20130328-080504
advertisement

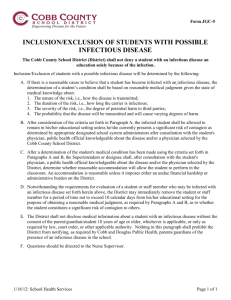
Theme 6. Mental disorders during infectious diseases. 1. Ethiology of infectious diseases. 2. The clinical courses of mental disturbances in infectious diseases. -transient (short-term) psychoses; -prolonged (lingering) psychoses. 3. Irreversible mental disorders. 4. Certain specific infectious diseases. 5. Treatment, prophylaxis and examination. 6. Course and prognosis. Tests 1. When may mental disorders occur? a) in general infections b) in the infections of the central nervous system c) in the some specific infections only d) all listed e) nothing listed 2. Which of the listed mental disturbances in infectious diseases have the prolonged clinical courses? a) dementia b) delirium c) sopor d) epilepsy-like agitation e) all listed 3. All the listed statements about prolonged psychoses are correct, except: a) may end in long-term asthenic states b) do not have any serious after-effects for the patient c) do not include disturbances of consciousness d) may end in amnestic syndrome e) nothing listed 4. Which infectious disease has such features as Sydenham's chorea? a) flu b) syphilis c) cerebral rheumatism d) AIDS e) all listed 5. What is the main manifestation of organic psychiatric disorders in AIDS? a) asthenic syndrome b) amnestic syndrome c) psychoorganic syndrome d) dementia e) all listed 6.Which of the listed mental disturbances in infectious diseases have the transient clinical courses? a) paranoid states b) delirium c) hallucinosis d) depressive states e) all listed 7. All the listed statements about transient psychoses are correct, except: a) they are short-term b) do not have any serious after-effects for the patient c) do not include disturbances of consciousness d) occur in acute infectious illnesses e) nothing listed 8. Which of the listed mental disorders are the most frequent type of the central nervous system reaction to infection? a) oneiroid b) delirium c) sopor d) epilepsy-like agitation e) all listed 9. Which infectious disease usually provokes adjustment disorders and neurotic reactions? a) flu b) syphilis c) cerebral rheumatism d) AIDS e) all listed 10. When the neuropsychiatric symptoms of tertiary syphilis after the primary infection may emerge? a) from 1 to 2 months b) from 1 to 2 years c) from 4 to 7 years d) more than 10 years e) all listed Clinical task 1. A male patient 22 years old, two weeks ago had flue, but didn't stay in bed and continued to work. Complains of constant pain in his throat, supposes that he "is ill with the larynx tuberculosis", that his throat "has decomposed", all his teeth have fallen out, and the brain "has dissolved." Refuses to walk, because all his organs were "pasted together." Assured everybody around that he has died, remaining "a living corps." His mood is gloomy and sad. Refuses to communicate with people, because his "mouth is full of dangerous germs." 1. What symptoms does the patient have? 2. What psychopathological syndromes does the patient have? 3. What disease can you think of? 4. Prescribe treatment to the patient. Clinical task 2. A woman aged 35 has been suffering with pulmonary tuberculosis for 10 years. When in phthisiatric clinic, she started to act strangely: put on a gaudy make-up, gathered the other patients around herself, was singing and dancing with them. Highly excited, passed all the time among males, flirted, started sexually-biased conversations. The whole night absented from the clinic ("was on a date"). 1. What symptoms does the patient have? 2. What psychopathological syndromes does the patient have? 3. What disease can you think of? 4. Prescribe treatment to the patient. Clinical task 3. Patient S., female, 38 years old was hospitalised to a tuberculosis hospital. Her somatic state was grave: she had fever, tachicardia, and breathlessness. In bed she constantly moved, waved her arms, sometimes lay across the bed with the risk of falling down. Didn't answer questions or react to any contact. Sometimes smiled and seamed to listen to something, her speech was incoherent and senseless. On recovery the patient didn't remember anything about her experiences during the illness. She had psychoorganic syndrome after the described state. 1. What symptoms does the patient have? 2. What psychopathological syndromes does the patient have? 3. What disease can you think of? 4. Prescribe treatment to the patient. List of recommended literature Basic literature. 1. Concise Oxford Textbook of Psychiatry. M. Gelder, D. Gath, R.Mayou. – Oxford; New York; Tokyo; Oxford University Press, 2007. – 953 p. 2. Modern Synopsis of Psychiatry. A.M. Freedman, H.I. Kaplan, B.J. Sadock. – USA, 1982. – 433 p. 3. Psychiatric Dictionary / 5th ed. R.J. Campbell. – Oxford; New York; Oxford University Press, – 1981. – 693 p. 4. Psychopatology and addictive Disorders / Ed. By Meyer. - New York; London, 1986. – 283 p. 5. Psychiatry: course of lecture /Ed.by V.S. Bitensky. – Odessa, 2005. – 336 p. 6. Zimbardo Ph.G. Psychology and Life. - USA, 19991. – 189 p. Additional literature. Brundtland G.H. Mental health in the 21st century // Bulletin of the World Helth Organization. – 2000. - №87. – Р. 411. Desjarlais R., Eisenberg L., Good B. et al. World Mental Health: Problems and Priorities in Low-Income Countries. – New York: Oxford University Press, 1995. – 144 p. Marsella A., Kleinman A., Good B. Cross-cultural studies of depressive disorders. An overview. Culture and depression. – Berkley: University of California Press, 1985. – 213 p. Mulrow C.D., Williams J.W. Jr., Trivedi M., et al. Treatment of depression: newer pharmacotherapies. Rockville, MD: Agency for Health Care Policy and Research, 1999. – 253 р. Murray C.J.L., Lopez A.D. The global burden of disease: a comprehensive assessment of mortality and disability from disease, injuries and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press, 1996. – 68 p. Kielholz P. Masked Depression. — Berne, 1973. – 97 p. Lopez-Ibor J. J. The Present Status of Psychotropic Drugs / Ed. by A. Cerletti, F. J. Bove. - New York, 1999. - 519 p Preskorn, S.H. Outpatient management of depression: A guide for the Primarycare practitioner/ S.H. Preskorn. - Wichita; Kansas: Professional Communications,Inc., 1994. - 147 p. Ustun T.B., Sartorius N. Mental Illness in General Health Care. An International Study. – Chichester: John Willey @ Sons Ltd, 1995. – 336 p.