ASD_review_Dec02
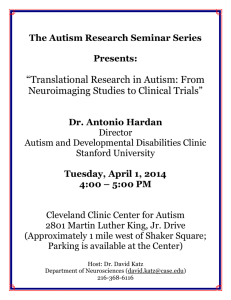
advertisement

Psychiatric Clinics of North America Volume 25 • Number 4 • December 2002 Copyright © 2002 W. B. Saunders Company Review article The autistic spectrum: subgroups, boundaries, and treatment Sophie H.N. Willemsen-Swinkels, PhD * Jan K. Buitelaar, MD, PhD Department of Child and Adolescent Psychiatry University Medical Center PO Box 85500 3508 GA Utrecht, The Netherlands * Corresponding author E-mail address: s.h.n.willemsen@psych.azu.nl PII S0193-953X(02)00020-5 Leo Kanner posited in 1943 [1] the existence of a syndrome called “early infantile autism.” In 1956, Kanner and Eisenberg laid down two criteria for the definition of the disorder: (1) profound lack of affective contact at least up to age 5 and (2) elaborate repetitive routines [2] . At that time there was a general belief that Kanner's classic autism was a unique and discrete condition. The concept of autism was found to be useful in clinical practice in which many practitioners who had lived or worked with autistic children were sure they could instantly identify any other child with the same type of handicap [3] . In the decades that followed, however, it proved to be difficult to reach consensus about the definition and validity of autism. Specifying and operationalizing the essential characteristics necessary for a diagnosis took a much longer time than originally anticipated. We have come to realize that the boundaries of autism are not that clear. Many behaviors commonly observed in autism (eg, stereotypies) also can be seen in non-autistic individuals. Second, there is a complex influence of developmental level or intelligence on symptom expression. Finally, there is a considerable amount of clinical and etiologic heterogeneity in people with autism. Over the past decades this has led to an inconsistent use of various diagnostic labels, which is illustrated by the results of prevalence studies. Early studies reported prevalence rates of 2 to 5 in 10,000 for autism. Recently, prevalence rates up to 60 in 10,000 were reported [4] [5] . These differences in prevalence rates are believed to be caused mainly by improved detection and recognition through systematic population approaches in later prevalence studies together with a broadening of the diagnostic concept rather than to a secular increase in the incidence of the disorder [6] . Successive editions of the World Health Organization's “International Classification of Diseases” (ICD) and the American Psychiatric Association's “Diagnostic and Statistical Manual of the Mental Disorders” (DSM) have reflected changing ideas of autism and related disorders. Almost 50 years after Kanner's first description, the latest versions of ICD [7] and DSM-IV [8] provided virtually identical definitions of autism and autistic-like disorders [9] . In both systems the overall construct of autistic and autistic-like behavior problems has been given the name pervasive developmental disorders (PDD). The term “pervasive” was meant to emphasize that in autism development was disturbed over a range of different domains, in contrast to the relatively more delineated difficulties of the specific developmental disorders and the centrality of cognitive problems in mental retardation. The term “developmental” implies that individuals with these conditions suffer from disturbances in the normative unfolding of multiple developmental competencies, including social relations and communication [10] . These disorders have their onset in the first years of life, and developmental correlates have important implications throughout the life span. The latest versions of the systems—ICD-10 and DSM-IV—largely agree on the disorders that fall under this construct of PDD. To be diagnosed as autistic disorder in the DSMIV, a child must meet a minimum of six criteria among the following three areas of impairment: qualitative impairments in social interaction, qualitative impairments in verbal and nonverbal communication, and restricted repetitive and stereotyped patterns of behavior, interest, and activities. An additional requirement is that delays or abnormal functioning in at least one of the areas of social interaction, language, and symbolic or imaginative play have been noted before the age of 3 years. The category PDD-Not Otherwise Specified (including atypical autism) (PDD-NOS) is used for conditions that are characterized by pervasive impairments in reciprocal social interaction, verbal and nonverbal communication, or rigid and stereotyped behavior patterns but fail to meet the full set of criteria for autistic disorder. A classification of PDD-NOS may be given in the following instances: (1) the case fails to have an onset before age 3 years; (2) the case presents with atypical symptoms that do not fit with the 12 criteria of autistic disorder of DSM-IV; (3) the case is a subthreshold variant of autistic disorder and has less than the cut-off point of six symptoms listed under autism; or (4) the case fails to meet the pattern of criteria of autism (eg, less than two social symptoms or no symptoms in either the communication or activity/interest domain). A category similar to PDD-NOS is included in ICD-10 under the label of atypical autism. As a result of being a residual category, positive or explicit diagnostic criteria were not provided [11] . One of the intriguing aspects of autism is the marked clinical heterogeneity. Lack of responsiveness to people can express itself as a total avoidance of social interactions. Lack of responsiveness also can be found, however, in patients who do show an interest in other people and friendships. In these patients, lack of responsiveness is expressed as a deficit in the understanding of conventions of social interaction. Communicative impairments can range from total lack of expressive language to reasonably fluent speech with abnormalities in pitch, intonation, rate, rhythm, or stress. Finally, the criterion of bizarre responses to the environment includes behaviors as diverse as self-mutilation, obsessive insistence on sameness, and preservative, stereotyped preoccupations. The course of autism also varies. Some children seem to develop normally for several months to several years and then show deterioration, whereas other children show an abnormal course of development from birth onward. Some children with autism can have a stable course with only minimal fluctuations in symptoms, whereas other children show either a deterioration or improvement with age. There are also major individual differences in responsivity to behavioral interventions. Another source of clinical heterogeneity is the wide variation in level of intellectual functioning among individuals with autism. Recent reports indicate a rate of mental retardation between 26% and 55%, which is lower than the approximate 75% rate of studies of older date [4] . Individuals with autism may have a range of other behavioral symptoms, including hyperactivity, short attention span, impulsivity, aggressiveness, and temper tantrums. There also may be abnormalities in eating, sleeping, or mood. Heterogeneity in nonspecific neurologic symptoms or signs also may be noted. 10% to 15% of cases of autism are observed in association with various neurologic or other medical conditions. Approximately 25% of the subjects with autism develop seizures. Despite this marked heterogeneity, the DSM-IV field trial has established that autism is one of the most robust diagnoses in the system [9] . In this trial, information was obtained from 21 sites on 977 children, adolescents, and adults with severe developmental disturbances. A standard coding system, which included basic demographic information, the rater's clinical diagnosis, and explicit ratings of diagnostic criteria derived from the various “official” diagnostic systems, was used by each of the 125 raters. For inexperienced raters, a revised ICD-10 definition was found to have excellent sensitivity (0.82) and specificity (0.87). The DSM-IV criteria were modeled on these revised ICD10 criteria. Although the definition of autistic disorder in the latest versions of the classification systems is one of the most reliable and valid diagnoses in psychiatric research, the diagnosis of PDD-NOS is still problematic. The validity of autistic-like conditions such as Asperger's disorder requires more clarification [12] . A diagnostic category must meet two criteria to fulfill taxonomic validity [13] : (1) internal validity (ie, it should be possible to measure or operationalize the category) and (2) external validity (ie, it should differ from related disorders on attributes other than the behavioral descriptors by which the disorder was originally defined). Examples of possible attributes are associated nondiagnostic behaviors;, possible markers of etiology, such as pregnancy and birth complications, family history, associated neurologic diseases, and epidemiologic correlates, such as sex ratio and socioeconomic status; clinical course or outcome; and response to treatment [13] . The following section discusses the many issues that relate to the internal and external validity of the classification of the various PDDs. Autistic disorder and pervasive developmental disorder Autistic core group together with other pervasive developmental disorder remainder groups The formal diagnostic systems of ICD and DSM are organized around dichotomous categories (ie, an individual either has or does not have a disorder). These diagnostic systems are intended to divide populations into categories that share a common symptom presentation and maybe common etiology and course that is distinct from those of other categories. Within the domain of PDD there is a wide range of severity of symptoms. To incorporate some indication of severity of symptoms, the ICD-10 and DSM-IV make a distinction between individuals with many severe behavior problems and individuals with fewer or less severe behavior problems. The result is a classification system that assumes the existence of a core syndrome—autistic disorder—and other PDD remainder groups. In essence, this distinction is based on the number or severity of autistic symptoms. This leaves the question of where the boundary should be drawn. Justification for a particular set or number of criteria can be based on the historical precedent for criteria such as Kanner's original description [14] , pragmatics (eg, selection of the system with the greatest coverage) [15] , or the best fit with current clinical practice on the basis of consensus by clinical experts [16] . An example of an attribute that has a clear danger of circularity is age of onset. The term “age of recognition” is probably more appropriate than “age of onset” because parents may not detect the early signs of abnormal development. An earlier age of recognition (onset) is found to coincide with more profound disruption of normal developmental processes [17] . Age of recognition (onset) may be an indicator of severity and pervasiveness, but on its own it cannot be considered a specific characteristic that discriminates between discrete disorders. In DSM-III, types of PDD were distinguished in terms of age of onset. Dahl et al [17] addressed the question of whether children who suffer from autism and children who suffer from what was called childhood-onset PDD in DSM-III form homogeneous and discrete diagnostic categories. They concluded that age of onset did not emerge as a differentiating characteristic for either PDD group. Based on a study of 274 case records, Rescorla et al [18] also concluded that the DSM-III concept of distinguishing types of PDD in terms of age of onset lacks firm empirical validity. Levels of cognitive or language development are other discriminators that easily suffer from a circularity when severity of autistic symptoms was the differentiating descriptor from the beginning. The validation of the distinction between a core group and other remainder groups preferably must come from features such as prognosis and course, etiology, and response to treatment. Regarding prognosis, follow-up studies [19] often have been limited to cases with autistic disorder. Results suggest that outcome at adult age is unrelated to the presence of individual symptoms (other than lack of speech) but seems to be related to the total number of autistic symptoms. The crucial question that remains to be addressed, however, is which number of autistic symptoms is associated with an increased risk to poor long-term outcome. Knowledge regarding the origin of autism so far does not support such a distinction. Autistic disorder and PDD-NOS may be associated with other medical conditions, although there is some suggestion that this holds more for cases with atypical phenomenology (PDD-NOS) than for typical cases. A uniquely and pathognomonic neural deficit has not (yet) been found for either autistic sisorder or PDD-NOS. There is a widespread agreement that the PDDs are caused largely by genetic factors. The genes for autistic disorder also confer susceptibility to the lesser variant, as is indicated by the fact that the lesser variant occurs more commonly than expected in relatives of autistic probands. This finding suggests that autistic disorder and the lesser variant PDD share common genetic mechanisms [20] . There are several suggestions for cognitive functional deficits that might be responsible for several or all of the autistic features, such as deficits in theory of mind, central coherence, or executive functioning. There is no suggestion that any one of them can be considered specific for autistic disorder, however. On the contrary, most of these deficits have been found not only in children with PDD-NOS but also to some degree in children with other non-autistic conditions, such as mental retardation or attention deficit hyperactivity disorder. In clinical practice, the distinction between core autism and remainder PDD groups has no real meaning with respect to treatment. The level of language development and the overall level of cognitive functioning are of much greater importance for the choice of treatment. In summary, many discriminators between autistic disorder and PDD-NOS suffer from a danger of circularity and cannot be considered conclusive with respect to the external validity of the distinction between core autism and PDD-NOS. Currently no clear nonbehavioral marker discriminates people with core autism from other people. The current state of knowledge is that the remainder PDD group overall expresses a pattern of autistic characteristics that is nearly identical to the pattern found for “core autism” [16] , with the only difference being the severity of symptoms. Several autistic groups One approach to limit the heterogeneity of the PDDs is to look for more homogeneous behavioral subgroups. The identification of behaviorally similar subtypes of children with autism may lead to clarifications regarding the cause because behaviorally similar children may share specific pathologic etiologic conditions. Second, membership in specific, behaviorally defined subcategories of PDD might have prognostic significance. Third, subtypes of children with autism might respond differently to various treatments. For example, autistic children with certain behavioral characteristics might respond more favorably to particular pharmacologic or behavioral interventions [21] . For these reasons, various investigators have attempted to subcategorize children based on, for example, putative etiology, behavior or symptom clusters, cognitive profile, and differential outcome. By putative etiology In some cases, PDDs are associated with, and presumably caused by, some medical condition, of which infantile spasms, congenital rubella, tuberous sclerosis, cerebral lipidosis, and the fragile X chromosome anomaly are among the most common. Efforts to limit heterogeneity have included the creation of subgroups by presence of organic features. Some controversy exists with respect to the frequency with which the basis of autism is accounted for by a known diagnosable medical condition. Scandinavian (and some other) studies reported high rates of associated medical conditions; for example, Gillberg [22] mentioned a rate of 37%. Other investigators found approximately 8% to 10% of the PDD cases to be associated with medical conditions [23] [24] . Part of the explanation lies in the IQ distribution of the different samples [25] . Known medical conditions are much more common when autism is accompanied by severe or profound mental retardation. Comparisons of the clinical pictures in PDDs that occur with and without associated biologic syndromes are scarce and have not, as yet, reliably identified any specific differences, apart from the fact that individuals with an associated biologic syndrome tend more often to be severely or profoundly mentally retarded [25] . An exception is the association of fragile X syndrome with gaze avoidance [26] . By social functioning A subgroup classification system proposed by Wing and Gould [27] emphasized differences in the social behavior of children with autism. Three subgroups were distinguished: (1) “Aloof” children are characterized by a failure to approach others and a tendency to ignore or withdraw from others when approached. (2) “Passive” children, on the other hand, are responsive when approached and remain socially engaged (albeit in a limited manner) as long as the other person maintains the interaction. (3) “Active-butodd” children actively seek interaction with others but do so in an odd, awkward, and overly persistent manner. Initially, the social subtyping scheme forwarded by Wing and Gould was well received and described as heuristically and clinically useful. The findings of Volkmar et al [28] with regard to the validity of the social subtypes were somewhat disappointing, however, because subtype assignment was not strongly related to independent measures of either social interaction or development. A second problem was the interobserver reliability for assignment to the passive group. Several studies reported difficulties with the assignment to the passive group and failed to validate the division in three groups [28] [29] . Finally, a strong relationship was found between Wing and Gould subtype assignment and level of intellectual functioning [28] [29] . Volkmar et al [28] found that IQ was actually a slightly better predictor of Wing subgroup assignment (based on clinician's ratings) than the summary score of items drawn from the description of the Wing and Gould subtypes. By level of functioning The apparent relationship between IQ and prognosis suggests that autistic subjects might be subclassified according to level of intellectual functioning. Level of intellectual functioning has been found to correlate significantly with severity of symptoms in all three domains of autistic impairment. A subclassification according to level of intellectual functioning is, however, fundamentally different from a division between autism and PDD-NOS, because the subcategory of PDD-NOS includes high-functioning and low-functioning atypical groups of children. Table 1 presents results from studies that have addressed this issue by using cluster analytic techniques to determine whether natural homogeneous subtypes emerge from the data. A major constraint of cluster analytic techniques is that the clustering algorithm can operate only on variables that the researcher has entered into the analysis. Selection of variables to be clustered reflects the researcher's best guess as to the most important dimensions that differentiate subgroups within the sample [30] , and clustering techniques identify groups in any dataset. Further study is needed to investigate whether these groups represent internally or externally valid PDD subtypes with distinctive and unique patterns of symptomatology for which criteria could be specified [31] . Table 1. Studies since 1990 that have used cluster analysis to find subgroups in children with PDD Subjects Naam n Diagnosis Age in Description of clusters years Eaves et al 1994 [97] 166 AD, PDD-NOS, or 3–12 autistic spectrum disorder 1: typical autistic group 2: low-functioning group 3: high-functioning group Table 1. Studies since 1990 that have used cluster analysis to find subgroups in children with PDD (Asperger/schizoid) 4: hard-to-diagnose group with mildmoderate retardation and a family history of learning difficulties Sevin et al 1995 [21] 34 Austism (27) and PDD-NOS (7) (DSM-III-R) 2–22 1: high functioning/atypical PDD 2: mild autism 3: moderate autism 4: low functioning/severe autism Waterhouse et al 1996 [14] 194 Some form of PDD 3–7 A: other-PDD/active but odd/higher cognitive and adaptive functioning/relatively fewer autistic behaviors B: autistic/aloof/lower cognitive and adaptive functioning/relatively more autistic behaviors Prior et al 1998 [32] 135 High functioning with autistic behaviors (DSMIII-R) 3–21 A: autistic-like B: Asperger-like C: mild PDD or PDD-NOS–like Authors suggested: clusters based on severity of symptoms and level of cognitive functioning rather than distinctive symptom patterns Stevens et al 2000 [34] 138 Autistic disorder 7 or 9 – High-functioning subgroup (DSM-III-R) – Low-functioning subgroup Differentiated at school age by behavioral measures of social abnormality, language ability, and cognitive level In most studies summarized in Table 1 , differences found are related to severity of impairment—especially level of cognitive and adaptive functioning—rather than to distinctive diagnostic patterns of behavior [32] . Even studies that explored developmental level along with other variables support the role of intellectual functioning as one of the strongest indicators of subtype [33] . In a longitudinal study with autistic children, the lower functioning preschool subgroup children overwhelmingly remained in the lower functioning school-age group, whereas the higher functioning preschool group split into a poor outcome and a less good outcome group [34] . Several recent pharmacologic studies have indicated a differential response to pharmacologic therapy as a function of IQ [35] [36] [37] [38] , which suggests the presence of biochemical differences in low- versus high-functioning autistic children. In a review of the genetic epidemiology of autism and other PDDs, it was suggested that higher and lower functioning PDDs do arise from nonidentical genetic mechanisms [20] . This was based on two findings. First, IQ and measures of adaptive functioning seem to run true within families. Higher functioning autistic people tend to have higher functioning affected siblings, and lower functioning autistic people have similarly affected siblings [39] . Second, for relatives of autistic people the risk of having the lesser variant of autism varies by level of functioning of the person with autism [20] [40] . Table 2 summarizes reports on the differences between high- and low-functioning people with autism. In conclusion, a subclassification by developmental level may offer clinical utility. Two aspects must be kept in mind, however. First, apart from the differences between high- and low-functioning people with autism, the two groups also show a significant behavioral overlap. Second, in the current state of knowledge, the choice for a particular IQ cut-off score that sets the boundary between high and low functioning is arbitrary. Table 2. Differences between low-functioning and high-functioning people with PDD Low functioning relative to high functioning Reported by Developmentally lower and more severe manifestations of the symptoms, greater adaptive behavior impairment [98] [99] Poorer outcome, more behavioral and cognitive decline over time [34] [100] [101] Higher association with known medical conditions, more neurologic signs, higher proportion of organic pathology, structural brain abnormalities, epilepsy [13] [14] [25] [103] Higher proportion of female subjects [105] Siblings have greater risk of the lesser variant of PDD [20] [40] Lower prevalence of family psychiatric history [103] [102] [104] An autistic continuum without a bounded core or discrete clinical groups Clinical intuition and studies [27] [41] suggest that autistic-like symptoms better fit to a multivariately distributed dimensional trait than to categorical entities. Many researchers have argued for an autistic continuum without sharp boundaries between an autistic core group and other PDD remainder groups rather than for a sharp cut-off between these groups [3] [31] [42] [43] . In this continuum, multiple and interacting biologic and environmental influences are believed to determine the severity of impairment [44] . The results of an epidemiologic study of children with special educational needs in one area in London suggested that the autistic continuum is characterized by a set of three features with a strong tendency to cluster together [27] : impairments of reciprocal social interaction, verbal and nonverbal communication, and imagination (identified as being closely related to the narrow, rigid, repetitive pattern of behavior). This cluster has been referred to as the triad of impairments. Within this concept of an autistic continuum it is uncertain as to where the cut-off from normality actually falls. There is evidence from family studies of an elevated risk for social, communication, and repetitive impairments among the relatives of probands with autism. The social difficulties are qualitatively similar to, although milder, than those who typify autism and are sometimes apparent in childhood [45] . Should the boundaries of the autistic continuum be extended to include these relatives? This question poses a risk of the diagnosis of autism being extended to include anyone whose odd and troublesome personality does not readily fit some other category. Such overinclusion is likely to devalue the diagnosis to a meaningless label [43] . The current versions of the two leading classification systems give no suggestions for the cut-off of PDDs from normality. Within these classification systems, cases at the less severe end of the continuum (mild phenotype expression) are likely to be classified as PDD-NOS, the residual category; however, PDD-NOS is defined by what it is not (ie, autistic-like but not autistic) rather than by explicit criteria. No threshold is given in the differentiation between PDD-NOS and non-PDD conditions. In two independent datasets, a scoring rule for the differentiation between PDD-NOS and non-PDD conditions has been derived and tested [46] [47] . The best separation between PDD-NOS and non-PDD conditions could be obtained with a cut-off point of at least four or five items of the full set of DSM-IV criteria for autistic disorder, and with one of the social interaction criteria set as mandatory. This diagnostic rule was found to be the best estimate for the diagnostic rules that underlie the attribution of a clinical diagnosis of PDD-NOS in current clinical practice. An autistic spectrum Many researchers have argued for the existence of an autistic spectrum rather than for an autistic continuum. The term “continuum” suggests a simple straight line from severe to mild (Fig. 1 ). With respect to the autistic disorders, the situation is believed to be much more complex. The manifestations of the social and other problems vary widely in type and severity, and all kinds of combinations of impairments are seen in clinical practice. Some of these combinations have been named as syndromes. These syndromes are discussed in the next section. Many other combinations of impairments have not (yet) been assigned a separate identity. The term “spectrum” is used to indicate the fact that although there is a common denominator, different types of children with a PDD present with their own pattern of symptoms. These types of children differ by nature and not merely by degree. This is reminiscent, metaphorically speaking, of the spectrum of distinct colors after refraction of light by a prism [48] . Fig. 1. (A) Autistic core with other PDD remainder groups. (B) Several autistic groups. (C) An autistic continuum without a bounded core or discrete clinical groups. (D) An autistic spectrum. Measurement issues To advance our knowledge about the nosology of the autistic spectrum disorders and facilitate further work on defining valid subgroups, several measurement issues should be resolved. The first and most important issue is the establishment of biologic or psychological markers of autism. The second issue involves introducing developmentally sensitive criteria for autism and related disorders that enable researchers to arrive at developmental age-corrected severity scores of the social, communicative, and rigidity and other symptom domains. Third, attempts should be made to calibrate severity of symptoms against levels of language ability and nonverbal skills. Fourth, the further operationalization and specification of the as-yet abstract and complex diagnostic criteria of autistic spectrum disorders, as listed in DSM-IV and ICD-10, will improve possibilities to obtain reliable ratings about autistic symptoms in various contexts and according to different informants, such as parents and teachers. Fifth, the development of diagnostic instruments that quantify the symptom domains of social interaction, communication, and rigidity and other symptoms is necessary. Commonly used standard diagnostic instruments, such as the Autism Diagnostic Interview-Revised and the Autism Diagnostic Observation Schedule, have been developed particularly to measure the extreme manifestations of autistic symptoms and are less sensitive to the range of more subtle manifestations that lie between normality and extreme pathology. Consequently, the distances between values of these scales are uneven. Resolution of these measurement issues gives new impetus to multivariate model fitting of subgroups of autistic spectrum disorders. Other pervasive developmental disorders Several researchers and clinicians have searched for disorders that may be delineated within the broad and heterogeneous class of PDDs. The ICD-10 and DSM-IV provide tentative diagnostic descriptions of some other disorders in the PDD class in addition to autistic disorder as the most nuclear type of PDD and PDD-NOS as the residual category. These disorders include Asperger's disorder, Rett's disorder, childhood disintegrative disorder, and overactivity disorder associated with mental retardation and stereotyped movements (the latest one only in the ICD-10). Asperger's disorder One year after Kanner's first description of autism, the Austrian physician Asperger described several cases whose clinical features largely resembled Kanner's. Asperger's description differed from Kanner's, however, in that speech was less commonly delayed, motor deficits were more common, the onset appeared somewhat later, and all the initial cases occurred in boys [49] . Currently, Asperger's disorder is included in the DSM-IV and the ICD-10. In DSM-IV, the criteria for Asperger's disorder on the domains “qualitative impairment in social interaction” and “restricted, repetitive and stereotyped patterns of behavior, interests, and activities” are identical to those for autistic disorder. Asperger's disorder contrasts to autistic disorder in that there are no clinically significant delays in the early development of language around age 1 to 2 years. There are also no clinically significant delays in cognitive development or the development of age-appropriate selfhelp skills, adaptive behavior (other than social interaction), and curiosity about the environment in childhood. Clumsiness also has been proposed as a diagnostic feature of Asperger's disorder. Of 23 children with Asperger's disorder subjected to a clinical study, 83% were found to have motor coordination problems [50] . The clinical description of Asperger's disorder in the ICD-10 mentions a marked clumsiness as a common feature. Subsequent studies have shown that clumsiness is not specific to Asperger's disorder, however, but is a feature that is common in all PDDs and that patients with autism may even be more clumsy than individuals with Asperger's disorder [51] . Data on the prevalence of Asperger's disorder are inconclusive. Two surveys conducted in Sweden [52] [53] reported high prevalence estimates (28.5 and 48.4 per 10,000, respectively). These studies reported wide confidence intervals, however, which indicates an extreme lack of precision of these estimates because of small studies [5] . On the other hand, six epidemiologic surveys that have simultaneously assessed the presence of autistic disorder and Asperger's disorder all reported a rate of Asperger's disorder consistently lower than that of autistic disorder. A pooled analysis of these six studies suggests a prevalence of 2 per 10,000 for Asperger's disorder [5] . The validity of Asperger's disorder as distinct from other PDDs remains controversial, as is explicitly noted in the ICD-10 [7] . The key question is whether Asperger's disorder is qualitatively different from autism unaccompanied by mental retardation. The alternative interpretation would be that Asperger's disorder is just a variant expression of “high functioning autism” (HFA) [12] . Several studies have attempted to identify discriminating criteria between Asperger's disorder and high functioning autism, with mixed results [9] [54] [55] [56] . The differences between the results of the studies can be explained by the differences in nosologic approach. The use of a less systematic and stringent diagnostic assignment (eg, broader definitions of Asperger's disorder) may explain the failure of finding significant differences between Asperger's disorder and HFA groups in some studies [56] . On the other hand, these studies suffer from the danger of circularity because findings of differences often reflect the criteria adopted in the assignment of the diagnosis Asperger's disorder and HFA in the first place. The DSM-IV autism/PDD field trial compared individuals with Asperger's disorder with individuals with HFA (full scale IQ > 85). Individuals with Asperger's disorder were found to be less likely to have exhibited delays in the development of spoken language or currently exhibit language/communication deviance; motor delays and “clumsiness” were more variable; isolated special skills (often related to abnormal preoccupations) were more frequent; and social, communicative, and “resistance to change” symptoms were less frequent. Individuals with Asperger's disorder were more likely to exhibit verbal IQ scores greater than performance IQ scores, whereas the opposite trend was obtained for individuals with HFA [9] . A subsequent study compared groups of Asperger's disorder and HFA individuals whose diagnostic assignment was made after stringent criteria [56] . A comparison of neuropsychological profiles revealed that 11 areas discriminated between the two conditions. The neuropsychological differences between Asperger's disorder and HFA were captured in the discrepancy between verbal IQ and performance IQ, with verbal IQ being universally higher than performance IQ for individuals with Asperger's disorder, whereas no verbal IQ-performance IQ discrepancy was found for individuals with HFA. The Asperger's disorder and HFA groups did not differ in terms of full scale IQ. In a comparative study of the cognitive profiles of 120 children with Asperger's disorder, autistic disorder, and attention disorders, the intergroup discrimination overall was found to be far from perfect [57] . The overall rate of correct diagnostic classification using stepwise logistic regression analysis was found to be only 63%. The results indicated that Asperger's disorder and autism share certain cognitive deficits on the Wechsler Intelligence Scale for Children-Revised. Differences between Asperger's disorder and autistic disorder were found on IQ level and verbal ability, with Asperger's disorder characterized by a significantly better verbal ability. Klin et al [56] argued that Asperger's disorder and HFA still could share the same origin or other pathogenetic processes while having phenotypic differences solely accounted for by neuropsychological differences. In this sense, Asperger's disorder and HFA could be seen as the same diagnostic entity expressed differently because of different neuropsychological endowment, which is similar, to some extent, to the phenomenologic differences between lower functioning and higher functioning autism. Whether Asperger's disorder and HFA are truly different diagnostic entities will be clarified only with additional knowledge on the developmental, behavioral genetics, and neuroanatomic aspects of the two conditions. Concerning developmental trajectories, children with Asperger's disorder had less severe early behavioral abnormalities than children with HFA. At follow-up in adolescence, however, the Asperger's disorder and the HFA groups had similar behavioral manifestations [58] . Few data are available on the cause of Asperger's syndrome as distinct from autism. One study compared 23 children with Asperger's disorder to 23 age- and IQ-matched children with infantile autism (DSM-III). Children with autism were found to have more prenatal, perinatal, and neonatal problems [50] . Overall, the differences reported between Asperger's syndrome and autism on etiologic parameters are relatively small and of uncertain clinical significance. There is a high incidence of Asperger's syndrome in family members of high-functioning autistic subjects [59] . Currently, it seems best to conclude that the two syndromes are variable expressions of the same underlying disorder and share a common etiology [60] . Childhood disintegrative disorder The general guidelines to the diagnosis of childhood disintegrative disorder (CDD) are (1) onset of the condition after a fairly prolonged period of normal development and (2) marked deterioration in multiple developmental areas accompanied by development of various “autistic-like” features. Once the disorder is established, children with CDD clearly resemble autistic children of the same intellectual level in terms of their behavior, limited communication skills, pattern of long-term outcome, and the need for various special services. CDD is included in the DSM-IV as part of the PDDs. The DSM-IV criteria describe the period of normal development to have been at least 2 years but less than 10 years. Volkmar and Rutter [61] mentioned a child who appeared to develop normally for 18 months and then had a marked regression. Although good epidemiologic data are lacking, it is undoubtedly true that CDD is a relatively uncommon condition, much less frequent than autism [62] . Some controversy still exists as to whether CDD should be regarded as a diagnostic category separate from other variants of autistic disorder. The main question is whether autism that seems to have been preceded by a period of definitely normal development differs in any fundamental way from autism in which development has been abnormal from the outset. Another problem is the fact that for the differentiation between autistic disorder and CDD, clinicians must rely on information from the parents about the child's behavior in the first years of life. An argument in favor of a distinction is the finding that CDD seems to have an even worse prognosis than autism in multiple respects. Volkmar et al [63] compared 10 children with CDD to 165 individuals with autism. The children with CDD were found to be significantly more likely to be mute and significantly more likely to be in residential placement than children with autism. As a group, the 10 children with CDD had a significantly lower mean IQ than the children with autism. Similar results were found with the data of the DSM-IV Autism Field Trial [61] . In this study, 26 children with CDD were compared with a group of children with autism. The children with CDD were found to be more likely to be mute, have IQ scores of less than 40, and more often be in a residential placement than children with autism. The median age of onset in the CDD group was 36 months; the latest age at onset was 70 months. Mouridsen et al [64] further contributed to the validation of CDD with their finding that CDD and autistic disorder could be distinguished with reference to epilepsy. Thirteen children who had normal or near-normal development for several years followed by a loss of skills and speech were compared to 39 matched cases with autism. Significantly more children with disintegrative disorders had developed seizures (77% versus 33%). Although this finding suggests that CDD is caused by a significant neuropathologic process, extensive evaluations usually fail to reveal identifiable medical conditions. Rett's disorder Just like CDD, Rett's disorder also starts with an initial period of normal development, including normal perinatal head circumference. In contrast with CDD, the period of normal development is usually short (ie, typically a matter of months) [65] . Then there is a deceleration of head growth followed by a loss of hand skills and the appearance of stereotypic hand-wringing movements. Social skills and expressive and receptive language development also deteriorate at 2 to 3 years of age. Ataxia and apraxia become prominent, and gait becomes broad-based and jerky, with stiff legs and side-to-side swaying. Breathing dysfunctions may be severe [66] . Once established, the disorder contains autistic features, such as impairments in social interaction, impairments in communication, and stereotyped behaviors. Rett's disorder has enough distinguishing features to warrant a distinct diagnostic entity, however. For instance, the course of the disorder is different, with Rett's disorder progressing to various forms of neurologic impairment that are not seen in autism. Overall, the prognosis of Rett's disorder is much worse than that of autism, with marked motor impairment and the development of scoliosis [65] . The prevalence of Rett's disorder was studied in a part of southwestern Sweden. In a population of 315,469 children aged 6 to 17 years, 10 cases were detected, all of whom were girls. The corresponding prevalence was 0.65 per 10,000 girls [67] . Recently it has been shown that familial cases are an X-linked dominant disorder and the disease locus maps to Xq28. A candidate gene called methyl-CpG-binding protein 2 (MeCP2) was identified from the Xq28 region and was shown to contain mutations in approximately 77% of Rett's disorder patients [68] . Multiple complex developmental disorder/multidimensionally impaired Several cluster analytic studies on children with severe developmental problems have identified a group of children characterized by social problems, bizarre and disorganized thinking, recurrent anxieties, inappropriate affect, and mood lability [17] [69] [70] . The childhood-onset PDD category included in DSM-III was defined by, among others, unexplained panic attacks, rage reactions, and lack of appropriate affective responses. This led to an alternative operationalization of a severe developmental disorder under the label of multiple complex developmental disorder (MCDD) [71] [72] [73] . In the MCDD concept, emphasis is put on the presence of an impaired regulation of affective state, primitive anxieties and thought disorders, and impairments in social interaction and social sensitivity. As a first-cut test of the clinical usefulness of MCDD, children with MCDD were compared to children with dysthymia and conduct disordered children. A retrospective chart review indicated that children with MCDD had earlier symptom onset, earlier age of first hospitalization, higher psychopathology scores on the Child Behavior Checklist, poorer peer relationships, and greater psychopathology than comparison groups of children [73] . Another chart review study [48] compared 105 children with MCDD with 32 children with autism, 56 children with disruptive disorder, and 51 children with emotional disorder. Multivariate analyses were performed on characteristics extracted from the charts. The outcome of a cluster analysis indicated that MCDD subjects were similar to each other in their symptom profile, whereas they seemed to be dissimilar to children with autistic disorder, disruptive disorder, or emotional disorder. MCDD children proved to be less disturbed in social interaction, communication, and stereotyped and rigid behavior than children with autism. In contrast, MCDD children were found to be more impaired than children with autism in thought disorders, primitive anxieties, and aggression. Children with MCDD and autistic behavior were significantly different on factors that reflected developmental and environmental background variables. Compared to non-PDD children, children with MCDD were marked by more severe abnormalities in all symptoms areas, including social interaction and communication and rigid behavior patterns. These data did suggest that MCDD is not so much a subthreshold variant or an atypical expression of autism as a representation of a PDD subcategory in its own right. The suggestion has been raised that MCDD represents an early manifestation of major affective disorder or schizophrenia [66] . In a study of early-onset schizophrenia, approximately 30% of the cases screened for childhood-onset schizophrenia had complex developmental disorders and brief psychotic symptoms. The impression of a consistent clinical picture led to the proposal of a subgroup of children with atypical psychosis, which was provisionally labeled “multidimensionally impaired.” The characteristics were described as (1) poor ability to distinguish fantasy from reality, as evidenced by ideas of reference and brief perceptual disturbances during stressful periods or while falling asleep, (2) nearly daily periods of emotional lability disproportionate to the precipitants, (3) impaired interpersonal skills despite desire to initiate social interaction with peers, (4) cognitive deficits indicated by multiple deficits in information processing, and (5) absence of formal thought disorder. Similarities between subjects who were multidimensionally impaired and subjects with early-onset schizophrenia were found in the pattern of premorbid developmental difficulties, a discrepancy between word-reading ability and IQ and the increased rate of schizophrenic-spectrum disorders in first-degree relatives. On the other hand, subjects who were multidimensionally impaired were found to differ from subjects with earlyonset schizophrenia in that they had earlier cognitive and behavioral difficulties, earlier age of onset of psychotic symptoms, and a less deviant pattern of autonomic activity. Schizoaffective disorder was found to develop in 3 (27%) of 11 multidimensionally impaired patients [74] . In these multidimensionally impaired patients, transient features of PDD were reported. The relation of this construct of multidimensionally impaired to the somewhat similar construct of MCDD is still unclear. Overall, the nosologic status of the MCDD concept is unclear [75] . There are arguments for and against including MCDD in the PDD category. A contra argument, for example, is that the social relatedness of subjects with MCDD is variable, frequently ambivalent, and different from the typical pattern found in autism. One also may object to including MCDD in the category of personality disorders because no clear continuity between MCDD and any of the personality disorders in adults has been demonstrated. Further research, particularly including follow-up studies, is necessary to resolve these issues. Overactive disorder associated with mental retardation and stereotyped movements The ICD-10 describes a disorder whose diagnosis depends on the combination of developmentally inappropriate severe overactivity, motor stereotypies, and severe mental retardation. The ICD-10 acknowledges that this is an ill-defined disorder of uncertain nosologic validity [7] . Pathogenesis and treatment Pathogenesis Progress in understanding the cause, let alone developing new approaches to treatment, has been painfully slow [71] . Research on the pathogenesis of PDD has focused almost exclusively on autism. Substantial evidence from twin and family-genetic studies exists that autism has strong genetic components [76] [77] . The recurrence risk for autism after the birth of an autistic child is 60 to 150 times the population base rate. Epidemiologically based same-gender twin studies have reported higher concordance rates for autism among identical twins than among nonidentical twins. The mode of genetic transmission is unclear. The marked fall-off in rate of autism that occurs from identical to nonidentical twins or siblings suggests that a small number of interacting genes rather than one single gene is involved, with estimates of genes involved ranging from 2 to 20. The genetic loading seems to be conferred to a broad phenotype that includes lesser variants of autism with subtle social, communicative, and language problems. Several full genome searches for susceptibility loci in autism using affected sibling pairs have been performed, as have a dozen candidate genes studies. Although several areas of the genome (ie, on chromosome 7q, 1, 2, 6, 13 and 16) have been identified as regions of interest, currently no specific variation in a specific gene has been firmly established as a susceptibility gene for autism [77] . Postmortem studies on small case series report cellular abnormalities in the limbic system and cerebellum. An in vivo MRI study on 59 autistic subjects also reported anatomic abnormalities within the limbic system [78] . Another finding with respect to brain morphology is that between 10% and 20% of individuals with autism have macrocephalia, which is in accordance with MRI findings of an increased total brain tissue volume and enlargement most prominent in the occipital and parietal lobes [79] [80] [81] . An interesting study on 60 autistic boys aged 2 to 16 years concluded that abnormal regulation of brain growth in autism results in early overgrowth with hyperplasia of cerebral gray matter and cerebral and cerebellar white matter at approximately age 2 to 4 years followed by abnormally slowed growth and reduced cerebral gray and white matter at an older age [82] . The area dentata, part of the hippocampus, was significantly smaller in autism compared to normal children, particularly at approximately age 2 to 5 years [83] . Another robust and well-replicated neurobiologic abnormality in autism is an elevation of whole blood serotonin, which is found in more than 30% of patients [84] [85] . These and other studies together present overwhelming evidence that abnormalities of brain structure and function underlie the autistic syndrome. The following points are also clear, however: reported abnormalities are heterogenous and based on studies of small samples, most reported abnormalities have not been replicated, findings specific to the core social and communicative deficits have not yet been demarcated from nonspecific findings, and neurobiologic abnormalities have not been examined in a genetic perspective, which leaves open the question as to whether, where, and to what extent genetic influences on autism produce aberrant brain morphology or brain function. Drug treatment Given that the neurochemical basis of autism is unknown, there is as yet no place for pharmacotherapy based on defined pathogenesis of the core social and communicative deficits. The exception, perhaps, is intervention in the serotonin neurotransmitter system, which may be based on evidence for abnormalities in whole blood serotonin in a subgroup of individuals with autism. Fenfluramine is a halogenated amphetamine that promotes the release and inhibits the reuptake of serotonin and blocks dopamine receptors. Early studies reported dramatic improvements, but subsequent large-scale and controlled trials could not support the initial claims. Because of the potential neurotoxicity and reports of serious adverse effects, fenfluramine is no longer recommended for clinical use [86] . Clomipramine is a tricyclic antidepressant and a potent nonselective serotonin reuptake inhibitor. Treatment with clomipramine led to improvements in—among other areas— social behavior and aggression in two open-label studies, one with autistic patients [87] and one with adults with PDD [88] . Clomipramine was found to be superior to desipramine, a tricyclic noradrenergic uptake inhibitor, in a controlled study in autistic children and adolescents [89] . Treatment with clomipramine may result in troublesome and serious physical and behavioral side effects, however, and should be used judiciously. Three selective serotonin reuptake inhibitors—fluvoxamine, fluoxetine, and sertraline—also have been studied in autism. Overall, the results of the selective serotonin reuptake inhibitors are encouraging in adults with autism who are characterized by strong behavioral rigidity and obsessive-compulsive disorder-like symptoms. In contrast, children and adolescents seem to be sensitive to the stimulating adverse effects of selective serotonin reuptake inhibitors and have a much lower response rate [86] . Buspirone, an agonist of the serotonin 5-HT1a receptor, has been reported to decrease anxiety and affective lability [90] . So far only open studies have been reported. Other interventions have been developed, not so much based on a defined pathogenesis of autism but from a pragmatic perspective. Distressing or maladaptive symptoms, such as hyperactivity, aggression, anxiety, negativism, ritualized repetitive behaviors, and selfinjurious behaviors, can be the target of (drug) intervention. Although treatment of these symptoms does not cure autism, their effective treatment improves quality of life and enhances opportunities for appropriate education and community independence [91] . For these reasons an intervention with classic neuroleptic drugs, for example, the newer or “atypical” neuroleptic drugs, or psychostimulants can be an option, depending on the severity of symptoms such as motor stereotypies or hyperactivity (Table 3 ). Drug treatment, however, is seldom considered as a single intervention and is mostly part of a comprehensive, multidisciplinary treatment approach. Table 3. Treatment options for distressing or maladaptive symptoms Abbreviation: SSRIs = selective serotonin reuptake inhibitors. Rigidity, rituals SSRIs X Atypical antipsychotics X Hyperactivity, impulsiveness Aggression, self-injury Anxiety, affective symptoms X X X X X Stimulants X Naltrexone X Clonidine X Lithium X Beta-blockers X Anticonvulsants X Buspirone X Social and behavioral therapies There are many treatments for autism, most of which demand a substantial sacrifice of time, attention, and funds. The overall approach for PDD-NOS does not differ in a substantial way from strategies used in autism. Overall, it is generally accepted that behavior modification procedures can enable a child to develop better social and emotional relationships, learn better communicative skills, and decrease the intensity of stereotypic and bizarre behaviors. No single mode of treatment is ever likely to be effective for all children and all families. Instead, intervention must be adapted to the child's individual pattern of strengths and handicaps [92] [93] . Treatment should begin early and may need to continue, in one form or another, into adulthood [94] . Several specific treatments for autism are advocated with great enthusiasm. These approaches are often based on reports of open, uncontrolled experiments that made little allowance for natural developmental change and included only small sample sizes, however [43] . There are hardly any comparison studies between methods of treatment and few investigations designed to identify when and where a particular approach works best. The approaches to modify behavior in autistic subjects can be divided roughly into two different strategies: massed, discrete-trial learning (also called teacher- or therapistcentered learning or traditional behavioral learning) and social-pragmatic teaching (also called child-centered therapy, pivotal-behavior therapy, or incidental teaching) [66] . Eventually, many of the named therapies evolve to a point at which they include elements of both strategies. Summary There is consensus about the disorders that comprise the autistic spectrum, with autistic disorder, Asperger's disorder, and PDD-NOS as the most typical examples and Rett's disorder and disintegrative disorder as the other components. Important controversies regarding the precise definitions of autistic spectrum disorders and the boundaries between the milder manifestations of those disorders, particularly PDD-NOS, and nonautistic conditions have not been and cannot be resolved fully as long as there is no known biologic cause or consistent biologic or psychological marker. This includes issues as basic as whether the autistic spectrum is a predominantly unitary entity or a collection of more or less similar phenotypes with multiple, varying etiologies. This is why the highest long-term priority in the area of definite diagnosis is the search for biologic marker(s) for autism and related autism spectrum disorders [91] . In the absence of a medical test to unequivocally diagnose autism, definitions of autism and related conditions are based only on manifestations in overt behavior, with all the unreliability this entails. In the future, the discovery of biologic correlates, causes, and pathogenetic pathways will undoubtedly change the way in which autism is diagnosed and lead to a new nosology [95] . Until that time the definitions in the current versions of the classification systems should be considered in a state of evolution. The key problem of the current classification systems is the fact that the boundaries between the various disorders are fuzzy. Instead of a categorical approach, a more useful description might be that of “autistic spectrum disorder,” which reflects the range of severity of symptoms. Such a dimensional understanding of PDD is useful to clinicians, who may otherwise use nonspecific terms to avoid the categorical diagnosis of autism [31] . Rutter and Schopler [96] argued for separate clinical and research schemes because clinical and research needs are different. For research purposes it is desirable to have as much direct comparability across studies as possible. The focus is on a high degree of homogeneity within diagnostic groupings. A price must be paid for this detailed specification, and the main cost lies in the proportion of cases left undiagnosed. For example, there may be good scientific reasons for a narrowly defined categorical diagnosis that includes only individuals who definitely and clearly have a specifically defined condition and excludes individuals who may have the condition. For clinicians and educators, classification helps guide the selection of treatments for an individual. From this point of view, broader diagnostic concepts may be most appropriate [95] . References Kanner L. Autistic disturbances of affective contact. Nervous Child 1943;2:217-50. Kanner L, Eisenberg L. Early infantile autism:1943–1955. Am J Orthopsychiatry 1956;26:55-65. [3]. Waterhouse L, Wing L, Fein D. Re-evaluating the syndrome of autism in the light of empirical research. In: DawsonG, editors. Autism: nature, diagnosis and treatment New York: Guilford Press; 1989. p. 263-81. [4]. Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children. JAMA 2001;285:3093-9. Abstract [5]. Fombonne E. What is the prevalence of Asperger disorder? J Autism Dev Disord 2001;31:363-4. Citation [6]. Gillberg C, Wing L. Autism: not an extremely rare disorder. Acta Psychiatr Scand 1999;99:399-406. Abstract [7]. World Health Organization. Geneva: World Health Organization; 1992. International statistical classification of diseases and health related problems. 10th revision [8]. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4 th Washington, DC: American Psychiatric Association; 1994. [9]. Volkmar FR, Klin A, Siegel B, et al. Field trial for autistic disorder in DSM-IV. Am J Psychiatry 1994;151:1361-7. Abstract [10]. Volkmar FR, Cohen DJ. Debate and argument: the utility of the term pervasive developmental disorder. J Child Psychol Psychiatry 1991;32:1171-2. Citation [11]. Buitelaar JK, Van der Gaag RJ, Klin A, et al. Exploring the boundaries of PDD-NOS: analyses of data from the DSM-IV Autistic Disorder field trial. J Autism Dev Disord 1999;29:33-43. Abstract [12]. Schopler E, Mesibov GB, Kunce LJ. Asperger syndrome or high-functioning autism? New York: Plenum Press; 1998. [13]. Szatmari P. The validity of autistic spectrum disorders: a literature review. J Autism Dev Disord 1992;22:583-600. Abstract [14]. Cohen DJ, Paul R, Volkmar FR. Issues in the classification of pervasive and other developmental [1]. [2]. disorders: toward DSM-IV. J Am Acad Child Adolesc Psychiatry 1986;25:213-20. [15]. Waterhouse L. Severity of impairment in autism. In: BromanSH, GrafmanJ, editors. Atypical cognitive deficits in developmental disorders: implications for brain function Hillsdale: Lawrence Erlbaum; 1994. p. 263-81. [16]. Waterhouse L, Morris R, Allen D, et al. Diagnosis and classification in autism. J Autism Dev Disord 1996;26:59-86. Abstract [17]. Dahl EK, Cohen DJ, et al. Clinical and multivariate approaches to the nosology of pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry 1986;25:170-80. [18]. Rescorla L. Preschool psychiatric disorders. J Am Acad Child Adolesc Psychiatry 1986;25:162-9. [19]. Gillberg C. Outcome in autism and autistic-like conditions. J Am Acad Child Adolesc Psychiatry 1991;30:375-82. Abstract [20]. Szatmari P, Jones MB, Zwaigenbaum L, et al. Genetics of autism: overview and new directions. J Autism Dev Disord 1998;28:351-68. Abstract [21]. Sevin JA, Matson JL, Coe D, et al. Empirically derived subtypes of pervasive developmental disorders: a cluster analytic study. J Autism Dev Disord 1995;25:561-78. Abstract [22]. Gillberg C. Autism and autistic-like conditions: subclasses among disorders of empathy. J Child Psychol Psychiatry 1992;33:813-42. Abstract [23]. Rutter M, Bailey A, Bolton P, et al. Autism: syndrome definition and possible genetic mechanisms. In: PlominR, McLearnGE, editors. Nature, nuture, and psychology Washington, DC: American Psychological Association Press; 1993. [24]. Fombonne E. The epidemiology of autism: a review. Psychol Med 1999;29:769-86. Abstract [25]. Rutter M, Bailey A, Bolton P, et al. Autism and known medical conditions: myth and substance. J Child Psychol Psychiatry 1994;35:311-22. Abstract [26]. Cohen IR, Vietze PM, Sudhalter V, et al. Parent-child dyadic gaze patterns in fragile X males and in non-fragile X males with autistic disorder. J Child Psychol Psychiatry 1989;30:845-56. Abstract [27]. Wing L, Gould J. Severe impairments of social interaction and associated abnormalities in children: epidemiology and classification. J Autism Dev Disord 1979;9:11-29. Abstract [28]. Volkmar FR, Cohen DJ, et al. An examination of social typologies in autism. J Am Acad Child Adolesc Psychiatry 1989;28:82-6. Abstract [29]. Borden MC, Ollendick TH. An examination of the validity of social subtypes in autism. J Autism Dev Disord 1994;24:23-37. Abstract [30]. Rescorla L. Cluster analytic identification of autistic preschoolers. J Autism Dev Disord 1988;475-92. Abstract [31]. Myhr G. Autism and other pervasive developmental disorders: exploring the dimensional view. Can J Psychiatry 1998;43:589-95. Abstract [32]. Prior M, Eisenmajer R, Leekam S, et al. Are there subgroups within the autistic spectrum? A cluster analysis of a group of children with autistic spectrum disorders. J Child Psychol Psychiatry 1998;39:893902. Abstract [33]. Beglinger LJ, Smith TH. A review of subtyping in autism and proposed dimensional classification model. J Autism Dev Disord 2001;31:411-22. Abstract [34]. Stevens MC, Fein DA, Dunn M, et al. Subgroups of children with autism by cluster analysis: a longitudinal examination. J Am Acad Child Adolesc Psychiatry 2000;39:346-52. Full Text [35]. Aman MG, Kern RA. Review of fenfluramine in the treatment of developmental disabilities. J Am Acad Child Adolesc Psychiatry 1989;28:549-65. Abstract [36]. August GJ, Raz N, Baird TD. Fenfluramine response in high and low functioning autistic children. J Am Acad Child Adolesc Psychiatry 1987;26:342-6. Citation [37]. Ritvo ER, Freeman BJ, Geller E, et al. Study of fenfluramine in outpatients with the syndrome of autism. J Pediatr 1984;105:823-8. Abstract [38]. Buitelaar JK, Dekker M, Van Ree JM, et al. A controlled trial with ORG 2766, an ACTH(4–9) analog, in 50 relatively able children with autism. Eur Neuropsychopharmacol 1996;6:13-9. Abstract [39]. Szatmari P, Jones MB, Holden J, et al. High phenotypic correlations among siblings with autism and pervasive developmental disorders. Am J Med Genet 1996;67:354-60. Abstract [40]. Bolton P, Macdonald H, Pickles A, et al. A case-control family history study of autism. J Child Psychol Psychiatry 1994;35:877-900. Abstract [41]. Tanguay P, Robertson J, Derrick A. A dimensional classification of autism spectrum disorder by social communication domains. J Am Acad Child Adolesc Psychiatry 1998;37:271-7. Abstract [42]. Wing L. The continuum of autistic characteristics. In: SchoplerE, MesibovG, editors. Diagnosis and assessment in autism New York: Plenum Press; 1988. p. 91-110. [43]. Berney TP. Autism: an evolving concept. Br J Psychiatry 2000;176:20-5. Abstract [44]. Provence S, Dahl K. Disorders of atypical development: diagnostic issues raised by a spectrum disorder. In: CohenD, DonnellanA, PaulR, editors. Handbook of autism and pervasive developmental disorders New York: Wiley; 1987. p. 677-89. [45]. Bailey A, Palferman S, Heavey L, et al. Autism: the phenotype in relatives. J Autism Dev Disord 1998;28:369-91. Abstract [46]. Buitelaar JK, Van der Gaag RJ. Diagnostic rules for children with PDD-NOS and multiple complex developmental disorder. J Child Psychol Psychiatry 1998;39:911-20. Abstract [47]. Buitelaar JK, Van der Gaag RJ, Klin A, et al. Exploring the boundaries of PDD-NOS: analyses of data from the DSM-IV Autistic Disorder Field Trial. J Autism Dev Disord 1998; in press [48]. Van der Gaag RJ, Buitelaar J, Van der Ban E, et al. A controlled multivariate chart review of multiple complex developmental disorder. J Am Acad Child Adolesc Psychiatry 1995;34:1096-106. Abstract [49]. Wing L. Asperger's syndrome: a clinical account. Psychol Med 1981;11:115-30. Abstract [50]. Gillberg C. Asperger's syndrome in 23 Swedish children. Dev Med Child Neurol 1989;81:520-31. Abstract [51]. Ghaziuddin M, Butler E. Clumsiness in autism and Asperger syndrome: a further report. J Intellect Disabil Res 1998;42:43-8. Abstract [52]. Ehlers S, Gillberg C. The epidemiology of Asperger syndrome. J Child Psychol Psychiatry 1993;34:1327-50. Abstract [53]. Kadesjo B, Gillberg C, Hagberg B. Brief report: autism and Asperger syndrome in seven-year-old children: a total population study. J Autism Dev Disord 1999;29:327-31. Citation [54]. Ozonoff S, Rogers SJ, Pennington BF. Asperger's syndrome: evidence of an empirical distinction from high-functioning autism. J Child Psychol Psychiatry 1991;32:1107-22. Abstract [55]. Szatmari P, Tuff L, Finlayson AJ, et al. Asperger's syndrome and autism: neurocognitive aspects. J Am Acad Child Adolesc Psychiatry 1990;29:130-6. Abstract [56]. Klin A, Volkmar FR, Sparrow SS, et al. Validity and neuropsychological characterization of Asperger syndrome: convergence with nonverbal learning disabilities syndrome. J Child Psychol Psychiatry 1995;36:1127-40. Abstract [57]. Ehlers S, Nyden A, Gillberg C, et al. Asperger syndrome, autism and attention disorders: a comparative study of the cognitive profiles of 120 children. J Child Psychol Psychiatry 1997;38:207-17. Abstract [58]. Gilchrist A, Green J, Cox A, et al. Development and current functioning in adolescents with Asperger syndrome: a comparative study. J Child Psychol Psychiatry 2001;42:227-40. Abstract [59]. deLong GR, Dwyer J. Correlation of family history with specific autistic subgroups: Asperger's syndrome and bipolar affective disorder. J Autism Dev Disord 1988;18:593-600. Abstract [60]. Szatmari P. Asperger's syndrome: diagnosis, treatment, and outcome. Psychiatr Clin North Am 1991;14:81-93. Abstract [61]. Volkmar FR, Rutter M. Childhood disintegrative disorder: results of the DSM-IV autism field trial. J Am Acad Child Adolesc Psychiatry 1995;34:1092-5. Abstract [62]. Volkmar FR. Childhood disintegrative disorder: issues for DSM-IV. J Autism Dev Disord 1992;22:625-42. Abstract [63]. Volkmar FR, Cohen DJ. Disintegrative disorder or “late onset” autism. J Child Psychol Psychiatry 1989;30:717-24. Abstract [64]. Mouridsen SE, Rich B, Isager T. Epilepsy in disintegrative psychosis and infantile autism: a long-term validation study. Dev Med Child Neurol 1999;41:110-4. Abstract [65]. Tsai L. Is Rett syndrome a subtype of pervasive developmental disorder? J Autism Dev Disord 1992;22:551-61. Abstract [66]. Tanguay PE. Pervasive developmental disorders: a 10-year review. J Am Acad Child Adolesc Psychiatry 2000;39:1079-95. Full Text [67]. Hagberg B. Rett's syndrome: prevalence and impact on progressive severe mental retardation in girls. Acta Paediatr Scand 1885;74:405-8. [68]. Shastry BS. Molecular genetics of Rett syndrome. Neurochem Int 2001;38:503-8. Abstract [69]. Prior MR, MacMillan MB. Kanner's syndrome or early onset psychosis: a taxonomic analysis of 142 cases. Journal of Autism and Childhood Schizophrenia 1973;5:71-80. [70]. Siegel B, Anders TF, Ciaranello RD, et al. Empirically derived subclassification of the autistic syndrome. J Autism Dev Disord 1986;16:275-93. Abstract [71]. Cohen DJ, Paul R, Volkmar FR. Issues in the classification of pervasive developmental disorders and associated conditions. In: CohenDJ, DonnellanAM, editors. Handbook of autism and pervasive developmental disorders New York: Wiley & Sons; 1987. p. 20-40. [72]. Cohen DJ, Towbin KE, Mayes L, et al. Developmental psychopathology of multiplex developmental disorder. In: FriedmanSL, HaywoodHC, editors. Developmental psychopathology of multiplex developmental disorder New York: Academic Press; 1994. [73]. Towbin K, Dykens EM, Pearson GS, et al. Conceptualizing “borderline syndrome of childhood” and “childhood schizophrenia” as a developmental disorder. J Am Acad Child Adolesc Psychiatry 1993;32:775-82. Abstract [74]. Kumra S, Jacobsen LK, Lenane M. Multidimensionally impaired disorder: is it a variant of very earlyonset schizophrenia? J Am Acad Child Adolesc Psychiatry 1998;37:91-9. Abstract [75]. Ad-Dab'bagh Y, Greenfield B. Multiple complex developmental disorder: the “multiple and complex” evolution of the “childhood borderline syndrome” construct. J Am Acad Child Adolesc Psychiatry 2001;40:954-64. Abstract [76]. Smalley SL. Genetic influences in childhood-onset psychiatric disorders: autism and attentiondeficit/hyperactivity disorder. Am J Hum Genet 1997;60:1276-82. Citation [77]. Cook EH. Genetics of autism. Child Adolesc Psychiatr Clin N Am 2001;10:333. Abstract [78]. Saitoh O, Karns CM, Courchesne E. Development of the hippocampal formation from 2 to 42 years. Brain 2001;124:1317-24. Abstract [79]. Woodhouse W, Bailey A, Rutter M, et al. Head circumference in autism and other pervasive developmental disorders. J Child Psychol Psychiatry 1996;37:665-71. Abstract [80]. Piven J, Arndt S, Bailey J, et al. Regional brain enlargement in autism: a magnetic resonance imaging study. J Am Acad Child Adolesc Psychiatry 1996;35:530-6. Abstract [81]. Filipek PA. Brief report: neuroimaging in autism: the state of the science 1995. J Autism Dev Disord 1996;26:211-5. Citation [82]. Courchesne E, Karns BS, David HR, et al. Unusual brain growth patterns in early life in patients with autistic disorder: an MRI study. Neurology 2001;57:245-54. Full Text [83]. Saitoh O, Karns CM, Courchesne E. Development of the hippocampal formation from 2 to 42 years: MRI evidence of smaller area dentata in autism. Brain 2001;124:1317-24. Abstract [84]. Anderson GM, Horne WC, Chatterjee D, et al. The hyperserotonemia of autism. Ann N Y Acad Sci 1990;600:331-42. Abstract [85]. Cook EHJ, Leventhal BL, Heller W, et al. Autistic children and their first-degree relatives: relationships between serotonin and norepinephrine levels and intelligence. J Neuropsychiatry Clin Neurosci 1990;2:268-74. Abstract [86]. Buitelaar JK, Willemsen-Swinkels SHN. Autism: current theories regarding its pathogenesis and implications for rational pharmacotherapy. Paediatric Drugs 2000;2:1-5. [87]. McDougle CJ, Price LH, Volkmar FR, et al. Clomipramine in autism: preliminary evidence of efficacy. [case study] J Am Acad Child Adolesc Psychiatry 1992;31:746-50. Abstract [88]. Brodkin ES, McDougle CJ, Naylor ST, et al. Clomipramine in adults with pervasive developmental disorders: a prospective open-label investigation. J Child Adolesc Psychopharmacol 1997;7:109-21. Abstract [89]. Gordon CT, Cotelingam GM, Stager S, et al. A double-blind comparison of clomipramine and desipramine in the treatment of developmental stuttering. J Clin Psychiatry 1995;56:238-42. Abstract [90]. Buitelaar JK, Van der Gaag RJ, Van der Hoeven J. Effects of buspirone in the management of anxiety and irritability in children with pervasive developmental disorders: open pilot data. J Clin Psychiatry 1998;56-9. Abstract [91]. Bristol-Power MM, Spinella G. Research on screening and diagnosis in autism: a work in progress. J Autism Dev Disord 1999;29:435-8. Abstract [92]. Howlin P. Prognosis in autism: do specialist treatments affect long-term outcome? Eur Child Adolesc Psychiatry 1997;6:55-72. Abstract [93]. Howlin P. Practitioner review: psychological and educational treatment for autism. J Child Psychol Psychiatry 1998;39:307-22. Abstract [94]. Rogers SJ. Brief report: early intervention in autism. J Autism Dev Disord 1996;26:243-6. Citation [95]. Volkmar FR, Klin A, Cohen DJ. Diagnosis and classification of autism and related conditions: consensus and issues. In: CohenDJ, VolkmarFR, editors. Handbook of autism and pervasive developmental disorders New York: Wiley; 1997. p. 5-40. [96]. Rutter M, Schopler E. Classification of pervasive developmental disorders: some concepts and practical considerations. [see comments] J Autism Dev Disord 1992;22:459-82. Abstract [97]. Eaves LC, Ho HH, Eaves DM. Subtypes of autism by cluster analysis. J Autism Dev Disord 1994;24:3-22. Abstract [98]. Fein D, Stevens M, Dunn M. Subtypes of pervasive developmental disorder: clinical characteristics. Child Neuropsychology 1999;5:1-23. [99]. Carpentieri S, Morgan S. Adaptive and intellectual functioning in autistic and nonautistic retarded children. J Autism Dev Disord 1996;26:611-20. Abstract [100]. DeMyer MK, Barton S, DeMyer W, et al. Prognosis in autism: a follow-up study. J Autism Child Schizophr 1973;3:199-246. Citation [101]. Bartak L, Rutter M. Differences between mentally retarded and normally intelligent autististic children. Journal of Autism and Childhood Schizophrenia 1976;6:109-20. [102]. Waterhouse L, Fein D. Developmental trends in cognitive skills for children diagnosed as autistic and schizophrenic. Child Dev 1984;55:236-48. Abstract [103]. DeLong R. Children with autistic spectrum disorder and a family history of affective disorder. Dev Med Child Neurol 1994;36:674-87. Abstract [104]. Volkmar FR, Cohen DJ, Hoshino Y. Phenomenology and classification of the childhood psychoses. Psychol Med 1988;18:191-201. Abstract [105]. Volkmar FR, Szatmari P, Sparrow SS. Sex differences in pervasive developmental disorders. J Autism Dev Disord 1993;23:579-91. Abstract Review article Autism Roberto Tuchman, MD Dan Marino Center Department of Neurology Miami Children's Hospital 2900 South Commerce Parkway Weston, FL 33331, USA E-mail address: tuchman@att.net PII S0733-8619(03)00011-2 Autism is a complex neurodevelopmental disorder that is behaviorally defined. The behavioral manifestations that define autism include qualitative deficits in social interaction and communication and restricted repetitive and stereotyped patterns of behavior, activities, and interests [1] . Autism defines children at a behavioral level and is associated with multiple etiologies. The phenotypic presentation of autism is influenced by factors that are not part of the defining features of this disorder. One aspect of autism that is not part of the diagnostic criteria but is an important prognostic indicator is cognitive ability. The wide range of social skills, communication abilities, and patterns of behavior that occur in autism are best captured by the term “autism spectrum disorders” (ASDs) [2] [3] . Autism is a prototype disorder of sociocognitive development that provides an important opportunity to observe and delineate the regions of the brain that are responsible for behaviors that define social cognition and communication. Recent reports indicate that there is an explosion of children given the diagnosis of an ASD. Prevalence figures range from 4 to 10 per 10,000 up to 2 to 5 per 1000 [4] . Reports disagree, however, on whether or not prevalence truly has increased. One explanation for the increased diagnosis is that there is a greater awareness of the ASDs, especially in mildly affected children and in those with severe mental retardation [5] . The purpose of this article is to review the current clinical and neurobiologic understanding of autism. Clinical perspective Impairment of social interaction in ASD may manifest as social isolation or inappropriate social behavior. These deficits in social interaction are represented by gaze avoidance, failure to respond when called, failure to participate within groups, lack of awareness of others, indifference to affection or inappropriate affection, and a lack of social or emotional empathy. As individuals enter adulthood, there is in general an amelioration of the social isolation, but the poverty of social skills and the impaired ability to make peer friendships persist. Adolescents and adults with autism have significant misperceptions of how others perceive them, and the adult with autism and adequate cognitive skills is in general a loner. Impairment in communication affects verbal and nonverbal abilities to share information with others. Deficits in communication are variable. In some children they are characterized by failure to develop expressive and receptive language skills. In others, language is immature and characterized by echolalia, pronoun reversals, unintelligible jargon, and abnormal melody (sing-song prosody, monotonous tone, or abnormal tone). In those who have adequate speech there may be an inability to initiate or sustain an appropriate conversation. Language and communication deficits persist into adulthood and a significant proportion of individuals with autism remains nonverbal. Those who do acquire verbal skills demonstrate persistent deficits in conversational skills, such as taking turns and understanding the subtleties of language including jokes or sarcasm. Deficits in communication also manifest as an impaired ability to interpret body language, intonation, and facial expressions. Repetitive and stereotyped patterns of behavior characteristic of autism include resistance to change, insistence on certain routines, attachments to objects, and fascination with parts and movement of objects, such as the turning wheels of cars or fans. Children may play with toys but are preoccupied with lining up or manipulating the toys, as opposed to using them symbolically. Motor and verbal stereotypies, such as flapping, humming, rocking, running around in circles, or repetition of certain words, phrases, or songs, also are frequent manifestations of autism. In the adult with autism, adaptation to change improves but the restricted interests persist and those with adequate cognitive skills tend to focus on narrow topics, such as train schedules, maps, or historical facts, which dominate their lives. In the absence of a biologic marker, diagnosing autism and delineating its boundaries remain somewhat arbitrary clinical decisions. The behavioral manifestations of individuals with autism are not limited to this group of children and can be seen in the larger population of individuals with social communication spectrum disorders [6] . The DSM-IV criteria classify children under the terminology, “pervasive developmental disorders,” and include five subgroups in this category (Table 1 ). The core clinical feature that defines autism and related disorders is a disturbance of social interaction, but this deficit in social interaction is not absolute and the social behaviors of individuals with autism differ depending on their cognitive level, developmental stage, associated disabilities, and the type of social structure in which they are observed [7] . It is reasonable to postulate that the regions in the brain essential for social cognition and communication are distributed widely and may be affected to different degrees in individuals with social communication disorders. The degree to which these social brain regions are affected and the degree to which other associated brain regions, such as those of language and motor function, are involved account for the clinical heterogeneity of social communication spectrum disorders. Table 1. Pervasive developmental disorders Subtypes of autistic Characteristics spectrum disorders Autistic disorder Classic autism with deficits in sociability and language and with repetitive behaviors and a restricted repertoire of interests. Symptoms usually are present from infancy or the toddler years (<3 years). Approximately 30% of children have unexplained regression, usually between 18 and 24 months, of language and sociability. Asperger syndrome (AS) Language develops better than in classical autism and cognition is better. Individuals with AS, however; have problems with the semantic and pragmatic use of language. Many of these individuals are misdiagnosed early on and in adulthood may be described as odd or eccentric. Pervasive developmental disorder, not otherwise specified These are individuals who do not meet full criteria for any other subtype of pervasive developmental disorder. There is wide range of cognitive and behavioral problems in this group of children, but in general, the social, communicative, and behavioral deficits, although similar to autism, are less severe. Childhood disintegrative disorder Children who between ages 2 and 10, after entirely normal early development of language, sociability, and cognition, experience a regression in at least two of the following areas: language, social skills, bowel or bladder control, play or motor skills. Cognitive skills usually are significantly impaired. Rett syndrome Specific X-linked genetic deficit strongly associated with mutations of the MECP2 gene. It affects postnatal birth growth, resulting in severe mental retardation and motor deficits. It is associated with a specific “hand-washing” stereotypy. Although there is loss of social interaction early, if often improves later in the course of the disorder. There is no biologic test to diagnose autism; as such, the goal of neurologic examination is to assess which, if any, tests are needed depending of course on the history and neurologic examination. The initial work-up (Table 2 ) of an individual with autism should have a clear clinical purpose and should be differentiated from research goals. There are evidence-based guidelines that have been established for the diagnosis of autism and related disorders [8] . Autism may be associated with diverse etiologies and with a variety of medical disorders including seizures. The role of the neurologist is to determine if a specific etiology can be established in an individual with autism and to determine how this information has an impact on prognosis, genetic counseling, and, in the rare situation, a specific therapeutic intervention. Table 2. Initial diagnostic evaluation of autistic spectrum disorder From Filipek PA, Accardo PJ, Ashwal S, et al. Practice parameter: screening and diagnosis of autism: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology 2000;55:468; with permission. Work-up Key points Clinical history (1) Parental report is usually better than what one observes in a brief office visit. Gathering several sources of information sometime may be essential for diagnosis. (2) The use of standardized questionnaires is extremely helpful in the screening and diagnosis of autism. (3) A family history specifically probing for a history of other family members with social deficits, manic-depression, obsessivecompulsive disorder, language disorders, or seizures. Clinical examination (1) Observation of how a child plays, especially with representational toys, is an important clinical tool and essential to assess a young child's language, cognitive ability, sociability, and affect. (2) Look for physical abnormalities, usually minor, that may help diagnose a genetic disorder. (3) Examine for skin manifestations that may suggest a neurocutaneous syndrome. (4) Stereotypies are not diagnostic but are present in the majority of children with autism. (5) The head circumference in children with autism may be at upper limit of normal. Standarized tests and (1) Hearing test evaluations (2) Communication assessment by speech and language pathologist. (3) Assessment by occupational or physical therapist specifically in those with motor deficits, motor planning, or sensory dysfunction. (4) Neuropsychologic batteries are valuable for planning individualized intervention programs. Genetic and metabolic studies (1) Chromosome studies to detect a syndromic condition, fragile-X, or some other possibly genetic etiology. Depending on the clinical situation, genetic consultation may be appropriate. (2) Metabolic tests are needed only if the history or examination suggests (ie, family history of mental retardation or if the child has not been screened at birth). Neuroimaging studies (1) Imaging studies are indicated only if the neurologic examination suggests it or if the child is a candidate for specific intervention such as epilepsy surgery. Table 2. Initial diagnostic evaluation of autistic spectrum disorder Neurophysiology studies (1) A one-hour sleep EEG should be done if any suspicious behavioral episode that might represent a seizure. (2) In selective situations, such as children with a history of autistic regression, no speech, and severe comprehension deficits, an overnight EEG that captures slow-wave sleep is indicated. (3) Prolonged video-EEG monitoring also may be indicated if suspicious behavioral episodes persist despite a normal one-hour sleep EEG and in those children with severe comprehension deficits that are not improving. Social, cognitive, and related disabilities The defining features of the social communication deficits in children with autism include deficits in joint attention (defined as the behaviors used to share the experience of objects or events with others), disturbances in affect, impairments in imitation, impairments in the capacity for pretend play with objects or people, and impairments in the ability to attribute beliefs to the self and others (theory of mind) [9] [10] [11] [12] [13] [14] [15] . In addition, cognitive level, language and communication skills, motor function, patterns of behavior, interests, and activities all contribute to social functioning. Assessment in autism requires a multidisciplinary approach and the use of objective scales. One of the most widely used assessment tools in the United States is the Childhood Autism Rating Scale (CARS) [16] . Evidence suggests that factor analysis– based scores using the CARS is helpful in identifying subgroups of children with autism. Five factors have emerged from this factor analysis, including social communication, emotional reactivity, social orienting, cognitive and behavioral consistency, and odd sensory exploration [17] . This study [17] suggests that even within the ASD population there are distinguishing aspects of the social deficit that can be quantified objectively and used to differentiate subgroups within the larger spectrum. The most comprehensive systems available for the diagnosis of autism are the Autism Diagnostic Observation System and the Autism Diagnostic Interview, which together provide a structured detailed interview and an observation method to assess objectively an individual's social ability, communication skills, and behavior [18] [19] [20] [21] [22] . Specific “social communication” handicaps can be identified in ASD using the Autism Diagnostic Observation Schedule, and three factors seem to play a crucial role: joint attention, affective reciprocity, and theory of mind [23] . These three social communication domains are central to social development in most children, and when they do not develop appropriately they account for the core deficits seen in social communication spectrum disorders. Cognition is not part of the clinical criteria for autism but is an important variable that influences diagnosis, is related to associated medical disabilities (such as rates of epilepsy), and predicts outcome [24] [25] . Measures of nonverbal problem solving in highfunctioning individuals with autism correlate with outcome, and the severity of autistic behaviors is a poor predictor of prognosis [26] . Children and adults with autism who have severe cognitive deficits and those who have normal or above-average intelligence may form distinct subgroups [27] . Symptoms or behaviors of autism represent a different dimension from level of functioning, and these two factors largely are responsible for the variability of the phenotype that occurs in autism [28] . Cognitive deficits in autism are characterized by impairment in the processing of information and the transfer of this information into symbolic representations [29] . There is evidence suggesting that all persons with autism have a cognitive deficit affecting their perception of the world, that they have an impaired capacity to see things from another person's point of view, and that they have little awareness of the mental states of other people (metacognition theory) [30] [31] [32] . This “theory of mind” has been proposed as central to the cognitive dysfunction of the individual with autism; evidence suggests that understanding of false belief and understanding of emotion may be distinct aspects of social cognition in young children [33] . Approximately one third of children fulfilling criteria for a diagnosis of autism are reported to lose language and social skills in the second year of life [34] [35] [36] . There is no accepted definition of regression and, despite reports by parents of single words or phrases that drop out accompanied by decreased social play and increased irritability, this phenomena frequently is overlooked. It often is difficult to ascertain if development truly was normal before the regression [37] . Investigators who examined family videotapes made before the identification of symptoms of autism often found evidence of preexisting developmental differences [38] [39] . There is some preliminary evidence that cognitive impairment is more likely in people with ASD who experience regression [40] . There also is controversy regarding whether or not disintegrative disorder and autistic regression are discrete entities [41] . There are no prospective studies of autistic regression, therefore the true nature and incidence of regression are not well understood. Epilepsy is common in autism, but the rates of seizures vary, with the highest risk in those with the greatest degree of cognitive and motor impairment and the most significant deficits in receptive language deficit. There has been significant controversy regarding the causal role of seizures in autism. The relationship of children who have autism, regression of language, and an epileptiform EEG to those children with Landau-Kleffner syndrome (LKS) is not presently understood. Specific age, behavioral, and EEG profile differences between children with autistic regression and seizures or an epileptiform EEG and those children with LKS do exist, and this may have important etiologic and therapeutic implications. The complex and controversial relationship between autism and epilepsy (clinical and subclinical) recently has been reviewed by Tuchman and Rapin [42] . Neurobiologic overview Earlier studies of autism suggested that cerebellar abnormalities in autism may account for inability to execute rapid attentional shifts and that this impairment in shifting attention, possibly in conjunction with abnormalities in other neuronal systems, impairs social and cognitive development and produces the behavioral manifestations characteristic of autism [43] . More recent studies have focused on specific cortical areas and, at least in boys with autism, a significant asymmetry reversal in language-related inferior-lateral-frontal and posterior-superior-temporal regions and in inferior temporal regions involved in visual face processing has been identified [44] . One of the more interesting and relevant areas to the understanding of a social cognition neuronal network is the evidence that facial recognition is impaired early on in autism and that the amygdala is crucial in the development of this facial recognition by providing emotional valence to the fusiform face area [45] [46] [47] . It now can be reasonably stated that neuronal networks dedicated to social cognition do exist and that specific regions of the brain important for social cognition can be reliably identified and measured [48] . Current understanding of the neuropathology of autism is limited. In the small number of brains studied, investigators have found consistent neuropathologic changes in the limbic system and in cerebellar circuits. Cells in the limbic system (hippocampus, amygdala, mamillary body, anterior cingulate gyrus, and nuclei of the septum) are small in size and increase in number per unit volume (increased cell packing density). In these studies, the cerebellum showed a decreased number of Purkinje cells, especially in the posterolateral neocerebellum and adjacent archicerebellar cortex (posterior and inferior portions of the cerebellum) [49] [50] [51] . In addition to the developmental abnormalities of the brainstem, cortical abnormalities have been found in the few number of brains that have been studied [52] . Recently, a paradigm that emphasizes the role of circuits and information processing within the brain, rather than single-cell pathology, has been introduced to investigate the neuropathology of autism and other developmental disorders of the brain [53] . This paradigm is based on the finding that minicolumnar organization of the brain of individuals with autism is abnormal and shows cell columns that are more numerous, smaller, and less compact in their cellular configuration and have reduced neuropil space in the periphery [54] . MRI studies have demonstrated abnormalities of the posterior fossa structures in autism, including hypoplasia of cerebellar vermal lobules VI and VII and diminished size of the brainstem [55] [56] [57] . Findings of cerebellar abnormalities have not been consistently reproduced and some investigators have stated that previous reports of posterior fossa abnormalities may be related to technical and methodologic factors [58] . A meta-analysis of data from separate laboratories suggests a bimodal distribution in the measurements of the cerebellar vermis in subjects with autism. A subgroup with hypoplasia of vermal lobules VI and VII and a subgroup with hyperplasia were found. The majority (>80%) of patients fell into the hypoplasia group. Besides differing from each other, the groups differed significantly from control patients [43] [59] . There is a discrepancy, however, between neuropathologic and neuroradiologic studies. Neuropathologic studies have shown that maximal anatomic abnormalities are in the posterior and inferior portions of the cerebellar hemispheres and involve cell loss. The cell loss now has been found in the entire cerebellum and affects the vermis evenly (it is not confined to lobules VI and VII). Neuroimaging studies demonstrate a decrease in tissue area confined mostly to lobules VI and VII. The vermis, however, may turn out to be the best in vivo indicator that the cerebellum as a whole is abnormal in autism and the emphasis on MR imaging of vermal lobules I-V and VI-VII in the autism literature may reflect merely the ease and reliability with which these structures can be measured [60] . Other studies suggest that, in children with cerebellar hypolasia and autism, the degree of cerebellar hypoplasia can be correlated with slowed attentional responses to visual cues in a spatial attention paradigm [61] . This has become a timely topic of discussion, as the literature continues to suggest that the cerebellum may have an important role not only in autism but also in other disorders of higher cognitive function [50] . There also is some preliminary data suggesting that deficits in procedural learning in autism may be important and that these deficits may reflect dysfunction in the cerebellum [62] . Morphometric analysis has demonstrated that male autistic subjects have enlarged brains and that the enlargement of the brain is a result of greater brain tissue volume and greater lateral ventricle volume [63] . Other morphometric studies did not find a larger brain in autistic patients compared with control patients but did report reductions in volume in the amygdala and in the hippocampus, particularly in relation to total brain volume [64] . These studies suggest that the histopathology of autism and that the reductions of volume are related to dendritic tree and neuropil underdevelopment and that this likely reflects the lack of fully developed connections between limbic structures and cerebral cortex. Structural MRI data in high-functioning individuals with autism has identified graymatter differences in an amygdala-centered system relative to age- and IQ-matched control patients. Decreases in gray matter were found in anterior parts of this system (right paracingulate sulcus and left inferior frontal gyrus) and increases were found in posterior parts (amygdala/periamygdaloid cortex, middle temporal gyrus, and inferior temporal gyrus) and in regions of the cerebellum [65] . Several studies have found that brain development in autism follows an abnormal pattern [66] . These studies have found accelerated brain growth during the first few years in children with autism resulting in brain enlargement in early childhood [67] . In adolescents and adults with autism, brain volume is normal secondary to a slight decrease in brain volume during late childhood, the time when most children experience a slight increase in brain growth [68] [69] . The role of the amygdala and related structures in autism also has been documented by functional MRI (fMRI) studies in patients with autism or Asperger syndrome in whom activation of the front temporal regions, but not the amygdala, occurs when making mentalistic (theory of mind) inferences from the eyes [70] . This is in contrast to control patients who did show activation of the superior temporal gyrus and amygdala, which is the brain system proposed to be at the core of the “social brain network.” Positron emission tomography (PET) findings in autistic subjects include modest and not always significant global increase in resting cerebral glucose use, mostly in the basal ganglia, frontal, temporal and parietal lobes, whereas others have found no significant differences between autistic and control subjects [71] . The lack of consistent abnormalities in PET studies of autism may be the result of the heterogeneous nature of the disorder that makes comparisons of group differences unreliable. A PET study of a group of five highfunctioning autistic males (compared with a control group) showed (1) reversed hemispheric dominance during verbal auditory stimulation; (2) a trend toward reduced activation of auditory cortex during acoustic stimulation; and (3) reduced cerebellar activation during nonverbal auditory perception [72] . PET using “theory of mind” tasks in control subjects and in subjects with Asperger syndrome have demonstrated a lack of normal activation of the left prefrontal area in those with Asperger syndrome. Instead, children with Asperger syndrome activated neighboring areas of the brain, suggesting a nonspecific reasoning mechanism for inferring mental states [73] . The most consistent neurochemical finding in autism has been an elevation in platelet serotonin levels [74] . Despite extensive research, neither the relationship of this finding to concomitant mental retardation nor the mechanism of the hyperserotoninemia has been elucidated. Cook has suggested that hyperserotoninemia in autism may be heterogeneous, as one subgroup of subjects demonstrated increased 5-HT uptake and another subgroup decreased 5-HT2 binding [75] . A role for other monoamine neurotransmitters has been suggested, however; aside from serotonin, the only other consistently replicated neurochemical finding in autism has been elevated norepinephrine plasma levels [76] . In a series of studies using PET scans, altered serotonin synthesis in the dentatothalamocortical pathway in autistic males has been demonstrated. Furthermore, it has been documented that there is a lack of the normal high-brain serotonin synthesis period in children with autism [77] [78] . Electrophysiologic studies of autistic children have included clinical EEG studies and evoked potential studies. Clinical EEG studies performed on autistic children have revealed abnormal EEGs in 13% to 83% of cases [36] . The clinical diagnostic criteria used for autism, the associated medical disorders that coexist, and the methods of recording and interpreting clinical EEGs likely account for the variability in rates among studies. Prolonged EEG studies are significantly more likely to identify abnormalities than routine one-hour studies, at least in children with ASD and a history of regression. VideoEEG 23-hour overnight telemetry studies of children with ASD and regression, but without seizures, have found that 46% have an epileptiform EEG [24] . Magnetoelectroencephalography (MEG) studies of children with ASD and regression (and suspected history of seizures) have found epileptiform activity in 82% [79] . The high rate of seizures and epileptiform abnormalities in ASD are especially interesting in light of emerging data on the role of the amygdala in autism, as the amygdala also is a known to be a highly epileptogenic structure. It is likely, however, that the immunologic abnormalities described previously and the EEG findings reported in autism represent epiphenomena and are not a primary etiology in autism. Evoked potential studies have shown no consistent abnormality in either the brainstem auditory evoked potential (BAEP) or the middle latency responses (MLRs) of patients with nonretarded autistic disorder [80] . Clinical reports and research, however, continue to suggest the possibility of specific abnormalities [81] [82] [83] . In general, reviews of the literature on auditory brainstem response in autism have found overall contradictory results, with some studies finding prolongation but others shortening and no abnormalities in central transmission latencies [84] . Evoked potential studies also have been used to document abnormalities in face processing and attention in children with autism [45] [85] . Genetic studies have demonstrated an increased recurrence risk for autism of approximately 3% to 8% in families with one autistic child [86] . The search for autism genes is complicated and, although many chromosomes have been implicated in autism, no definite answers are available [87] [88] [89] . One point learned from experience determining genetic links in autism is that specific clinical characterization of the language and social deficits of the individuals studied has to be performed [22] [90] . This has been shown in work looking at the relationship between chromosome 2 and autism [91] [92] . Other chromosomes of interest in autism include chromosome 15 [93] [94] and chromosome 7 [95] [96] [97] . Despite rare clinical reports documenting mutations in methylCpG-binding protein 2 (MECP2) gene, which is a known cause of Rett syndrome, this gene does not play a major role in the majority of individuals with autism [98] . Other possible genetic causes that have been investigated are the roles of the HOXA1 gene and the reelin gene, but the data implicating these genes in the etiology of autism is inconsistent [99] [100] [101] [102] [103] [104] . No genes or chromosomes involved in autism have been definitely identified, but the heritability of autism is difficult to dispute. Investigators have become increasingly aware of the importance of identifying and quantifying the core social and communication deficits in the broader autism phenotype to elucidate the specific contribution of genetics to this heterogeneous disorder [105] . Overview of intervention The data from neurobiologic investigations of autism suggest that specific networks in the brain, such as the amygdala and related regions crucial for social communication, can be identified [48] [106] . When these regions of the brain are dysfunctional, there are deficits in joint attention, affective reciprocity, and theory of mind. If these deficits can be identified early, then specific interventions can be implemented. Then understanding of the plasticity of the brain can be used to maximize potential. To a limited extent, this is currently ongoing in autism behavioral and educational intervention research in young children with autism [107] [108] [109] [110] . Management of individuals with autism requires a multidisciplinary approach. Appropriate behavioral management techniques, educational or work programs, and communication techniques form the basis of management. Working with a psychologist or educators well versed in functional behavioral analysis and behavioral management techniques is essential. In individuals with autism and deficits in motor function, such as problems with motor planning, an occupational therapist is helpful. The role of the neurologist is to coordinate these diverse interventions and guide the family in evidencebased interventions that take into account the findings of the neurologic examination and assessment. As understanding of the neurochemical basis of the social networks of the brain becomes more sophisticated, specific pharmocotherapeutic interventions will be developed. At present, there is emerging evidence to suggest that in autism, serotonergic neurotransmission is dysfunctional [74] [111] . In light of these findings, specific interventions that modulate the serotonergic system, such as the selective serotonin reuptake inhibitors (SSRIs), may have a role in the treatment of autism and related disorders of social communication [112] [113] . The atypical antipsychotics that block postsynaptic dopamine and serotonin receptors have attracted clinical and research interest as potential agents in the treatment of autism. A multisite randomized double-blind trial found that specific symptoms significantly improved with the use of risperidone compared with placebo [114] . McCracken et al demonstrated that risperidone, over an eight-week period, was well tolerated and effective for the treatment of tantrums, aggression, or self-injurious behavior in children and adolescents with autism [114] . This study highlights many of the shortcomings of clinical and research drug therapy for autism in that the core symptoms of autism (ie, social communication and language) are not targeted. In general, improvement in core symptoms is difficult to measure and in the vast majority of clinical situations medications are treating the associated and not the core symptoms of autism. The known increased risk of seizures in autism has led to clinical, but mostly anecdotal, reports of treatment with antiepileptic drugs (AEDs) in individuals with autism. In the absence of clinical trials, however, no definite recommendations can be made regarding any specific AEDs treatment. The role of AEDs in the treatment of autism recently has been reviewed [115] . The co-occurrence of autism, epilepsy, and affective disorders is common, and these disorders may therefore share a common neurochemical substrate, which is targeted by the psychotropic mechanism of action of several AEDs [116] . There continues to be a great deal of interest regarding immunologic abnormalities in autism and the possibility of a specific abnormality in the opioid system, which could lead to specific types of interventions [117] [118] [119] . Several studies have attempted treatment using immunoglobulins, steroids, diet, and specific opioid blockers such as naltrexone [120] [121] [122] [123] [124] . This line of research, however, has been controversial and the scientific evidence to suggest that interventions based on these theories are successful has been inconsistent [125] [126] [127] [128] . The use of medication in autism remains limited. Nevertheless, there are well documented successful uses of medications in autism to treat symptoms such as anxiety, obsessive-compulsive behaviors, aggression, impulsivity, and hyperactivity [129] [130] [131] [132] . Intervention programs in autism emphasize an applied behavior analysis approach and have in common key elements such as intensity, structure, and frequency, but there still is significant controversy over the most effective types of intervention for maximizing an individual's potential and leading to successful outcome [133] [134] [135] [136] . The types of intervention and potential neurobiologic factors that predict successful outcome need to be clarified further [137] [138] [139] . Being social is a complex act that touches the essence of humanity. The networks in the brain responsible for social cognition and communication are distributed widely and are linked to many regions of brain function. These neuronal networks are specified by the genome, but just as genetics dictate how these pathways develop, the experiences of being social in turn sculpt these networks. As such, the importance of early intervention for all children with developmental disorders of social communication cannot be overemphasized [140] . Social, affective, and cognitive developmental research into ASDs will continue to provide a window into the complexities of brain-behavior relationships with practical implications for all members of society. References Pervasive developmental disorders. In: American Psychiatric Association, editors. Diagnostic and statistical manual of mental disorders Washington, DC: American Psychiatric Association; 1994. p. 65. [2]. Szatmari P. The validity of autistic spectrum disorders: a literature review. J Autism Dev Disord 1992;22:583. Abstract [3]. Rapin I. The autistic-spectrum disorders. N Engl J Med 2002;347:302. Citation [4]. Fombonne E. Epidemiological trends in rates of autism. Mol Psychiatry 2002;7(Suppl 2):S4. Citation [5]. Wing L, Potter D. The epidemiology of autistic spectrum disorders: is the prevalence rising? Ment Retard Dev Disabil Res Rev 2002;8:151. Abstract [6]. Tanguay P. Infantile autism and social communication spectrum disorder. J Am Acad Child Adolesc Psychiatry 1990;29:854. Abstract [7]. Mundy P, Sheinkopf S. Social behavior and the neurology of autism. Int Pediatr 1993;8:205. [8]. Filipek PA, Accardo PJ, Ashwal S, et al. Practice parameter: screening and diagnosis of autism: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology 2000;55:468. Full Text [9]. Stone WL, Caro-Martinez LM. Naturalistic observations of spontaneous communication in autistic children. J Autism Dev Disord 1990;20:437. Abstract [10]. Mundy P, Sigman M, Kasari C. A longitudinal study of joint attention and language development in autistic children. J Autism Dev Disord 1990;20:115. Abstract [11]. Hobson RP. Concerning knowledge of mental states. Br J Med Psychol 1990;63:199. Abstract [12]. Baron-Cohen S. The development of a theory of mind in autism: deviance and delay? Psychiatr Clin North Am 1991;14:33. Abstract [13]. Baron-Cohen S. Out of sight or out of mind? Another look at deception in autism. J Child Psychol Psychiatry 1992;33:1141. Abstract [14]. Calder AJ, Lawrence AD, Keane J, et al. Reading the mind from eye gaze. Neuropsychologia 2002;40:1129. Abstract [15]. Lord C, Volkmar F. Genetics of childhood disorders:XLII. Autism part 1: diagnosis and assessment in autistic spectrum disorders. J Am Acad Child Adolesc Psychiatry 2002;41:1134. Full Text [16]. Schopler E, Reichler R, Renner B. Childhood Autism Rating Scale (CARS). Los Angeles: Western Psychological Services; 1986. [17]. Stella J, Mundy P, Tuchman R. Social and nonsocial factors in the Childhood Autism Rating Scale. J Autism Dev Disord 1999;29:307. Abstract [18]. Lord C, Rutter M, Goode S, et al. Autism diagnostic observation schedule: a standarized observation of communicative and social behavior. J Autism Dev Disord 1989;19:185. Abstract [19]. LeCouteur A, Rutter M, Lord C, et al. Autism diagnostic interview: a standardized investigator-based instrument. J Auism Dev Disord 1989;19:363. [20]. Lord C, Pickles A, McLennan J, et al. Diagnosing autism: analyses of data from the Autism Diagnostic Interview. J Autism Dev Disord 1997;27:501. Abstract [21]. Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord 2000;30:205. Abstract [22]. Lord C, Leventhal BL, Cook Jr. EH. Quantifying the phenotype in autism spectrum disorders. Am J Med Genet 2001;105:36. Abstract [23]. Robertson JM, Tanguay PE, L'Ecuyer S, et al. Domains of social communication handicap in autism [1]. spectrum disorder. J Am Acad Child Adolesc Psychiatry 1999;38:738. Abstract [24]. Tuchman R, Jayakar P, Yaylali I, et al. Seizures and EEG findings in children with autism spectrum disorders. CNS Spectrums 1997;3:61. [25]. Gillberg C, Coleman M. The biology of the autistic syndromes, 3rd edition London: Mac Keith Press; 2000. [26]. Szatmari P, Tuff L, Finlayson MA, et al. Asperger's syndrome and autism: neurocognitive aspects. [see comments] J Am Acad Child Adolesc Psychiatry 1990;29:130. Abstract [27]. Liss M, Harel B, Fein D, et al. Predictors and correlates of adaptive functioning in children with developmental disorders. J Autism Dev Disord 2001;31:219. Abstract [28]. Szatmari P, Merette C, Bryson SE, et al. Quantifying dimensions in autism: a factor-analytic study. J Am Acad Child Adolesc Psychiatry 2002;41:467. Full Text [29]. Sigman M, Ungere JA, Mundy P, et al. Cognition in autistic children. In: CohenDJ, DonellanA, editors. Handbook of autism and pervasive developmental disorders New York: John Wiley; 1987. p. 103. [30]. Frith U, Baron-Cohen S. Perception in autistic children. In: CohenDJ, DonellanA, editors. Handbook of autism and pervasive developmental disorders New York: John Wiley; 1987. p. 85. [31]. Frith U, Morton J, Leslie AM. The cognitive basis of a biological disorder: autism. Trends Neurosci 1991;14:433. Abstract [32]. Serra M, Loth FL, van Geert PL, et al. Theory of mind in children with ‘lesser variants’ of autism: a longitudinal study. J Child Psychol Psychiatry 2002;43:885. Abstract [33]. Baron-Cohen S. Do people with autism understand what causes emotion? Child Dev 1991;62:385. Abstract [34]. Kurita H. Infantile autism with speech loss before the age of thirty months. J Am Acad Child Psychiatry 1985;24:191. Citation [35]. Tuchman RF, Rapin I, Shinnar S. Autistic and dysphasic childrenI: clinical characteristics. Pediatrics 1991;88:1211. Abstract [36]. Tuchman RF, Rapin I. Regression in pervasive developmental disorders: seizures and epileptiform electroencephalogram correlates. Pediatrics 1997;99:560. Abstract [37]. Shinnar S, Rapin I, Arnold S, et al. Language regression in childhood. Pediatr Neurol 2001;24:183. Abstract [38]. Osterling J, Dawson G. Early recognition of children with autism: a study of first birthday home videotapes. J Autism Dev Disord 1994;24:247. Abstract [39]. Osterling JA, Dawson G, Munson JA. Early recognition of 1-year-old infants with autism spectrum disorder versus mental retardation. Dev Psychopathol 2002;14:239. Abstract [40]. Burack JA, Volkmar FR. Development of low- and high-functioning autistic children. J Child Psychol Psychiatry 1992;33:607. Abstract [41]. Dawson G. What is Childhood Disintegrative Disorder, how is it different from autism, and what is believed to be its cause? J Autism Dev Disord 2000;30:177. Citation [42]. Tuchman R, Rapin I. Epilepsy in autism. Lancet Neurology 2001;1:352. [43]. Courchesne E, Townsend J, Saitoh O. The brain in infantile autism: posterior fossa structures are abnormal. [see comments] Neurology 1994;44:214. Abstract [44]. Herbert MR, Harris GJ, Adrien KT, et al. Abnormal asymmetry in language association cortex in autism. Ann Neurol 2002;52:588. Abstract [45]. Dawson G, Carver L, Meltzoff AN, et al. Neural correlates of face and object recognition in young children with autism spectrum disorder, developmental delay, and typical development. Child Dev 2002;73:700. Abstract [46]. Schultz RT, Gauthier I, Klin A, et al. Abnormal ventral temporal cortical activity during face discrimination among individuals with autism and Asperger syndrome. Arch Gen Psychiatry 2000;57:331. Abstract [47]. Grelotti DJ, Gauthier I, Schultz RT. Social interest and the development of cortical face specialization: what autism teaches us about face processing. Dev Psychobiol 2002;40:213. Abstract [48]. Adolphs R, Baron-Cohen S, Tranel D. Impaired recognition of social emotions following amygdala damage. J Cogn Neurosci 2002;14:1264. Abstract [49]. Bauman M, Kemper T. Neuroanatomic observations of the brain in autism. In: BaumanM, KemperT, editors. The neurobiology of autism Baltimore: John Hopkins University Press; 1994. p. 119. [50]. Schmahmann J. The cerebellum in autism: clinical and anatomic perspectives. In: BaumanM, KemperT, editors. The neurobiology of autism Baltimore: John Hopkins University Press; 1994. p. 195. [51]. Kemper TL, Bauman ML. Neuropathology of infantile autism. Mol Psychiatry 2002;7(Suppl 2):S12. Citation [52]. Bailey A, Luthert P, Dean A, et al. A clinicopathological study of autism. Brain 1998;121(Pt 5):889. Abstract [53]. Casanova MF, Buxhoeveden DP, Brown C. Clinical and macroscopic correlates of minicolumnar pathology in autism. J Child Neurol 2002;17:692. Abstract [54]. Casanova MF, Buxhoeveden DP, Switala AE, et al. Minicolumnar pathology in autism. Neurology 2002;58:428. Full Text [55]. Courchesne E, Yeung-Courchesne BA, Press GA, et al. Hypoplasia of cerebellar vermal lobules VI and VII in autism. N Engl J Med 1988;318:1349. Abstract [56]. Kleiman MD, Neff S, Rosman NP. The brain in infantile autism: are posterior fossa structures abnormal? Neurology 1992;42:753. Abstract [57]. Hashimoto T, Tayama M, Murakawa K, et al. Development of the brainstem and cerebellum in autistic patients. J Autism Dev Disord 1995;25:1. Abstract [58]. Holttum JR, Minshew NJ, Sanders RS, et al. Magnetic resonance imaging of the posterior fossa in autism. Biol Psychiatry 1992;32:1091. Abstract [59]. Courchesne E, Saitoh O, Yeung-Courchesne R, et al. Abnormality of cerebellar vermian lobules VI and VII in patients with infantile autism: identification of hypoplastic and hyperplastic subgroups with MR imaging. AJR Am J Roentgenol 1994;162:123. Abstract [60]. Courchesne E. New evidence of cerebellar and brainstem hypoplasia in autistic infants, children and adolescents: the MR imaging study by Hashimoto and colleagues. J Autism Dev Disord 1995;25:19. Citation [61]. Harris NS, Courchesne E, Townsend J, et al. Neuroanatomic contributions to slowed orienting of attention in children with autism. Brain Res Cogn Brain Res 1999;8:61. Abstract [62]. Mostofsky SH, Goldberg MC, Landa RJ, et al. Evidence for a deficit in procedural learning in children and adolescents with autism: implications for cerebellar contribution. J Int Neuropsychol Soc 2000;6:752. Abstract [63]. Piven J, Arndt S, Bailey J, et al. An MRI study of brain size in autism. Am J Psychiatry 1995;152:1145. Abstract [64]. Aylward EH, Minshew NJ, Goldstein G, et al. MRI volumes of amygdala and hippocampus in nonmentally retarded autistic adolescents and adults. Neurology 1999;53:2145. Full Text [65]. Abell F, Krams M, Ashburner J, et al. The neuroanatomy of autism: a voxel-based whole brain analysis of structural scans. Neuroreport 1999;10:1647. Abstract [66]. Sparks BF, Friedman SD, Shaw DW, et al. Brain structural abnormalities in young children with autism spectrum disorder. Neurology 2002;59:184. Full Text [67]. Courchesne E, Karns CM, Davis HR, et al. Unusual brain growth patterns in early life in patients with autistic disorder: an MRI study. Neurology 2001;57:245. Full Text [68]. Aylward EH, Minshew NJ, Field K, et al. Effects of age on brain volume and head circumference in autism. Neurology 2002;59:175. Full Text [69]. Courchesne E. Abnormal early brain development in autism. Mol Psychiatry 2002;7(Suppl 2):S21. Citation [70]. Baron-Cohen S, Ring HA, Wheelwright S, et al. Social intelligence in the normal and autistic brain: an fMRI study. Eur J Neurosci 1999;11:1891. Abstract [71]. Siegel Jr. B, Asarnow R, Tanguay P, et al. Regional cerebral glucose metabolism and attention in adults with a history of childhood autism. J Neuropsychiatry Clin Neurosci 1992;4:406. Abstract [72]. Muller RA, Behen ME, Rothermel RD, et al. Brain mapping of language and auditory perception in high-functioning autistic adults: a PET study. J Autism Dev Disord 1999;29:19. Abstract [73]. Happe F, Ehlers S, Fletcher P, et al. ‘Theory of mind’ in the brain. Evidence from a PET scan study of Asperger syndrome. Neuroreport 1996;8:197. Abstract [74]. Anderson GM. Genetics of childhood disorders: XLV. Autism, part 4: serotonin in autism. J Am Acad Child Adolesc Psychiatry 2002;41:1513. Full Text [75]. Cook Jr. E, Arora RC, Anderson GM, et al. Platelet serotonin studies in hyperserotonemic relatives of children with autistic disorder. Life Sci 1993;52:2005. Abstract [76]. Cook E. Autism: review of neurochemical investigation. Synapse 1990;6:292. Abstract [77]. Chugani DC, Muzik O, Rothermel R, et al. Altered serotonin synthesis in the dentatothalamocortical pathway in autistic boys. Ann Neurol 1997;42:666. Abstract [78]. Chugani DC, Muzik O, Behen M, et al. Developmental changes in brain serotonin synthesis capacity in autistic and nonautistic children. Ann Neurol 1999;45:287. Abstract [79]. Lewine JD, Andrews R, Chez M, et al. Magnetoencephalographic patterns of epileptiform activity in children with regressive autism spectrum disorders. Pediatrics 1999;104:405. Abstract [80]. Grillon C, Courchesne E, Akshoomoff N. Brainstem and middle latency auditory evoed potentials in autism and developmental language disorder. J Autism Dev Dis 1989;19:255. [81]. Maziade M, Merette C, Cayer M, et al. Prolongation of brainstem auditory-evoked responses in autistic probands and their unaffected relatives. Arch Gen Psychiatry 2000;57:1077. Abstract [82]. Nagy E, Loveland KA. Prolonged brainstem auditory evoked potentials: an autism-specific or autismnonspecific marker. Arch Gen Psychiatry 2002;59:288. Citation [83]. Coutinho MB, Rocha V, Santos MC. Auditory brainstem response in two children with autism. Int J Pediatr Otorhinolaryngol 2002;66:81. Abstract [84]. Klin A. Auditory brainstem responses in autism: brainstem dysfunction or peripheral hearing loss? J Autism Dev Disord 1993;23:15. Abstract [85]. Townsend J, Westerfield M, Leaver E, et al. Event-related brain response abnormalities in autism: evidence for impaired cerebello-frontal spatial attention networks. Brain Res Cogn Brain Res 2001;11:127. Abstract [86]. Ritvo ER, Jorde LB, Mason-Brothers A, et al. The UCLA-University of Utah epidemiologic survey of autism: recurrence risk estimates and genetic counseling. Am J Psychiatry 1989;146:1032. Abstract [87]. Szatmari P. Heterogeneity and the genetics of autism. [see comments] J Psychiatry Neurosci 1999;24:159. Abstract [88]. Geschwind DH, Sowinski J, Lord C, et al. The autism genetic resource exchange: a resource for the study of autism and related neuropsychiatric conditions. Am J Hum Genet 2001;69:463. Citation [89]. Liu J, Nyholt DR, Magnussen P, et al. A genomewide screen for autism susceptibility loci. Am J Hum Genet 2001;69:327. Abstract [90]. Lamb JA, Parr JR, Bailey AJ, et al. Autism: in search of susceptibility genes. Neuromolecular Med 2002;2:11. [91]. Shao Y, Raiford KL, Wolpert CM, et al. Phenotypic homogeneity provides increased support for linkage on chromosome 2 in autistic disorder. Am J Hum Genet 2002;70:1058. Abstract [92]. Borg I, Squire M, Menzel C, et al. A cryptic deletion of 2q35 including part of the PAX3 gene detected by breakpoint mapping in a child with autism and a de novo 2;8 translocation. J Med Genet 2002;39:391. Abstract [93]. Cook Jr. EH, Courchesne RY, Cox NJ, et al. Linkage-disequilibrium mapping of autistic disorder, with 15q11–13 markers. Am J Hum Genet 1998;62:1077. Abstract [94]. Fantes JA, Mewborn SK, Lese CM, et al. Organisation of the pericentromeric region of chromosome 15: at least four partial gene copies are amplified in patients with a proximal duplication of 15q. J Med Genet 2002;39:170. Abstract [95]. Sultana R, Yu CE, Yu J, et al. Identification of a novel gene on chromosome 7q11.2 interrupted by a translocation breakpoint in a pair of autistic twins. Genomics 2002;80:129. Abstract [96]. Auranen M, Vanhala R, Varilo T, et al. A genomewide screen for autism-spectrum disorders: evidence for a major susceptibility locus on chromosome 3q25–27. Am J Hum Genet 2002;71:777. Abstract Alarcon M, Cantor RM, Liu J, et al. Evidence for a language quantitative trait locus on chromosome 7q in multiplex autism families. Am J Hum Genet 2002;70:60. Abstract [98]. Beyer KS, Blasi F, Bacchelli E, et al. Mutation analysis of the coding sequence of the MECP2 gene in infantile autism. Hum Genet 2002;111:305. Abstract [99]. Andres C. Molecular genetics and animal models in autistic disorder. Brain Res Bull 2002;57:109. Abstract [100]. Krebs MO, Betancur C, Leroy S, et al. Absence of association between a polymorphic GGC repeat in the 5′ untranslated region of the reelin gene and autism. Mol Psychiatry 2002;7:801. Abstract [101]. Li J, Tabor HK, Nguyen L, et al. Lack of association between HoxA1 and HoxB1 gene variants and autism in 110 multiplex families. Am J Med Genet 2002;114:24. Abstract [102]. Fatemi SH, Stary JM, Egan EA. Reduced blood levels of reelin as a vulnerability factor in pathophysiology of autistic disorder. Cell Mol Neurobiol 2002;22:139. Abstract [103]. Zhang H, Liu X, Zhang C, et al. Reelin gene alleles and susceptibility to autism spectrum disorders. Mol Psychiatry 2002;7:1012. Abstract [104]. Talebizadeh Z, Bittel DC, Miles JH, et al. No association between HOXA1 and HOXB1 genes and autism spectrum disorders (ASD). J Med Genet 2002;39:e70. Citation [105]. Klin A, Jones W, Schultz R, et al. Defining and quantifying the social phenotype in autism. Am J Psychiatry 2002;159:895. Abstract [106]. Grady CL, Keightley ML. Studies of altered social cognition in neuropsychiatric disorders using functional neuroimaging. Can J Psychiatry 2002;47:327. Abstract [107]. Koegel RI, Frea WD. Treatment of social behavior in autism through the modification of pivotal social skills. J Appl Behav Anal 1993;26:369. Abstract [108]. McEachin JJ, Smith T, Lovaas OI. Long-term outcome for children with autism who received early intensive behavioral treatment. Am J Ment Retard 1993;97:359. Abstract [109]. Ozonoff S, Cathcart K. Effectiveness of a home program intervention for young children with autism. J Autism Dev Disord 1998;28:25. Abstract [110]. Koegel RL, Koegel LK, McNerney EK. Pivotal areas in intervention for autism. J Clin Child Psychol 2001;30:19. Abstract [111]. Anderson GM, Gutknecht L, Cohen DJ, et al. Serotonin transporter promoter variants in autism: functional effects and relationship to platelet hyperserotonemia. Mol Psychiatry 2002;7:831. Abstract [112]. DeLong GR, Teague LA, McSwain Kamran M. Effects of fluoxetine treatment in young children with idiopathic autism. Dev Med Child Neurol 1998;40:551. Abstract [113]. DeLong GR, Ritch CR, Burch S. Fluoxetine response in children with autistic spectrum disorders: correlation with familial major affective disorder and intellectual achievement. Dev Med Child Neurol 2002;44:652. Abstract [114]. McCracken JT, McGough J, Shah B, et al. Risperidone in children with autism and serious behavioral problems. N Engl J Med 2002;347:314. Abstract [115]. Tuchman R. Treatment of seizure disorders and EEG abnormalities in children with autism spectrum disorders. J Autism Dev Disord 2000;30:485. Abstract [116]. Di Martino A, Tuchman RF. Antiepileptic drugs: affective use in autism spectrum disorders. Pediatr Neurol 2001;25:199. Abstract [117]. Lipkin WI. Banbury Center of Cold Spring Harbor meeting on microbiology, immunology and toxicology of autism and other neurodevelopmental disorders February 11–14, 2001. Mol Psychiatry 2002;7(Suppl 2):S1. [118]. Krause I, He XS, Gershwin ME, et al. Brief report: immune factors in autism: a critical review. J Autism Dev Disord 2002;32:337. Abstract [119]. Wakefield AJ, Puleston JM, Montgomery SM, et al. Review article: the concept of entero-colonic encephalopathy, autism and opioid receptor ligands. Aliment Pharmacol Ther 2002;16:663. Abstract [120]. Scifo R, Cioni M, Nicolosi A, et al. Opioid-immune interactions in autism: behavioural and immunological assessment during a double-blind treatment with naltrexone. Ann Ist Super Sanita 1996;32:351. Abstract [97]. Gupta S. Immunological treatments for autism. J Autism Dev Disord 2000;30:475. Abstract Sandman CA, Touchette P, Marion S, et al. Disregulation of proopiomelanocortin and contagious maladaptive behavior. Regul Pept 2002;108:179. Abstract [123]. Garvey J. Diet in autism and associated disorders. J Fam Health Care 2002;12:34. [124]. Matarazzo EB. Treatment of late onset autism as a consequence of probable autommune processes related to chronic bacterial infection. World J Biol Psychiatry 2002;3:162. [125]. Willemsen-Swinkels SH, Buitelaar JK, van Engeland H. The effects of chronic naltrexone treatment in young autistic children: a double-blind placebo-controlled crossover study. Biol Psychiatry 1996;39:1023. Abstract [126]. Buitelaar JK, Willemsen-Swinkels S, Van Engeland H. Naltrexone in children with autism. J Am Acad Child Adolesc Psychiatry 1998;37:800. Citation [127]. Willemsen-Swinkels SH, Buitelaar JK, van Berckelaer-Onnes IA, et al. Brief report: six months continuation treatment in naltrexone-responsive children with autism: an open-label case-control design. J Autism Dev Disord 1999;29:167. Citation [128]. Zimmerman AW. Commentary: immunological treatments for autism: in search of reasons for promising approaches. J Autism Dev Disord 2000;30:481. Citation [129]. Gilman JT, Tuchman RF. Autism and associated behavioral disorders: pharmacotherapeutic intervention. Ann Pharmacother 1995;29:47. Abstract [130]. Tsai LY. Psychopharmacology in autism. Psychosom Med 1999;61:651. Abstract [131]. Aman MG, Langworthy KS. Pharmacotherapy for hyperactivity in children with autism and other pervasive developmental disorders. J Autism Dev Disord 2000;30:451. Abstract [132]. Santosh PJ, Baird G. Pharmacotherapy of target symptoms in autistic spectrum disorders. Indian J Pediatr 2001;68:427. Abstract [133]. Rogers SJ. Interventions that facilitate socialization in children with autism. J Autism Dev Disord 2000;30:399. Abstract [134]. Koegel LK. Interventions to facilitate communication in autism. J Autism Dev Disord 2000;30:383. Abstract [135]. McConnell SR. Interventions to facilitate social interaction for young children with autism: review of available research and recommendations for educational intervention and future research. J Autism Dev Disord 2002;32:351. Abstract [136]. Goldstein H. Communication intervention for children with autism: a review of treatment efficacy. J Autism Dev Disord 2002;32:373. Abstract [137]. Howlin P. Prognosis in autism: do specialist treatments affect long-term outcome? Eur Child Adolesc Psychiatry 1997;6:55. Abstract [138]. Kasari C. Assessing change in early intervention programs for children with autism. J Autism Dev Disord 2002;32:447. Abstract [139]. Wolery M, Garfinkle AN. Measures in intervention research with young children who have autism. J Autism Dev Disord 2002;32:463. Abstract [140]. Eisenberg L. Experience, brain, and behavior: the importance of a head start. Pediatrics 1999;103:1031. Abstract [121]. [122].