and #5T 71NC0009-10 (SKH; Maternal and Child Health Bureau Leadership in Education for Adolescent Health) 20 10. Flynn BS, Worden JK, Bunn JY, Solomon LJ, Ashikaga T, Connolly SW, Ramirez AG: Mass media interventions to reduce youth smoking prevalence. American Journal of Preventive Medicine 39(1):53-62, 2010. 11. Flynn BS, Wood ME, Ashikaga T, Stockdale A, Dana GS, Naud S: Primary care physicians’ use of family history for cancer risk assessment. BMC Family Practice 11(1):45, 2010. 12. Jensen A, Geller BM, Gard CC, Miglioretti DL, Yankaskas B, Carney PA, Rosenberg RD, Vejborg I, Lyng E. Performance of diagnostic mammography differs in the United States and Denmark. Intl J Cancer. 2010 Jan 26. [Epub ahead of print] PMID: 20104518. 13. Ichikawa LE, Barlow WE, Anderson ML, Taplin S, Geller BM, Brenner JR. Time trends in screening mammography performance from the community-based Breast Cancer Surveillance Consortium, 1996-2004. Radiology 10091881; Published online May 26, 2010, doi:10.1148/radiol.10091881v. 14. Yankaskas BC, Haneuse S, Knapp JM, Kerlikowske K, Geller BM, Buist DSM. Performance of First Mammography Examination in Women under Age 40. J Natl Cancer Inst. 2010 May 19;102(10):692701. Epub 2010 May 3.PMID: 20439838. 15. Bowles EA, Geller BM. Understanding the best ways to provide feedback to radiologists on mammography performance. AJR Am J Roentgenol. 2009 Jul;193(1):157-64. 16. Miglioretti DL, Gard C, Carney PA, Onega TL, Buist DSM, Sickles EA, Kerlikowske K, Rosenberg RD, Yankaskas BC, Geller BM, Elmore JG.. When Radiologists Perform Best: The Learning Curve in Screening Mammography Interpretation. In press, Radiology. 17. Gallagher TH, Cook AJ, Brenner RJ, Carney PA, Miglioretti DL, Geller BM, et al. Disclosing Harmful Mammography Errors to Patients., In press, AJR. 18. Jacobs A. - Colchester Sun, various medical columns, 2005-present; Essex Reporter, various medical columns, 2005-present. 19. Kessler, R. The problem of integrating addiction in the medical home. Meeting on Addiction and the Primary Care Medical Home: Developing a research agenda. NIDA, Rockville. 20. Kessler, R. With Benjamin Miller Psy.D. A Collaborative Care Practice Base Research Network. AHRQ, Rockville. 21. Kessler R, 2010. What We Need to Know About Behavioral Health and Psychology in the PatientCentered Medical Home. Clinical Psychology Science and Practice 17: 215–217. 22. King J MD, and McCray L MD, Residency Director and Associate Residency Director respectively, presented a well-attended workshop titled “Competency-Based Criteria for Advancement: Setting Expectations to Create Success,” at the program directors’ workshop held June 6-8 in Kansas City. 23. Koutras A. , "Interview Process" - for medical students; Sept 2009 24. Koutras A., "Exercise and Pregnancy" presented at the UVM Sports Medicine Conference in Sept 2009 25. Koutras A. - “The 5-Minute Clinical Consult 2010-18th Edition, and 2010-18th Edition, Frank J. Domino, MD Editor, Chapter on Breast Abscess. March 2010. 26. Little DN, Hatch RL Proceedings of the 2009 Annual Predoctoral Education Conference of the Society of Teachers of Family Medicine. Teaching and Learning in Medicine 22:1, 60-67, 2010. 27. Peterson T. - has authored health information articles for the Colchester Chronicle 28. Romanko M. Course organizer and instructor: "Building Capacity for Agricultural Heath and Safety", held in Lake Morey, VT, April 2010. 29. Ward N. World Research Group seminars for Physician Advisors - - topics - "Front End" Case Management, Reducing Readmissions, Implementation of an Electronic Health Record. Las Vegas April 2010 21 SERVICE 1. Peterson, Thomas. 2009 - Association of Departments of Family Medicine, 2010 Annual Program Planning Committee Member. 2. Peterson, Thomas. 2008, 2009 - American Academy of Family Physicians, Vermont Delegate to National Congress of Delegates. 3. Boland, K. Drug Utilization Review Board, Member, Pharmacy Benefits Management Program, Office of Vermont Health Access (appointed by Governor of Vermont) 2007-Present. 4. Burke, Karen. Annual medical service trip to Bilwaskarma, Nicaragua. January 2010. 5. Eyler, Evan. Member of the Task Force on Gender Identity Disorder for the American Psychiatric Association, and as an APA Transformational Leadership Fellow. 6. Geller, BM, Healing Legacies, Burlington, VT: Board member, 1999- present; chair, 11/01- present. 7. Khan OA. Led workshop on Mentorship in Developing Country National Institutes of Health. 4th annual meeting of the International Association of International Public Health Institutes (IANPHI), Johannesburg, South Africa, Oct. 2009. 8. Khan OA. Travel to Bangladesh as part of student Global Health abroad elective (FM1130), 2008 and 2009. 9. King, John. Committees: University of Vermont Family Medicine Residency Education committee, chair; Blue Print for Health, Vermont, Provider Practice Committee; Family medicine leadership; Department of Family Medicine Quality assurance and improvement; Fletcher Allen Health Care Graduate Education Committee; Family medicine OB committee, Obstetrics/L&D operations committee. 10. King, John. National Ski Patrol, 1973-present. 11. King, John. Special Olympics Vermont Volunteer 2004-present. 12. Nicholas, C. College of Medicine Admission Committee- full member 2007-present 13. Nicholas, C. Ex-Officio member of the College of Medicine Advancement Committee- 2007-present 14. Nicholas, C. Assocation of Standardized Patient Educators:2006-present: Elected to Vice President of Operations for ASPE; Executive Committee Member; Grants and Research Committee member; International ASPE Committee member 15. Nicholas, C. Faculty Senate- senator for Family Practice 2004-present 16. Richardson-Nassif, K. Chair-Outstanding Service Award at the Northeast Group on Educational Affairs (NEGEA) meeting in Farmington, CT, March 2010. The inscription reads “In Recognition of your outstanding leadership and contributions to the Northeast Group on Educational Affairs.” 17. Romanko, M. Vermont AHEC Board Member and member of the AgriSafe Network (national agricultural health organization). 22 MAINE MEDICAL CENTER DEPARTMENT OF FAMILY MEDICINE GRANTS, PRESENTATIONS, PUBLICATIONS JANUARY – DECEMBER 2009 PUBLICATIONS Kligler, B. Lebensohn, P. Koithan, M, Schneider, C et al. Measuring the “whole system” outcomes of an educational innovation: experience from the integrative family medicine program. Fam Med, 2009; 41(5):342-9. Schneider, C. Segre, T. Green tea: potential health benefits. American Family Physician. 2009;79(7) 591-594. Schirmer, JM, Montegut, AJ. (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Radcliffe Publishers. October, 2009. Schirmer, JM, Ninh, L.H. Behavioral medicine: principles and practices. In Schirmer JM, Montegut AJ, (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publishers.October, 2009. Schirmer JM, Thuy B. The mind body connection: patients with somatic complaints with no organic cause. In: Schirmer JM, Montegut AJ, (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publishers. October, 2009. Schirmer JM, Green K, Huy NVQ. Behavioral change. In: Schirmer JM, Montegut AJ, (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publishers. October, 2009. Schirmer JM, Phong ND. Counseling in primary care. In: Schirmer, JM, Montegut, AJ, (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publishers. October, 2009. Schirmer JM, Holt C, Chuc NTK, Dung PH, Montegut AJ. Advancing behavioral medicine in primary care settings. In: Schirmer JM, Montegut AJ, (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publishers. October, 2009. Morrow, C., Schirmer, J. M., Nguyen, V. S. Provider well-being in primary care settings. In Schirmer, JM, Montegut, AJ. (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publisher. October, 2009. Lorenz, A., Schirmer, JM, Nguyen, KC, Nguyen, VH. Family systems in behavioral health in primary care settings. In: Schirmer, JM, Montegut, AJ. (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publishers. October, 2009. Meyer, DL, Schirmer, JM, Nguyen, MT. Social and cultural influence on health in primary care settings.In: Schirmer, JM, Montegut, AJ. (eds.) Behavioral Medicine in Primary Care: A Global Perspective. Oxford, UK: Radcliffe Publishers. October, 2009. PRESENTATIONS Braden, Colianni, Dexter and Schneider, Counterstrain in Family Medicine: a workshop. Maine Medical Center Family Medicine Residency Program. Portland, ME. January 2009. Botler J. Geriatric Grand Rounds- Transitional Care, January 2009 Dreher G. Elder Substance Abuse Psychiatry Grand Rounds Jan 27, 2009 Botler J. Medicine Grand Rounds, Care Transitions, February 2009 Schneider C. It’s only natural. Group facilitator. Maine Medical Center/University of Vermont College of Medicine Bridge Curriculum. Portland, ME. February 2009. 23 Drher G. Treating Pain in the Patient with Addiction – Palliative Care monthly seminar and Outreach Education Conference Plenary, March 2009 Schneider C. Botanicals and Dietary supplements in psychiatry. Maine Medical Center Psychiatry Residency Program/Child Psychiatry Residency Program. Portland, ME March 2009. Schneider C. Integrating CAM Intro Your Practice: Reliable Resources. American Academy of Pediatrics, Maine Chapter. Sunday River, ME. May 2009. Schneider C. Integrative Medicine. University of New England College of Osteopathic Medicine, Clown Patch Club. April 2009 Dreher G. Educating Maine Physicians in Better Chronic Pain Management - workshop at Federation of State Medical Boards annual meeting in Washington DC. Dreher G. PRISM plenary talk on Practical Motivational Interviewing Schirmer J. Share Your Work and Build Community Using STFM’s Family Medicine Digital Resources Library (FMDRL), STFM Annual Meeting, Denver, CO, May, 2009, J. Schirmer, R. Usatine, S. Burge, C. Richardson, T. Nolte Schirmer J. Core Principles of Behavioral Science: From Basics to Beyond, STFM Annual Meeting, Denver, CO, May, 2009, J. Schirmer, D. Taylor and R. Zylstra Schirmer J. Facilitation and Group Medical Visits, STFM Annual Meeting, Denver, CO, May 2009, J. Schirmer, C. Strickland, E. Shahady, and M. Talen, Schirmer J. Group Medical Visits for Patients with Chronic Pain, Maine Medical Center PRISM Conference, Freeport, ME, May, 2009, J. Schirmer and M. McDonough Bouchard M. ACSM annual meeting - Panel for Lower Extremity injuries. June 2009. Howe A. Pediatric Obesity, Obesity Symposium, Uniformed Services Academy of Family Physicians, Annual Meeting, Orlando, Florida, April 2009. Howe A. Examination of the Throwing Athlete: Moving Beyond the Shoulder American College of Sports Medicine, Annual Meeting, Seattle, Washington June 2009. Schirmer, JM, Social Work in Health Settings: Best Practices, National Conference on the Development of Social Work in Viet Nam, DaNang, Viet Nam, November, 2009 Schirmer, JM, Cross Cultural Health Care, Collaborative Family Health Care Association Annual Meeting, San Diego, CA, October, 2009 Seymour, D., Schirmer, JM, Wilson, C., Ivbijaro, G. Integration of Mental Health and Primary Health Care in Global Projects, Collaborative Family Health Care Association Annual Meeting, San Diego, CA, October, 2009 Dreher G. Ethics training with UVM students in surgery rotation; MMC Clinical Ethics Retreat copresentation on Health Care Reform issues; and Mind-Body talk with COM-CAM program (September 2009) Dreher G. “Brief Interventions” plenary session at Maine Health PRISM session; “Chronic Pain Management Addiction Issues” plenary session in Auburn with CMMC primary care physician group at request of MMA / Gordon Smith; and “Drug testing” with Michael Blanchard COO NorDx at Mercy Pain Seminar (October 2009) Schneider C. Integrative Medicine and Inflammatory Bowel Disease. Crohn’s & Colitis Foundation of America and Maine Medical Center Patient & Family IBD Symposium. Portland, ME. November 2009. Howe A. What Adolescents are Taking and Not Telling You: Performance Enhancing Substance Use in Teenagers. American Academy of Family Physicians Annual Assembly, Boston Massachusetts, October 2009. Howe A. Pediatric Sports Injuries: Challenges of the Growing Athlete. American Academy of Family Physicians Annual Assembly, Boston Massachusetts, October 2009. 24 MacQueen A, McAteer T, O'Neill D, Howe A. How to Get Injured Athletes Back in the Game: Extending Beyond the Physical Recovery. American College of Sports Medicine, New England Chapter, Providence, Rhode Island, November 2009. GRANTS Glazer JL and McAteer T. Immersion in Tepid Water as a Superior Treatment for Exertional Heat Exhaustion, MMC MRC Grant, $7,644. June 2009. Schneider, C. Osteopathic Heritage Fund 2009 $13,000 for Osteopathic Manual Medicine Precepting in for Integrative Family Medicine Project. 25 FORMAL PRESENTATIONS GRAND ROUNDS 2009-2010 September 14 ------------ The Older Shoulder John King, MD September 21 ------------ Child Sexual Abuse Exam Karyn Patno, MD September 28 ------------ Irritable Bowel Syndrome Doris Strader, MD October 5 ----------------- Keep it Simple – What Parents Need to Know or Not Amy Spangler, MN, RN, IBCLC October 12 --------------- Morbidity and Mortality Rounds Charlotte Reback, MD, Yannis Felemegos, MD October 19 ---------------- Basic EKG Interpretation and Clinical Management Robert Lobel, MD October 26 ---------------- State of Healthcare in Ethiopia Rebecca Winokur, MD November 2 -------------- Breast Masses and Common Breast Conditions Ted A. James, MD, FACS November 9 -------------- Options Counseling for Unintended Pregnancy Linda Prine, MD November 16------------- Interventional Therapies for Treating Chronic Low Back Pain Clarence Ivie III, DO, MPH November 23------------- Heel Pain Stephen Merena, DPM November 30------------- Perioperative Evaluation of Cardiac Risk – A Road to Nowhere Friederike Keating, MD December 7 -------------- Hand Injury Evaluation and Management John G. King, MD, MPH December 14 ------------- The Impaired Physician-Help is Available David John Simmons, MD, FACP December 21 ------------- Trauma from A to E Stephen M. Leffler, MD January 11 ---------------- Approaching Advance Care Planning Discussions with Seriously Ill Patients Juliet Jacobsen, MD January 25 ---------------- M & M Rounds Heather Stein, MD February 1 ---------------- The Evaluation of Hip Pain Jennifer S. Weibel, DO February 8 ---------------- Why Take the Plunge: The Benefits of Aquatic PT Natalie Bradford, PT, & Sheila Reid, PT February 22 -------------- Anemia Work-up Neil Zakai, MD March 1 ------------------- Questions and Answers about the Ambulatory PRISM Module Peter Igneri, PA-C, MMSc March 8 ------------------- M & M Rounds Terry Stein, MD 26 March 15------------------ Adolescent Substance Abuse John Koutras, MD March 22------------------ Stress: Health and Healing Stephen Mann, MD March 29------------------ Medical Hazards of the Nuclear Age and the Necessary Changes in Human Behavior to Stop Environmental Destruction Helen Caldicott, MD April 5 --------------------- Helping in Haiti – Perspectives from Family Medicine Jean Andersson-Swayze, MD April 12 ------------------- Alaska: Frontier Medicine Sarah Davies, MD April 19 ------------------- Hip and Knee Care 2010 David Halsey, MD April 26 ------------------- Occupational Medical Issues for Farmers and Farmworkers John May, MD May 5 ---------------------- Innovations in Medical Education Patricia Carney, PhD May 10 -------------------- Anticoagulation in the Elderly Nathan B. Adams MS, MT (ASCP) May 17 -------------------- Health Care Policy in an Aging America John B. Murphy, MD May 24 -------------------- Colorectal and Prostate Cancer Screening and Medical Malpractice Justin Karlitz-Grodin, MD Attacking Obesity in Just 15 Minutes Yannis Felemegos, MD; Michael Graham, MD; June 7 ---------------------- Authentic Clinical Assessment for Medical Students: The Integrated Standardized Patient Exam Andrea Manyon, MD June 14 -------------------- Influenza – What Happened, What to Expect? Thomas Peterson, MD June 28 -------------------- AED Program Implementation in Schools Craig Sillick, MD The Uninsured Farm Worker Clinic Meera Ramachandran, MD 27 2009-2010 TEACHING CONTRIBUTIONS Allyson M. Bolduc, MD Residency Attending Faculty Doctoring in Vermont, Preceptor Faculty Mentor to Family Medicine Residents Co-Leader for Balint Group for Residents Residency Balint Group Coordinator Director, Annual Family Medicine Review Course CME Committee Karen H. Burke, MD 10 Geriatrics lectures to the residents/year. Supervise the Wake Robin portion of the 3rd year geriatrics rotation Resident Geriatric education coordinator.VIC Generations block, Senior Housing alternatives and Geriatric interviewing. VIC International Health Bridge, evolution of my own medical volunteer work. John C. Ferguson, MD Medical Director, Milton Family Practice Residency Attending Faculty Doctoring in Vermont, Preceptor Third and Fourth Year Clerkship Preceptorship Candace L. Fraser, MD Teaching - clinical precepting for 1st - 4th year medical students at CFP as part of their DIV, Clerkship and 4th yr elective rotations TA for all 3 years of FM residents at MFP Oct ’09 to present – Course Director for Clerkship FM Bridge Course on skin procedures/suturing and musculoskeletal Exam Committee –Medical Director CFP 1/09 to 09/30/09 – which included Blue Print for Chronic Care Committee, and the Quality Assurance Committee and the PRISM role out committee Clerkship Director for FM 10/09 to present Kimberly A. Hageman, MD Residency Attending Faculty Doctoring in Vermont, Preceptor Coordinator/provider – MFP Women’s Health Procedure Clinic Residency Advisor Program Clerkship Preceptor OB Preceptor/Antepartum OB Audits presenter Charles L. Hulse, MD, PhD Inpatient and outpatient (Milton) preceptor (medical students and residents) Ecosystem Change and Human Health 4th year medical student elective 28 MSLG 1 group project on Environmental Health Community Medicine projects Alicia Jacobs, MD Doctoring in Vermont Preceptor Third and Fourth Year Clerkship Preceptor Educational Sessions presenter Grand Rounds presenter Medical Director - Colchester Family Practice Kristopher Jensen, MD Residency Attending Faculty Third and Fourth Year Clerkship, Preceptor Doctoring in Vermont, Preceptor John G. King, MD, MPH Residency Program Director Residency Attending Faculty Anya Koutras, MD Teaching Attending for the inpatient FMS Teaching Attending on OB (L&D) Weekly Preceptor at Milton Family Practice Monthly Didactic Lecturer on Maternal Child Health Advisor to 3 residents currently Lecturer in Generations Course (“Breastfeeding”) Small Group Facilitator in Attacks and Defenses Course Director for Family Medicine AI on FMS 4th year Advanced Integration Director for Family Medicine (overseeing other 4th year electives in Family Medicine, including Reading Month, Preceptorship) Core Faculty and Advisor for 4th year elective Lactation Management Medical Student Advisor to 14 medical students currently Faculty for 3rd year Family Medicine Clerkship Faculty for DIV Lise Kowalski, MD Doctoring in Vermont, Preceptor Third and Fourth Year Clerkship, Preceptor Residency Attending Faculty David N. Little, MD Third Year Clerkship Director through 9/09 Residency Attending Faculty / Mentor Third Year/Fourth Year Advisor Predoctoral Committee FMIG, Faculty Advisor 29 Robert A. Luebbers, MD Medical Director, South Burlington Family Practice Third and Fourth Year Preceptor Residency Attending Faculty Faculty mentor to FP Residents Doctoring in Vermont, Preceptor Laura McCray, MD Teaching- doctoring in Vermont Weekly inpatient chalk talk series every Friday Associate Director residency program Thomas C. Peterson, MD Interim Chair, Department of Family Medicine Vice Chair for Clinical Operations Residency Attending Faculty Third Year Clerkship, Preceptor Fourth Year Preceptorship Hospital Rounding Instructor Allan M. Ramsay, MD Third Year Clerkship, Preceptor Fourth Year Preceptorship Residency Attending Faculty Director, Family Medicine Inpatient Service, FAHC Medical Director at Palliative Care Service, FAHC Charlotte Reback, MD Medical Director, Walk-In Care Clinic Physician and Society, Group Leader Medical Interviewing Skills, Group Leader Doctoring in Vermont Medical Student Leadership Group Residency Attending Faculty Course Director for Generations Karen Richardson -Nassif, PhD Bridge Clerkship, Group Discussion Leader Family Medicine/Pediatrics/Internal Medicine Bridge – Intimate Partner Violence WorkshopCoordinator and Group Discussion Leader Foundations Advisor Medical Student Leadership Group Medical Student Scholarly Project Introduction to Clinical Decision Making Martha P. Seagrave, PA-C, BSN Director of Predoctoral Programs in Family Medicine Associate Clerkship Director in Family Medicine Medical Student Advisor 30 Family Medicine Interest Group Faculty Advisor Family Medicine Underserved Course Director--Advanced Integration Course Medquest Advisor Bridge Instructor Fourth Year Preceptor Clinician, UVM Center for Health and Wellbeing Center for Health and Wellbeing Electronic Health Record Implementation Leader Michael Sirois, MD Teaching attending TA in Milton Hospital attending Family Medicine Clerkship third year medical students – SBFP Doctoring in Vermont Dale D. Stafford, MD Doctoring in Vermont, Preceptor Third and Fourth Year Clerkship, Preceptor Residency Attending Faculty Norman S. Ward, MD Family Medicine Clerkship third year medical students – SBFP Daniel Weinstein, MD Residency Attending Faculty DIV Student Mentor Stuart E. Williams, MD Doctoring in Vermont, Preceptor Third and Fourth Year Clerkship, Preceptor Residency Attending Faculty Risk Management Committee at CVMC TA Milton Family Practice 31 COMMITTEE SERVICE THE UNIVERSITY OF VERMONT / FLETCHER ALLEN HEALTH CARE Allyson M. Bolduc, MD 1998-present Member, the UVM Medical School Admissions Committee (Interviewer and Reviewer) 2003-present Member, QA&I Committee Karen Burke, MD COM Faculty Advancement and Promotion (Faculty Standards) VNA Physician Advisory Council Vermont Farm Health Task Force Medical Volunteer work in Bilwaskarma, R.A.A.N., Nicaragua David Lisle, MD Sports medicine and orthopaedic curriculum for the family medicine residents. Clearinghouse Committee for the FAHC faculty practice. Brian S. Flynn, ScD 1999-present. Director, Office of Health Promotion Research, College of Medicine, University of Vermont. 1999-present Program Leader for Cancer Prevention and Control, Vermont Cancer Center, College of Medicine, University of Vermont 2002- present Chair, State of Vermont, Tobacco Evaluation & Review Board 2005-2010 Board of Directors and Vice-Chair, Vermont Public Health Association, 2006-present Planning Committee, Center for Clinical and Translational Science, University of Vermont 2006-present Site visit review committee member, University of Minnesota Cancer Center P30 renewal application, for the National Cancer Institute Candace Fraser, MD 1996-present Residency Candidate Review Committee 1998-present Committee for Primary Care Teaching Awards 2003 to present Medical Director, Colchester Family Practice 2003-present Quality Assurance Committee 2003-present Operations Committee 2007-present Vermont Blueprint Team Charles L. Hulse, MD, PhD 1999-present Member, Pharmacy and Therapeutics Committee, FAHC Committee Service Medication Safety Subcommittee (of P&T Committee) UVM Trans-disciplinary Research Initiative – Complexity Subcommittee Alicia Jacobs, MD Committee Member - Vermont Practitioner Health Program - Vermont Medical Society 32 John G. King, MD 2004-present Special Olympics Volunteer 2004-present Member, Vermont Blueprint for Health Committee 2004-present Member, FAHC Obstetrics Operations Committee Anya Koutras, MD Committee Service 2009: Newborn QA Breastfeeding Task Force Maternal Child Coalition Vermont Lactation Consultant Association Conference Committee Dept of Health Committee on Breastfeeding David N. Little, MD 1994-present UVM College of Medicine, Clerkship Course Directors Committee 1995-present Family Medicine Clerkship Director 2009 Board member, Vermont Academy of Family Physicians 2006-present STFM Predoctoral Director Institute, Steering Committee 2007-present STFM Education Committee Robert A. Luebbers, MD Member, Family Medicine Credentials Committee Thomas C. Peterson, MD Community Benefits Advisory Committee, Fletcher Allen Health Care 1993-present Member, Anti-Infective Committee Volunteer Community Health Center Burlington during “Free Clinic Day” Jon K. Porter, MD Current Task Force on Attention Deficit Disorders Current Alcohol and Drug Resource Team 1998-present Co-Chair, Center for Health and Wellbeing Quality Improvement Committee Allan M. Ramsay, MD 1993-present 1995-present 1995-present 1996-present 1997-present Medical Director, Green Mountain Nursing Home Member, Dept. of Family Medicine, Credentials Committee Member, Dept. of Family Medicine, Quality Assurance Committee Member, FAHC, Wellness Committee Member, Board of Directors, Community Health Center, Burlington, VT Charlotte A. Reback, MD 2001-present Chairperson FAHC Family Practice Health Care Service, Quality Assurance and Improvement Committee 2006-present Director Family Medicine Morbidity and Mortality Grand Rounds Martha Seagrave, PA-C, BSN 2000-present Member, UVM College of Medicine, Clerkship Course Directors Committee 33 2002-present Member, Primary Care Bridge Committee 2002-present Member, ADD Task force, Center for Health and Wellbeing 2003-present Member, ADRT Team, Center for Health and Wellbeing 2005-present Member and List Owner, Society of Teachers of Family Medicine Group on On-line Cases 2005-present Member, Planning Committee Society of Teachers of Family Medicine Northeast Regional Meeting 2007-present Project Leader for Selection and Implementation of HER at Center for Health and Well-being Norman S. Ward, MD Committees: FAHC Med Staff Credentials, Bylaws, Utilization Review, Quality Assurance and Improvement, Medical Records FAHC RAC Work Team FAHC Education Subcommittee FAHC Plan of Care/Assessment Subcommittee FAHC Standards of Operation FAHC Quality Committee FAHC Safety Committee FAHC CMI Improvement Task Force FAHC Prism/Joint Commission Compliance Committee FAHC EDRS/PROD Implementation Committee FAHC Faculty Practice Orientation Task Force FAHC Organization Ethics Committee FAHC Touch Point Committee UVM COM Family Medicine Chair Search Committee State of Vermont - BISHCA Utilization Study Program State of Vermont - Medicaid Drug Utilization Review Board FAHC Prism Physician Advisory Committee FAHC Plan of Care/Assessment Subcommittee CENTRAL VERMONT MEDICAL CENTER Kristopher Jensen, MD Member, Credentials Committee Lise Kowalski, MD DSCU Committee (Intensive Care Unit Committee at CVH) Morbidity and Mortality Committee Stuart E. Williams, MD President Elect, VT Chapter AAFP 2002-present Member, Risk Management Committee, Central VT Medical Center 2002-present Member, Physician Council, VM 2006-present Co-Chair, Appropriate Care Committee, CVMC 34 FACULTY / PROVIDERS Providers Specific Roles/Location Kathleen Boland, PharmD Clinical Associate Professor Milton Family Practice Allyson M. Bolduc, MD Clinical Assistant Professor South Burlington Family Practice Kristin Burdick, MD Clinical Assistant Professor Colchester Family Practice Timothy Burdick, MD Assistant Professor Berlin Family Health Karen H. Burke, MD Clinical Associate Professor Medical Director, Wake Robin Life Care Retirement Community South Burlington Family Practice Whitney Calkins, MD Assistant Professor South Burlington Family Practice Eileen CichoskiKelly, PhD Research Assistant Professor Instructional Designer, Office of Medical Education, Vermont Integrated Curriculum Robert Davidson, PA-C Clinical Instructor Berlin Family Health John Ferguson, MD Clinical Associate Professor Milton Family Practice Brian S. Flynn, ScD Research Professor Director, Office of Health Promotion Research Candace L. Fraser, MD Associate Professor Director, Family Medicine Clerkship Colchester Family Practice Berta M. Geller, EdD Research Professor Office of Health Promotion Research Melisa Gibson, MD Clinical Assistant Professor Milton Family Practice Kimberly Hageman, MD Clinical Assistant Professor Milton Family Practice 35 Charles L. Hulse, MD, PhD Associate Professor Director, Vermont Program on Ecology and Health Director, Research and Scholarship Program Joanne Hunt, NP Colchester Family Practice Alicia Jacobs, MD Clinical Assistant Professor Medical Director Colchester Family Practice Kristopher Jensen, MD Clinical Assistant Professor Berlin Family Health Director, Senior Selective Programs John G. King, MD, MPH Associate Professor Director, Family Medicine Residency Program Milton Family Practice Anya Koutras, MD Assistant Professor Colchester Family Practice Lise Kowalski, MD Clinical Assistant Professor Berlin Family Health David Lisle, MD Clinical Assistant Professor South Burlington Family Practice David N. Little, MD Associate Professor Director, Family Medicine Clerkship Milton Family Practice Robert A. Luebbers, MD Clinical Assistant Professor Member, Family Medicine Credentials Committee Nancy Morris, PA Clinical Instructor Colchester Family Practice Laura McCray, MD Clinical Assistant Professor Associate Director, Family Medicine Residency South Burlington Family Practice Catherine Nicholas, PA-C Clinical Instructor Director of Standardized Patient Program Office of Medical Education Charles Osler, NP Clinical Instructor Walk-In Care Center Sahir Patel, MD Clinical Assistant Professor Colchester Family Practice Anne Pelkey, PA Clinical Instructor South Burlington Family Practice Thomas C. Peterson, MD Professor Interim Chairman, Department of Family Medicine Family Medicine Health Care Service Fletcher Allen Health Care 36 Maria Puglisi, RN, NP Clinical Instructor Berlin Family Health Allan M. Ramsay, MD Professor Vice Chair of Academic Affairs Colchester Family Practice Charlotte Reback, MD Clinical Assistant Professor Medical Director, Walk-In Care Center Fanny Allen Campus Karen Richardson-Nassif, PhD Research Associate Professor Associate Dean for Faculty and Staff Development Diversity Monica Romanko, MD Clinical Assistant Professor Associate Director, Family Medicine Residency Milton Family Practice John J. Saia, MD Associate Professor Emeritus Milton Family Practice & Colchester Family Practice Martha Seagrave, PA-C, BSN Research Associate Director of Predoctoral Programs in Family Medicine Family Medicine Staff Clinician, Center for Health and Well Being (UVM Student Health Center) Charles Schmitt, MD Clinical Assistant Professor Walk-In Care Center Michael Sirois, MD Clinical Assistant Professor South Burlington Family Practice Caroline Slimovitch, MD Clinical Assistant Professor South Burlington Family Practice Laura Solomon, PhD Research Professor Emerita Office of Health Promotion Research Marga Sproul, MD, MS Associate Professor Associate Dean for Student Affairs (Retired, August 2004) Colchester Family Practice Dale Stafford, MD Clinical Assistant Professor Berlin Family Health Deborah Thompson, PA-C Clinical Instructor Colchester Family Practice Norman S. Ward, MD Associate Professor South Burlington Family Practice 37 Daniel Weinstein, MD Clinical Assistant Professor Walk-In Care Center Stuart Williams, MD Clinical Assistant Professor Medical Director, Berlin Family Health Jeri Wohlberg, NP Clinical Instructor Walk-In Care Center John K. Worden, PhD Research Professor Emeritus Office of Health Promotion Research 38 RESIDENTS & 2010 GRADUATES First Year: Medical School: Ewa Dziewiecka Karen Fromhold Jennifer Kaufman Michelle Paavola Aaron Reiter Jagiellonian University University of Vermont Saint-George’s University University of Vermont Sackler School of Medicine Second Year: Medical School: Heather Doyle Stein Alicia Guilford Rachel Humphrey Debbie Lieber Ben Newton Terry Stein Marie Walsh West Virginia University University of Vermont University of Vermont University of Arkansas Ross University West Virginia University University of Missouri Third Year: Medical School: Sarah Davies Yannis Felemegos Mick Graham Justin Karlitz-Grodin Meera Ramachandran Craig Sillick Georgetown University Windsor University New York University SUNY Downstate College of Medicine Louisiana State University University of Maryland June 30, 2010 Graduates: Practice Site: Sarah Davies Green Mountain Family Practice, Norwich, VT Community Health Center, Cornwall, Ontario Addison Family Medicine in Middlebury, VT Central Vermont Primary Care in Berlin, VT VA primary locum tenens program in Baton Rouge, Louisiana F.F. Thompson Hospital, Canandaigua, NY Yannis Felemegos Mick Graham Justin Karlitz-Grodin Meera Ramachandran Craig Sillick 39 VERMONT PART-TIME FACULTY Jean Anderson-Swayze, MD Debbie Atkinson, MD Lorne Babb, MD Sheilla Bachelder, MD Robert Backus, MD Richard Baker, MD James Bergmann, MD Richard Bernstein, MD Paul Bertocci, MD Donald Bicknell, MD Kathleen Boland, PharmD Allyson Bolduc , MD Kenneth Borie, DO Marian Bouchard, MD David Bourgeois, MD Stephanie Briggs, MD John Brooklyn, MD Kimberly Bruno, MD Karen Burke, MD Joseph Capobianco, MD Harry Chen, MD C. Edward Clark, MD David Coddaire, MD John Conlon, DO Francis Cook, MD Timothy Cope, MD Michael Corrigan, MD William Cove, DO Marcus Coxon, MD William Craig, MD Ruth Ann Crose, MD Kevin Crowley, MD Barbara Dalton, MD Sarah Davies, MD Pamela Dawson, MD Laurel Decher, MD Mary Dill, MD Rachel DiSanto, MD Joyce Dobbertin, MD Jeffrey Dodge, MD H. Daniel Donnelly, MD Richard Dooley, PA Marjorie Douglass, FNP Therese Dranginis, MD Robin Edelman, RD Vivian Esparza, MD Dorothy Federman, MD Yannis Felemegos, MD John Ferguson, MD Jan Ferris, DO William Fifield, MD Sharon Fine, MD Ann Fingar, MD Patricia Fisher, MD George Fjeld, MD Angela Gatzke, MD Argilla George-Reynolds, MD Michele Gerin-Lajoie, MD Maurice Geurts, MD Cathleen Gleeson, PhD Ann Goering, MD Daniel Goodyear, MD Mick Graham, MD Alicia Guilford, MD Kimberly Hageman, MD John Hartmann, MD John Hearst, MD David Hobbs, MD Mark Hoffman, MD Cheri Holton, MSN Rachel Inker, MD Alicia Jacobs, MD Yumi Jarris, MD Kristopher Jensen, MD Michael Johnson, MD Andrew Kaplan, MD Justin Karlitz-Grodin, MD Richard Katzman, MD Robert Keith, MD Omar Khan, MD Philip Kiely, MD Dayle Klitzner, MD Anne Knott, MD Lise Kowalski, MD Dana Kraus, MD Lisa LaCarrubba-Blondin, MD Erick Lavallee, MD John Lawlis III, MD Melanie Lawrence, MD Yoland Lawrence, MD 40 Mark Lichtenstein, MD Moss Linder, MD Robert Luby, MD Robert Luebbers, MD Edd Lyon, MD John Macy, MD Stephen Mann, MD Jeffrey Martin, PhD John Matthew, MD Laura McCray, MD Louise McDevitt, FNP Sharon McDonnell, MD Michael McNamara, MD John McPartland, DO, MS Mark Messier, MD Donald Miller, Jr., MD Sarah Morgan, MD Robert Murray, MD Terence Naumann, MD Elizabeth Newman, MD Laura Norris, MD Robert Orr, MD Lee Orsky, PA W. Mark Peluso, MD Robert Penney, Jr., MD Yvette Pigeon, EdD Jon Porter, MD S. Hannah Rabin, MD Meera Ramachandran, MD Barbara Raskin, MD Mary Ready, MD Charlotte Reback, MD Andrea Regan, MD Paul Reiss, MD John Reynolds, MD Diane Rippa, MD Kevin Rodgers, MD Paul Rogers, MD Jessica Rouse, MD Margaret Russell, PA-C Toby Sadkin, MD Susan Saferstein, MD Linda Sanborn, MD Charles Schmitt, MD Elizabeth Schneider, MD Clinton Seger, MD Timothy Shafer, MD Susan Shane, MD Craig Sillick, MD Michael Sirois, MD Caroline Slimovitch, MD Christine Staats, MD Dale Stafford, MD Daniel Steinbauer, MD Miriam Sturgis, MD Craig Sullivan, MD Carol Thayer, MD Deborah Thompson, PA-C Robert Tortolani, MD Mattie Towle, MD Ronald Vallario, MD Gary Waring, MD Wayne Warnken, MD Daniel Weinstein, MD Joanna Weinstock, MD Lee Weisman, MD Lynn Wilkinson, MD Stuart Williams, MD Jennifer Willingham, MD Rebecca Winokur, MD Jeffrey Wulfman, MD Maja Zimmerman, MD MAINE PART-TIME FACULTY Jeffrey Aalberg, MD Douglas Aiken, MD Peter G. Amann, MD Steven Barter, MD Charles Belisle, MD Lisa Belisle, MD Francis Bellino, MD Michael Bither, MD Laura Blustein, MD Cameron Bopp, MD Mark Bouchard, MD Kathryn Bourgoin, MD Donna J. Carr, DO Phillip A. Carter, MD Cynthia Cartwright, MS Nichole Cherbuliez, MD Patrick Connolly, MD Catherine Crute, MD Stephen Cummings, MD Peggy Cyr, MD Marcus Deck, MD Joseph deKay, DO Charles DeSieyes, MD William Dexter, MD Mary Dowd, MD Rebecca Fried, MD Daniel Friedland, MD Christine Gates, MD Pamela Gardiner, MD James Glazer, MD James Haller, MD Louis Hanson, DO James Harper, MD Hugh Harwood, MD David Haskell, MD Victoria Hayes, MD Christina Holt, MD Wesley Johnson, MD Stephan Kirsch, MD Burton Knapp, MD Neil Korsen, MD David Loxterkamp, MD Cydney Mahoney, MD Scott Marr, MD Richard Marino, MD Stephen Martin, MD 41 Kathleen Mcgarr, MD George McNeil, MD Alain Montegut, MD Kristy Murray-Pulsifer, DO Jeffery Patch, MD Stephen Paulding, MD Daniel Pierce, MD Jeffrey Ray, DO Challa Reddy, MD Usha Reddy, MD Deborah Rothenberg, PhD Jeffrey Saffer, MD Allison Samitt, MD Julie Schirmer, LCSW Craig Schneider, MD Kristen Silvia, MD Ann Skelton, MD Michael Stadnicki, MD Meagan Staton, MD Steven Stein, MD David Strassler, MD Frederick VanMourik, MD Lisa Wendler, MD STAFF UVM ACADEMIC OFFICE, ROWELL 235 Susan Weber-Flynn, Department Administrator Emira Smailagic, Front Desk, Assistant to the Chair Administrative/Financial Assistant Kathryn Beaudry, Predoctoral Education Coordinator Penilee Saulnier, Grant Coordinator FAHC, HCS LEADERSHIP TEAM Randy Messier/David Serle, Director, Family Medicine and PC/IM Kathy Perez, Operations Specialist Suzanne Lee, Executive Administrative Assistant BERLIN FAMILY HEALTH Nursing Staff Office Staff MaryHelen Bayerle, RN Bonnie Benoit, RN Heather Coletti, LPN Cathy Craige, RN Averil Dunham, LPN Kelly Hanley, LPN Lori Hoskins-Deharak, LPN Chantelle Safford, RN Sharon Williard, LPN Mark Bailey, PSS Manon Cote, HIM Michelle Dickinson, PSS Lesley Dinesen, PSS Susan Duprey, PSS Sheila Fraser, PSS Diane Fusco, HIM Ginny Himmelsbach PSS Linda Kilburn, PSS Tammy Lenentine, HIM Donna Poitras, PSS Ellen Young, Certified Professional Coder Rhodelene Premont, OSS Clinical Practice Supervisor Patrick Clark 42 COLCHESTER FAMILY PRACTICE Nursing Staff Office Staff Cynthia Baranski, MA Julie Bergeron, LPN Kim Cronin, RN Lynn Heffelfinger, LPN Lauren Higgins, MA Erica Lyons, MA Jan Messina, LPN Cheryl Rogers, LPN Alyce Brouillard, PSS Amy Bushey, Referral Specialist Nicole Couture, PSS Sue Groff, HIM Margaret Kimball, HIM Clerk II Jeannine Kneeland, HIM Virginia Lawrence, PSS Victoria Mitchell, PSS Jamie Morrison, PSS Nancy Morse, PSS Shelley Pariseau, PSS Kayleigh Shappy, PSS Mental Health Counselors Judith Gerber, PhD Angela Paoli, LICSW Clinical Practice Supervisor Donna Kaynor MILTON FAMILY PRACTICE Nursing Staff Office Staff Shelley Billings, LPN Laura Campo, RN Dori Fredette, RTR/CMA Carri Gale, LPN Barbara Miller, RN Kathy Reilly, RN Theresa Sadlier, LPN Monique Van Leuven, LPN Cecile Vosburg, LPN Michelle Wright, LPN Holly VanWinkle, LPN Patricia Armstrong, CPC Jeanette Baylis, HIM Clerk II Randi Beauchemin, PSS Heather Hawkins, PSS Holly Jamison, PSS Kelly Lavery, PSS Tara Libby, PSS Sarah Maloney, PSS Rose Myers, PSS Jessica Ploesser, HIM Clerk II Angela Rollins, PSS Kim St. Hilaire, PSS Valerie Tatro, PSS Residency Program Coordinator Mental Health Counselor Clinical Practice Supervisor Jennifer Wilson Louise George, LICSW Residency Education Coordinator Research Project Assistant Lise Vance Amy Danielson 43 SOUTH BURLINGTON FAMILY PRACTICE Nursing Staff Mental Health Counselor Heidi Bean, RN Kristina Danaher, MA Louise Greco, LPN Paige Jipner, MA Donna Langdeau, LPN Joann Mogielnicki, RN Victoria Provost, MA Nancy Racine, LPN Kate Morrissey, LCMHC Office Staff Jill Chagnon, PSS Suzanne Cooper, PSS Kim Laurie, PSS Sonya Martin, PSS Maureen Moffett, HIM Lisa Thompson, Transcription Wendy Tatro, PSS Karen Trayah, PSS Clinical Practice Supervisor Charleen Tuthill WALK-IN CARE CENTER Nursing Staff Office Staff Adam Boise Nancy Boutin, RN Donna Butkus, RN Geralyn Carpenter, RN Leslie Goldring, Radiology Joyce Guillemette, RN Francine Hughes, RN Julia Jacques, LPN Judie Jerger, LPN Mary Jane Lamare, LPN Danielle Latreille, RN Kasey Lyman, MA Lisa Middleton, RN Danielle Picarello, MA Medora Plimton, RN Cynthia Senical, RN Judy Theoret, RN Brian Thompson, Radiology Carol Tifft, LPN Claire Truso, RN Danijela Vujanovic, MA Judy Bailey-Relyea Catherine Bombardier James Cueto Kathy Fernald Allston Gilmond Jeanne Gosselin, CPC Patricia Martines, CPC Sherri A Pierce Kerry Rice Wanita Weeks Samuel Yanulavich Clinical Practice Supervisor Tammy Yohn/Keven Eriksen 44