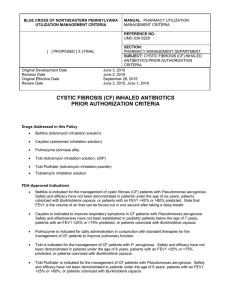
INHALED ANTIMICROBIAL THERAPY
advertisement

INHALED ANTIMICROBIAL THERAPY Advantage: Ability to provide a greater concentration of antibiotics directly into the target organ, the lung, avoiding systemic complications with a noninvasive method. Disadvantage: • The high cost. • The inefficiency of the currently available delivery systems in delivering drugs to the lower airways. • The time spent by the patient. Successful development of aerosolized anti-microbial therapy depend on 3 major factors 1. Nature of disease process. Diseases that involve infection of the airway without a substantial systemic component (eg, cystic fibrosis, bronchiectasis) are much more suitable for aerosolized therapy than diseases of the parenchyma that are associated with substantial risk of systemic complications (eg, pneumococcal pneumonia). 2. The delivery system. Produce respirable particles & targeting lower airways 3. The antimicrobial agent. Schematic outlining the factors that prevent extrapolation of lung dose from the nominal dose placed in the delivery system Nominal dose Aerosolized Remained in device (Dead volume & impaction) Vented to external environment Inhaled Deposited Extrapulmonary deposition Exhaled Pulmonary deposition Bronchial deposition Systemic exposure Alveolar deposition Excretion Indications for aerosolized anti-microbial: - Bacterial infections. - Fungal infections. - Viral infections. Bacterial infections: 1- Tobramycin sulfate: - TOBI is a sterile preservative-free aqueous solution containing 300mg tobramycin/5mL - Licensed for long-term management of chronic pulmonary infection due to Pseudomonas aeruginosa in cystic fibrosis patients aged 6 years and older. - TOBI should be administered over 15 minutes, using a hand-held PARI LC PLUS reusable nebuliser in repeated cycles of 28 days on drug followed by 28 days off drug. It is hoped that intermittent administration will allow bacteria that become resistant to tobramycin to regain sensitivity. - Patients should inhale TOBI, 300mg twice daily (as close as possible to 12 hours) during the 28 day on drug period regardless of age or weight. - TOBI for inhalation is a new formulation of tobramycin which is preservative-free. This is an advantage over nebulised intravenous formulations of tobramycin in terms of airway tolerability 2- Pentamidine isothionate: NebuPent® is a preservative free powder for solution (for nebulization) containing 300mg pantamidine isothionate • Licensed for treatment and prevention (prophylactic) of pneumonia caused by Pneumocystis carinii (PCP) in HIV patients. • Dose: Inhalation 300 mg every 4 weeks via Respirgard® II. Deliver until nebulizer is gone (30-45 minutes). Requirements for commercial jet nebulizer • First, they need to provide small particles (mass median aerodynamic diameter of approximately 1 mm) to optimize delivery to the lung periphery rather than to the central airways. • Second, they must incorporate an exhalation filter to reduce environmental contamination. Respirgard® II - Its design incorporates an external baffle to remove large particles from the aerosol, and the treatment time is 40 minutes to nebulize 6 mL, with approximately 10% of the drug depositing in the lung. - Because alveolar clearance of relatively insoluble particles is slow compared to the clearance of particles depositing in ciliated airways (weeks instead of hours), the drug needs to be administered at only 2week or 4-week intervals 3- Colomycin (colistimethate sodium): • Colistimethate is FDA approved for intravenous or intramuscular injection but not as a liquid to be inhaled via nebulizer. • After mixing with sterile water and a buffer, colistimethate undergoes spontaneous hydrolysis to the bioactive form colistin. A component of colistin, polymyxin E1, is toxic to lung tissue. • phase III trials is now being conducted on a new dry powder antibiotic formulation which drastically reduces the daily treatment time. • The new inhalation system is called Colobreathe, for use by cystic fibrosis patients whose lungs are infected by pseudomonas aeruginosa bacteria. Fungal infections: • Amphotericin B is tested to be prophylactically administered via inhalation for invasive pulmonary aspergillosis which is one of the most devastating complications of bone marrow transplantation and aggressive anticancer chemotherapy regimens. • Its use has not been adequately evaluated. Viral infections: Ribavirin: • Ribavirin aerosol is indicated in the treatment of carefully selected hospitalized infants and young children (<3 yrs old) with severe lower respiratory tract infections due to respiratory syncytial virus (RSV). • Suspected to be teratogenic so never to be given to lactating or pregnant females also health care workers should be protected from exposure. • Dose: A concentration of 20 mg/mL (6 g reconstituted with 300 mL of sterile water without preservatives) administered for 12-18 hours/day for 3 days, up to 7 days in length using Viratek®. • Aerosol inhalation is done only by Viratek® Which is a small particle aerosol generator (SPAG-2). • The nebulizer generates a fine aerosol of hydrated Virazole, and the drying chamber further dehumidifies the aerosol. • It may be also connected to mechanical ventilation circuit. Zanamivir: • Powder for oral inhalation: 5 mg/blister [4 blisters per Rotadisk® foil pack packaged with Diskhaler® inhalation device. • Used for the prophylaxis & treatment of uncomplicated acute illness due to influenza virus A and B in patients who have been symptomatic for no more than 2 days. • Two inhalations (10 mg total) twice daily for a period depending on indication. • Reports of neuropsychiatric events have been submitted. Notes from the lecture Suppurative diseases: Diseases which produce a large amount of purulent sputum. 1- Bronchectasis. 2- Lung abscess. 3- Empyema (pus in pleural cavity). Bronchectasis Permanent dilatation and destruction of bronchi and airways associated with irreversible damage of wall. It may be: Congenital: Deficiency of immunoglobulins or deficiency in mucocilliary escalator (immotile syndrome) Acquired: Occurs as a cause of cystic fibrosis which is a genetic disease with a defect in cilia and lung so favor infection. Treatment: 1- Physiotherapy and chest percussion. 2- Antibiotics to decrease incidence of infection due to increased mucus, pus and lung destruction. 3- Surgical treatment. In cases of: - Localized disease. - Severe hemoptysis. - Offensive sputum. Note: Accumulated experience with tobramycin and colistin indicates that bronchospasm can be a significant adverse effect. It can be prevented or resolved by inhaled bronchodilators but in some cases it precludes the use of aerosol antibiotics. Table 1—Indications for Aerosolized Antibiotics* Bacterial Infections Proven beneficial effects Suppressive therapy for Pseudomonas in CF patients Probably beneficial Mild exacerbations with Pseudomonas in CF patients Pseudomonas in patients with non-CF bronchiectasis Highly controversial with serious risks Ventilator-associated pneumonia No information but of potential benefit Ventilator tracheostomy–associated tracheobronchitis Chronic purulent bronchitis with Pseudomonas Other Infections Amphotericin B for Aspergillus spp after lung transplantation Pentamidine for Pneumocystis prophylaxis *CF = cystic fibrosis.