PULMONARY TUBERCULOSIS
advertisement

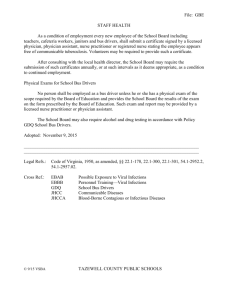
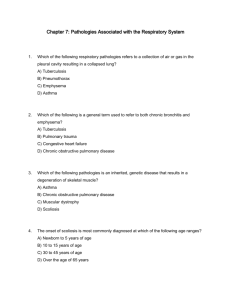
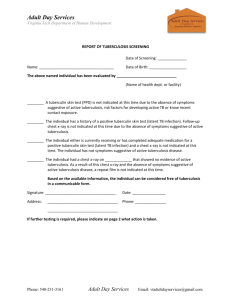
PULMONARY TUBERCULOSIS General Considerations: Tuberculosis is a chronic infection ,potantially of lifelong duration,caused by two species of mycobacteria M.tuberculosis and, rarely, M.bovis. Which causes nodular, caseating granuloms called tubercles that fibrose,ulcerate or calcify. The disease is confined to the lungs in most patients but may spread to almost any part of the body. Etiology: The tubercle bacillus (M.Tuberculosis) is aerobic, non-motile,non-spore-forming, high in lipid content, and acid and alcohol-fast. It grows slowly and differs form other mycobacteria by its ability to produce niacin. Pathogenesis: Tuberculosis is transmitted by airborne droplet nuclei (containing tubercle bacilli) Many droplet nuclei are capable of floating in the immediate environment for several hours. Large particles may be inhaled by a person breathing the same air and impact on the trachea or wall of the upper airway As the bacilli multiply, they spread through lymphatic channels to regional lymph nodes, and through the blood stream to the rest of the body Immunity and Tuberculin Hypersensitivity: The bacilli within 4 to 8 weeks after infection cellular immunity develop, so that the macrophages are "activated" and are capable of not only phagocytizing but also killing tbe organisms. Coincident with tfae development of cellular immunity, the delayed type of skin hypersensitivity to tuberculoprotein can be demonstrated. The Tuberculin Test The tuberculin test is best performed by intracutaneous injection of 0.1 ml 1:2000 of old tuberculin. Old tuberculin (OT) is now the standard substance used in intradermal testing. The classic test is carried out by the intradermal injection of 0.1ml of (OT) containing 5 tuberculin units (OT) and then measuring the diameter of induration produced 48 to 72 horns later. A reaction of less than 5 mm is considered negative, 5-9 mm is considered positive (+); 10-19 mm is considered positive (++); and more than 20 mm is considered positive (+++). A positive tuberculin skin test indicates tuberculous infection, with or without disease. Common Clinical Patterns 1.Primary tuberculosis (Primary Complex and Bronchial Lymphnod_Tbuerculosis). 2.Milliary Tuberculosis (acute, subacute and chronic hematogenous pulmonary tuberculosis) 3.Secondary pulmonary tuberculosis:including infiltrative pulmonary tuberculosis. and chronic fibrocavenous pulmonary tuberculosis.. 4.Tubercolous pleuritis. 5.Extrapulmonary tuberculosis Clinical Manifestations Most patients present as cases of pulmonary tuberculosis with fever, asthma. cough, weight loss, anorexia, fatigue, night sweats wasting, and pulmonary hemorrhage. Weight loss and fatigue are more likely to lead to medical attention than is fever usually in the afternoon, which is often unrecognized. Cough may vary from mild to severe, and sputum may be scant and mucoid or copious and purulent. Hemoptysis may be due to cough of a caseous lesion or bronchial ulceration. Particularly in late chronic disease, bleeding may be copious and sudden owing to rupture of an artery within the fibrous walls of a cavity. Radiology The following characteristics of a chest radiograph favour the diagnosis of tuberculosis: (1). shadows mainly in the upper zone; (2).patchy or nodular shadows; (3).the presence of a cavity or cavities, although these, of course, can also occur in lung abscess, carcinoma, etc; (4).the presence of calcification, although a carcinoma or pneumonia may occur in an areas of the lung where there is calcification due to tuberculosis; (5).bilateral shadows, especially if these are in the upper zones; (6).the persistence of the abnormal shadows without alteration in an x-ray repeated after several weeks; this helps to exclude a diagnosis of pneumonia or other acute infection. The X-ray features of Secondary pulmonary tuberculosis Diagnosis A patient with tuberculous pulmonary disease will come to the physician for one of three reasons: (1). Suggestive symptoms; (2).a positive finding on routine tuberculin testing; (3).a suspicious routine chest roentgenogram. The following need to be considered: (1). Sputum examination There are direct smear and culture. Direct smear examination is only positive when large numbers of bacilli begin to be excreted, so that a negative smear by no means excludes tuberculosis. A negative smear in the presence of extensive disease and cavitation makes the diagnosis less likely, particularly if the negatives are frequently repeated. (2). Tuberculin testing: A positive tuberculin test although it is of great use in children, has limited diagnostic significance in older age groups. Tuberculin Test The tuberculin test in complished with old tuberculin (OT) and purified protein derivative (PPD) of tuberculin that is a crude culture filtrate of M.tuberculosis. OT and PPD dilute 0. 1 ml (unit and content) (3). White blood count The white blood count is usually normal. In practice the white blood count is only useful in a minority of cases. When the patient is less ill and the radiological shadowing less extensive the count is Often normal or high normal. Besides these routine investigations the history is sometimes of value. Differential Diagnosis: Although tuberculosis may be confused with virtually any intrathoracic condition, certain diseases are frequently considered in differential diagnosis. (1). bronchiectasis may present with symptoms sugesting tuberculosis. And bronchiectatic and emphysematous areas surrounded by infiltrate may mimic cavitation roentgenographically. (2). Cavitary lung abscess often involves the dorsal segments of the lower lobes and posterior segments of the upper lobes. Typically lung abscess causes little in the way of physical findings, may have a fluid level, and is not associated with patchy bronchogenic infiltrates, in contrast, physical findings are prominent over tuberculous cavities, fluid levels are rare. and patchy infiltrates elsewhere are the rule. (3).Acute bacterial pneumonias may resemble florid tuberculosis in all particularsexcept for the sputum examination and response to antimicrobial drugs. (4). Neoplasm may resemble tuberculosis, as in an isolated coin lesion. An obstructing and inconspicuous endobronchial tumor causing distal chronic inflammation or a caviting neoplastic mass. (An irregular cavity wall suggests necorotic neoplasm.) Treatment Non-compliance of patients on chemotherapy is the most difficult problem in TB control. The critical issue in TB control is adopting the DOTS (directly observed short-term therapy) .strategy recommended by the WHO TB Programme. Chemotherapeutic Agents.The principles of antituberculous chemotherapy involve earlier,combination, appropriate drugs and durations. Isoniazid. streptomycin, rifampin and pyrazinamide kill organisms, ethambutal and para-amino-salicylic acid restraint organisms. Isoniazid (INH) Isoniazia is a principal agent used to treat tuberculosis. It is universally accepted for initial treatment. Rifampin (RFP) This is the newest drug effective against tuberculosis. Like isoniazid it is bacterieidal and highly effective, unlike isoniazid, it is also effective against most other mycobacteria as well as other organisms. Streptomycin (SM) This was the first trully effective drug for the treatment of tuberculosis. It is administered only parenterally. Pyrazinamide (PZA) Pyrazmamide is a major oral agent used against mycobacteria but can produce gastro intestinal and liver toxicity. Regimens of chemotherapy Because of concern over the rising prevalence of drug resistance, recent CDC recommendations advocate a four-drug regimen for most cases of known or suspected tuberculosis. INH and RFP are the central agent of any regimen based on their superior bactericidal activity and low toxicity. PZA has special utility in promoting rapid, early reduction in bacillary burden; in drug-susceptible cases. PZA need be given only for the initial 2 months to produce this effect. EMB is useful primarily to protect against the emergence of drug resistance in cases with unknown initial susceptibility patterns and large mycobacterial burdens; EMB may be terminated if susceptibility is reported or be continued throughout the duration of treatment if resistance is noted. Streptomycin(SM), parenteral agent, has found a diminishing role in modem therapy due to problems with regularly administering intramuscular injections; however, for patients with very extensive tuberculosis, SM may accelerate initial bactericidal activity. routine chemotherapy. Based on the character of the disease, the following drug regimens are recommended for initiation of therapy. INH+SM+PAS 12-lSmonth. but the regimen is too long. Patients are unlikely to comply with treatement. hi actfel practice, me shoH-tenn chemotherapy is asually adopted- The therapeutic effect of the short-term chemotherapy is as well as the routine chemotherapy. Short-term chemotherapy Two or three drugs killing oforganisms+one drug restraint of organisms. For example: INH+RfP+SM(EMBXPZA) 2M / INH+RFP 4-7M in usual mild or Moderate disease with small infiltrates and thin wall cavities. INH*RfP+SM+EMB(PZA) 2M / INH+RfP 4-7M in extensive and severe Disease, particularly when large areas of caseation or thick-waited cavities are identified. To initial patients : we can select short-term chemotherapy 2HRZS(E)/4HR, the duration lasts 6 months. To retreatment patients:3HRZSE/5HRZ , the duration lasts 6-12 months. To MDR-TB: MDR-TB means that resistant to both INH and rifampin. We can select five kinds of antitubercule drugs in the stage of extensive .these drugs include aminoglycosides(amikacin, kanamycin, capremycin), cycloserine, EMB, quinolones(levofloxacin, ofloxacin), PZA, ethionamide. In the stage of consecutive, we can select three kinds of drugs,including ethionamide, quinolones and EMB.The whole therapy lasts at least 18 months. Retreatment of Tuberculosis Surgical Intervention Surgery was thought to be a valuable adjunct to treatment. Prevention of Tuberculsis Vaccination BCG(bacille. Calmette Guerin) is a strain ofM.bovis with aaemuated virulence for man. BCG Vaccination can obtain immunity acquired for tubercle bacillus, therefore.is one of the most important tuberculosis prevention. Vaccination target: infants children and youngster of tuberculin negative (vaccination is of course, of no use in tuberculin-positive persons).