Nogales, Samantha - American Academy of Optometry

Bilateral Central Retinal Vein Occlusion Leads to the Diagnosis of
Waldenstrom’s Macroglobulinemia
Resident: Samantha L. C. Nogales, OD
Attending: Amy Grimes, OD, FAAO
ABSTRACT:
Concurrent bilateral CRVO with no known associated underlying systemic condition at presentation will be discussed. The diagnosis of Waldenstrom’s macrogobulinemia was later revealed.
I.
CASE HISTORY
Patient Demographics and Chief Complaints: 74-year-old Caucasian male, new to the clinic, presented with a complaint of gradually declining distance and near vision OU over the past six months. Current glasses are
1.5 years old and he felts that they needed updating.
Ocular History: Non-contributory
Medical History: Gout, Anemia, Impaired fasting glucose, DJD/chronic back pain, GERD, Hypertension, Asthma, Obesity
Medications: Acetaminophen 500mg/Hydrocone 5mg 1 tab po TID;
Albuterol HFA 90mcg/dose 6.7gm inhaler po Q4H/PRN; Colchicines
0.6mg po BID; Lisinopril 40mg 1 tab po daily; Omeprazole 20mg 1 cap po daily
Allergies: beta-lactams antimicrobials
Other: Reported dizziness and gait instability with overall fatigue for the past several months
II.
PERTINENT FINDINGS:
Clinical findings:
BCVA:
OD +1.00 +1.50 x 174 20/50
OS +1.00 +1.50 x 004
Pupils: (3/3) RRL (2+/2+), No APD
20/40-1
Confrontations: Full to Finger Counting OD, OS
Slit Lamp Examination: unremarkable other than mild cataract OU
Applanation Tonometry: (Fluress/mmHg) 23/23 @ 9:35am
Gonioscopy: OU cilliary body band 360
/ no peripheral anterior synechae, no neovascularization of the angle/ slightly
bowed approach/ 1+ pigment
Pachemetry: OD 633/ OS 619
Dilated Fundus Exam
Vit OD PVD
OS PVD, mild peripheral asteroid hyalosis
C/D OD 0.4 round, full pink rim, distinct margins, no edema
OS 0.4 round, full pink rim, distinct margins, no edema
Mac OD diffuse central thickening w/ scattered dot hemorrhages, mild surrounding pigment mottling
OS diffuse central thickening w/ petalloid, surrounding pigment
PP mottling, few dot hemorrhages
OU diffuse dot/blot hemorrhages w/ a few flame hemorrhages in all four quadrants extending to the periphery
Ves OU A/V 1:4, marked venous beading w/ dilated & tortuous
veins, arterial attenuation, no cotton wool spots
Peri OU no tears/holes/breaks; scattered dot/blot hemorrhages 360
in mid periphery extending to periphery
OCT Cirrus Macular Cube:
OD CT: 590; diffuse retinal thickening (> inferior) and low intraretinal reflectivity consistent w/ intraretinal fluid accumulation and edema
OS CT: 524; diffuse diffuse retinal thickening (> inferior) and low intraretinal reflectivity consistent w/ intraretinal fluid accumulation and edema
Physical Findings:
Blood pressure: 136/74
HbA1c: 6.2
Pulse: 91
Temperature: 98 F [36.7 C]
Respiration: 16
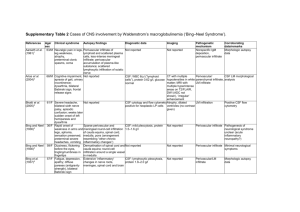
Laboratory Tests:
PROTN
EGFR
Potassium
11.6 High
40 Low
Range 6.0 – 8.0
Range >= 60
Units g/dL
Creatinine
Urea Nitrogen
Calcium (serum) 11.1 High Range 8.4 – 10.2 Units mg/dL
Magnesium
5.8 High
1.7 High
60 High
3.1 High
Range 3.5 – 5.5
Range 0.7 – 1.4
Range 5 – 20
Range 1.5 – 2.6
Units mEq/L
Units mg/dL
Units mg/dL
Units mg/Dl
TOTAL PROTIEN 11.4 HIGH Range 6.0 – 8.0 Units g/Dl
WBC
RBC
3.3 Low Range 4.5 – 11.0
1.99 Low Range 4.7 – 6.1
Hemoglobin 7.4 Low Range 14 – 16
Units #x1000/Ul
Units million/uL
Units g/dL
Diagnosis: Bilateral central retinal vein occlusion w/ chronic macular edema OU secondary to Waldenstrom’s Macroglobulinemia
Hematocrit 21.0 Low Range 40 – 52
MCV 105.6 High Range 80 – 99
Units %
Units fL
MCH
Platelets
37.5 High
72 Low
Range 27 – 31
Range 150 – 400
Neutrophil 70.3 High Range 36 – 68
Units pg
Units #x1000/uL
Units %
Alpah-1 Globulin 0.2 Low
Beta Globulin 0.5 Low
Gamma Globulin 7.6 High
M – Protein 7.0 High
Range 0.3 – 0.5
Range 0.6 – 1.1
Range 0.7 – 1.6
Units g/dL
Units g/dL
Units g/dL
Units g/dL
SERUM VISCOSITY >4.6 High Range 1.1- 2.0 Units mPa.s
IgM 2218 High Range 40 - 250 Units mg/dL
Other Tests:
Bone Marrow Biopsy: Lymphoplasmacytic lymphoma/ Waldenstrom’s
Macroglobulinemia
IVFA was scheduled but the patient declined to have the test preformed
III.
DIFFERENTIAL DIAGNOSIS
Leading ocular diagnosis:
Bilateral Non-ischemic CRVO: Referral to PCP for systemic workup to r/o hypervicosity syndrome
Other ocular diagnosis:
Concurrent venous stasis retinopathy OU
Borderline Ocular HTN with thick CCT
Mild Cataract OU
Leading medical diagnosis:
Waldenstrom’s Macroglobulinemia
Other differential medical diagnosis:
IgM monoclonal gammopathy
Lymphoplasmacytic lymphoma
Small lymphocytic lymphoma
IV.
DIAGNOSIS AND DISCUSSION
Waldenstrom’s Macroglobulinemia (WM) is hemotologic cancer characterized by a combination of bone marrow infiltration by lymphoplasmacytic lymphoma and IgM monoclonal gammopathy. Incidence of
WM is approximately three per million people per year
1,2
and accounts for approximately 2% of hematolitic cancers.
3
WM is more common in Caucasians with African-Americans and patients of Mexican decent accounting for about five percent of all cases.
4,5
Age of onset usually varies between 63 and 68 years with
55% or greater being males.
4,6
The etiology of WM is unknown but some studies have shown a familial predisposition present in approximately 20 percent of cases.
7-12
The most common complication related to WM is hyperviscosity syndrome and is seen in approximately 30 percent of patients.
13
Hyperviscosity syndrome usually always occurs with in patients who have under lying lymphoma and is caused high levels of circulating IgM.
3 Symptoms of hyperviscosity include fatigue, dizziness, vertigo, ataxia, blurred vision, diplopia, tinnitus, sudden deafness, and easy bleeding of mucus membranes. In approximately 34 percent of cases hyperviscosity causes funduscopic abnormalities including dilated, tortuous retinal veins with a “sausage link” appearance, retinal hemorrhages, exudates, papilledema,
14
central retinal vein occlusion,
15-17
and serous macular detachments.
18,19
Other complications from WM include cryoglobulinemia, cold agglutinin anemia, neuropathy, glomerular disease, amyloidosis, and tumor infiltration in to bone marrow, lymph nodes and the spleen.
20,21
V.
TREATMENT AND MANAGEMENT
This patient was admitted to VA hospital for symptoms of hyperviscosity and was treated with 2 cylces of plasmapheresis, as well as a transfusion of 8 units of pRBC’s for symptoms of anemia. At the time of admission, the patient was also treated for acute renal failure likely secondary to paraproteinemia, with
Kayexalate and was also given IV fluids. The patient was then discharged to the palliative care unit and was started on cycle 1 of chemotherapy with Rituximab
375 mg/m2 on day 1 plus Cladribine 0.12 mg/kg for five days. Fluconazole
200mg po daily, Acyclovir 400mg po BID, and Dapsone 100mg po daily were given for infection prophylaxis.
Chemotherapy was well tolerated but on the fifth day of treatment the patient developed some mild lightheadedness, hot flashes, and nausea. A degree of myelosuppression was noted after treatment but not more than would expected with the underlying disease and chemotherapy treatment (cladribine is nucleoside analog and can result in prolonged myelosuppression). IgM was markedly decreased from 7 g/dL to 3.6 g/dL and serum viscosity was stable at 1.4 which was also decreased from >4.6. After a few more days the patient was discharged and scheduled to return in 3 weeks for Cycle 2 of chemotherapy. Four cycles of chemotherapy are anticipated with a seven-day inpatient stay for each cycle. An optometry follow up with dilated fundus exam and repeat Cirrus macular cube is to be scheduled during Cycle 3 of chemotherapy. The patient was advised to continue prophylactic infection control with the above named medications for a
six-month minimum and a SPEP, serum viscosity, and beta-2 microglobulin were ordered to be taken prior to the next cycle of chemotherapy.
Treatment for Waldenstrom’s Macroglobulinemia is meant to improve quality and duration of life while minimizing side effects. Among the treatments that are available there is not a specific treatment that is considered a first-line therapeutic agent for WM so choices must be made on individual basis.
22 The main treatments for WM include alkylating agents (chlorambucil, cyclophosphamide, melphalan), nucleoside analogs (cladribine, fludarabine), and monoclonal antibody (rituximab [anti-CD20]).
23
Studies have shown a response rate for Cladribine to range from 44% to 90%.
24,25
In patients with IgM autoantibody-related neuropathies, high dose Rituximab has been shown to improve nerve conduction velocities and decrease anti-MAG antibody titers.
26,27
Fifty four percent of patients who start rituximab have shown increases in IgM titers that may persist for up to four months. However, this does not indicate treatment failure but does necessitate the use of plasmapheresis to reduce hyperviscosity.
28,29 Plasmapheresis has been shown to be effective in the removal of circulating IgM and is indicated patients with hyperviscosity symptoms.
23,30
WM patients with retinal vein occlusions may also experience an improvement in vision after plasmapheresis
16 and it may be effective in resolving neurosensory retinal detachments.
18
Combination therapy of nucleoside analogs (cladribine) and monoclonal antibodies (rituximab) have been shown to increase response rates and is considered a reasonable choice for primary treatment of WM.
31,32
Nucleoside analogs combined with alkylating agents have also been shown to be an effective treatment.
31,32
VI.
CONCLUSION
Hyperviscosity should be considered in patients presenting with bilateral CRVO.
Referral for additional testing including, serum electrophoresis and CBC, should always be indicated in these cases.
REFERENCES
1.
Herrington LJ, Weiss NS. Incidence of Waldenstrom’s macroglobulinemia.
Blood. 1993; 82: 3148-3150.
2.
Groves FD, Travis LB, Devesa SS, Ries LA, Fraumeni JF Jr. Waldenstrom’s macroglobulinemia: incidence patterns in the United States, 1988-1994. Cancer.
1998; 82: 1078-1081.
3.
Dimopoulos MA, Alexanian R. Clinical Review Article: Waldenstrom’s macroglobulinemia. Blood. Vol 83, No 6(March 15), 1994: pp 1452-1459
4.
Benjamin M, Reddy S, Brawley OW. Myeloma and race: a review of the literature. Cancer Metastasis Rev. 2003;22:87-93.
5.
Fonseca R, Hayman S. Waldenstrom macroglobulinemia. Br J Haematol 2007;
138: 700.
6.
Dimopoulos MA, Panayiotidis P, Moulopoulos LA, Sfikakis P, Dalakas M.
Waldenstrom’s macroglobulinemia: clinical features, complications, and management. J Clin Oncol. 2000;18:214-226.
7.
Renier G, Ifrah N, Chevailler A, et al. Four brothers with Waldenstrom’s macroglobulinemia. Cancer 1989; 64: 1554.
8.
McMaster ML, Csako G, Giambarresi TR, et al. Long-term evaluation of three multiple-case Waldenstrom macroglobulinemia families. Clin Cancer Res 2007;
13:5063.
9.
McMaster ML, Goldin LR, Bai Y, et al. Genomewide linkage screen for
Waldenstrom macroglobulinemia susceptibility loci in high-risk families. Am J
Hum Genet 2006; 79: 695.
10.
Treon SP, Hunter ZR, Aggarwal A, et al. Characterization of familial
Waldenstrom’s macroglobulinemia. Ann Oncol 2006; 17:488.
11.
Altieri A, Bermejo JL, Hemminki K. Familial aggregation of lymphoplasmacytic lymphoma with non-Hodgkin lymphoma and other neoplasms. Leukemia 2005;
19: 2342.
12.
Kristinsson SY, Bjorkolm M, Goldin LR, et al. Risk of lymphoproliferative disorders among first-degree relatives of lymphoplasmacytic lymphoma/Waldenstrom macroglobulinemia patients: a population-based study in
Sweden. Blood 2008; 112: 3052.
13.
Garcia-Sanz R, Montoto S, Torrequebrada A, et al. Waldenstrom macroglobulinemia: presenting features and outcome in a series with 217 cases.
Br J Haematol 2001; 115: 575.
14.
Fahey JL, Barth WF, Solomon A: Serum hyperviscosity syndrome. JAMA 192:
120, 1965.
15.
Chanana B, Gupta N, Azad RV. Case report: Bilateral simultaneous central retinal vein occlusion in Waldenstrom’s macroglobulinemia. Optometry 2009; 80: 350-
353.
16.
Alexander P, Flanagan D, Rege K, Foss A and Hingorani M. Bilateral simultaneous central retinal vein occlusion secondary to hyperviscosity in
Waldenstrom’s macroglobulinemia. Eye. 2008; 22: 1089-1092.
17.
Fadilah SAW, Muhaya M, Azlin I. Irreversible Visual Loss and Optic Nerve
Dysfunction Associated with Central Retinal Vein Occlusion in Waldenstrom macroglobulinemia. Med J Malaysia. Vol 62; No 4:October 2007.
18.
Pilon AF, Rhee PS, Messner LV. Bilateral, Persistent Serous Macular
Detachments with Waldenstrom’s macroglobulinemia. Optometry and Vision
Science. Vol 82, No 7; July 2005.
19.
Quhill F, Khan I, Rashid A. Bilateral serous macular detachments in
Waldenstrom’s macroglobulinemia. Postgrad Med J 2009; Vol 85: No 1005.
20.
Kraus MD. Lymphoplasmacytic Lymphoma/Waldenstrom macroglobulinemia.
Am J Clin Pathol 2001; 116:799-801.
21.
Mansoor A, Medeiros LJ, Weber DM, Alexanian R, et al. Cytogenic findings in lymphoplasmacytic lymphoma/Waldenstrom macroglobulinemia. Am J Pathol
2001; 116: 543-549.
22.
Treon SP, Gertz MA, Dimopoulos M, et al. Update on treatment recommendations from Third International Workshop on Waldenstrom’s macroglobulinemia. Blood. 2006; 107: 3442-3446.
23.
Vijay A, Gertz MA. Review in translational hematology: Waldenstrom macroglobulinemia. Blood. June 2007; Vol 109, No 12.
24.
Delannoy A, Van Den Neste E, Michaux JL, Bosly A, Ferrant A. Cladribine for
Waldenstrom’s macroglobulinemia. Br J Haematol. 1999; 104: 933-934.
25.
Fridrik MA, Jager G, Baldinger C, Krieger O, Chott A, Bettelheim P. First-line treatment of Waldenstrom’s disease with cladribine. Arbeitsgemeinschaft
Medikamentose Tumortherapie. Ann Hematol. 1997; 74:7-10.
26.
Gertz MA, Anagnostopoulos A, Anderson K, et al. Treatment recommendations in Waldenstrom;s macroglobulinemia: consensus panel recommendations from the Second International Workshop on Waldenstrom’s Macroglobulinemia. Semin
Oncol. 2003; 30: 121-126.
27.
Renaud S, Fuhr P, Gregor M, et al. High-dose rituximab and anti-MAGassociated polyneuropathy. Neurology. 2006;66:742-744.
28.
Ghobrial IM, Fonseca R, Greipp PR, et al. Initial immunoglobulin M ‘flare’ after rituximab therapy in patients diagnosed with Waldenstrom macroglobulinemia: an
Eastern Cooperative Oncology Group Study. Cancer. 2004; 101: 2593-2598.
29.
Treon Sp, Branagan AR, Hunter Z, Santos D, Tournhilac O, Anderson KC.
Paradoxical increases ins erum IgM and viscosity levels following rituximab in
Waldenstrom’s macroglobulinemia. Ann Oncol, 2004; 15: 1481-1483.
30.
Patel TC, Moore SB, Pineda AA, Witzig TE. Role of Plasmapheresis in
Thrombocytopenic Purpura Associated with Waldenstrom’s macroglobulinemia.
Mayo Clin Proc 1996; 71: 597-600
31.
Tedesh A, Alamos SM, Ricci F, Greco A, Morra E. Fludarabine-based combination therapies for Waldenstrom’s macroglobulinemia. Clin Lymphoma
Myeloma: 2009 Mar; 9(1):67-70.
32.
Dimopoulos MA, Gertz MA, Kastritis E, et al. Update on treatment recommendations from the Fourth International Workshop on Waldenstrom’s macroglobulinemia. J Clin Oncol. 2009 Jan 1; 27(1): 120-6.