EP8-B - Acuity Classification levels for NMH ICUs Item 5 of 5)
advertisement
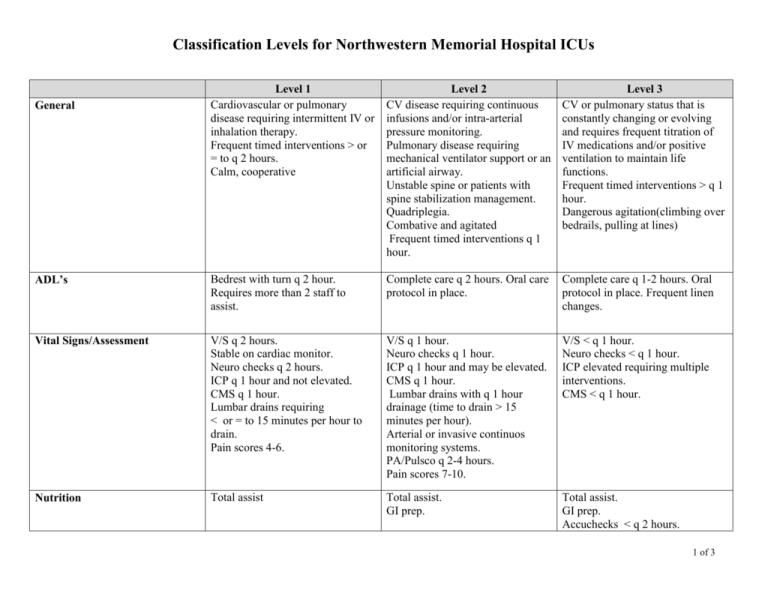
Classification Levels for Northwestern Memorial Hospital ICUs Level 1 Cardiovascular or pulmonary disease requiring intermittent IV or inhalation therapy. Frequent timed interventions > or = to q 2 hours. Calm, cooperative Level 2 CV disease requiring continuous infusions and/or intra-arterial pressure monitoring. Pulmonary disease requiring mechanical ventilator support or an artificial airway. Unstable spine or patients with spine stabilization management. Quadriplegia. Combative and agitated Frequent timed interventions q 1 hour. Level 3 CV or pulmonary status that is constantly changing or evolving and requires frequent titration of IV medications and/or positive ventilation to maintain life functions. Frequent timed interventions > q 1 hour. Dangerous agitation(climbing over bedrails, pulling at lines) ADL’s Bedrest with turn q 2 hour. Requires more than 2 staff to assist. Complete care q 2 hours. Oral care protocol in place. Complete care q 1-2 hours. Oral protocol in place. Frequent linen changes. Vital Signs/Assessment V/S q 2 hours. Stable on cardiac monitor. Neuro checks q 2 hours. ICP q 1 hour and not elevated. CMS q 1 hour. Lumbar drains requiring < or = to 15 minutes per hour to drain. Pain scores 4-6. V/S q 1 hour. Neuro checks q 1 hour. ICP q 1 hour and may be elevated. CMS q 1 hour. Lumbar drains with q 1 hour drainage (time to drain > 15 minutes per hour). Arterial or invasive continuos monitoring systems. PA/Pulsco q 2-4 hours. Pain scores 7-10. V/S < q 1 hour. Neuro checks < q 1 hour. ICP elevated requiring multiple interventions. CMS < q 1 hour. Nutrition Total assist Total assist. GI prep. Total assist. GI prep. Accuchecks < q 2 hours. General 1 of 3 Classification Levels for Northwestern Memorial Hospital ICUs IV’s/Meds Intermittent IV medications to maintain HR and B/P parameters. Continuous non-vasoactive IV medication infusion (heparin, PCA). Cardiotonic medications with stable V/S. Chemical elective cardioversion. Inhaled medications by nebulizer or albuterol inhaler. IV pain management with scores 4-6. Blood product infusions. Chemotherapy. CVHD meds IV. Insulin drip with q 1 hour checks. Labs q 2-4 hours not including accuchecks. Cardiac dysrhythmias or unstable hemodynamic status requiring intermittent or continuous medications or electrical therapy. (DCCV). Chemotherapy with protocols. Multiple vasopressors with titration. Stable CVVH. Multiple drips with frequent adjustments. Rapid infuser for IV fluids/blood. Multiple transfusions or pressure bag infusions. Triple H Therapy with 2 or > IV drips. Hourly cc per cc replacements. Neuromuscular blockaide. Unstable CVVH. Labs q 2 hour not including accuchecks. O2 FIO2 < or = to 50%. BiPAP first 24 hours. Suction q 2-4 hours. PG2 Ventilator. Vital capacity q 2 hour with stable respiratory status. FIO2 > 50%. Artificial airway or recent extubation ( < 2 hrs ). Suction q 1-2 hours. Ventilators: CPAP or SIMV AC. Nursing Treatments Treatments requiring 2 hours per shift. Chest tube to continuous suction. Education Intense teaching done at bedside requiring reinforcement and discharge planning. Treatments requiring > 2 hours per shift. Rotorest bed. B/P support IV. Advanced education on treatments and/or equipment. Labs q 1-2 hours. Hemogram with q 2 hour transfusions and multiple blood products. FIO2 > 60% and mechanically ventilated patients with PEEP levels > 10. Frequent ventilator changes > 1 x/hour. Frequent suctioning > 30 minutes per hour. Impending respiratory failure. Treatments requiring > 1 RN. Labs Frequent education/counseling on multiple issues regarding patient care. Language/communication barrier. 2 of 3 Classification Levels for Northwestern Memorial Hospital ICUs Psychosocial Functional family with minimal issues. Patient and family coping well. Patient family issues requiring q 24 hour interventions. Patient and family having trouble coping. Tests/ Transport Status Requires competent and trained nurse to administer IV or inhaled drugs during study and transport. Critical care or nurse and a Critical Care Respiratory therapist ( if applicable for airway and ventilator support) needed for transport and presence throughout the procedure. A member of the Critical Care physician team must be immediately available throughout the study for urgent or emergent interventions. Off Unit procedure time Exception to nurse transporting: (Written transfer order to general care floor, awaiting bed – off cardiac monitor, all invasive monitoring line D/CD) Exception to nurse staying during procedure: All anesthesia managed cases except patients with EVD/Lumbar drains Time off unit with nurse: Dysfunctional patient/family. Multiple issues requiring multiple interventions from care team. Crisis intervention. Critical care nurse, critical care Respiratory Therapist, critical care physician (attending, fellow or minimum 2nd year resident with critical care skills) and transport personnel to facilitate emergency movement and/or return to units. Time off unit with team: ____________________________ Time off unit with nurse: ____________________________ 3 of 3