Hesham Khalid Rashid Mosa_thalassamia
advertisement

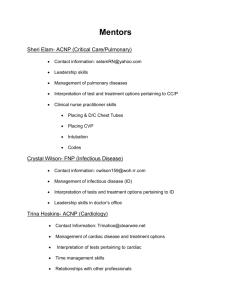
CARDIAC AND PULMONARY FUNCTIONS ABNORMALITIES IN CHILDREN WITH BETA THALASSEMIA MAJOR Khaled M. (MD)*, Moaz EBN Gabal S. (MD)*, and Hesham Rashid . (MD) ** From departments of Pediatric* and Cardiology** Benha Faculty of Medicine – Zagazig University - Egypt ABSTRACT Background: Chronic administration of large quantities of blood and inappropriate increase in iron absorption from the gastrointestinal tract inevitably lead to severe hemosiderosis in the whole body organs with impaired functions. Cardiac disorders related to biventricular failure are the most frequent cause of death in patients with betathalassemia major. Pulmonary complications in the form of restrictive and obstructive lung disease due to pulmonary hemosiderosis, recurrent heart failure. Objective: to assess cardiac and pulmonary functions in patients with beta thalassemia major. Patients & methods: This prospective study was conducted on 25 known - thalassemia major children, 14 males and 11females, their age ranged from 5.4 years to 15 years. They were selected from the pediatric clinic of Benha University Hospital. The study also included 25 apparently healthy children as a control group with matched age and sex during the period from March 2003 to January 2004. All patients were subjected to thorough history taking , full clinical examination , ECG , echocardiography , and pulmonary function testes. Results: The mean LVEDD ( left ventricular end diastolic dimension ) among cases was (4.728 + 0.592) which was significantly higher than among controls (4.0 +0.504) ( p<0.05) .The mean LVESD ( left ventricular end systolic dimension ) among cases was (3.076 +0.58) which was significantly higher than among controls (2.464 + 0.429) (P < 0.01) .The mean LVM(left ventricular mass) among cases (123.68 +13.034) was significantly higher than among controls (97.44 + 10.52) and this difference was highly significant (P < 0.001).The tricuspid E/A ratio was reversed in 5 (20%) of patients indicating right ventricular diastolic dysfunction. The ECG results revealed voltage criteria consistent with the diagnosis of left ventricular hypertrophy in 11 patients (44%), two patients (8%) showed right ventricular hypertrophy ,one patient (4%) showed left atria dilatation, and none of patients showed right atria dilatation. The mean FVC ( forced vital capacity ) among cases was ( 81.68 + 11.025 ) and among controls ( 87.52 + 3.584 ) and this difference was statistically significant (P<0.05). The mean FEV1/FVC (forced expiratory volume in first second / forced vital capacity ) among cases (93.68 + 6.447) was significantly higher than the control group (90.36 + 1.868) (P < 0.05) . Conclusions: we conclude that patients with B-thalassemia major have abnormal left and right dimensions as well as relaxation abnormalities which may be a reflection of early myocardial damage. This early damage is detectable by a widely applicable echocardiography. Also the present study has shown that restrictive disease and reduced lung diffusing capacity are the predominant abnormalities of pulmonary function due to lung fibrosis . INTRODUCTION absorption from Thalassemia is the most gastrointestinal tract the inevitably common type of chronic hemolytic lead to severe hemosiderosis in the anemia in Mediterranean countries. whole body organs with impaired It consists of several genetically functions (1). determined disorders due to unequal synthesis of globin amino Cardiac disorders related to acids chains that cause ineffective biventricular failure are the most erythropoiesis, frequent cause of death in patients anemia. The depends on hemolysis patients and survival repeated blood with beta-thalassemia major. Initial cardiac changes have been transfusions. documented Chronic administration of large echocardiography before clinical; quantities and ECG iron manifestations became apparent (2). inappropriate of blood increase in by or conventional radiological Pulmonary complications in the pediatric form of restrictive and obstructive University Hospital during the lung disease due to pulmonary period hemosiderosis, heart January 2004. The study also vascular included 25 apparently healthy congestion, microthrombosis and children as a control group with impaired alveolar growth are of matched age and sex. failure, recurrent pulmonary clinic from of March Benha 2003 to great interest because of their effect on expectancy the patient’s life quality of and All cases and control children were subjected to the following: 1- Full medical history: with life(3),(4),(5),. special emphasis on history of AIM OF THE WORK The aim of this work is to assess cardiac and pulmonary functions in patients with beta thalassemia major echocardiography, function using pulmonary tests and transfusion, desferoxamine therapy, and cardiac and chest symptoms. 2- Clinical examination: including examination general and inspection, local palpation, percussion and auscultation, electrocardiogram. PATIENTS AND METHODS This blood study was conducted on 25 well known thalassemia major children, 14 males and 11 females, their age ranged from 5.4 to 15 years. They were selected randomly from the of heart and chest. 3- Chest x-ray was done to all patients. 4- ECG: using Fukuda M-E, 500 AX. 5- Echocardiography: using ATL5000, echocardiography examination included dimensional, color 2 flow irregularly chelated. RESULTS mapping, Doppler display Table (1) shows that the and M-mode modalities. The mean LVEDD, among cases was LVEDD, LVESD, LVM, FS, 4.728 0.592 and among controls EF, pulmonary acceleration was 4.0 0.504 , and this time , and tricuspid E/A ratio statistically were measured. significant ( P > 0.05 ) . The mean 6- Pulmonary function testing; FVC and FEV1/ FVC were measured. difference was LVESD among cases was 3.076 0.58 and among controls 2.464 0.429 and the difference between Blood transfusion was given to all patients when hemoglobin (Hb) reached or decreased below 10 gm/dl. Every patient received 10-15 ml/kg packed red cells. The frequency of transfusion depended on Hb level and was nearly the same in all patients, (every 3-4 cases and controls was highly significant (P < 0.01). The mean LVM among cases was 123.68 13.034 and among controls was 97.44 10.52 and this difference was highly significant (P<0.001). Also the mean FS and EF among cases was 31.84 + 5.713 and 61.88 weeks). + 4.784 respectively and among 9 patients did not receive desferoxamine and 16 patients received it irregularly after blood transfusion by subcutaneous infusion. That is why all our patients are poorly transfused and controls was 29.4 + 2.661 and 60.24 + 2.223 and this difference was statistically non significant (P >0.05). The mean pulmonary acceleration time among cases was 112.76 11.727 and among controls was 121.6 4.301 and the showed left atria dilatation, and difference none of patients showed right atria was significant dilatation. (P< 0.05). Table (2) shows that the tricuspid E/A ratio was reversed in Table (4) shows the mean 5 (20%) of patients indicating right FVC among cases was 81.68 ventricular diastolic dysfunction. 11.025 and among controls 87.52 that Table (3) the ECG results 3.584 and this difference was revealed statistically significant (P<0.05). voltage criteria consistent with the diagnosis of The left ventricular hypertrophy in 11 cases was 93.68 6.447 and patients (44%), two patients (8%) among control group was 90.36 showed 1.868 and this difference was right ventricular hypertrophy, one patient (4%) mean FEV1/FVC among statistically significant (P < 0.05). Table (1): Mean LVEDD, LVESD, LVM, FS, EF, and pulmonary acceleration time among cases and controls. controls Cases X Range SD X Range SD T LVEDD In cm 4.728 3.7-5.7 0.592 4 3.3-4.9 0.504 4.482 <0.05 ( significant ) LVESD In cm 3.076 2-4.1 0.58 2.464 1.2-3.1 0.429 4.242 <0.01( highly significant) LVM In grams 123.68 90-150 13.034 97.44 80-144 10.52 7.83 <0.001(highly significant) FS% 31.84 21-41 5.713 29.4 24-35 2.661 1.936 >0.05 ( not significant) EF% 61.88 54-70 4.784 60.24 55-65 2.223 1.554 >0.05 ( not significant) 112.76 80-123 11.727 121.6 113-130 4.301 3..539 <0.05 ( significant) Pul. Acc. Time In milliseconds P Table (2): Distribution of the studied groups according to tricuspid E/A ratio. Cases Controls No. % No. % T P value Normal 20 80.0 25 100.0 236 Reversed 5 20.0 0 0.0 1.118 Total 25 100.0 25 100.0 -- < 0.05 significant > 0.05 not significant -- Table (3): ECG results. Cases (n = 25) Controls (n= 25) LV hypertrophy LA Dilatation RV hypertrophy RA Dilatation 11 (44%) - 1 (4%) - 2 (8%) - - Table (4): Mean FVC and FEV1/FVC among cases and controls. X Cases (n = 25) Range X Controls (n = 25) Range SD SD T FVC 81.68 55-94 11.025 87.52 81-92 3.584 2.521 FEV1/FVC 93.68 78-102 6.447 90.36 85-94 1.868 2.473 P value <0.05 significant <0.05 significant Fig (1) show pulsed wave Doppler on tricuspid valve there is RV diastolic dysfunction ( Case No. 5) higher in patient than control DISCUSSION Thalassemia is the most group ( p > 0.05 ),and (P< 0.01) common type of chronic hemolytic respectively . Cardiac dilatation anemia in Mediterranean countries occurs secondary and it is believed to be the most anemia which prevalent of all human genetic association diseases. It’s inherited as an dilatation and chronic anemia. Our autosomal genetic disorder (6). finding to chronic means strong between are cardiac similar to Cardiac disorders related to Khalifa et al ,(9) who showed a biventricular failure are the most significant increase of all cardiac common cause of death in patients dimensions by echocardiography with beta-thalassemia major. Heart (LAD- LVEDD-LVESD) more in failure anemic regularly transfused patients. They hypoxia, cardiac hemosiderosis, stated that these cardiac structural arrhythmias changes are due to chronic anemia is caused and by hyperdynamic more than siderosis. circulatory overload (7). In the present study finding Beta-thalassemia major also affects pulmonary functions where coincides with Walker restrictive Kushner, et al predominant pattern is abnormality the in the mean (11) (10) and , they found that LVM index pulmonary function tests. A mild significantly obstructive element can coexist thalassemic with restrictive lung disease in a controls (P < 0.05) , while in the small number of patients (8). present study there was highly In this study both LVEDD and LVESD were significantly increased was patients in versus significant increased LVM among cases versus controls (P>0.001 ) . As regard the FS and EF right ventricular there was no significant difference dysfunction between patient and control group thalassemic patients more than (P > 0.05). These results are control group. similar to other reports which also demonstrated preserved left was tricuspid observed in The ECG results revealed voltage criteria consistent with the ventricular systolic function inspite diagnosis of cardiac dilatation (2), (3). hypertrophy in 11 patients (44%) , Khalifa Desideri et et al.(9) al. (12) and found of left ventricular two patients (8%) showed right ventricular hypertrophy , one insignificant difference between all patient (4%) showed left atria the studied cases and controls as dilatation, and none of patients regards the mean values of EF and showed FS (P>0.05). Khalifa et al. right atria (9) dilatation. found voltage In this study the mean criteria fulfilling left ventricular pulmonary acceleration time was hypertrophy in (33%) of patients, significantly decreased in patient voltage criteria of right ventricular than control group (P<0.05). This hypertrophy in (15%) of patients finding coincides with a study and deep Q in V5 or V6 indicating done by Hahalis et al. showed that the (13) , they pulmonary septal hypertrophy in (7%) of patients. thalassemic A significant decrease in patients results from pulmonary FVC was found in the patient's hemosiderosis. group compared to the control hypertension in In this study and study done by Gharzuddine et al. (14) , the group (P<0.05). This indicates that the patient's group have restrictive pattern of pulmonary function (17) , (mild to moderate restriction). Cunningham et al. Also FEV1/FVC was significantly the restrictive lung disease to be higher in patient group than in the not control (P<0.05). This indicates a hemosiderosis but also due to mild degree of obstructive pattern transfusion major due to pulmonary dependent chronic - volume overload with decrease of patients. lung capacity causing progressive of pulmonary function in thalassemia only explained Analysis of these values indicated a restrictive and obstructive lung restriction. Vittorio et al. (5) , found that disease in the studied cases with hypoxemia predominance of the restrictive abnormality in patients with beta- pattern. thalassemia major that stimulates Pulmonary patients with functions in beta-thalassemia major were the subjects of many previous studies (15), (16), (17), is a consistent excessive alveolar growth. This hypoxia induced alveolar proliferation is both excessive that (with no corresponding increase in reported the presence of restrictive bronchial and bronchiolar tree) and lung disease. aberrant Fung et al. (15) since some of the , found that proliferating alveoli are not in the means for FEV1 and FVC for direct continuity with the bronchial thalassemia tree. This results in distal gas group were significantly smaller than those for trapping and air way obstruction. However, Carnell; et al. (18), found that difference in FEV1/FVC was not restrictive disease and reduced statistically significant (P>0.05). lung diffusing capacity are the the control group. predominate abnormalities of pulmonary function in patients with thalassemia major. They appropriate for those developing suggested that these pulmonary countries dysfunctions are due mainly to affected by thalassemia. lung fibrosis and/or interstitial with a population Also the present study has edema related to iron overload. shown that restrictive disease and CONCLUSION reduced lung diffusing capacity are From our data we conclude the predominant abnormalities of that clinically patients with B- pulmonary function in patient with thalassemia major have abnormal thalassaemia major due to lung left and right dimensions as well as fibrosis and / or interstitial edema relaxation related abnormalities which to iron overload, cardiac damage, may be a reflection of early hypoxemia, myocardial damage. This early decreased alveolar growth and damage is detectable by a widely pulmonary vascular involvement applicable by microthrombosis. method which echocardiographic may be more REFERNCE 1-Pearson, H.A. and Benz, E.l. (1990): Thalassemia syndromes. In: Blood disease of infancy and childhood ed. By Miller, D.R., Baehner, R.L. and Miller, L.P. 6th ed. St. Louis, Philadelphia, Washington DC. Toronto, CV Mosby Company, 428-63. 2-Hui ,L. , Leung, M.p., Ha, S.Y., Chau ,A.K., and Cheung, Y.F.(2003) Early left ventricular dysfunction and chelation therapy in thalassemia major. Heart; 89:669-70. 3-Griasaru, D.; Goldfarb, A.W. and Hasin, Y. (1990): Cardiac damage an important aetiology in production of pathological lung disease. Arch. Intern. Med., 146: 2344-2349. 4-Mansell, A.; Bryan, C. and Levinson, H. (1987): Airway closure in children. J. Appl. Physiol., 39:711. 5-Vittorio,C., Emanuela, D.,Matteo, p., and Edgardo,D.(2003): Pulmonary function abnormalities in Transfusiondependent patients with Betathalassemia. Am J Respir Crit Care Med; 168:180-184. 6-Honig, G.R. and Sharon, B.I. (1996): Globin synthesis, thalassemia syndrome. In: Hematology, A problem oriented approach ed. By Gross, S. and Roath, S. 16th ed. Baltimore, Williams and wilkins, 648-1112. 7-Landzkowsky,P. (2000): Hemoglobin defects, thalassemias, manual of pediatric hematology and oncology, 3rd ed. Churchill, Livingstone, New York, London and Tokyo, P. 182-191. 8-Jefrey, M.F.; Sumana, R.P.; Pottipati, I.R.; Ingrid, K.R.; Martin, L.L. and patrica, J.G. (1994): Pulmonary function abnormalities in thalassemia major and the role of iron overload. Am. J. Respir. Crit. Care Med., 149: 1570-4. 9-Khalifa, A.S; Ayoub, A.M.; Al-Shabrawy, L.; Shatla, H.; ElBaz, F., Gadallah, M. and Azmy, M. (1989): Cardiac changes in Betathalassemia major and effect of treatment. Egypt. J. Ped., 6: 415. 10- Walker, J. M (2002). The cardiac changes in thalassemia major. Their assessment by Doppler echocardiography. Eur.Heart J. January; 23(2):102-105. 11-Kushner, J.P.,Porter ,J.P.and Olivieri, N.F.(2001). Quantitative ultrasonic analysis of myocardium in patients with thalassemia major and iron overload. Hematology, January; 1:47-61. 15 -Fung, K.P.; Chow, O.K.; Yeung, S.O.S. and Yuen, P.M. (1987): Pulmonary function in thalassemia major. J. Ped., 111: 634-37. 12-Desideri, A.; Scatolin, G.; Gobellini, A. and Cavuto, F. (1994): Left ventricular function in thalassemia major: protective effect of desferoxamine. Can. J. Cardiol. Jan. Feb., 10(1): 63-6. 13-Hahalis,G.,Manolis A.S., Apostolopoulos,D., Alexopoulos, D.,Vagenakis A.G., and Zoumbos. N.C.(2002): Right ventricular dysfunction in B-Thalassemia major. Eur.Heart J, January;23(2):147-156. 16 - Bccalo, M.D.; Shumud, k.; Naw af, H.; Greif, Z. and Grief, J. (1992): Blood transfusion and lung function in children with betathalassemia major. Chest; 101 (2): 362-365. 14Gharzuddine,W.S.,Kazma,H. K.,Nuwayhid,I.A.,Bitar,F.F.,Ko ussa, S.F.,Moukarbel,G.V.,and Taher ,A.T(2002). Left ventricular diastolic Doppler characteristics in BetaThalassemia Major. Evidence of and early stage of impaired relaxation. Eur J Echocardiogr; 3:47-51. 18 - Carnelli, V.; D, Angelo, E.; Pecchiari, M.; Ligorio, M. and D. Angelo E. (2003): Pulmonary dysfunction abnormalities in Betathalassemia major and the role of iron overload. Am. J. Resp. Crit. Care Med. 168 (2): 180. 17 - Cunningham, M.J.,Acklin ,E.A.,Neafeld ,E.J., and Cohen ,R.(2004) Complications of thalassemia major North America Blood.February; 26:80-85. الملخص العربى مقدمة : بعتبر مرض السالسيميا من اهم انواع األنيميا التى ينتج عنها تخثر خاليا الدم الحمراء وينتشر هذا المرض فى األقطار التى تطل على البحر األبيض المتوسط نتيجة لخلل جينى متوارث . وتؤدى عملية نقل الدم المتعددة لهؤالء المرضى إلى زيادة نسبة الحديد بالدم مما يؤدى إلى ترسيبه فى أعضاء متعددة من جسم اإلنسان .ويؤدى ترسب الحديد بالقلب إلى فشل وظيفى فى البطينين األيمن واأليسر كما يترسب فى الرئتين ويؤدى إلى فشل فى الوظائف التنفسية . الهدف من البحث :يهدف البحث إلى االكتشاف المبكر للخلل الوظيفى فى القلب وكذلك الرئتين فى مرضى انيميا البحر المتوسط . طرق البحث :تم اجراء البحث على 52طفالً يتراوح اعمارهم بين 2.5و 52سنة مصابون بانيميا البحر المتوسط ومن المترددين على مستشفى بنها الجامعى – كما تم إجراء البحث على 52 طفالً طبيعيين ظاهريا ً من نفس السن والنوع كمتطوعين .وتم أخذ التاريخ المرضى لكل طفل وعمل كشف طبى كامل ,وعمل رسم قلب ,وموجات فوق صوتية على القلب وعمل اختبار للوظائف التنفسية للرئتين . نتيجة البحث :وتبين من البحث اآلتى : زيادة فى حجم البطين األيسر أثناء االنقباض واالنبساط فى مرضى أنيميا البحر المتوسط بالمقارنة بالمتطوعين ,كما وجد أن % 52من المرضى يعانون من خلل فى الوظيفة االنبساطية للبطين األيمن .كما أثبت البحث أن هناك % 55من المرضى المصابين بأنيميا البحرالمتوسط يعانون من تضخم فى البطين األيسر ,ونسبة % 8تضخم بالبطين األيمن .كما أثبت البحث وجود خلل فى الوظيفة التنفسية للرئتين فى مرضى أنيميا البحرالمتوسط بالمقارنة بالمتطوعين. الخالصة :إن مرضى أنيميا البحرالمتوسط يعانون من خلل فى الوظيفةاالنبساطية للبطين األيمن وزيادة فى حجم البطين األيمن واأليسر ويمكن بمتابعة هؤالء المرضى االكتشاف المبكر لهذا الخلل من خالل عمل متابعة بالموجات فوق الصوتية على القلب . كما أن هؤالء المرضى أيضا ً يعانون من خلل فى الوظائف التنفسية للرئتين نتيجة لترسيب الحديد بهما مما يؤدى إلى حدوث تليف فى نسيج الرئتين .