RCGP clinical priority on eye health - survey report 1
advertisement

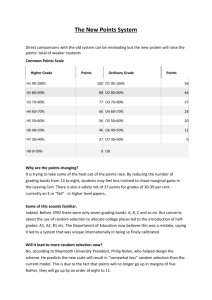
UK Vision Strategy RCGP – Royal College of General Practitioners The Royal College of General Practitioners clinical priority on eye health: summary analysis of UK data Table of Contents 1 2 3 Introduction .......................................................................... 1 Methods ............................................................................... 2 Results ................................................................................. 2 3.1 Key findings ................................................................... 2 3.2 Summary of results ........................................................ 3 4 Statistical reporting and accuracy......................................... 6 Introduction The Royal College of General Practitioners (RCGP) has selected eye health with a focus on ageing and sight loss as one of their clinical priorities until March 2016. The aims of the eye health clinical priority programme include reducing preventable sight loss amongst patients aged 65 plus to help improve their quality of life; and to provide more effective management of patients with eye conditions. The RCGP has appointed a Clinical Champion, Dr Waqaar Shah, to lead this programme in partnership with the RCGP and the UK Vision Strategy. The purpose of this survey was to establish levels of awareness of General Practitioners (GPs) and their Practice Teams in regards to managing the eye health of their patients and the needs of their patients with sight loss. The information gained from the survey will help to inform the RCGP clinical priority for eye health programme and to assess the programme’s impact in general practice and across primary care. Methods An online survey of General Practitioners (GPs) and primary care practice staff was conducted between November 2013 and January 2014. Participants were invited to complete the survey via an email sent to all the Royal College of GPs 50,000 members and via a targeted marketing and public relations programme including RCGP blogs, GP internet sites and media coverage in primary care trade magazines and networks. The survey was administered in SurveyMonkey. Voluntary sampling was used to generate the sample. Survey data were exported into SPSS (version 20), cleaned, duplicates removed and descriptive analyses applied to the data. This report presents analysis of the UK-wide data. Separate country reports will be presented in future releases of the data. Throughout the report percentages are given when the base sample is greater than 20. For samples sizes smaller than 20, whole numbers are reported. Results Key findings Only twenty per cent of GPs and ten per cent of nurses were aware of the RCGP clinical priority for eye health with a focus on ageing and sight loss. Fewer than half of respondents said their practice made information regarding bookings and appointments, or information about the practice available in accessible formats. GPs' confidence in their ability to spot the symptoms or signs of eye conditions was dependent on the condition. Confidence in spotting the signs or symptoms of cataract was high, but low for age related macular degeneration. Confidence in the ability to spot the symptoms or signs of different eye conditions was lower among nursing staff, compared with GPs. There was limited awareness of the eye conditions that are more prevalent in minority ethnic groups or the prevalence and eye care needs of people with learning disabilities. The majority of patients presenting with concerns about sight problems or eye conditions are referred to either an optometrist or ophthalmologist, according to the diagnosis and severity of the condition. Nurses are more likely to refer patients presenting with concerns about sight problems or eye conditions to a GP colleague rather than an optometrist or ophthalmologist. www.rcgp.org.uk/eyehealth circ@rcgp.org.uk 020 7391 2177 The majority of respondents believe that talking to patients about their sight and educating patients about sight loss; supporting patients to comply with their eye health medication; and incorporating eye health into wider work around obesity, falls, diabetes and smoking, are important facets of their role. The majority of respondents support guidance for patients on the management of eye conditions; information/literature and guidance for patients regarding sight loss; training for practice staff to support patients with sight impairment; and better working with other local health and social care services as a means of improving the management of patients' eye health. Summary of results Respondent characteristics In total, 296 people responded to the survey. Of these, 194 were based in England (65.5 per cent), 78 in Scotland (26.4 per cent), 19 in Wales (6.4 per cent) and 5 in Northern Ireland (1.7 per cent). Of the 296 respondents, 205 were GPs (69.3 per cent) and 45 were nurses (15.2 per cent). There were 10 GPs with a special interest in ophthalmology (3.4 per cent). The GP sample represents less than 1 per cent of the GP population. Of the 205 GPs, 133 were based in England (64.9 per cent), 50 were based in Scotland (24.4 per cent), 18 in Wales (8.8 per cent) and 4 in Northern Ireland. Number of years in current profession A third of respondents (34.1 per cent) had been practicing for more than 20 years, representing the largest group in terms of the number of year practicing. A quarter (24.3 per cent) had been practicing for less than 5 years. Among GPs, 36.6 per cent had been practising for more than 20 years; although the proportion was substantially higher in Scotland (48.0 per cent). 7 out of 18 GPs in Wales had been practicing for more than 20 years and 1 GP in Northern Ireland. Among nursing staff, 36.6 per cent had been practising for more than 20 years, compared with 8.9 per cent for less than 5 years. In general, nurses had been practicing for more years than their GP colleagues. Knowledge of RCGP priority A fifth of GPs (19.5 per cent) was aware of the RCGP clinical priority for eye health with a focus on ageing and sight loss. www.rcgp.org.uk/eyehealth circ@rcgp.org.uk 020 7391 2177 Overall, 8.9 per cent of nurses were aware of the clinical priority for eye health. Patient attendance due to problems of vision The majority (63.6 per cent) of clinical staff (i.e. GPs and nursing staff) reported that fewer than 5 per cent of patients presenting at the surgery each week did so because of problems of vision. Professionals ability to recognise the symptoms or signs of eye conditions A third of GPs (34.1 per cent) were confident (ie responded 'somewhat confident' or 'very confident') they could spot the symptoms or signs of age related macular degeneration (AMD). A large majority of GPs (89.8 per cent) were confident they could spot the symptoms or signs of cataract. Approximately half of GPs were confident they could spot the symptoms or signs of diabetic retinopathy (48.8 per cent), glaucoma (51.2 per cent), or refractive error (49.3 per cent). Confidence in the ability to spot the symptoms or signs of different eye conditions was lower among nursing staff, compared with GPs. Only 4.5 per cent of nursing staff were confident they could spot the symptoms or signs of AMD; the majority (81 per cent) were 'not at all confident'. A quarter of nurses (22.7 per cent) were confident they could spot the symptoms or signs of cataract; 13.6 per cent were confident they could spot the symptoms or signs of diabetic eye disease; 9.1 per cent were confident they could spot the symptoms or signs of glaucoma; and 6.8 per cent were confident they could spot the symptoms or signs of refractive error. Management of eye conditions and the role of health professionals in supporting patients The majority of GPs supported (ie either 'agree' or 'agree strongly') the statements: I think it is important that I ask my patients about their sight (75.6 per cent); Eye health promotion and education to prevent avoidable sight loss is an important part of my role (63.4 per cent); Supporting (through guiding, educating, encouraging compliance) my patients to comply with their eye health medication is a vital part of my role (75.6 per cent); Eye Health is addressed as part of my work around obesity, falls, diabetes and smoking (59.8 per cent). www.rcgp.org.uk/eyehealth circ@rcgp.org.uk 020 7391 2177 However, only a small minority GPs supported the statements: I am well informed on the eye conditions that are more prevalent in some minority ethnic groups (9.2 per cent). I am well informed about prevalence and eye care needs of people with learning disabilities (12.6 per cent). Only 6 GPs with a special interest in ophthalmology were well informed about eye conditions prevalent in ethnic minority groups. Four were well informed about eye conditions prevalent in people with learning disabilities. A slightly higher proportion of nurses supported the statements: 'I think it is important I ask my patients about their sight (80.0 per cent); and 'Eye Health is addressed as part of my work around obesity, falls, diabetes and smoking' (68.9 per cent). However, nurses were less informed on the eye conditions that are more prevalent in minority ethnic groups (2.2 per cent) and the prevalence and eye care needs of people with learning disabilities (4.5 per cent). Referral routes for patients presenting with concerns about sight problems or eye conditions Asked where they would refer patients presenting with concerns about sight problems or eye conditions, 90.2 per cent of GPs indicated they would refer to either an optometrist or ophthalmologist, according to the diagnosis and severity of the condition. Conversely, only 22.2 per cent of nursing staff would refer a patient direct to optometry or ophthalmology. The most common direct route of referral would be to a GP colleague (46.7 per cent). The provision of accessible information by practices Fewer than half of respondents (43.2 per cent) said their practice made information regarding bookings and attending appointments available in accessible formats. 40.5 per cent said general information about the practice (signage, newsletter, reception information) was available in accessible formats. A large majority of respondents (80.4 per cent) said they would be interested in finding out how they can provide information in accessible formats. www.rcgp.org.uk/eyehealth circ@rcgp.org.uk 020 7391 2177 The extent of training offered to practice staff to support patients who were blind and partially sighted A quarter of respondents (26.1 per cent) had been offered training on how to support patients who were blind and partially sighted. For GPs it was 25.6 per cent. The proportion of nurses offered training was markedly lower (18.2 per cent); only 1 GP in training had received guidance. 81.1 per cent of respondents said they would be interested in receiving training or guidance on how to support patients who were blind and partially sighted. Suggestions for improving services Respondents were provided with a series of statements and asked to select which they thought would improve the management of patients' eye health. The majority of respondents supported each of the following statements: Training and guidance on the management of eye conditions 71.3 per cent); Information/literature and guidance for patients regarding…' (72.6 per cent); Training for practice staff to support patients with sight impairment (77.4 per cent) and Joined up working with other local health and social care services (60.8 per cent) A higher proportion of nursing staff supported each statement, compared with overall respondents (80.0 per cent, 88.9 per cent, 82.2 per cent and 62.2 per cent, respectively). Statistical reporting and accuracy Voluntary sampling was used to generate the survey sample. As such, the findings are applicable only to the survey respondents. Inferences about UK or country representativeness are not applicable and should not be drawn. www.rcgp.org.uk/eyehealth circ@rcgp.org.uk 020 7391 2177