Abstracts
advertisement

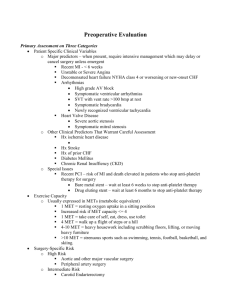
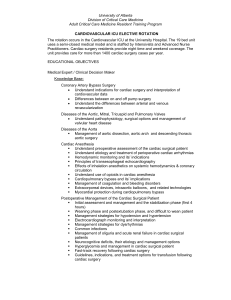
Abstracts submitted to ACTA Cambridge 20 June 2003 1 of 12 Tracheostomy practice on a cardiothoracic intensive care unit Briggs S, Ambler J, Smith D. Department of Anaesthesia, Southampton General Hospital, Tremona Road, Southampton, SO16 6YD, UK. Introduction: Tracheostomies are frequently formed in intensive care patients. The perceived benefits are reduction in work of breathing, reduction in sedation, and increase in communication. It is a maximally invasive procedure, and the consequences of error can be rapidly life threatening. Similarly, day-to-day usage, although usually straightforward, can become complicated, with disastrous consequences [1]. We examine a series of one hundred tracheostomies formed in patients on the cardiothoracic intensive care unit, to assess current practice, complication rates, and identify areas of clinical practice that could be improved. Methods: We selected the most recent series of one hundred tracheostomies that were formed in patients on the unit, and reviewed the case notes retrospectively. We looked at reasons why tracheostomies are formed, the time course of events, the seniority of clinicians performing the procedures, procedure details, and occurrence of complications until the tracheostomy was either removed or the patient died. Results: A total of 95 patients each had one tracheostomy formed, whilst one patient had the tracheostomy formed twice, and one patient had the tracheostomy formed three times. Six sets of notes were entirely missing whilst nine sets were partially missing. The median time from endotracheal intubation to tracheostomy formation was 5 days (25th percentile 4 days, 75th percentile 8 days), and median period between insertion and decannulation was 20 days (25 th percentile 12 days, 75th percentile 25 days). The most common reason for insertion was anticipated long wean (55% (52/94)), followed by insertion after failed extubation (32% (30/94)). Registrars are the most frequent operators (66% (62/94). Percutaneous dilatational techniques were used for 89% (64/72) of tracheostomy formations, whilst surgical techniques were used for 8% (6/72). The Ciaglia method was used for percutaneous dilatational trachesotomy formation. A bronchoscope was used to aid placement of the percutaneous tracheostomy on 94% (63/67) of occasions, whilst direct laryngoscopy was used alone, on 6% (4/67) of occasions. Upon decannulation, tracheostomy tubes were replaced with ‘Minitrach tubes’ on 35% (33/94) of occasions. The most common complication was either complete or partial obstruction of the tracheostomy tube (24% (23/94)) requiring either removal alone, or removal and replacement. Infection of the tracheostomy site occurred in 18% (17/94). Conclusion: The percutaneous dilatational technique of tracheostomy formation is used predominantly on our unit. The most common complications are tracheostomy obstruction and site infection. A significant number of cases have a ‘Minitrach tubes’ inserted following decannulation. In order to improve clinical practice, documentation of the insertion procedure and complications both on the ICU and ward must be improved. Reference: Grover ER, Bihari DJ: The role of tracheostomy in the adult intensive care unit. Postgrad Med J 1992, 68(799): 313-7. Abstracts submitted to ACTA Cambridge 20 June 2003 2 of 12 Transoesophageal echocardiography aided endovascular stent-graft repair of a ruptured aortic aneurysm S T Clinton, SS Shah, S McPherson, H McKeague General Infirmary at Leeds, Great George Street, Leeds, LS1 3EX Introduction Endovascular aortic repair of thoracic aortic pathology is less invasive and potentially safer than open surgery. Transoesophageal echocardiography (TOE) provides excellent views of the distal aortic arch, descending thoracic aorta and can aid stent deployment. We report the use of TOE in the endovascular repair of a ruptured aortic aneurysm presenting as an aortic-bronchial fistula. Case report A 68-year-old lady presented to the emergency department with massive haemoptysis and cardiovascular collapse. She had been recently diagnosed as having an aneurysm of the distal arch and proximal descending thoracic aorta. This was believed to have occurred at the site of a previous transection following significant thoracic trauma 12 years earlier. Her past medical history included controlled hypertension, poor respiratory function, smoking and morbid obesity. Following emergency intubation, ventilation and CT scanning, she was transferred to theatre where endovascular stenting was performed. TOE was invaluable in localizing the aneurysm, monitoring haemodynamics, and confirming successful stent placement excluding flow within the sac. Discussion As thoracic endovascular procedures become more commonplace, the utility of TOE will become more apparent. TOE provides instantaneous views, which aid identification of aortic pathology, estimates endograft sizing, guide stent deployment and confirm exclusion of the aneurysmal sac. It has been shown to be superior to perioperative angiography both in diagnosing endograft leakage (sensitivity and specificity of 100 %) and diagnosing iatrogenic dissections [1]. References 1. Kahn RA, Moskowitz DM: Endovascular aortic repair. J Cardiothorac Vasc Anesth 16:218-233, 2002 Abstracts submitted to ACTA Cambridge 20 June 2003 3 of 12 Optimising Blood Conservation In Cardiac Surgery – A Randomised Double Blind Placebo Controlled Trial Of Two Anti-Fibrinolytics Used In Addition To Intra-Operative Cell Salvage Diprose P, Herbertson M, Deakin CD, O’Shaughnessy D¶, Gill R Departments of Anaesthesia and Haematology¶, Southampton University Hospitals NHS Trust, Tremona Road, Southampton, SO16 6YD, UK Cardiac surgery utilises a large proportion of blood and blood products. The reasons for this are multi-factorial and include pre-operative anti-platelet therapy, cardiopulmonary bypass effects and the extent of surgery. Previous work has confirmed that intra-operative cell salvage (ICS) was the most effective mechanical method of reducing exposure to blood and blood products.1 Our aim was to ascertain the optimal combined mechanical and pharmacological methods of blood conservation in cardiac surgery. Following institutional ethics approval, patients were approached for inclusion into the study if they presented for first time coronary artery surgery or first time single valve repair/replacement. Patients were included if they were taking aspirin but excluded if on any other anti-platelet therapy. Once informed consent had been obtained, patients were randomised to receive either aprotinin with the standard ‘Hammersmith’ regime (APR group), 5g Tranexamic acid with equivalent volumes of normal saline (TXA group), or, equivalent volumes of normal saline as a placebo group (PLA group). All drugs were prepared and blinded by independent practitioners within the hospital’s pharmacy technical services unit. All patient groups received intra-operative cell salvage with a standardised protocol. The trigger for blood transfusion was a haemoglobin of less than 85g/l post-op. Blood product transfusion was guided by a protocol largely based on previous work by Shore-Lesserson et al.2 Primary outcome measures were exposure to blood or blood products. Secondary outcomes were mediastinal drainage and cardiac indicators of myocardial infarction. A total of 186 patients were randomised, 180 (60 in each group) of which received the full treatment regime and were studied. There were no significant differences between groups in terms of age, Parsonnet score, aspirin usage, procedure performed, cardiopulmonary bypass or cross clamp times. Exposure to any blood or blood products was significantly less between anti-fibrinolytic groups and placebo and between aprotinin and tranexamic acid (proportions given any transfusion : APR 15%, TXA 35%, PLA 60%). Mediastinal drainage was significantly less in the APR group as compared to either TXA or PLA. There was no statistically significant difference between groups for the number of patients that required reopening (number re-opened APR=2, TXA=5, PLA=7). No difference was shown between groups for indicators of myocardial infarction. Aprotinin in the dosing regime tested is more efficacious than both placebo and 5g of tranexamic acid in reducing exposure to blood and blood products following first-time cardiac surgery. References 1. McGill N, O'Shaughnessy D, Pickering R, Herbertson M, Gill R. Mechanical methods of reducing blood transfusion in cardiac surgery: randomised controlled trial. BMJ 2002; 324: 1299. 2. Shore-Lesserson L, Manspeizer HE, DePerio M, Francis S, Vela-Cantos F, Ergin MA. Thromboelastography-guided transfusion algorithm reduces transfusions in complex cardiac surgery. Anesth Analg. 1999; 88: 312-9 Abstracts submitted to ACTA Cambridge 20 June 2003 4 of 12 The presence of a radiological gastric gas shadow and nausea and vomiting after cardiac surgery V Gaur, A Gaur, JLC Swanevelder, RR Govindaswami, U Singh Department of Cardiology, Department of Anaesthesia and Critical Care, Glenfield Hospital, University Hospitals of Leicester. Department of Bio-statistic, Sanjay Ghandi Postgraduate Institute of Medical Sciences, Lucknow, India. Introduction: The incidence of postoperative nausea and vomiting (PONV) after cardiac surgery is around 45% reaching 70% in female population. Numerous factors have been implicated including patient weight, use of nitrous oxide and experience of anaesthetist. [1, 2] In this prospective audit we investigated the presence of gas in the stomach on chest X-ray and its correlation with PONV after cardiac surgery. Methods: We looked for the presence of gas in the stomach on chest X-ray in 27 consecutive patients listed for cardiac surgery. A routine chest X-ray was performed for two consecutive days in all the patients and the investigators did not influence its frequency or timing. Type of surgery, age, gender, preoperative gastric disorders, size of gas shadow on chest X-ray and presence of nausea and vomiting was documented. Chest X-rays were interpreted preoperatively, postoperatively with the endotracheal tube in situ, after extubation of the trachea on day one, and on postoperative day two. The Chi-squared Fisher’s Exact Test was performed to determine any significance of a gas shadow in the stomach on PONV. The relative risk was also calculated. Results: One patient was ventilated for several days and was excluded from the study leaving 26 subjects. The average age was 64.64 + 14 and 70 % were male. A gas shadow was present on preoperative chest X-ray in 15 patients, however, only one had gastric symptoms (indigestion). After tracheal extubation on postoperative day one, chests X-rays demonstrated a gas shadow present in 9 of the 26 patients and 8 of them complained of PONV. Of the remaining 17 patients without gas shadow only 3 complained of PONV. The relationship between a gas shadow on chest X-ray and PONV on postoperative day one was therefore very significant (p value=0.0008) with the relative risk of 4.94 (95% confidence interval 1.76-14.50). This correlation could not be demonstrated on postoperative day 2. Conclusion: Presence of a gas shadow on the postoperative chest X-ray after cardiac surgery has a significant correlation with PONV. This could be due to various reasons e.g. residual effect of anaesthetic, opioid analgesics, etc. The risk of PONV is higher in obese or female patients. The prophylactic use of an antiemetic drug or nasogastric tube to decompress the stomach may therefore be indicated. A prospective randomised trial is planned to investigate this observation further. References 1. Pollard BJ, Elliott RA, Moore EW. Eur J Anaesthesiol 2003 Jan;20(1):1-92. 2. Hovorka J, Korttila K, Erkola O. Acta Anaesthesiol Scand 1990 Apr;34(3):203-5 Abstracts submitted to ACTA Cambridge 20 June 2003 5 of 12 Brain Metabolism Following Hypothermic Circulatory Arrest: To Perfuse Or Not Perfuse? D Harrington, T Clutton-Brock, D Green, P Hutton, JP Lilley, D Riddington, P Townsend, D Turfrey, M Wilkes, M Faroqui. Cardiothoracic Unit, Queen Elizabeth Hospital, Birmingham, UK. Objective. Hypothermic circulatory arrest (HCA) is associated with a cerebral metabolic deficit manifest by increased cerebral oxygen extraction as measured by jugular bulb hypoxaemia. We hypothesised that cold selective antegrade cerebral perfusion (SACP) with moderate corporeal hypothermia, would attenuate this phenomenon. Methods. In a prospective, randomised trial, HCA for arch reconstruction occurred at a nasopharyngeal temperature of 15ºC. SACP occurred at a nasopharyngeal temperature of 25ºC with a cerebral perfusate of 15ºC. Paired arterial and jugular venous samples were taken pre and post arrest. Middle cerebral artery velocity (MCAV) was measured by transcranial Doppler. Analysis was performed using Mann Whitney U tests. Results. There were 22 HCA and 20 SACP patients. There were 3 deaths (7.1%) and 2 strokes (4.8%). The mean HCA time was 33min (SD 19.4) and the mean SACP + HCA time was 47 min (SD 17.7) (p=0.003). Mean cardiopulmonary bypass times were similar, (221min (63.7) and 203min (41.8) p=0.554). The groups were comparable in terms of pre arrest haematocrit. From pre to post arrest, jugular bulb pO2 changed by -21.67mmHg (26.4) in the HCA group versus +2.27mmHg (18.8) in the SACP group (p=0.007). Oxygen extraction changed by +1.7ml/dl (1.3) in the HCA group versus -1ml/dl (2.4) in the SACP group (p<0.001). MCAV increased by 6.25cm/s (9.1) in the HCA group and 19.2cm/s (10.1) in the SACP group (p=0.001). Conclusion. This data demonstrates that selective antegrade cerebral perfusion during aortic arch surgery attenuates the metabolic deficit seen following hypothermic circulatory arrest. Abstracts submitted to ACTA Cambridge 20 June 2003 6 of 12 Evolving anaesthetic and perfusion techniques for thoraco-abdominal aortic aneurysm repair Karim A, Kalkat M, Faroqui M, Lilley J, Townsend P, Green D, Wilkes M, Riddington D, Turfrey D, Srinivas L, Clutton-Brock T, Jackson P, Bonser RS. Cardiothoracic Anaesthesia & Surgery, University Hospital Birmingham NHS Trust Thoraco-abdominal aneurysm(TAAA) repairs have significant risks of mortality and paraplegia which may be attenuated by some adjunctive techniques. Most outcome reports are derived from large aortic programmes and there have been few reports of UK practice. Between April 1994-March 2002 we undertook 52 primary repairs of TAAAs. Degenerative 26, chronic dissection 15, Marfan’s dissection 9, acute type B dissection 1, giant cell arteritis 1. Acute presentation was present in 37/52 (rupture 14, pain 22, bronchus compression 1). We report the progression of our anaesthetic/perfusion technique and outcomes. 100 90 80 70 60 % 50 40 30 20 10 0 HCA Cell saver CSF drain 1994-97 1998-99 2000-01 2002- Extent Number Mortality Paraplegia No. Ruptured Mortality ruptured Total 52 5 (10%) 1 (2%) 15 3 (20%) I & II 48 4 (8.3%) 1 (2.2%) 13 2 (15.4%) III & IV 4 1 (25%) 0 2 1 (50%) No. non ruptured Mortality non ruptured 37 2 (6%) 35 2 (6%) 2 0 There has been an evolution of practice to use profound hypothermia, cell salvage and CSF drainage for complex TAAA repair. Satisfactory outcomes can be achieved in smaller volume centres with a multi-disciplinary approach to management. Abstracts submitted to ACTA Cambridge 20 June 2003 7 of 12 Evaluation of a long radial artery catheter for the PiCCO system R.M.L’E. Orme, D.W. Pigott Nuffield Department of Anaesthetics, John Radcliffe Hospital, Oxford, UK. Introduction It has been shown that there is close agreement between cardiac output as determined by pulmonary artery thermodilution (PACO), aortic transpulmonary thermodilution (TPCO) and pulse contour analysis (PCCO) [1] using the PiCCO system (Pulsion Medical Systems, Munich, Germany). The use of a long radial catheter to measure aortic pressure was described as early as 1974 [2], prompting the development of a 4Fr 50 cm catheter for the PiCCO system. We have compared the accuracy of this catheter to a pulmonary artery catheter (TruCCOMs®, Aortech Critical Care, Bellshill, UK) and investigated whether the use of a shorter catheter might be possible. Methods We studied 22 patients undergoing coronary artery surgery. Measurements were made post-operatively. TPCO was determined using 20ml of iced injectate. PCCO was then recorded. Simultaneously, PACO was determined using 10ml of room temperature injectate. After 3 measurements, the catheter was withdrawn by 5cm and the measurements repeated. Further withdrawals were made until TPCO was unrecordable. Statistical analysis was by the method of Bland and Altman. There were no complications related to the radial catheter. Catheter Length 50 cm 45 cm 40 cm 35 cm 30 cm TPCO vs. PACO Bias (precision) l.min-1 0.38 (0.77) 0.45 (1.18) 0.64 (1.37) 1.03 (1.30) 1.29 (1.56) PCCO vs. PACO Bias (precision) l.min-1 0.39 (0.76) 0.41 (1.10) 0.55 (1.34) 0.92 (1.17) 1.23 (1.22) No. of Measurements 54 54 51 36 27 Results Data is presented for 18 patients. Bias and precision for PCCO and TPCO versus PACO are shown in the table. TPCO and thus PCCO could be measured in all patients after a single 5cm pullback, but could only be recorded in 17 patients at 10 cm pullback, and 9 patients at 20cm pullback. Conclusions Our results show bias and precision comparable to previous studies [1]. This catheter may have considerable practical advantages over a femoral catheter and ensures that central arterial pressure will be used for reliable blood pressure monitoring. The use of a shorter catheter appears impossible since TPCO cannot be determined to calibrate the PiCCO system. References 1. Zollner C, Haller M, Weis M et al. Beat-to-beat measurement of cardiac output by intravascular pulse contour analysis. J Cardiothorac Vasc Anesth 2000; 14: 125-129 2. Gardner RM, Schwartz RN, Wong HC, Burke JP. Percutaneous indwelling radial artery catheters for monitoring cardiovascular function. N Engl J Med 1974; 290: 1227-31 Abstracts submitted to ACTA Cambridge 20 June 2003 8 of 12 Metabolic Substrate Support during Coronary Artery Bypass Surgery The MESSAGE trial D Quinn & MESSAGE trialists. Queen Elizabeth Hospital, Birmingham Background Post-ischaemic myocardial dysfunction following coronary artery bypass grafting (CABG) may be ameliorated by systemic glucose-insulin-potassium (GIK) therapy. GIK may favourably alter the balance of intracellular myocardial metabolism during ischaemia/reperfusion and promote adequate haemodynamic conditions in the early post-operative period. Objectives To determine the effects of GIK therapy on myocardial protection and function in non-diabetic patients undergoing first-time elective/urgent CABG utilising cardiopulmonary bypass (CPB), moderate hypothermia and antegrade intermittent cold blood cardioplegia Methods A prospective randomised double-blind placebo-controlled trial of peri-operative high-dose central intravenous GIK therapy from sternotomy to 6 hours following release of the aortic cross clamp was conducted in 280 patients (GIK n=139, dextrose 5% n= 141) using standardised protocols for anaesthesia, surgery, CPB, myocardial protection, blood glucose management and inotropic and vasoconstrictor support. Haemodynamic function was monitored using sequential pulmonary artery flotation balloon catheter measurements. Serial sampling of blood glucose, potassium and cardiac troponin I was performed from baseline in all patients. Low cardiac output state (LCOS) incidence was assessed by an independent committee. A standard battery of neuropsychometric tests were administered at baseline, 5-7 days and 8 weeks after surgery in 68 patients. Statistical analysis was performed using repeated measures for sequential data and 2 analysis of dichotomous variables. Results Groups were comparable for all pre- and intra-operative variables. There were 5 deaths (GIK n=3) and no difference in treated infection episodes (GIK 27%, control 22%), post-operative focal neurological (GIK 1.4%, control 3.6%) or neuropsychometric deficit (at 5 days and 8 weeks), post reperfusion ventricular (GIK 14.3%, control 12.9%) and atrial fibrillation (GIK 53.6, control 46%). GIK patients had higher blood glucose levels (p=0.003) and required more exogenous insulin. GIK resulted in a higher cardiac index (p<0.0001) and a lower systemic vascular resistance index (p<0.0001) over the first 12 hours post ischaemia. GIK recipients were less likely to experience a LCOS (GIK 16.5%, control 26.9%) or inotropic support (GIK 26.1%, control 43.1% p < 0.0001) However during this period the requirements for noradrenaline were greater for these patients (GIK 69%, control 45.1%). Troponin I release over the first 12 hours was lower in GIK recipients (p = 0.03). Conclusion GIK therapy increases cardiac output and reduces vascular resistance. This translates into a reduced incidence of LCOS and inotrope requirement. Lower troponin release suggests enhanced myocardial protection. Important side effects were not increased in the GIK group. Abstracts submitted to ACTA Cambridge 20 June 2003 9 of 12 A study of the variation in beta hydroxybutyrate concentrations in perioperative diabetic cardiac surgical patients A Relwani, GR McAnulty, S Stacey, A Crerar-Gilbert Anaesthetic Department, St George's Hospital, London, UK Introduction: Conventional perioperative diabetic management maintains blood glucose concentrations within a desired range. Normalisation of blood –hydroxybutyrate may be beneficial in diabetic ketoacidosis[1].We measured perioperative changes in hydroxybutyrate (-OHB) concentrations in type 1 and 2 diabetic cardiac surgical patients to assess its potential as an additional monitor for adequacy of metabolic control. Materials and methods: This was a pilot observational study approved by the local Ethics Committee. Patients gave written consent. All patients underwent coronary artery bypass grafting. -OHB concentrations were measured using MediSense® Optium™ ketone electrodes and sensor (Abbott Laboratories). 10 bedside measurements of OHB were made for each patient: 6 at hourly intervals were taken from the time of induction of anaesthesia followed by 4 at 6 hourly intervals. Prescribed treatment was 20 ml/hr 50% glucose and variable rate of soluble human insulin (intravenous infusions) to maintain blood glucose between 4.7-6.4 mmol/l from midnight before the surgery till the re-establishment of pre-operative therapy. This was not achieved at all times. Results: 17 patients were studied, 4 females, 13 males, aged 51 to 81years (mean 64). 9 patients were type 2 and 8 type 1 diabetics. Type 2 diabetics were treated with gliclazide(3), metformin(3), metformin and glibenclamide(1) and metformin with insulin(1). Mean blood glucose during the study period was 6.75 0.49 mmol/l (range 4.1-20.6). -OHB was detected in 10 patients (4 type 1, 6 type 2). Concentrations were low in most patients and ranged between 0.1 - 0.3 mmol/l (normal < 0.5 mmol/l). In 2 patients, (one type 1, one type 2) peak -OHB concentrations were 1.3 and 1.7 mmol/l. These high -OHB levels occurred when prescribed insulin infusions had been interrupted and decreased once insulin treatment was re-started (figure 1). -OHB concentrations did not correlate with blood glucose concentrations. (Spearman r = 0.2569, p = 0.0008). Summary and conclusions: -OHB concentrations may be elevated in the presence of relatively normal blood glucose in both type 1 and type 2 diabetics following cardiac surgery. -OHB may be a more sensitive indicator of metabolic derangement than glucose concentrations alone. Further studies are needed to determine clinical application. TIME (hours post induction) PATIENT 1 (Type 1 DM) 0 1 2 3 4 5 6 12 18 24 BLOOD GLUCOSE (mmol l-1) 6.6 10.6 11.9 14.3 13.8 8.7 4.1 11.2 7.4 8.3 b-OHB (mmol l-1) 0.9 1.1 1.3 0.2 0 0 0 0 0 0 0 0 5 8 10 10 5 5 1 1 BLOOD GLUCOSE (mol l-1) 7.5 9.7 11 11 11.5 12.9 7.9 7.4 11.7 10.8 b-OHB (mol l-1) 0.5 0.2 0.2 0.3 0 0 0 0.1 0 1.7 1 3 6 6 6 6 3 3 6 0 INSULIN DOSE (last hour, International Units) PATIENT 2 (Type 2 DM) INSULIN DOSE (last hour, International Units) References: 1.Wiggam MI, et al. Treatment of diabetic ketoacidosis using normalization of blood 3hydroxybutyrate concentration as an endpoint of emergency management. Diabetes Care 1997; 20:1347-52. Abstracts submitted to ACTA Cambridge 20 June 2003 10 of 12 Differential temperature management during cardiopulmonary bypass surgery to achieve cerebral hypothermia and corporeal normothermia in humans Authors: Srinivas LV, Kaukuntla H, Townsend P, Green DH, Riddington DR, Bonser RS & Study Group Cardiothoracic Surgical Unit, Queen Elizabeth Hospital, Birmingham, United Kingdom. Objectives Normothermic cardiopulmonary bypass (CPB) has become popular over the last decade as it has been shown to have various benefits although at a potentially increased risk of neurological injury compared to hypothermic CPB. A new technique which utilises a dual lumen aortic cannula (Cobra catheter, Cardeon Corp, Cupertino, USA) to segment the aortic arch and achieve cerebral cooling in association with body normothermia has been described. The aim of our study was to investigate the thermal efficacy of this technique to achieve and maintain a temperature differential of greater than 5º C between the brain and the body during CPB Methodology After ethical approval, 30 adult patients underwent CPB using the Cardeon Cobra cannula to differentially cool the brain while maintaining body normothermia. Nasopharyngeal (NPT) and bladder temperatures (BLT) were used as surrogates of brain and body temperatures. Brain (radial) and corporeal (femoral) mean arterial pressure (MAP) together with jugular bulb and mixed venous saturations were monitored to assess perfusion adequacy to cerebral and corporeal circulations. Results The catheter was successfully placed in all patients without any difficulty. The procedures performed were coronary artery bypass surgery (n=23), valve (n=2) and combined valve & graft (n=5). A 3.2±0.46oC differential between BLT and NPT was reached in all patients after 5.5±3.6 minutes (p<0.001). A 5oC differential was reached in 29 patients after 12±7.5 minutes. The mean difference was 6.6±1 oC. Mean arterial pressures were maintained above 50mmHg and venous saturations above 60% throughout. Conclusions Differential temperature management using the new aortic cannula is possible. Cerebral hypothermia can be achieved while maintaining corporeal normothermia with adequate perfusion to both circulations reliably. This could potentially give the benefits of hypothermic and normothermic CPB. Abstracts submitted to ACTA Cambridge 20 June 2003 11 of 12 Mannitol in the bypass prime does not modify renal tubular function Yallop K, Twyman S1, Tang A, Smith D Wessex Cardiothoracic Centre, and 1Dept of Biochemistry, Southampton General Hospital, Southampton, England Introduction: Renal dysfunction occurs in 2-5% of adult patients following cardiopulmonary bypass (CPB), causing significant morbidity and mortality of 1020% [1]. Mannitol is often added to the CPB prime to reduce renal damage, but previous studies using mannitol have produced conflicting results. Method: In a double blind, randomised, controlled trial in 40 cardiac surgical patients with normal renal function, 20 patients had 5ml kg-1 of 10% mannitol in the CPB prime, while 20 had an equivalent volume of Hartmann’s solution. Standard CPB prime was with Hartmann’s solution 1000ml, gelofusine 500ml and 5000 iu heparin. Blood and urine samples were taken on admission (baseline), on arrival in the ITU and for 5 postoperative days for measurement of plasma urea and creatinine, urinary creatinine, microalbumin and retinol binding protein (RBP) [2]. Urinary microalbumin and RBP were indexed to urine creatinine, to indicate renal glomerular and tubular damage respectively. Data were analysed using area under the curve methodology and Mann-Whitney U testing in SPSS for Windows. Results: The two groups were similar in terms of pre-operative variables. The study had a power of 0.97 to detect a 10% difference in RBP between groups. There were no significant differences between mannitol and control patients for urine output, fluid balance, plasma creatinine or urea, or urinary microalbumin or RBP indexed to creatinine. - pre-op 5 Log RBP/creat - day0 4 Log RBP/creat - day1 3 Log RBP/creat - day2 Log RBP/creat 2 - day3 Log RBP/creat 1 - day4 Log RBP/creat - day5 0 mannitol control Figure: Log10 urinary RBP:creatinine index from baseline to post-operative day five in the two study groups. Values increased significantly between admission and arrival on ITU, then returned slowly to normal. Discussion: Mannitol has little impact on indices of renal function in patients with normal pre-operative plasma creatinine, and its routine use should therefore be reconsidered. References: 1 Conlon PJ, Stafford-Smith M, White WD, et al. Acute renal failure following cardiac surgery. Nephrol Dial Transplant 1999; 14: 1158-1162. 2 Twyman SJ, Overton J, Rowe DJ. Measurement of urinary retinol binding protein by immunonephelometry. Clin Chim Acta 2000; 297: 155-61. Abstracts submitted to ACTA Cambridge 20 June 2003 12 of 12 Impact of new transfusion guidelines on reduction of blood product use in cardiac surgery B Yim, R Parker, D Pigott Oxford Heart Center, John Radcliffe Hospital Background: According to the 2001 national benchmarking audit of blood and component use in primary myocardial revascularisation [1], the rate of blood product usage at our cardiac unit was far above the national average. During this period, blood products were prescribed as per clinical impression of the treating anaesthetist or surgeon. A new transfusion protocol was therefore implemented to rationalize the use of blood products in our unit. In particular, in line with current research and practice [2], we have introduced haemoglobin of less than 7.0g/dL as a trigger for red cells transfusion. Methods: A new transfusion protocol was introduced in our cardiac unit on the 1 st December 2002. Red cells were only transfused if hemoglobin fell to <7g/dl. Coagulation factors were only indicated in bleeding patients with abnormal findings as per standard coagulation tests and thromboelastogram findings. After introduction of the new protocol, 170 patients were followed up prospectively with respect to blood product usage. The results were then compared with the group of patients used for the national benchmark audit. Results: Pre protocol Post protocol Red cell use % Patient Mean no transfused units used 75% 3.3 FFP use % Patient transfused 51% 2.1 33 Mean no units used 1.4 Platelets use % Patient Mean no transfused units used 31% 0.5 12% 0.6 21% 0.4 Discussion: Since the introduction of our new transfusion protocol, we have significantly reduced the use of blood products in our unit. This represents a potential reduction in risk inherently associated with blood transfusion and a significant cost savings to our unit. References [1]National Benchmarking Audit of Blood and Component use in Primary Myocardial Revascularisation [2]Herbert PC, Yetisir E, Martin C, Blajchman MA, Wells, G, Marshall J, Tweeddale M, Pagliarello G, Schweitzer I: Is a low transfusion threshold safe in critically ill patients with cardiovascular diseases. Crit Care Med 2001 Vol. 29, No 2, pp227-34