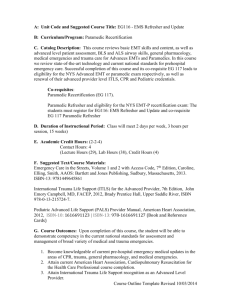
History - Georgetown County Fire/EMS
advertisement

THIS PAGE INTENTIONALLY LEFT BLANK PATIENT CARE PROTOCOLS AND STANDING ORDERS Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Table of Contents GENERAL PROTOCOLS Page 9 Universal Patient Care Protocol------------------------------------------------------- 10 Airway, ADULT---------------------------------------------------------------------------- 11 Airway, ADULT FAILED----------------------------------------------------------------- 12 Airway, PEDIATRIC---------------------------------------------------------------------- 13 Back Pain------------------------------------------------------------------------------------ 14 Behavioral----------------------------------------------------------------------------------- 15 Fever ---------------------------------------------------------------------------------------- 16 IV Access------------------------------------------------------------------------------------ 17 Pain Control--------------------------------------------------------------------------------- 18 MEDICAL PROTOCOLS Page 19 Abdominal Pain---------------------------------------------------------------------------- 20 Allergic Reaction--------------------------------------------------------------------------- 21 Altered Mental Status (AMS) ----------------------------------------------------------- 22 Asystole-------------------------------------------------------------------------------------- 23 Bradycardia, ADULT--------------------------------------------------------------------- 24 Cardiac Arrest------------------------------------------------------------------------------ 25 Chest Pain / Suspected Cardiac Event---------------------------------------------- 26 Dental Problems--------------------------------------------------------------------------- 27 Epistaxis------------------------------------------------------------------------------------- 28 Hypertension ----------------------------------------------------------------------------- 29 Hypotension Shock (Non-Trauma), ADULT---------------------------------------- 30 Overdose / Toxic Ingestion ------------------------------------------------------------- 31 Post Resuscitation------------------------------------------------------------------------ 32 Pulmonary Edema------------------------------------------------------------------------ 33 Pulseless Electrical Activity (PEA) ---------------------------------------------------- 34 Revised: 07/11/2011 M. Stover, MD 2 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control MEDICAL PROTOCOLS, Continued Respiratory Distress, ADULT------------------------------------------------------------ 35 Seizures, ADULT ---------------------------------------------------------------------- 36 Atrial Fibrillation / Atrial Flutter ------------------------------------------------------ 37 Supraventricular Tachycardia (SVT), ADULT Suspected Stroke Syncope ---------------------------------- 38 ---------------------------------------------------------------------- 39 ------------------------------------------------------------------------------- 40 Ventricular Fibrillation (VF) / Pulseless Ventricular Tachycardia ------------ 41 Ventricular Tachycardia (VT) Vomiting and Diarrhea ------------------------------------------------------ 42 --------------------------------------------------------------- 43 PEDIATRIC & OBSTETRIC (OB) PROTOCOLS Childbirth / Labor Page 44 ---------------------------------------------------------------------- 45 Newly Born ------------------------------------------------------------------------------- 46 Obstetrical (OB) Emergency Bradycardia, PEDIATRIC ------------------------------------------------------- 47 --------------------------------------------------------- 48 Head Trauma, PEDIATRIC -------------------------------------------------------- 49 Hypotension Shock (Non-Trauma), PEDIATRIC ------------------------------- 50 Multiple Trauma, PEDIATRIC ---------------------------------------------------- 51 Pulseless Arrest, PEDIATRIC ---------------------------------------------------- 52 Respiratory Distress, PEDIATRIC ---------------------------------------------------- 53 Seizures, PEDIATRIC ------------------------------------------------------------- 54 Supraventricular Tachycardia (SVT), PEDIATRIC TRAUMA PROTOCOLS Bites & Envenomations ------------------------- 55 Page 56 ------------------------------------------------------------- 57 Aquatic Life ------------------------------------------------------------------------------- 58 Burns ---------------------------------------------------------------------------------------- 69 Drowning / Near Drowning ------------------------------------------------------------- 60 Revised: 07/11/2011 M. Stover, MD 3 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control TRAUMA PROTOCOLS, Continued Electrical Injuries ---------------------------------------------------------------------- 61 Extremity Trauma ---------------------------------------------------------------------- 62 Head Trauma, ADULT ------------------------------------------------------------- 63 Hyperthermia ---------------------------------------------------------------------- 64 Hypothermia ---------------------------------------------------------------------- 65 Multiple Trauma, ADULT ------------------------------------------------------------- 66 Spinal Immobilization --------------------------------------------------------------- 67 WMD-Nerve Agent Protocol ---------------------------------------------------- 68 EMS TREATMENT & PATIENT CARE POLICIES------------------------Page 70 Air Transport -------------------------------------------------------------------------------- 71 Child Abuse Recognition & Reporting -------------------------------------------- 75 Criteria for Death / Withholding Resuscitation ----------------------------------- 76 Deceased Subjects ----------------------------------------------------------------------- 77 Discontinuation or Prehospital Resuscitation ----------------------------------- 78 Disposition / Patient Discharge Instructions (Refusal) -------------------------- 79 South Carolina DO NOT RESUSCITATE Form ----------------------------------- 80 Documentation of the Patient Care Report Documentation of Vital Signs ----------------------------------- 81 ----------------------------------------------------- 82 Domestic Violence (Partner and/or Elder Abuse) Recognition & Reporting- 83-84 Infant Abandonment ------------------------------------------------------------------- 85 Patient Without a Protocol -------------------------------------------------------------- 86 Physician on Scene ----------------------------------------------------------------------- 87 Poison Control Center ------------------------------------------------------------------ 88 Safe Transport of Children -------------------------------------------------------------- 89 Transport -------------------------------------------------------------------------------- 90 Revised: 07/11/2011 M. Stover, MD 4 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control PATIENT CARE PROCEDURES----------------------------------------------Page 91 Acute Myocardial Infarct / STEMI Patient-------------------------------------------- 92 12 Lead ECG ------------------------------------------------------------------------------- 93 Airway- Combitube ---------------------------------------------------------------------- 94 Airway- King LTD -------------------------------------------------------------------------- 95 Airway- LMA --------------------------------------------------------------------------------- 96 Airway- Intubation Confirmation, End Tidal CO2 Detector -------------------- 97 Airway- Nasotracheal Intubation -------------------------- ---------------------------- 98 Airway- Nebulizer Inhalation Therapy ------------------------------------------------ 99 Airway- Orotracheal Intubation ------------------------------------------------------- 100 Airway- Respirator Operation ---------------------------------------------------------- 101 Airway- Suctioning, Advanced --------------------------------------------------------- 102 Airway- Suctioning, Basic ---------- ---------------------------------------------------- 103 Airway- Ventilator PEEP/CPAP ------------------------------------------------ 104-105 Arterial Line Maintenance ------------------------------------------------------------ 106 Assessment, Adult ---------------------------------------------------------------------- 107 Assessment, Pediatric ------------------------------------------------------------------ 108 Blood Glucose Analysis ----------------------------------------------------------------- 109 Capnography ------------------------------------------------------------------------------ 110 Cardioversion ----------------------------------------------------------------------------- 111 Chest Decompression ------------------------------------------------------------------ 112 Childbirth ------------------------------------------------------------------------------------ 113 CNS Catheter- Epidural Maintenance ----------------------------------------------- 114 CNS Catheter- Ventricular Catheter Maintenance ------------------------------- 115 Cardiopulmonary Resuscitation (CPR) ---------------------------------------------- 116 Decontamination ------------------------------------------------------------------------- 117 Defibrillation- Manual ------------------------------------------- ------------------------ 118 Defibrillation- Automated --------------------------------------------------------------- 119 External Cardiac Pacing ----------------------------------------------------------------- 120 Injections- Subcutaneous (SQ), Intramuscular (IM) ------------------------------ 121 Revised: 07/11/2011 M. Stover, MD 5 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control PATIENT CARE PROCEDURES, Continued Military Anti-Shock Trouser (M.A.S.T.) -------------------------------------------- 122 Pain Assessment and Documentation --------------------------------------------- 123 Pulse Oximetry --------------------------------------------------------------------------- 124 Venous Access- Blood Draw ---------------------------------------------------------- 125 Venous Access- Central Line Maintenance --------------------------------------- 126 Venous Access- External Jugular Access ----------------------------------------- 127 Venous Access- Extremity ------------------------------------------------------------- 128 Venous Access EZ-IO -------------------------------------------------------------- 129-136 Venous Access- Intraosseous (IO), Pediatric --------------------------------- 137 Wound Care -------------------------------------------------------------------------------- 138 Restraints -------------------------------------------------------------------------------- 139 Spinal Immobilization Splinting -------------------------------------------------------------- 140 -------------------------------------------------------------------------- 141-142 Stroke Screening – L.A. Prehospital Stroke Scale Thrombolytic Screening -------------------------- 143 -------------------------------------------------------------- 144 APPENDICES----------------------------------------------------------------Page 145 APGAR Score ---------------------------------------------------------------------------- 146 Rule of Nines Burn Chart ------------------------------------------------------------- 147 Restraint Checklist Form ------------------------------------------------------------- 148 Los Angeles (L.A.) Prehospital Stroke Screening Form ----------------------- 149 Wong Baker Pain Scale------------------------------------------------------------------- 150 Pediatric Reference Chart --------------------------------------------------------- -151-152 Revised Trauma Score ------------------------------------------------------------------- 153 Glasgow Coma Score -------------------------------------------------------------------- 154 MEDICATION LIST ----------------------------------------------------------------Page 155 Adenosine (Adenocard) Revised: 07/11/2011 -------------------------------------------------------------- 156 M. Stover, MD 6 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR Albuterol EMT Intermediate Paramedic Medical Control ----------------------------------------------------------------------------------- 157 Amiodarone -------------------------------------------------------------------------- 158-159 Aspirin (ASA) ------------------------------------------------------------------------------ 160 Atropine ----------------------------------------------------------------------------- -161-162 Atrovent -------------------------------------------------------------------------------- -------163 Calcium Glucanate ---------------------------------------------------------------- ------164 D5W ----------------------------------------------------------------------------------------- 165 D50 ------------------------------------------------------------------------------------------ 166 Diazepam (Valium) ----------------------------------------------------------------- 167-168 Diltiazem (Cardizem) --------------------------------------------------------------------- 169 Diphenhydramine (Benadryl) ----------------------------------------------------------- 170 Dopamine ---------------------------------------------------------------------------------- 171 Epinephrine 1:1,000 ----------------------------------------------------------------- 172-173 Flumazenil (Romazicon) ------------------------------------------------------------ 174-175 Furosemide (Lasix) ---------------------------------------------------------------------- 176 Glucagon ------------------------------------------------------------------------------------ 177 Labetalol ------------------------------------------------------------------------------- 178-179 Lidocaine ------------------------------------------------------------------------------ 180-181 Magnesium Sulfate ----------------------------------------------------------------------- 182 Midazolam (Versed) Morphine Sulfate ------------------------------------------------------------- 183-184 ------------------------------------------------------------------ 185-186 Naloxone (Narcan) ---------------------------------------------------------------------- 187 Nitroglycerine ---------------------------------------------------------------------------- 188 Procainamide ---------------------------------------------------------------------- 189 Sodium Bicarbonate ----------------------------------------------------------190-192 Sodium Chloride (Normal Saline) ---------------------------------------------------- 193 Solumedrol (Methylprednisolone) ---------------------------------------------------- 193 Revised: 07/11/2011 M. Stover, MD 7 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Solumedrol --------------------------------------------------------------------------------- 194 Thiamine ----------------------------------------------------------------------------------- 195 Zofran --------------------------------------------------------------------------------------- 190 STANDARDS OF PRACTICE--------------------------------------------------Page 196 First Responder ------------------------------------------------------- 197 Emergency Medical Technician (EMT) ------------------------------------------- 198 Emergency Medical Technician- Intermediate (EMT-I) ----------------------- 199 Emergency Medical Technician- Paramedic (EMT-P) --------------------- 200-201 Revised: 07/11/2011 M. Stover, MD 8 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control General Protocols Revised: 07/11/2011 M. Stover, MD 9 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Universal Patient Care Protocol Scene Safety Primary Survey Ad. Vs. Ped. assessment (Broselow-Luten tape in pediatrics) Cardiac Arrest Airway Protocol Ad. / Ped. Cardiac Arrest Protocol Vital Signs w/ pulse oximetry (Temp if appropriate) P Refer to appropriate protocol Consider Cardiac Monitor w/ 12 lead M P B Blood Glucose B If patient does not fit into a protocol M CONTACT MEDICAL CONTROL Pearls: Any patient contact, which does not result in an EMS transport, must have a completed refusal form. Exam: Minimal exam if not noted on the specific protocol is vital signs, mental status, and location of injury or complaint. Required vital signs on every patient, per complaint, include blood pressure, pulse, respirations, pain / severity. Pulse oximetry and temperature documentation is dependant on the specific complaint. A pediatric patient is defined by the Broselow-Luten tape. If the patient does not fit on the tape, they are considered adult. Timing of transport should be based on patient’s clinical condition and the transport policy. Revised: 07/11/2011 M. Stover, MD 10 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Airway - ADULT Access ABC’s, Respiratory rate, Effort, Gag Reflex and SPO2 Adequate F R Pulse Oximetry F R Supplemental Oxygen indicated F R Basic Manual Maneuvers including O2 F R F R P M Nasotracheal Intubation P Obstructed Airway per AHA Guidelines F R Orotracheal Intubation F R P P F R P Digital Intubation P B BIAD B P Contact Medical M Control Consider Failed Airway Protocol M Pearls: F R Apnea or Absent Gag Reflex Positive Respirations or positive gag reflex F Nasopharyngeal Airway / R BVM Ventilations Obstructed Inadequate Contact Medical Control Direct P Laryngoscopy If capnography available, ventilate patient to maintain CO2 level between 35 and 45. M For this protocol, adult is defined as 12 years old or greater. Capnography is mandatory with all methods of intubation if available. Other secondary conformation devices will be used in the absence of capnograhy ie. End Tidal CO2 detector. Document results. Maintain C-spine immobilization for patients with suspected spinal injury. Do not assume hyperventilation is psychogenic – use oxygen, not a paper bag. Sellick’s maneuver should be used to assist with difficult intubations. Providers should consider using a BIAD (Blind Insertion Airway Device) when they are unable to intubate a patient. Hyperventilation in head trauma should only be used to maintain a pC02 of 30 – 35. Continuous pulse oximetry should be utilized in all patients with an inadequate respiratory function. Place all intubated patients in full spinal immobilization. (Inform the receiving RN and Physician as to the nature of the c-collar application- For TRAUMA or AIRWAY CONTROL ONLY; Assist with removal if requested by the receiving physician). Revised: 07/11/2011 M. Stover, MD 11 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Airway - Failed ADULT 2 Failed Intubation Attempts by most proficient technician on scene No more than 3 attempts F R SPO2 >90% with BVM No Yes If SPO2 <90% or if patient becomes difficult to ventilate F F Nasal / Oral Airway R R Facial Trauma or Swelling Yes F R Continue BVM P F R M F R Continue BVM F R No B Pearls: F R Digital Intubation BIAD Contact Medical Control P B If capnography available, ventilate patient to maintain CO2 level between 35 and 45. M If first intubation attempt fails, make an adjustment and then try again: (consider) * Different laryngoscope blade * Different ETT size * Change cricoid pressure * Apply BURP maneuver (Push trachea Back [posterior], up, and to patient’s right) * Change head positioning Continuous pulse oximetry or capnography should be utilized in all patients with an inadequate respiratory function. Notify Medical Control as EARLY AS POSSIBLE about the patient’s difficult / failed airway. Revised: 07/11/2011 M. Stover, MD 12 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Airway - PEDIATRIC Access ABC’s, Respiratory rate, Effort, Gag Reflex and Pulse Oximetry Adequate Obstructed Inadequate F Supplemental Oxygen R indicated F R F R Basic Maneuvers including O2 Positive Respirations or positive gag reflex F R F F R F R F R Apnea or Absent Gag Reflex Oxygenate, Ventilate, F Position, Reassess R Consider Early Rapid Transport F R P F R M Orotracheal Intubation P Direct Laryngoscopy F R P P F R Continue BVM Contact MCP Obstructed Airway per AHA Guidelines If capnography available, ventilate patient to maintain CO2 level between 35 and 45. M Pearls: For this protocol, pediatric is defined as less than 12 years. Capnography is mandatory with all methods of intubation if available. Other secondary conformation devices will be used in the absence of capnograhy ie, ETCO2 detector. Document results. Limit intubation attempts to 3 per patient. Back Pain If unable to intubate, continue BVM ventilations, transport rapidly, and notify receiving hospital early. Maintain C-spine immobilization for patients with suspected spinal injury. Do not assume hyperventilation is psychogenic – use oxygen, not a paper bag. Sellick’s maneuver should be used to assist with difficult intubations. Continuous pulse oximetry should be utilized in all patients with an inadequate respiratory function. All intubated patients will be placed in full spinal protocol. (Inform the receiving RN and Physician as to the nature of the c-collar application- For TRAUMA or AIRWAY CONTROL ONLY; Assist with removal if requested by the receiving physician). Revised: 07/11/2011 M. Stover, MD 13 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Back Pain History: Age Past Medical History Past Surgical History Medications Onset of pain/ injury Previous back injury Traumatic mechanism Location of pain Fever Improvement or worsening with activity Signs and Symptoms Differential Pain Swelling Pain with range of motion Extremity Weakness Extremity numbness Shooting pain into an extremity Bowel/ bladder dysfunction Muscle spasm/ sprain Herniated disc with nerve compression Sciatica Spine fracture Kidney stone Kidney infection Aneurysm Pneumonia Universal Patient Care Protocol Injury or traumatic mechanism Yes No Spinal F Immobilization R Protocol F R BP<90 regardless of postural position YES Signs of Shock I IV Protocol I No I Normal Saline Bolus I P Pain Control Protocol P M Pearls: No Contact Medical M Control Exam: Mental Status, HEENT, Neck, Chest, Lungs, Abdomen, Back, Extremities, Neuro Abdominal aneurysms are a concern in patients over the age of 50 Kidney stones typically present with an acute onset of flank pain which radiates around to the groin area. Patients with midline pain over the spinous processes should be placed in spinal immobilization. Any bowel or bladder incontinence is a significant finding, which requires immediate medical evaluation. If Spinal Immobilization is indicated and the patient refuses care, a Patient Refusal Form will be completed regardless of transport. Revised: 07/11/2011 M. Stover, MD 14 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Behavioral History: Situational crisis Psychiatric illness/ medications Injury to self or threats to others Medic alert tag Substance abuse/ overdose Diabetes Signs and symptoms: Anxiety, agitation, confusion Affect change, hallucinations Delusional thoughts, bizarre behavior Combative/ Violent Expression of suicidal/ homicidal thoughts Differential: Altered LOC differential ETOH Toxin/ Substance abuse Medication effect/ overdose Withdrawal symptoms Depression Bipolar Schizophrenia Anxiety Disorders Scene Safety Universal Patient Care Protocol Treat Suspected Medical or Trauma Problems Altered Mental Status, Overdose, Trauma Remove patient from stressful environment Verbal Techniques (reassurance, calm, establish rapport) B Restraint Procedure B M Contact Medical Control P Consider Valium 2-5mg M P Pearls: Exam: Mental Status, Skin, Heart, Lungs, Neuro Your Safety First!!!!!! Exam: Mental Status, Skin, Heart, Lungs, Neuro Be sure to consider all possible medical / trauma causes for behavior (hypoglycemia, overdose, substance abuse, hypoxia, head injury, etc.) Do not irritate the patient with a prolonged exam. Do not overlook the possibility of associated domestic violence or child abuse. Revised: 07/11/2011 M. Stover, MD 15 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Fever History: Age Duration/Severity of fever Past medical history Medications Immunocompromised Environmental exposure Last acetaminophen or ibuprofen and dosage Out of country travel within past 14 days Signs and Symptoms: Warm Flushed Sweaty Chills/ Rigors Associated Symptoms Myalgias, Cough, Chest pain, Headache, Dysuria, Abdominal pain, Mental status Changes Differential: Infections/ Sepsis Cancer Medication or Drug reaction Connective tissue disease Hyperthyroid Heat Stroke Universal Patient Care Protocol F BP <90 regardless of F R R postural position YES IV Protocol NS Bolus I Encourage PO Intake I F R Temperature >100 F Use methods in R PEARLS NO F R <100 F R Appropriate protocol by complaint M Contact Medical Control M Exam: Mental Status, Skin, HEENT, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro Febrile seizures are more likely in children with a history of febrile seizures and with a rapid elevation in temperature. Temperature may be decreased by a combination of 4 methods: 1. Radiation: Heat loss to air (unwrap or remove clothing) 2. Evaporation: Heat loss from the evaporation of sweat or liquid from the skin (tepid water bath to skin) 3. Convection: Heat loss from movement of air currents over the skin (increase air movement to skin) 4. Conduction: Heat loss from the contact with solid substances (with heat stroke use cool packs per protocol) Rehydration with fluids increases the patient’s ability to sweat and improves heat loss. Revised: 07/11/2011 M. Stover, MD 16 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control IV Access **Intraosseous infusion may be used in pediatric and adult patients deemed “critical” and venous access is required for fluid resuscitation or delivery of medications for resuscitation.** Universal Patient Care Protocol Access need for IV Emergent or potentially emergent medical or trauma I Peripheral IV External Jugular > 12 years old and life threatening Successful Reassess and monitor bolus M requires Medical M Control Order Intraosseous (ped or adult device) P EZ-IO P EJ < 12 yrs old I Unsuccessful M Contact Medical Control M Intraosseous with the appropriate device in life threatening events only where no obvious peripheral site is noted. Pediatric patients with life threatening events, consider IO as first access attempt. Any prehospital fluids or medications approved for IV administration may be given through an intraosseous IV. All IV rates should be at KVO (minimal rate to keep vein open) unless administering fluid bolus. External jugular and / or IO lines can be attempted initially in life threatening events where no obvious peripheral site is noted. Upper extremity IV sites are preferable to lower extremity sites. Lower extremity IV sites are contraindicated in patients with vascular disease or diabetes. In post-mastectomy patients, avoid IV, blood draw, injection, or blood pressure in arm on affected side. Revised: 07/11/2011 M. Stover, MD 17 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Pain Control U n iv e rs a l P a tie n t C a re P ro to c o l P a tie n t C a re B a s e d o n S p e c ific C o m p la in t P a in s e v e rity > 6 /1 0 No P a tie n t C a re B a s e d o n S p e c ific C o m p la in t Yes I IV P ro to c o l I C o n tra in d ic a tio n to s e d a tio n o r A b d o m in a l P a in ? No M M Yes P a tie n t C a re B a s e d o n S p e c ific C o m p la in t C o n ta c t M e d ic a l C o n tro l M o rp h in e S u lfa te A d u lt: 2 m g IV /IM q 3 -5 m in P a s n e e d e d fo r p a in U p to 1 0 m g T o ta l P M M P C o n s id e r Z o fra n a d u lt: 4 m g IV S lo w o v e r 2 m in u te s . P e d s: 0 .1 5 m g /k g IV P s lo w M ax dose of 4m g P Pearls: Exam: Mental Status, Area of Pain, Neuro Pain severity (0-10) is a vital sign to be recorded pre and post IV / IM / or PO medication delivery and at disposition. Vital signs should be obtained pre, 15 minutes post, and at disposition with all pain medications. Relative contraindications to Morphine use include hypotension, head injury, respiratory compromise or severe COPD, or known allergy. All patients should have drug allergies documented prior to administering pain medications. All patients who receive IM or IV medications must be observed 15 minutes for drug reaction. Revised: 07/11/2011 M. Stover, MD 18 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Medical Protocols Revised: 07/11/2011 M. Stover, MD 19 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Abdominal Pain History: Age Past Medical/ Surgical History Medications Onset Palliation/ Provocation Quality Region/ Radiation/ Referred Severity (1-10) Time (Duration/ repetition) Fever Last meal eaten Last bowel movement Menstrual history Signs and Symptoms: Pain Tenderness Nausea Vomiting Diarrhea Dysuria Constipation Vaginal bleeding/ Discharge Pregnancy Differential: Pneumonia or PE Liver Peptic ulcer disease Gallbladder MI Pancreatitis Kidney stone AAA Appendicitis Bladder/ Prostate disorder Pelvic Spleen enlargement Diverticulitis Bowel Obstruction Gastroenteritis Universal Patient Care Protocol I IV Protocol NaCl Bolus if Hypotensive I Nausea & Vomiting Consider Chest Pain Protocol I IV Protocol P Zofran Adult: 4mg IVP slow Peds: 0.15mg/kg IVP slow To max dose of 4mg I Consider Pain Control Protocol M Contact Medical Control P M Pearls: Required Exam: Mental Status, Skin, HEENT, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro. Document the mental status and vital signs prior to administration of Zofran. Abdominal pain in women of childbearing age should be treated as an ectopic pregnancy until proven otherwise. The diagnosis of abdominal aneurysm should be considered with abdominal pain in patients over 50. Appendicitis presents with vague, peri-umbilical pain which migrates to the RLQ over time. Revised: 07/11/2011 M. Stover, MD 20 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Allergic Reaction History: Onset and Location Insect sting or bite Food allergy/ exposure Medication allergy/ exposure New clothing, soap, detergent Past history of reactions Past medical history Medication history Signs and Symptoms: Itching and hives Coughing/ Wheezing or respiratory distress Chest or throat constriction Difficulty swallowing Hypotension or shock Edema Differential: Urticaria Anaphylaxis Shock Angioedema Aspiration/ Airway obstruction Vasovagal event Asthma/ COPD CHF Universal Patient Care Protocol Evidence of Impending Respiratory distress or shock? B Auto Injector Epi-Pen (Epi-Jr pen if < 12 y/o) Hives/ Rash Only No Respiratory Component B Diphenhydramine Adult: 25-50 mg IV/IM P Ped: 1 mg/kg IV/IM (Max Ped dose = 50 mg) Epinephrine 1:1,000 <50 y/o: 0.3-0.5mg SQ >50 y/o:MCP only Ped: 0.01 mg/kg SQ Max Ped dose 0.3mg P P P Reassess Patient Albuterol / if wheezing Adult:2.5-5.0mg via neb Ped: 2.5mg via neb May repeat up to 3x P P Diphenhydramine Adult: 50 mg IV/IM Ped: 1 mg/kg IV/IM (Max Ped dose = 50 mg) P Respiratory distress with evidence of increased work of breathing and / or wheezing. P Shock defined by tachycardia and or hypotension. P P IV / Cardiac Monitor If evidence of anaphylaxis Epinephrine 1:10,000 0.3 mg IV M Contact Medical Control M Exam: Mental Status, Skin, Heart, Lungs. Administering epinephrine in patients who are >50 years of age, or that have a history of cardiac disease, or if the patient’s heart rate is >150 may precipitate cardiac ischemia. These patients should receive a 12 lead ECG. May repeat Albuterol up to 3 times if no cardiac Hx and HR <150 ( HR < 200 in Peds) Any patient with respiratory symptoms or extensive reaction should receive IV or IM diphenhydramine. The shorter the onset from symptoms to contact, the more severe the reaction. EMT / I or EMT / B must receive medical control order prior to administration of epi pen unless patient has a prescription for same. Revised: 07/11/2011 M. Stover, MD 21 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Altered Mental Status History: Known diabetic Drugs Report of drug use Past medical history Medications Hx of trauma Signs/ Symptoms: Decreased mental status Change in baseline mental status Bizarre behavior Hypoglycemia Hyperglycemia Differential: Head trauma Infection CNS Thyroid Cardiac Shock Toxicologic Diabetes Acidosis/ Alkalosis Environmental exposure Pulmonary Electrolyte abnormality Psychiatric disorder Universal Patient Care Protocol F R Spinal Immobilization Protocol, If applicable Glucose <70 B Patient Conscious with intact gag reflex Oral Glucose I IV Protocol B Blood Glucose 12 Lead ECG If available P P I P Glucagon, if no IV Adult: 1 mg IM Ped > 3y/o 0.5mg IM Glucose >250 signs of dehydration P I Infant: 0.5g/kg of D25% P B P 50% Dextrose (D50%) Adult: 25 g IV I I Glucose 70- 250 B Consider Thiamine 100mg IM or slow IVP for suspected ETOH abuse F R Naloxone Adult:1 - 2 mg IV or IM for RR < 12 Ped: 0.1 mg/kg IV or IO Normal Saline Bolus P P NO Consider other causes: (Head Injury, Overdose, Stroke, Hypoxia) Refer to Appropriate Protocol Return to baseline? Yes Revised: M Contact Medical Control M Exam: Mental Status, HEENT, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro. Be aware of Altered Mental Status (AMS) presenting as a sign of an environmental toxin or HazMat exposure and protect personal safety. It is safer to assume hypoglycemia than hyperglycemia if doubt exists. Do not let alcohol confuse the clinical picture. Alcoholics frequently develop hypoglycemia. Low glucose (< 70), normal glucose (70 – 120), high glucose (>250)- These parameters are relative to the patients- if possible, try to ascertain patients normal glucose levels. Consider restraints for patient’s M. and/or personnel’s 07/11/2011 Stover, MD protection per the restraint procedure. If the patient is thought to have abused ETOH, administer Thiamine 100mg IM or slow IVP 22 I Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Asystole History: Past medical history Medications Events leading to arrest End stage renal disease Estimated downtime Suspected hypothermia Suspected overdose DNR or living will Signs and Symptoms: Pulseless Apneic No electrical activity on ECG Differential: Device error Medical or trauma Hypoxia Potassium (Hypo/ Hyper) Drug overdose Acidosis Hypothermia Death Universal Patient Care Protocol YES Criteria for Death? NO Withhold Resuscitation F R CPR 30:2 F R I IV & Airway Protocol I Epinephrine 1:10,000 IV/ET Adult: 1 mg q 3-5 min P Ped: 0.01 mg/kg IV/IO Max single dose 0.5 mg P Stop Resuscitation P YES P Criteria for discontinuation P P NO At any time Consider Sodium Bicarbonate Adult: 50 mEq IV Ped: 1mEq/kg IV or IO May repeat with half dose after 10 minutes P Return of spontaneous circulation M Contact Medical Control P M Go to Post Resuscitation Protocol Pearls: Exam: Mental Status Always confirm asystole in more than one lead. Consider underlying causes. Once patient is intubated, continue compressions at a rate of 100/minute Revised: 07/11/2011 M. Stover, MD 23 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Bradycardia, ADULT History: Past Medical history Medications o Beta blockers o Calcium channel blockers o Clonidine o Digitalis Pacemaker Signs and Symptoms: HR < 60BPM Chest pain Respiratory distress Hypotension/ Shock Altered LOC Syncope Differential: Acute MI Hypoxia Hypothermia Sinus Bradycardia Athletes Head injury or CVA Spinal cord lesion Sick Sinus Syndrome AV Blocks(1st , 2nd, 3rd Degree) Hypoglycemia Universal Patient Care Protocol P 12 Lead ECG if P available I IV Protocol I Symptomatic?= CP, RD, Hypotension w/ Signs of shock YES NO Monitor P M P Contact Medical Control Versed 2mg IV M Consider Sedation Atropine 0.5-1.0mg IV Repeat q 3-5 min Total Max 3 mg P External Pacing P P M Contact Medical Control M P Dopamine 5-20 mcg/kg/min IV Drip Titrate dosing to BP of 90mmHg P P Pearls: The use of Lidocaine in heart block can worsen bradycardia and lead to asystole and death. Pharmacological treatment of bradycardia is based upon the presence or absence of significant signs and symptoms (symptomatic vs. asymptomatic). If hypotension with signs of shock exists, treat ASAP. Revised: 07/11/2011 M. Stover, MD If blood pressure is adequate, monitor only. Avoid Atropine in second degree type II or third degree AV block. Sedation should take place as long as not contraindicated. For initial dose of versed consider decreased dose if B/P is 80-100mm/hg 24 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Cardiac Arrest History: Events leading to arrest Estimated downtime Past medical history Medications Existence of terminal illness Signs of lividity, rigor mortis DNR or Living will Signs and Symptoms: Unresponsive Apneic Pulselessness Differential: Medical vs. Trauma V-Fib vs. V-Tach Asystole PEA Universal Patient Care Protocol Criteria for Death? YES NO Withhold Resuscitation F R CPR F R F R AED Procedure F R P Assess Rhythm P At any time Return of spontaneous circulation Go to appropriate Protocol Go to Post Resuscitation Protocol Success is based on proper planning and execution. Procedures require space and patient access. Make room to work. Reassess airway frequently and with every patient move. Maternal Arrest – Treat mother per appropriate protocol with immediate notification to Medical Control and rapid transport. Follow current AHA recommendations. Revised: 07/11/2011 M. Stover, MD 25 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Chest Pain/ Suspected Cardiac Event History: Age Medications Past medical history Allergies Recent physical exertion Onset Palliation/ Provocation Quality Region Severity Time Signs and Symptoms: CP (Pain, pressure, aching, vice like tightness) Location (Substernal, epigastric, arm, jaw, neck, shoulder) Radiation of pain Pale, diaphoresis Shortness of breath Nausea, vomiting, dizziness Differential: Trauma vs. Medical Angina vs. MI Pericarditis PE Asthma/ COPD Pneumothorax Aortic dissection or aneurysm GE Reflux or Hiatial hernia Esophogeal spasm Chest wall injury Pleural pain Universal Patient Care Protocol P Aspirin 324mg P > 30 y/o 12 Lead ECG (if P available) transmit to ED I P P IV Protocol M P I Nitroglycerine Nitroglycerine if BP >110 > 100 Sys. if BP Sys. spray or or tab.SL 1 1spray tab. SL qq 55min min. Complete Thrombolytic Checklist IF STEMI IS NOTED FOLLOW STEMI PROTOCOL UNDER PATIENT PROCEDURES P Morphine 2mg IV q 3-5 min up to 10mg total MCP Only P Continue NTG and MS Therapy until pain is relieved as long as BP remains > 100 systolic P Consider Zofran adult: 4mg IV Slow over 2 minutes. P Peds: 0.15 mg/kg IVP slow P Max dose of 4mg P Contact Medical Control M Hypotension/ Dysrhythmias Treat per protocol Exam: Mental Status, Skin, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro. Avoid Nitro in patients who have used impotency (Viagra, Levitra and Cialis) medication in the past 48 hrs due to potential severe hypotension. If patient has taken nitroglycerin without relief, consider potency of the medication. If positive ECG changes, establish a second IV while en route to the hospital. Monitor for hypotension after administration of nitroglycerin and/or morphine. Revised: 07/11/2011 M. Stover, MD Diabetics and geriatric patients often have atypical pain, or only generalized complaints. Perform V4R if ST elevation noted in Lead II, III, and aVF. 26 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Dental Problems History: Age Past medical history Medications Onset of pain/ injury Trauma Location of tooth Whole vs. partial injury Signs and Symptoms: Bleeding Pain Fever Swelling Tooth missing or fractured Differential Decay Infection Fracture Avulsion Abscess Facial Cellulitis Impacted tooth TMJ Syndrome MI Universal Patient Care Protocol F Control Bleeding with R Pressure F R Tooth Avulsion YES Place tooth in milk or Normal Saline NO Pain Control Protocol Reassess and Monitor M Contact Medical Control M Significant soft tissue swelling to the face or oral cavity can represent a cellulites or abscess. Scene and transport times should be minimized in complete tooth avulsions. Reimplantation is possible within 4 hours if the tooth is properly cared for. All tooth disorders typically need antibiotic coverage in addition to pain control. Occasionally cardiac chest pain can radiate to the jaw. All pain associated with teeth should be associated with a tooth which is tender to tapping or touch (or sensitivity to cold or hot). Revised: 07/11/2011 M. Stover, MD 27 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Epistaxis History: Age Past medical history Medications Previous episodes Trauma Duration of bleeding Quantity of bleeding Signs and Symptoms: Bleeding from nasal passage Pain Nausea Vomiting Differential: Trauma Infection Allergic rhinitis Lesions Hypertension Universal Patient Care Protocol F R Ice Packs Compress Nostrils Tilt Head Forward F R I IV Protocol I BP < 90mm/hg and lungs clear No Consider Hypertension Protocol Yes I Normal Saline Bolus M I Contact Medical Control M Exam: Mental Status, HEENT, Heart, Lungs, Neuro. It is very difficult to quantify the amount of blood loss with epistaxis. Bleeding may also be occurring posteriorly. Evaluate for posterior blood loss by examining the posterior pharynx. Anticoagulants include Aspirin, Coumadin, non-steroidal anti-inflammatory medications (ibuprofen), and many over the counter headache relief powders. Revised: 07/11/2011 M. Stover, MD 28 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Hypertension History: Documented hypertension Related diseases (Diabetes, CVA, Renal failure, cardiac) Medications Pregnancy Signs and symptoms: One of these: Systolic BP >200 Diastolic BP >120 AND at least one of these: Headache Nosebleed Blurred vision Dizziness Differential: Hypertensive encephalopathy Primary CNS injury MI AAA Pre-eclampsia/ Eclampsia Universal Patient Care Protocol M I IV Protocol I P 12 Lead ECG If Available P Contact Medical Control M Symptomatic Patient P Asymptomatic Patient Consider Labetolol 10-20 mg IV slow (over 2 minutes) MCP Only P Continue Monitoring Continue Monitoring Pearls: Avoid Nitro in patients who have used impotency medication (Viagra, Levitra and Cialis) in the past 48 hrs due to potential severe hypotension. Never treat elevated BP based on one set of vital signs Symptomatic hypertension is typically revealed through end organ damage to the cardiac, CNS or renal systems. All symptomatic patients with hypertension should be transported with their head elevated. Revised: 07/11/2011 M. Stover, MD 29 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Hypotension Shock (Nontrauma), ADULT History: Signs and Symptoms: Restlessness/ Confusion Weakness/ Dizziness Weak rapid pulse Pale, cool clammy skin Delayed capillary refill Hypotension Coffee-ground emesis Tarry stools Blood loss Fluid loss Infection Cardiac ischemia Medications Allergic reaction Pregnancy Differential: Shock Hypovolemic, Cardiogenic, Septic, Neurogenic,, Anaphylactic Ectopic pregnancy Dysrhythmias PE Tension pneumothorax Medication effect Vasovagal Physiologic Universal Patient Care Protocol I Non Cardiac Non Trauma I Normal Saline Bolus IV Protocol I Cardiac Trauma I I M P Treat per appropriate cardiac protocol Treat per appropriate trauma protocol Contact Medical Control Consider Dopamine 5-20 mcg/kg/min titrate to systolic BP of 90 = mm/Hg No rales present I consider fluid bolus M P Pearls: Exam: Mental Status, Skin, Lung, Heart, Abdomen, Back, Extremities, Neuro Hypotension can be defined as a systolic blood pressure of less than 100. Consider all possible causes of shock and treat per appropriate protocol. Revised: 07/11/2011 M. Stover, MD 30 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Overdose/ Toxic Ingestion History: Ingestion or suspected ingestion of a potentially toxic substance Substance ingested, route, quantity Time of Ingestion Reason (Suicidal, accidental, criminal) Available medications in home Past medical history B Blood Glucose I IV Protocol Narcotic Overdose w/resp. depression Tricyclic Overdose P P Naloxone Adult: 2mg IV/IM Peds: 0.1 mg/kg IV / IO M Contact Medical Control B I Organophosphates Carbamates Contact Medical Control M P P Contact M M Medical Control Differential: Tricyclic antidepressants Acetaminophen Depressants Stimulants Anticholinergic Cardiac medications Solvents, Alcohols, Cleaning agents Insecticides Universal Patient Care Protocol ALWAYS CONSIDER CONTACTING POISON CONTROL WHENEVER NECESSARY Sodium Bicarbonate P Adult: 50 mEq IV + 100mEq in 1,000ml NaCl at 200 ml/hr Signs and Symptoms: Mental status changes Hypotension/ Hypertension Decreased respiratory rate Tachycardia, dysrythmias Seizures Atropine 1-2 mg IV/IM M Other Hypotension Seizures Dysrythmias Altered LOC M P M Contact Medical Control M Appropriate Protocol Pearls: Exam: Mental Status, Skin, HEENT, Lung, Heart, Abdomen, Extremities, Neuro Do not rely on patient history of ingestion, especially in suicide attempts. Bring bottles, contents, emesis to ED. Tricyclic: 4 major areas of toxicity: seizures, dysrhythmias, hypotension, decreased mental status or coma; rapid progression from alert mental status to death. TCA examples: amitriptyline (Elavil), ,desipramine, imipramine, nortriptyline. Acetaminophen: If not detected and treated, causes irreversible liver failure. Depressants: decreased HR, decreased BP, decreased temp., decreased respirations, non-specific pupils. Stimulants: increased HR, increased BP, increased temperature, dilated pupils, seizures. Anticholinergic: increased HR, increased temperature, dilated pupils, mental status changes. Cardiac Meds: dysrhythmias and mental status changes. Solvents: nausea, vomiting, and mental status changes. Insecticides: increased or decreased HR, increased secretions, nausea, vomiting, diarrhea, pinpoint pupils. Consider restraints if necessary for patient’s and/or personnel’s protection per the Restraint procedure Revised: 07/11/2011 M. Stover, MD Poison Control 1-800-222-1222 31 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Post Resuscitation History: Respiratory Arrest Cardiac Arrest Signs/ Symptoms: Return of pulse Differential: Continue to address specific differentials associated with the original dysrhythmia Repeat Primary Assessment F R Continue Ventilatory Support with 100% Oxygen I P F R I Pulse Oximetry IV Protocol F R I 12 lead ECG Transmit to ED if Available F R F R Vital Signs P Capnography If Available P F R P Hypotension? Ventricular Ectopy Bradycardia Consider Fluid Bolus Amiodarone 150mg IV over 10 min IV Drip at 1 mg/min P P Peds:5mg/kg over 20-60min Repeat 5mg/kg Max 15mg/kg Treat per Bradycardia Protocol I Consider Dopamine P 5-20 mcg/kg/min P titrate to BP of = 90 mmHg If Arrest Recurs Revert to Appropriate Protocol M Contact Medical Control M Pearls: Exam: Mental Status, Skin, Neck, Lungs, Heart, Abdomen, Extremities, Neuro Most patients immediately post resuscitation will require ventilatory assistance. The condition of post-resuscitation patients fluctuates rapidly and continuously, and they Revised: 07/11/2011 M. Stover, MD require close monitoring. Appropriate post-resuscitation management can best be planned in consultation with medical control. 32 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Pulmonary Edema History: Congestive heart failure Past medical history Medications Cardiac History Signs/ Symptoms: Respiratory distress, bilateral rales Apprehension, orthopnea Jugular vein distention Pink frothy sputum Peripheral edema, diaphoresis Hypotension, shock Chest Pain Differential: Myocardial Infarction Congestive heart failure Asthma and/or COPD Anaphylaxis Aspiration Pleural effusion Pneumonia Pulmonary embolus Pericardial tamponade Universal Patient Care Protocol P CPAP Procedure P P P Nitroglycerine if BP >100 I IV Protocol P I Furosemide 40mg / double daily dose up to 80 mg IV Total 12 Lead ECG If Available P Symptoms Resolved P P Symptoms Persist M Contact Medical Control Reassess and Monitor P M Pearls: Contact Medical Control M Morphine 2 mg IV, then 2 mg IV q3-5 min up to 10mg total Consider Zofran P Exam: Mental Status, Skin, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro Avoid Nitro in any patient who has used impotency medication in the past 48 hours due to possible severe hypotension. If patient has taken nitroglycerin without relief, consider potency of the medication. Concerns with Morphine include severe COPD and respiratory distress. Monitor the patient closely. Consider myocardial infarction in all these patients. Diabetics and geriatric patients often have atypical pain, or only generalized complaints. Careful monitoring of level of consciousness, BP, and respiratory status with treatments is essential. Allow the patient to be in their position of comfort to maximize their breathing effort. Revised: 07/11/2011 M. Stover, MD M 33 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Pulseless Electrical Activity (PEA), ADULT History: Past medical history; Medications Events leading to arrest End stage renal disease Estimated downtime Suspected hypothermia; Overdose Tricyclics, Digitalis, Beta blockers, Calcium channel blockers DNR/DNAR or Living will AT ANY TIME Return of spontaneous circulation Go to post resuscitation protocol Signs/ Symptoms: Pulseless Apneic Electrical activity on ECG Differential: Hypovolemia Cardiac tamponade Hypothermia Drug Overdose Massive MI Hypoxia Tension pneumothorax Pulmonary embolus Acidosis Hyper/ hypokalemia Universal Patient Care Protocol P F R CPR F R I IV and Airway Protocol I Epinephrine 1:10,000 1 mg q 3-5 min CONSIDER CAUSES EARLY IN ALL PEA PATIENTS P I Consider Fluid Bolus I I Consider 25 g of D50 If BG < 70 I Thiamine 100mg prior to D50 For Suspected ETOH Abuse P P Consider: Calcium Glucanate: 5-20ml slow IVP P Sodium Bicabonate: 50 mEq May repeat at half dose in 10 min P Dopamine: 5-20 mcg/kg/min titrate to systolic BP of 90 mmHg Chest Decompression P Criteria for Discontinuation NO M Pearls: Contact Medical Control P YES M P Stop Resuscitation Exam: Mental Status. Consider each possible cause listed in the differential: Survival is based on identifying and correcting the cause!!!!! Discussion with Medical Control can be a valuable tool in developing a differential diagnosis. Atropine may be of benefit in the presence of a brady or relative bradycardic rate. For Dialysis patients consider Calcium Glucanate early. Revised: 07/11/2011 M. Stover, MD 34 P Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Respiratory Distress, History: Asthma/ COPD CHF Home treatment Medications Toxic exposure Signs / Symptoms: Shortness of breath Pursed lip breathing Decreased ability to speak Increased respiratory rate Wheezing, rhonchi Use of accessory muscles Fever, cough Tachycardia Medical Control ADULT Differential: Asthma Anaphylaxis Aspiration COPD Pleural effusion Pulmonary embolus Inhaled toxin Pneumonia Pneumothorax Cardiac Pericardial tamponade Hyperventilation Universal Patient Care Protocol I IV Protocol I Rales/ Signs of CHF Wheezes Pulmonary Edema Protocol P Albuterol 2.5 mg + Atrovent 0.02 % 500 mcg P M Solu-Medrol 125 mg IV Contact Medical Control P P M Pearls: Exam: Mental Status, HEENT, Skin, Neck, Lung, Heart, Abdomen, Extremities, Neuro. Pulse oximetry should be monitored continuously if initial saturation is ≤96%, or there is a decline in patient’s status despite normal pulse oximetry readings. Status asthmaticus – severe prolonged asthma attack unresponsive to therapy – life threatening!!! Albuterol may be repeated up to 3 times if no cardiac history and HR < 150 bpm.. A silent chest in respiratory distress is a pre-respiratory arrest sign. Use capnography if available. Revised: 07/11/2011 M. Stover, MD 35 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Seizure, ADULT History: Reported/ witnessed seizure activity Previous seizure history Medic Alert bracelet Seizure medication History of trauma History of diabetes History of pregnancy Signs and symptoms: Decreased mental status Sleepiness Incontinence Observed seizure activity Evidence of trauma Differential: CNS Trauma Tumor Metabolic problem Hypoxia Electrolyte abnormality Drugs and/or Infection ETOH Withdrawal Eclampsia Stroke Hyperthermia Universal Patient Care Protocol F R Spinal Immobilization Protocol F R Status Epilepticus Focused HX and physical exam Postictal I IV Protocol I Airway Protocol B I IV Protocol Blood Glucose B I >70 P Seizure Recurs? Valium 5mg IV/IM/IO or PR P may repeat after 10 minutes Valium 5mg IV/IM/IO or PR may repeat after 10 minutes P (if sz persists contact medical control) M Pearls: < 70 Contact Medical Control I P M 50% Dextrose 25 grams IV or Glucagon 1mg IM if no IV access I Thiamine 100mg prior to P D50 for suspected ETOH abuse P Exam: Mental Status, HEENT, Lungs, Heart, Extremities, Neuro. Status epilepticus is defined as two or more successive seizures without a period of consciousness or recovery. This is a true emergency requiring rapid airway control, treatment, and transport. Grand mal seizures (generalized) are associated with loss of consciousness, incontinence, and tongue trauma. Focal seizures (petit mal) effect only a part of the body and are not usually associated with a loss of consciousness. Jacksonian seizures are seizures which start as a focal seizure and become generalized. Be prepared for airway problems and continued seizures. Assess for occult trauma and/or substance abuse. 07/11/2011 Stover, MD Be Revised: prepared to assist ventilations especially if Valium M. is used. For any seizure in a pregnant patient, follow the OB Emergencies Protocol. 36 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Atrial Fibrillation / Atrial Flutter Signs and Symptoms: History: Medications Diet Drugs Past medical history History of palpitations Syncope HR > 150 QRS < .12 Sec Dizziness Chest Pain Resp. Distress Differential: Heart Disease Sick sinus syndrome Myocardial infarction Exertion Pain Emotional Stress Fever Universal Patient Care Protocol Hx of WPW M Contact Medical M Control I 12 Lead ECG if available I Unstable/ Symptomatic M Contact Medical Control M P Contact Medical Control Sedate with Versed 2 mg P P M IV Protocol Stable/Symptomatic Stable/Asymptomatic P Differential Cont: Hypoxia Hypovolemia Drug overdose Hyperthyroidism Pulmonary embolus Electrolyte imbalance M P Cardizem 0.25 mg/kg SLOW IV; may repeat with 0.35 mg/kg after 15 min. MCP ONLY After Rate Control 12 lead ECG if available P (MCP Orders Only) P P P P M Cardioversion 100 Joules P Repeat Cardioversion 200j, 300j, 360j P Contact Medical Control M Perform 12 Lead on all suspected all A-Fib/A-Flutter Patients Pearls: Adenosine may not be effective in identifiable atrial flutter/fibrillation, yet is not harmful. Monitor for hypotension after administration of Cardizem Monitor for respiratory depression and hypotension associated with Versed. Continuous pulse oximetry is required for all Atrial Fibrillation/ Atrial Flutter Patients. Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention. Revised: 07/11/2011 M. Stover, MD 37 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Supraventricular Tachycardia (SVT), ADULT History: Medications Diet Drugs Past medical history History of palpitations Syncope Signs and Symptoms: HR > 150 QRS < .12 Sec Dizziness Chest Pain SOB Differential: Heart Disease Sick sinus syndrome Myocardial infarction Exertion Pain Emotional Stress Fever Contact Medical M Control I IV Protocol I Stable Unstable P 12 Lead ECG If available P P Vagal Maneuver P P P P Cardioversion 100 Joules P P Repeat Cardioversion 200j, 300j, 360j P P P M Sedate with Versed 2 mg P Adenosine 6mg Rapid IV Push, 12mg Rapid IV, 12mg Rapid IV P Hypoxia Hypovolemia Drug overdose Hyperthyroidism Pulmonary embolus Electrolyte imbalance Universal Patient Care Protocol Hx of WPW M Contact Medical Control M Cardizem 0.25 mg/kg SLOW IV; may repeat with 0.35 mg/kg after 15 min. P M P Adenosine 6mg Rapid IV Push, 12mg Rapid IV,12mg Rapid IV P Contact Medical Control M Cardizem 0.25 mg/kg SLOW IV; may repeat with 0.35 mg/kg after 15 min. P Pearls: Exam: Mental Status, Skin, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro Adenosine may not be effective in identifiable atrial flutter/fibrillation, yet is not harmful. Monitor for respiratory depression and hypotension associated with Versed. Continuous pulse oximetry is required for all SVT patients. Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention. Approved vagal maneuvers include coughing, straining as if attempting a bowel movement. Carotid sinus massage is not approved Unstable patients may require immediate Cardioversion without IV or sedation Revised: 07/11/2011 M. Stover, MD 38 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Suspected Stroke History: Previous CVA or TIA’s Previous cardiac or vascular surgery Associated diseases (HTN, DM, CAD) Atrial fibrillation Medications History of trauma Signs and Symptoms: Altered mental status Weakness/ Paralysis Blindness or other sensory loss Aphasia/ Dysarthria Syncope Vertigo Vomiting Headache Seizures Respiratory pattern change Hypertension/ hypotension Differential: See Altered LOC TIA Seizure Hypoglycemia Stroke o Thrombotic o Embolic o Hemorrhagic Tumor Trauma Universal Patient Care Protocol I IV Protocol I B Blood Glucose B <70 50% Dextrose I 12-25 grams IV Glucagon P 1mg IM if no IV P >70 I P Thiamine 100mg IV prior to D50 if suspected ETOH P P M LA Prehospital Stroke Scale P Contact Medical Control M Consider Causes Altered LOC Hypertension Seizure Pearls: Exam: Mental Status, HEENT, Lung, Heart, Abdomen, Extremities, Neuro. Thrombolytic Screening Checklist should be completed for any suspected stroke patient. With duration of symptoms of less than 3 hours, scene times and transport times should be minimized. Onset of symptoms is the last witnessed time the patient was symptom free (i.e. awakening with stroke symptoms would be defined as an onset time of the previous night when patient was symptom free). The differential listed on the Altered Mental Status Protocol should also be considered. Elevated blood pressure is commonly present with stroke. Consider treatment if diastolic is > 120mmhg. Be alert for airway problems (swallowing difficulty, vomiting). Hypoglycemia can present as a localized neurologic deficit, especially in the elderly. Revised: 07/11/2011 M. Stover, MD 39 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Syncope History: Cardiac history, stroke, seizure Occult blood loss (GI, eptopic) Females: LMP, vaginal bleeding Fluid loss: nausea, vomiting, diarrhea Past Medical History Medications Signs and Symptoms: Loss of consciousness with recovery Lightheadedness, dizziness Palpitations, slow or rapid pulse Pulse irregularity Decreased blood pressure Differential: Vasovagal Orthostatic hypotension Cardiac syncope Micturation/defecation syncope Psychiatric Stroke or Seizure Hypoglycemia Shock (see Shock Protocol) Toxicologic (Alcohol) Medication effect (HTN) Universal Patient Care Protocol Suspected Trauma YES F R NO P Cardiac Monitor Spinal Immobilization Protocol F R AT ANY TIME P If relevant signs / symptoms are found go to appropriate protocol. I IV Protocol I B Blood Glucose B Dysrhythmia Hypotension Altered Mental Status <70 >70 P P M Pearls: Revised: 12 Lead ECG I 50% Dextrose 25 grams I P If no IV access, Glucagon 1 mg IM P Thiamine 100mg IV prior to D50 if suspected ETOH abuse P P Contact Medical Control M Exam: Mental Status, Skin, HEENT, Lungs, Heart, Abdomen, Back, Extremities, Neuro. Assess for signs and symptoms of trauma if associated or questionable fall with syncope. Consider dysrhythmias, GI bleed, ectopic pregnancy, & seizure as possible cause of syncope. These patients should be transported. 07/11/2011 Stover, MD based. More than 25% of geriatric syncope is M. cardiac dysrhythmia If patient is suspected of ETOH abuse always administer Thiamine IVP before D50 40 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Ventricular Fibrillation/ Pulseless V-Tach History: Signs and Symptoms: Unresponsive, apneic, pulseless Ventricular fibrillation or ventricular tachycardia on ECG Estimated down time Past medical history Medications Events leading to arrest Renal failure / dialysis DNR or living will Cardiac Arrest Protocol For defibrillation purposes, all energy settings are set for Biphasic waveform patterns. If Monophasic monitor is present start with energy setting at 360 J. Defibrillate At 200 J Biphasic P I P P IV / Airway Protocol P Defibrillate At 360 J Biphasic Criteria to Discontinue NO P P P If rhythm converts P start Amiodarone Drip P P YES P Discontinue P P Consider Lidocaine 1.5mg/kg P P May repeat twice at .75mg/kg M I Defibrillate At 300 J Biphasic Amiodarone 150mg P P x1 Defibrillate Reminder: Continuous High Quality CPR Amiodarone 300mg Rapid P IVP P P P Epinephrine 1:10,000 1mg q 5 Min P At any time Return of spontaneous circulation Go to Post Resuscitation Protocol Differential: Asystole Artifact / Device failure Cardiac Endocrine / Metabolic Drugs Pulmonary Contact Medical Control P If Torsades is suspected Consider Mag Sulfate 1-2g IV P M Pattern should be CPR drug-shock, CPR, drug-shock, etc..(repeat drugs as per drug list). Reassess and document endotracheal tube placement and ET CO2 frequently, after every move, and at discharge. If defibrillation is successful and patient re-arrests, return to previously successful energy level. Calcium if hyperkalemia is suspected (renal failure, dialysis). Defibrillation takes precedence over all treatment once the defibrillator is available. Revised: 07/11/2011 M. Stover, MD If Defibrillation is underway by First Responders (FR), FR defibrillation should continue until 6 defibrillations are accomplished or patient is resuscitated. Polymorphic V-Tach (Torsades de Pointes) may benefit from magnesium sulfate IV. 41 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Ventricular Tachycardia w/ a Pulse History: Past medical history / medications, diet, drugs. Syncope / near syncope Palpitations Pacemaker Allergies: lidocaine / novacaine Signs and Symptoms: Ventricular tachycardia on ECG (Runs or sustained) Conscious, rapid pulse Chest pain, shortness of breath Dizziness Rate usually 150 – 180 bpm for sustained VTach Differential: Artifact / Device failure Cardiac Endocrine / Metabolic Drugs Pulmonary Universal Patient Care Protocol I IV Protocol I P 12 Lead ECG If available P Stable P Amiodarone 150mgIV over 10 min Persistant VT Repeat x1 P Start Drip @ 1mg/min if conversion P Consider Lidocaine, 1.5mg/kg M Contact Medical Control P M Unstable Sedate with Versed 2 mg IV P P P Cardioversion 100j, 200j, 300j, 360j P Amiodarone 150mg IV over 10 min P Persistant VT Repeat x1 P Start Drip @1mg/min if conversion P M Consider P Lidocaine, 1.5mg/kg Contact Medical Control M Pearls: Exam: Mental Status, Skin, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro. For witnessed / monitored ventricular tachycardia, try having patient cough. Polymorphic V-Tach (Torsades de Pointes) may benefit from the administration of magnesium sulfate. Stover, MDwithout an IV or sedation. Revised: Unstable07/11/2011 patients may require immediateM. Cardioversion 42 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Vomiting and Diarrhea History: Age Time of last meal Last bowel movement/emesis Improvement or worsening with food or activity Duration of problem Other sick contacts Past medical history Past surgical history Medications Menstrual history (pregnancy) Travel history Bloody emesis / diarrhea Signs and Symptoms: Pain Character of pain (constant, intermittent, sharp, dull, etc.) Distention Constipation Diarrhea Anorexia Radiation Associated symptoms: (helpful to localize source) Fever, headache, blurred vision, weakness, malaise, myalgias, cough, dysuria, mental status changes,rash Differential: CNS (increased pressure, headache, stroke, CNS lesions, trauma or hemorrhage, vestibular) Myocardial infarction Drugs (NSAID’s, antibiotics, narcotics, chemotherapy) GI or Renal disorders Diabetic ketoacidosis Gynecologic disease (ovarian cyst, PID) Infections (pneumonia, influenza) Electrolyte abnormalities Food or toxin induced Medication or Substance abuse Pregnancy Psychological Universal Patient Care Protocol Symptomatic I IV Protocol w/ bolus B Blood Glucose B F R BP< 90 F R Asymptomatic I Vomiting? P Zofran adult: 4mg IV Slow over 2 minutes. Peds: 0.15 mg/kg IVP slow Max dose of 4mg M Contact Medical Control P M Pearls: Exam: Mental Status, Skin, HEENT, Neck, Lungs, Heart, Abdomen, Back, Extremities, Neuro Document the mental status and vital signs prior to administration of Zofran. Revised: 07/11/2011 M. Stover, MD 43 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Pediatric And OB Protocols Revised: 07/11/2011 M. Stover, MD 44 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Childbirth/ Labor History: Due date Time contractions started / how often. Rupture of membranes Time / amount of any vaginal bleeding Sensation of fetal activity Past medical and delivery history Medications Signs and Symptoms: Spasmotic pain Vaginal discharge or bleeding Crowning or urge to push Meconium Differential: Abnormal presentation Buttock Foot Hand Prolapsed cord Placenta previa Abruptio placenta Universal Patient Care Protocol Left Lateral Position Hypertension Abnormal Vaginal Bleeding? YES NO Obstetrical Emergencies Protocol Inspect Perineum < 36 WEEKS GESTATION CROWNING ABNORMAL PRESENTATION SEVERE VAGINAL BLEEDING MULTIPLE GESTATIONS RAPID TRANSPORT IS INDICATED No Crowning Crowning PRIORITY SYMPTOMS: I IV Protocol I Monitor If prolapsed cord Knee to chest position Push up on head Newly Born Protocol M Contact Medical M Control Pearls: Exam: (Of Mother) Mental Status, Lungs, Heart, Abdomen, Neuro. Document all times (delivery, contraction frequency, and length). If maternal seizures occur, refer to the Obstetrical Emergencies Protocol. After delivery, massaging the uterus (lower abdomen) will promote uterine contraction and help to control post-partum bleeding. Some perineal bleeding is normal with any childbirth. Large quantities of blood or free bleeding are abnormal. Revised: 07/11/2011 M. Stover, MD 45 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Newly Born History: Due date and gestational age Multiple gestation (twins etc.) Meconium Delivery difficulties Congenital disease Medications (maternal) Maternal risk factors: substance abuse, smoking Paramedic Medical Control (Broselow Tape) Signs and Symptoms: Respiratory distress Peripheral cyanosis or mottling (normal) Central cyanosis (abnormal) Altered level of responsiveness Bradycardia Differential: Airway failure Secretions Respiratory drive Infection Maternal medication effect Hypovolemia Hypoglycemia Congenital heart disease Hypothermia Universal Patient Care Protocol Meconium in Amniotic Fluid YES NO Airway Suction Dry Warm Bulb suction mouth/nose Stimulate Note APGAR Score Respirations Present? No F R Yes BVM 40- 60 per minute F R Reassess Frequently Heart Rate <60 bpm 60- 100 bpm >100 bpm Pediatric Airway Protocol Pediatric Airway Protocol Monitor and Reassess HR >100 F R CPR F R I IV Protocol I Reassess Heart Rate Continue Oxygen HR 80-100 I I Dextrose 10% IV/IO Fluid Bolus I I M Pearls: IV Protocol Contact Medical Control M Exam: Mental Status, Skin, HEENT, Neck, Chest, Heart, Abdomen, Extremities, Neuro. Maternal sedation or narcotics will sedate infant (Naloxone effective). Consider hypoglycemia in infant Document 1 and 5 minute APGAR scores (see appendix). Consider Narcan 0.1 mg/kg IV / IO if known or suspected substance abuse by mother. Revised: 07/11/2011 M. Stover, MD 46 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Obstetrical Emergency History: Past medical history Hypertension meds Prenatal care Prior pregnancies / births Gravida / Para Signs and Symptoms: Vaginal bleeding Abdominal pain Seizures Hypertension Severe headache Visual changes Edema of hands and face Differential: Pre-eclampsia / Eclampsia Placenta previa Placenta abruptio Spontaneous abortion Universal Patient Care Protocol I IV Protocol I Vaginal Bleeding? Abdominal Pain? Yes Hypertension Left Lateral Position M Known Pregnancy Missed Period Yes F BP< 90 Regardless F R of Position R Contact Medical M Control Yes No B Blood Glucose B I Fluid Bolus Seizure or seizure like activity Magnesium Sulfate 2 gr over 2min IV Infusion P P Valium 5mg IVP P Quiet Rapid Transport Pearls: Abdominal Pain Protocol I Left Lateral Position if 3rd trimester No P No M Contact Medical M Control Exam: Mental Status, Lung, Heart, Abdomen, Neuro. Severe headache, vision changes, or RUQ pain may indicate pre-eclampsia. In the setting of pregnancy, hypertension (HTN) is defined as a BP greater than 140 systolic or greater than 90 diastolic, or a relative increase of 30 systolic and 20 diastolic from the patient’s normal (pre-pregnancy) blood pressure. Maintain patient in a left lateral position to minimize risk of supine hypotension syndrome. Ask patient to quantify bleeding – number of pads used per hour. Any pregnant patient involved in a MVA should be seen immediately by a physician for evaluation and fetal monitoring. For any hypoglycemic patient suspected of abusing ETOH, always administer 100 mg Thiamine before D50W. Revised: 07/11/2011 M. Stover, MD 47 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Bradycardia, PEDIATRIC History: Past Medical History Foreign body exposure Respiratory distress or arrest Apnea Possible toxic or poison exposure Congenital disease Medication (maternal or infant) Medical Control (Broselow Tape) Signs and Symptoms: Decreased heart rate Delayed capillary refill or cyanosis Mottled, cool skin Hypotension or arrest Altered level of consciousness Differential: Respiratory effort Respiratory obstruction Foreign body / Secretions Croup / Epiglotitis Hypovolemia Hypothermia Infection / Sepsis Medication or Toxin Hypoglycemia Trauma Universal Patient Care Protocol Pediatric Airway Protocol Poor Perfusion No Yes I IV Protocol I F R HR <60 CPR F R Monitor M Contact Medical Control M Epinephrine 1:10,000 0.01 mg/kg IV/IO Max single dose 0.5mg May repeat q 3-5 min P Atropine 0.02 mg/kg IV/IO Min 0.1mg dosing May repeat q 3-5 min P I P Pearls: Revised: Consider Transcutaneous Pacing P M Consider Dextrose 10% Narcan NS Bolus P P I Contact Medical Control M Exam: Mental Status, HEENT, Skin, Lung, Heart, Abdomen, Back, Extremities, Neuro. Infant = < 1 year of age. Most maternal medications pass though breast milk to the infant. The majority of pediatric arrests are due airway problems. 07/11/2011 M.to Stover, MD Hypoglycemia, severe dehydration and narcotic effects may produce bradycardia. Pediatric patients requiring external transcutaneous pacing require the use of pads appropriate for pediatric patients per the manufacturers guidelines. 48 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Head Trauma, PEDIATRIC History: (Broselow Tape) Signs and Symptoms: Time of injury Mechanism (blunt vs penetrating) Loss of consciousness Bleeding Past medical history Evidence for multitrauma Differential: Pain, swelling, bleeding Altered mental status Unconscious Respiratory distress / failure Vomiting Major traumatic mechanism of injury Seizure Skull fracture Brain injury (Concussion, Contusion, Hemorrhage or Laceration) Epidural hematoma Subdural hematoma Subarachnoid hemorrhage Spinal injury Abuse Universal Patient Care Protocol Isolated Head Trauma No Yes Multiple Trauma Protocol Spinal F Immobilization R Protocol F R I I IV Protocol Does patient opens eyes to “What happened to you”?, or other verbal commands Yes Response to pain? Maintain SPO2 >90% Yes B <60 I P Blood Glucose Seizure? B No Pediatric Seizure Protocol D25 2ml/kg P Intubate maintain CO2 30-35/O2 Sat >90% with Capnography if available P Monitor and Reassess I Glucagon If no IV Consider Narcan 0.1mg/kg No P M Contact Medical Control M Exam: Mental Status, HEENT, Skin, Lungs, Heart, Abdomen, Back, Extremities, Neuro If GCS < 12 consider air/rapid transport and if GCS < 8 intubation should be anticipated. Increased intracranial pressure (ICP) may cause hypertension and bradycardia (Cushing’s Response). Hypotension usually indicates injury or shock unrelated to the head injury. The most important item to monitor and document is a change in the level of consciousness. Revised:are07/11/2011 M. with Stover, Concussions periods of confusion or LOC associated trauma,MD which may have resolved by the time EMS arrives. Any prolonged confusion or mental status abnormality, which does not return to normal within 15 minutes, or any documented loss of consciousness, should be evaluated by a physician ASAP. 49 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Hypotension Shock(Non-Trauma), PEDIATRIC Broselow Tape History: Signs and Symptoms: Blood Loss Fluid Loss Vomiting Diarrhea Fever Infection Differential: Restlessness/ Confusion Dizziness Increased HR Decreased BP Pale, cool, clammy skin Delayed capillary refill Trauma Infection Dehydration Congenital heart disease Medication or Toxin Universal Patient Care Protocol I IV Protocol I Evidence or history of trauma? Yes No Pediatric Multiple trauma protocol B Blood Glucose B < 70 I Dextrose 10% IV I P Glucagon 0.5mg IM If no IV P > 70 I NS Bolus 20 cc / kg I M Contact Medical Control M P Consider Dopamine 5-20 mcg/kg/min titrate to systolic BP of 90 mmHg P Exam: Mental status, Skin, HEENT, Heart, Lung, Abdomen, Extremities, Back, Neuro Consider all possible causes of shock and treat per specific protocol Decreasing heart rate is a sign of impending collapse Most maternal medications pass through breast milk to the infant Revised: 07/11/2011 M. Stover, MD 50 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Multiple Trauma, PEDIATRIC History: Signs and symptoms: Time and mechanism of injury Damage to structure or vehicle Location in structure or vehicle Others injured or dead Speed and details of MVC Restraints / Protective equipment: Car seat, Helmet, Pads Ejection Past medical history Medications Differential (Life Threatening): Pain, swelling Deformity, lesions, bleeding Altered mental status Unconscious Hypotension or shock Arrest (Broselow Tape) Chest : Tension pneumothorax Flail Chest Pericardial Tamponade Open chest wound Hemothorax Intra-abdominal bleeding Pelvis / Femur fracture Spine fracture / Cord Injury Head injury (see Head Trauma) Extremity fracture / dislocation HEENT (Airway obstruction) Hypothermia Universal Patient Care Protocol Spinal Immobilization Protocol F R I IV Protocol F R I Vital Signs/ Perfusion Abnormal Rapid Transport Focused Exam I NS Bolus 20cc/kg Repeat as needed (max 60 cc/kg If lungs are clear) I P Tension Pneumothorax? Chest Decompression P M Normal Transport Contact Medical M Control Exam: Mental status, Skin, HEENT, Heart, Lung, Abdomen, Extremities, Back, Neuro Mechanism is the most reliable indicator of serious injury. Examine all restraints / protective equipment for damage. If prolonged extrication times of serious trauma consider air transportation to improve time to a trauma center and the ability to give blood products. Do not overlook the possibility of child abuse. Children should be removed from car seats to allow for complete examination. Revised: 07/11/2011 M. Stover, MD 51 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Pulseless Arrest, PEDIATRIC (Broselow Tape) History: Signs and Symptoms: Time of arrest Medical history Medications Possibility of foreign body Hypothermia Differential: Unresponsive Cardiac arrest Respiratory failure Foreign body Secretions Infection (Croup, Epiglotitis) Hypovolemia (Dehydration) Congenital Heart Disorder Trauma Tension pneumothorax Hypothermia Toxin or medication Hypoglycemia Acidosis Universal Patient Care Protocol F R CPR F R P Cardiac Monitor P V- Fib V- Tach Defibrillate 2 j/kg, CPR 5 cycles, defibrillate at 4 j/kg P P Endotracheal Intubation I IV Protocol M Revised: P Defibrillation 4 j/kg P Consider Amiodarone 5 mg/kg IV/IO Repeat x1 Contact Medical Control P Endotracheal Intubation I IV Protocol P P I P Epinephrine 1:10,000 0.01 mg/kg IV/IO Max dose 1mg Repeat q 3-5 min P Asystole PEA P I P P P M P I Epinephrine 1:10,000 0.01 mg/kg IV/IO Max dose 1mg Repeat q 3-5 min Dextrose 25% 2cc/kg Narcan 0.1mg/kg IV/IO (pearls) P I P Contact Medical Control Determine Causes: Hypoxia, Acidosis, Volume M Depletion, Hypothermia, Hypoglycemia M Exam: Mental Status Monophasic and Biphasic waveform defibrillators should use the same energy levels noted above. In order to be successful in pediatric arrests, a cause must be identified and corrected. 07/11/2011 M. This Stover, Airway is the most important intervention. shouldMD be accomplished immediately. Patient survival is often dependent on airway management success. Narcan for suspected or known substance abuse. 52 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Respiratory Distress, PEDIATRIC(Broselow Tape) History: Signs and symptoms: Time of onset Possibility of foreign body Medical history Medications Fever or respiratory infection Other sick siblings History of trauma Differential: Wheezing or stridor Respiratory retractions Increased heart rate Altered level of consciousness Anxious appearance Asthma Aspiration Foreign body Infection, Pneumonia, Croup, Epiglotitis Congenital heart disease Medication or Toxin Trauma Universal Patient Care Protocol Respiratory Insufficiency? Yes No Position patient for comfort Pediatric Airway Protocol P Yes Albuterol 2.5mg via HHN May repeat x3 P if HR < 200 bpm SEE PEARLS Wheezing? No I M IV Protocol If SPO2 <90% I Contact Medical Control M P Consider Epi 1:1,000 0.01 mg/kg SQ P Solumedrol 1mg/kg IV P P Pearls: Exam: Mental Status, HEENT, Neck, Skin, Lungs, Heart, Abdomen, Back, Extremities, Neuro. Pulse oximetry should be monitored continuously if initial saturation is < 96%, or there is a decline in patient status despite normal pulse oximetry readings. Do not force a child into a position. They will protect their airway by their body position. The most important component of respiratory distress is airway control. Epiglottitis typically affects children < 2 years of age. It is bacterial, with fever, rapid onset, possible stridor, patient wants to sit up to keep airway open, drooling is common. Airway manipulation may worsen the condition. Revised: 07/11/2011 M. Stover, MD 53 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Seizure, PEDIATRIC History: (Broselow Tape) Signs and Symptoms: Fever Prior history of seizures Seizure medications Reported seizure activity History of recent head trauma Congenital abnormality Medical Control Differential: Observed seizure activity Altered mental status Hot, dry skin or elevated body temperature Fever and/or Infection Head Trauma Medication or Toxin Hypoxia or Respiratory Failure Hypoglycemia Metabolic abnormality / acidosis Tumor Universal Patient Care Protocol Position on side to prevent aspiration Yes Cooling Measures Febrile? No I Blood Glucose <70 Dextrose 25% 2cc//kg I P Glucagon 0.5mg IM if no IV P Active Seizure Repeat Seizure I IV Protocol I P Valium 0.2 mg/kg IV/IO or 0.5 mg/kg Rectal M Contact Medical Control P M Exam: Mental Status, HEENT, Lung, Heart, Extremities, Neuro. Status Epilepticus is defined as two or more successive seizures without a period of consciousness or recovery. This is a true emergency requiring rapid airway control, treatment, and transport. Grand mal seizures are associated with loss of consciousness, incontinence, and tongue trauma. Focal seizures (petit mal) effect only a part of the body and are not usually associated with a loss of consciousness. Jacksonian seizures are seizures that start as a focal seizure and become generalized. Be prepared to assist ventilations especially if a benzodiazipine is used. If evidence or suspicion of trauma, spine should be immobilized. If febrile, remove clothing and sponge with room temperature water. In an infant, a seizure may be the only evidence of a closed head injury. Revised: 07/11/2011 M. Stover, MD 54 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Supraventricular Tachycardia, PEDIATRIC (Broselow Tape) History: Signs and Symptoms: Past medical history Medications or Toxic Ingestion (Aminophylline, Diet pills, Thyroid supplements, Decongestants, Digoxin) Drugs (nicotine, cocaine) Congenital Heart Disease Respiratory Distress Syncope or near syncope Differential: Heart Rate: Child > 180/bpm Infant > 220/bpm Pale or Cyanotic Diaphoresis Tachypnea Vomiting Hypotension Altered Level of Consciousness Pulmonary Congestion Syncope Heart disease (Congential) Hypo / Hyperthermia Hypovolemia or Anemia Electrolyte Imbalance Anxiety/Pain/Emotional stress Fever / Infection / Sepsis Hypoxia Hypoglycemia Medication / Toxin / Drugs Pulmonary embolus Trauma Tension Pneumothorax Universal Patient Care Protocol P Stable M Contact Medical Control Cardiac Monitor P Unstable M I IV Protocol P Valsalva Manv. P M Adenosine .1mg/kg then .2 mg/kg Contact Medical Control Pre- Arrest I P I IV Protocol I M Contact Medical Control M P Cardioversion 0.5 joules/ kg. P P Cardioversion 1-2 joules/ kg. P P M Pearls: Exam: Mental Status, HEENT, Skin, Lung, Heart, Abdomen, Back, Extremities, Neuro. Carefully evaluate the rhythm to distinguish Sinus Tachycardia, Supraventricular Tachycardia, and Ventricular Tachycardia. Separating the child from the caregiver may worsen the child’s clinical condition. Pediatric paddles should be used in children < 10kg or Broselow-Luten color Purple. Continuous pulse oximetry is required for all SVT patients if available. Document all rhythm changes with ECG strips and obtain monitor strips with each intervention. Revised: 07/11/2011 M. Stover, MD 55 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Trauma Protocols Revised: 07/11/2011 M. Stover, MD 56 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Bites and Envenomations History: Signs and Symptoms: Type of bite or sting Description or bring creature / photo with patient for identification Time, location, size of bite/sting Previous reaction to bite / sting Domestic vs Wild Tetanus and Rabies risk Immunocompromised patient Differential: Rash, skin break, wound Pain, soft tissue swelling, redness Blood oozing from bite wound Evidence of infection Shortness of breath, wheezing Allergic reaction, hives, itching Hypotension or shock Animal bite Human bite Snake bite (poisonous) Spider bite (poisonous) Insect sting / bite (bee, wasp, ant, tick) Infection risk Rabies risk Tetanus risk Universal Patient Care Protocol No Contact Animal Control (if required) EMS Transport? Yes Immobilize Area and Limb Allergic Reaction? Yes Allergic Reaction Protocol M Pearls: No Pain Control Protocol Contact Medical M Control Exam: Mental Status, HEENT, Skin, Lung, Heart, Abdomen, Back, Extremities (location of injury), and Neuro exam if systemic effects are noted. Human bites are much worse than animal bites due to normal mouth bacteria. Carnivore bites are much more likely to become infected and have risk of rabies exposure. Cat bites may progress to infection rapidly due to a specific bacterium. Poisonous snakes in our area are of the pit viper family: rattlesnake, copperhead, and water moccasin. Coral snake bites are rare: Very little pain…but very toxic. “Red on yellow – Kill a fellow, red on black – venom they lack”. Amount of envenomation is variable, generally worse with larger snakes and early spring. If no pain or swelling, envenomation is unlikely. Black widow spider bites tend to be minimally painful, but over a few hours, muscular pain and severe abdominal pain may develop (spider is black with red hour glass on belly). Brown Recluse spider bites are minimally painful to painless. Little reaction is noted initially but tissue necrosis at the site of the bite may develop over the next few days (brown spider with fiddle shape on back). Evidence of infection: swelling, redness, drainage, fever, red streaks proximal to wound. Immuno-compromised patients have an increased risk for infection: diabetes, chemotherapy, transplants,… Consider contacting the South Carolina Poison Control Center for guidance. Revised: 07/11/2011 M. Stover, MD 57 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Aquatic Life Universal Patient Care Protocol Yes Allergic Reaction Allergic Reaction Protocol No Attempt to Identify Type of Aquatic Life Involved Jelly Fish Sea Urchins/ Sea Cucumbers/ Starfish Stingrays Rinse with F F Seawater NOT R R Freshwater F R F R Apply copius amounts of vinegar F R F R Remove Tentacles with Forceps F R F Gently Shave Affected F R Area R Irrigate with NaCl F R Immerse area F in Warm water R 110-115 degrees F F Remove spines F R with forceps R F R F Cover with F R Sterile Dressing R P Pain Control Protocol F R Immerse area F in Warm water R 110-115 degrees F P Pain Control Protocol P P M Contact Medical Control M Jelly Fish- Venom is deposited by organelles called nematocysts. DO NOT APPLY FRESH WATER! Fresh water causes osmotic shock to organelles and will release any venom still in nematocysts. Vinegar is 5% acetic acid, which inactivates nematocysts. Stingrays- Whip like tail impales the foot. Can even penetrate shoes. Many spines on tail that contain venom glands. Pieces may remain hidden in the wound. Toxin inactivated by heat. Revised: 07/11/2011 M. Stover, MD 58 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Burns History: Signs and Symptoms: Type of Exposure (heat, gas, chemical) Inhalation injury Time of injury Past medical history Medications Other trauma Loss of consciousness Tetanus / Immunization status Differential: Burns, pain, swelling Dizziness Loss of consciousness Hypotension / shock Airway compromise / distress Singed facial or nasal hair Hoarseness / wheezing Superficial (1st degree) red and painful Partial thickness (2nd degree) blistering Full thickness (3rd degree) painless and charred or leathery skin Chemical Thermal Electrical Radiation Universal Patient Care Protocol Remove Jewelry Thermal Chemical If <10% BSA Cool down with Normal Saline Eye Involvement? Continuous Saline Flush Cover with dry sheet or dressing Remove Clothing Expose Area Flush Area with Normal Saline for 10- 15 minutes I IV Protocol Bolus I P Pain Control Protocol P M Contact Medical Control M Exam: Mental Status, HEENT, Neck, Skin, Lung, Heart, Abdomen, Back, Extremities, Neuro. Critical Burns: > 25% body surface area (BSA); 3’ burns > 10% BSA; 2’ and 3’ burns to face, eyes, hands or feet; electrical burns; respiratory burns; deep chemical burns; burns with extremes of age or chronic disease; and burns with associated major traumatic injury. Early intubation is required in significant inhalation injuries. Potential CO exposure should be treated with 100% oxygen. Circumferential burns to extremities can cause vascular compromise secondary to soft tissue swelling. Burn patients are prone to hypothermia – Never apply ice or try to cool burns that involve >10% BSA. Do not over look the possibility for child abuse with children and burn injuries or of multiple system trauma. See appendix for rule of nines. Revised: 07/11/2011 M. Stover, MD 59 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Drowning/ Near Drowning History: Submersion in water regardless of depth Possible history of trauma ie: diving board Duration of immersion Temperature of water Signs and Symptoms: Unresponsive Mental status changes Decreased or absent vital signs Vomiting Coughing Differential: Trauma Pre-existing medical problem Pressure injury (diving) Barotrauma Decompression sickness Universal Patient Care Protocol F R Spinal Protocol F R I IV Protocol I Monitor and Reassess P Resp. Distress? Wheezing Albuterol & Atrovent Pulmonary Edema CPAP M P Contact Medical M Control Pearls: Exam: Trauma Survey, Head, Neck, Chest, Pelvis, Abdomen, Back, Extremities, Neuro With cold water no time limit – resuscitate all with CPR and one round of drugs until patient is warmed. All victims should be transported for evaluation due to potential for worsening over the next several hours. Drowning is a leading cause of death among would-be rescuers. Allow appropriately trained and certified rescuers to remove victims from areas of danger. With pressure injuries (decompression / barotraumas), consider transport or availability of a hyperbaric chamber. Revised: 07/11/2011 M. Stover, MD 60 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Electrical Injuries History: Lightening or electrical l exposure Single or multiple victims Other trauma secondary from a fall from electrical highwire or MVC into power pole with lines down Voltage and current (AC / DC) Signs and Symptoms: Burns Pain Entry and exit wounds Hypotension or shock Arrest Differential: Cardiac Arrest Seizure Burns (see Burn Protocol) Multiple trauma Universal Patient Care Protocol P 12 Lead ECG if available P I IV Protocol Bolus I Focused History and Exam F R Dressings P Pain Control Protocol M Contact Medical Control F R P M Exam: Mental Status, HEENT, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro Ventricular fibrillation and asystole are the most common dysrhythmias. Damage is often hidden; the most severe damage will occur in muscle, vessels and nerves. In a mass casualty lightening incident, attend to victims in full arrest first. If the victim did not arrest initially, it is likely they will survive. Do not overlook other trauma (i.e. falls). Lightening is a massive DC shock most often leading to asystole as a dysrhythmia. In lightening injuries, most of the current will travel over the body surface producing flash burns. Revised: 07/11/2011 M. Stover, MD 61 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Extremity Trauma History: Type of injury Mechanism: crush / penetrating / amputation Time of injury Open vs. closed wound / fracture Wound contamination Medical history Medications Signs and Symptoms: Pain, swelling Deformity Altered sensation / motor function Diminished pulse / capillary refill Decreased extremity temperature Differential: Abrasion Contusion Laceration Sprain Dislocation Fracture Amputation U n iv e rs a l P a tie n t C a re P ro to c o l F R C o n tro l B le e d in g W o u n d C a re F R L ife o r L im b T h re a te n in g In ju ry I IV P ro to c o l I P a in C o n tro l P ro to c o l A m p u ta tio n F R P la c e A m p u ta te d P a rt in P la s tic B a g K e e p P a rt C o o l, B u t N o t in D ire c t C o n ta c t w ith Ic e W ra p w ith m o is t s te rile d re s s in g M C o n ta c t M e d ic a l C o n tro l F R M Pearls: Exam: Mental Status, Extremity, Neuro In amputations, time is critical. Transport and notify medical control immediately, so that the appropriate destination can be determined. Hip dislocations and knee and elbow fractures / dislocations have a high incidence of vascular compromise. Urgently transport any injury with vascular compromise. Blood loss may be concealed or not apparent with extremity injuries. Lacerations must be evaluated for repair within six hours from the time of injury. Revised: 07/11/2011 M. Stover, MD 62 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Head Trauma History: Time of injury Mechanism: blunt / penetrating Loss of consciousness Bleeding Medical history Medications Evidence of multi-trauma Helmet use or damage to helmet Signs and Symptoms: Pain, swelling, bleeding Altered mental status Unconscious Respiratory distress / failure Vomiting Significant mechanism of injury Differential: Skull fracture Brain injury (concussion, contusion, hemorrhage, or laceration) Epidural hematoma Subdural hematoma Subarachnoid hemorrhage Spinal injury Abuse Universal Patient Care Protocol Isolated Head Trauma No Yes Multiple Trauma Protocol Spinal F Immobilization R Protocol F R I I IV Protocol Pt. Alert & Responsive No Yes Is pt protecting airway? Yes Maintain SPO2 >90% Yes B Blood Glucose No P Seizure? Lidocaine 100 mg & Valium 10mg Consider Versed 5mg IV bolus P B No Seizure Protocol P Monitor and Reassess M Contact Medical Control Intubate / Ventilate Maintain CO2 @ 30-35w/ capnography if available P M Exam: Mental Status, HEENT, Lung, Heart, Abdomen, Back, Extremities, Neuro If GCS < 12 consider Air/Rapid Transport and if GCS < 9 intubation should be anticipated. Increased intracranial pressure (ICP) may cause hypertension, irregular respirations and bradycardia (Cushing’s Response) is the hallmark of herniation syndrome. Hypotension usually indicates injury or shock unrelated to the head injury and should be aggressively treated. The most important item to monitor and document is a change in the level of consciousness. Consider restraints if necessary for patient’s and/or personnel’s protection per the Restraint Protocol. Limit IV fluids unless patient is hypotensive (systolic BP < 90). Concussions are periods of confusion or LOC associated with trauma, which may have resolved by the time EMS arrives. Any prolonged confusion or mental status abnormality that does not return to normal within 15 minutes or any Revised: 07/11/2011 Stover, documented loss of consciousness should be M. evaluated by a MD physician ASAP. 63 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Hyperthermia History: Age Exposure to increased temperatures and/or humidity Past medical history / medications Extreme exertion Time and length of exposure Poor PO intake Fatigue and/or muscle cramping Signs and Symptoms: Altered mental status or unconsciousness Hot, dry or sweaty skin Hypotension or shock Seizures Nausea Differential: Fever (infection) Dehydration Medications Hyperthyroidism (Storm) Delirium tremens (DT’s) Heat cramps Heat exhaustion Heat stroke CNS lesions or tumors Universal Patient Care Protocol F R Document Temperature F R Remove Heat Source Remove Clothing Apply room temperature water to skin and increase air flow around patient I IV Protocol I Monitor and Reassess Appropriate Protocol M Pearls: Contact Medical M Control Exam: Mental Status, HEENT, Skin, Lungs, Heart, Neuro. Extremes of age are more prone to heat emergencies (i.e. young and old). Predisposed by use of: tricyclic antidepressants, phenothiazines, anticholinergic medications, and alcohol. Cocaine, Amphetamines, and Salicylates may elevate body temperatures. Sweating generally disappears as body temperature rises above 104 F (40 C). Intense shivering may occur as patient is cooled. Heat Cramps consist of benign muscle cramping secondary to dehydration and is not associated with an elevated temperature. Heat Exhaustion consist of dehydration, salt depletion, dizziness, fever, mental status changes, headache, cramping, nausea and vomiting. Vital signs usually consist of tachycardia, hypotension, and an elevated temperature. Heat Stroke consists of dehydration, tachycardia, hypotension, temperature > 104 F (40 C), and an altered mental status. Revised: 07/11/2011 M. Stover, MD 64 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Hypothermia History: Past medical history Medications Exposure to environment even in normal temperatures Exposure to extreme cold Extremes of age Drug use: Alcohol, barbiturates Infections / Sepsis Length of exposure / wetness Signs and Symptoms: Cold, clammy Shivering Mental status changes Extremity pain or sensory abnormality Bradycardia Hypotension or shock Differential: Sepsis Environmental exposure Hypoglycemia CNS dysfunction Stroke Head injury Spinal cord injury U n iv e r s a l P a tie n t C a r e P r o to c o l R e m o v e w e t c lo th in g T e m p e r a tu r e < 9 5 F (< 3 5 C ) Yes H a n d le G e n tly Hypothermic patients in cardiac arrest should receive only one defibrillation and only one round of medications until temp is > 85 F Hot Packs and B la n k e ts I IV P r o to c o l I No B O b ta in B G L A p p r o p r ia te P r o to c o l B M C o n ta c t M e d ic a l C o n tr o l M Pearls: Exam: Mental Status, Lung, Heart, Abdomen, Extremities, Neuro. NO PATIENT IS DEAD UNTIL THEY ARE WARM AND DEAD!!!!!!! Defined as core temperature < 35 C (95 F). Extremes of age are more susceptible (i.e. young and old). With temperature less than 31 C (88 F) ventricular fibrillation is common cause of death. Handling patients gently may prevent this (rarely responds to defibrillation). If the temperature is unable to be measured, treat the patient based on the suspected temperature. Hypothermia may produce severe bradycardia. Shivering stops below 32 C (90 F). Revised: 07/11/2011 M. Stover, MD Hot packs can be activated and placed in the armpit and groin area if available. Care should be taken not to place the packs directly against patient’s skin. Consider withholding CPR if patient has organized rhythm. Discuss with medical control. 65 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Multiple Trauma History: Time and mechanism of injury Damage to structure or vehicle Location in structure or vehicle Others injured or dead Speed and details of MVC Restraints / protective equipment Past medical history Medications Signs and Symptoms: Pain, swelling Deformity, lesions, bleeding Altered mental status or unconscious Hypotension or shock Arrest Differential: (Life threatening) Chest: Tension Pneumothorax Flail chest Pericardial tamponade Open chest wound Intra-abdominal bleeding Pelvis / Femur fracture Spine fracture / Cord injury Head injury (see Head Trauma) Extremity fracture / Dislocation HEENT (Airway obstruction) Hypothermia U n iv e r s a l P a tie n t C a r e P r o to c o l F R R a p id T r a u m a A ssessm ent F R C o n s id e r r a p id a ir tr a n s p o r t / T r a n s p o r t to tr a u m a c e n te r F R S p in a l P r o to c o l F R I IV P r o to c o l I V ita l S ig n s / P e r fu s io n A b n o rm a l I N S B o lu s N o rm a l O n g o in g A ssessm ent I R eassess A ir w a y P r o to c o l P C o n tin u e d H y p o te n s io n W itn e s s e d T r a u m a tic A r r e s t C o n s id e r C h e s t D e c o m p r e s s io n M P C o n ta c t M e d ic a l C o n tr o l M Pearls: Exam: Mental Status, Skin, HEENT, Heart, Lung, Abdomen, Extremities, Back, Neuro. Mechanism is the most reliable indicator of serious injury. In prolonged extrications or serious trauma, consider air transportation for transport times and the ability to give blood. Do not overlook the possibility of associated domestic violence or abuse. Revised: 07/11/2011 M. Stover, MD 66 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control Spinal Immobilization Clearance Neuro Exam: Any focal deficit? Yes No Patient > 65 or < 5 with SIGNIFICANT traumatic mechanism? Yes No Alertness: Any mental alteration in patient? Yes No Intoxication: Any evidence of drugs or alcohol? Yes No Distracting Injury: Any painful injury that might distract the patient from the pain of a spinal injury? Yes No P Spinal Exam: Point tenderness or P pain to ROM in spinal process? Yes No P Spinal Immobilization Not Required P Spinal Immobilization Required Exam: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro Significant mechanism includes high-energy events such as ejection, high falls, and abrupt deceleration crashes and may indicate the need for spinal immobilization in the absence of symptoms. Range of motion (ROM) should NOT be assessed if patient has midline spinal tenderness. Patient’s range of motion should not be assisted. The patient should touch their chin to their chest, extend their neck (look up), and turn their head from side to side (shoulder to shoulder) without spinal process pain. The acronym “NSAIDS” should be used to remember the stops in this protocol. “N” = Neurologic exam. Look for focal deficits such as tingling, reduced strength, or numbness in an extremity “S” = Significant mechanism in extremes of age “A” = Alertness. Is patient oriented to person, place, time, and situation? Any change to alertness with this incident? “I” = Intoxication. Is there any indication that the person is intoxicated (impaired decision making ability)? “D” = Distracting injury. Is there any other injury which is capable of producing significant pain in this patient? “S” = Spinal exam. Look for point tenderness in any spinal process or spinal process tenderness with range of motion. The decision to NOT implement spinal immobilization in a patient is the responsibility of the paramedic. In very old and very young patients, a normal exam may not be sufficient to rule out spinal injury. Revised: 07/11/2011 M. Stover, MD 67 Georgetown County Emergency Services Patient Care Protocols and Standing Orders FR EMT Intermediate Paramedic Medical Control WMD-Nerve Agent Protocol History: Exposure to chemical, biologic, radiologic, or nuclear hazard Potential exposure to unknown substance/hazard Signs and Symptoms: Visual Distrubances Headache Nausea/Vomiting Salivation Lacrimation Respiratory Distress Diaphoresis Seizure Activity Respiratory Arrest Differential: Nerve agent exposure (e.g., VX, Sarin, Soman, etc) Organophosphate exposure (pesticide) Vesicant exposure (e.g.,Mustard Gas, etc.) Respiratoy irritant Exposure (e.g., Hydrogen Sulfide, Ammonia, Chlorine, etc.) Ensure Scene Safety and Proper PPE Universal Patient Care Protocol Obtain history of exposure Observe for specific toxidromes Initiate triage and/or decontamination as indicated. Minor symptoms: Salivation, Lacrimation, Visual Disturbances P Atropine 2mg IV/IM q 5 min. (0.02-0.05 mg/kg) P Until symptoms resolve Mark One Kit IM x 3 rapidly (See Pediatric Doses Below) Monitor for appearance of major symptoms Major Symptoms: Altered Mental Status, Seizures, Respiratory Distress, Respiratory Arrest Assess for presence of major or minor symptoms P If Seizures: Valium 5mg IV/IM/PR may repeat up to 10mg P P Atropine 2mg IV/IM q 5 min. (0.02-0.05 mg/kg) Until symptoms resolve P In the face of a bona fide attack, begin with 1 Mark One kit for patients less than 7 years of age, 2 Mark one kits from 8 to 14 years of age, and 3 Mark One kits for patients 15 years of age and over. For patients with major symptoms, there is no limit for atropine dosing. Carefully evaluate patients to ensure they are not suffering from exposure to another agent (e.g., narcotics, vesicants, etc.) In the absence of Mark One kits, 0.5 mg Atropine pt < 40 lbs., 1 mg dose pt between 40-90 lbs., and 2 mg dose for pts > 90 lbs. Revised: 07/11/2011 M. Stover, MD 68