North Wales Cancer Network
advertisement

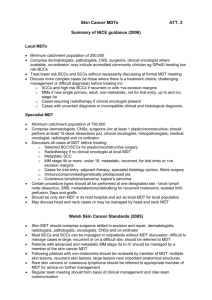
North Wales Haematological Cancers Multidisciplinary Team (MDT) Operational Policy FINAL DRAFT – June 2007 14th June 2007 Policy agreed: Policy to be reviewed by: 14th June 2008 Final Draft - Haematology Operational Policy June 2007 1 CONTENTS 1.0 INTRODUCTION 4 2.0 SCOPE OF THE SERVICE 4 2.1 RESOURCES AVAILABLE AT EACH SITE 5 3.0 MDT STRUCTURE AND IMPLEMENTATION 6 3.1 NORTH WALES MDT MODEL 6 3.2 CORE MDT MEMBERS 6 3.3 ROLE OF THE CORE MDT 7 3.4 CORE MDT LEAD CLINICIAN 7 3.5 LOCAL CLINICAL TEAM MEMBERS 7 3.6 ROLE OF THE LOCAL CLINICAL TEAMS 9 3.7 LOCAL CLINICAL TEAM LEAD CLINICIAN 10 4.0 ACCESSING THE SERVICE 10 4.1 URGENT ‘SUSPECTED CANCER’ GP REFERRALS 10 4.2 OTHER REFERRALS 10 4.3 EMERGENCY ACCESS TO CLINICAL TEAM 10 4.4 WAITING TIMES 10 5.0 TREATMENT PLANNING DECISIONS 11 5.1 YSBYTY GWYNEDD 11 5.2 YSBYTY GLAN CLWYD 11 5.3 YSBYTY MAELOR 11 5.4 JOINT/COMPLEX MEETINGS 11 6.0 ACCESS TO OTHER SERVICES 12 6.1 PSYCHOLOGICAL SUPPORT 12 6.2 FERTILITY SERVICES 12 6.3 OTHER SUPPORT SERVICES 12 6.4 PALLIATIVE CARE 12 Final Draft - Haematology Operational Policy June 2007 2 7.0 PATIENT PATHWAYS 12 8.0 CLINICAL GUIDELINES AND POLICIES 13 9.0 RISK MANAGEMENT 13 10.0 COMMUNICATION 13 10.1 COMMUNICATION BETWEEN TEAM MEMBERS 13 10.2 COMMUNICATION BETWEEN MDT AND PATIENT/CARER 14 10.3 COMMUNICATION SKILLS TRAINING 14 10.4 PATIENT WRITTEN INFORMATION 14 10.5 COMMUNICATION WITH GPs 14 11.0 DATA COLLECTION AND INFORMATION 14 12.0 AUDIT 15 13.0 CLINICAL TRIALS 15 14.0 NEW DRUGS 15 15.0 ONGOING EDUCATION 15 16.0 SERVICE IMPROVEMENT 15 17.0 AGREEMENT TO OPERATIONAL POLICY 16 APPENDIX 1 17 APPENDIX 2 19 Final Draft - Haematology Operational Policy June 2007 3 1.0 INTRODUCTION This operational policy details the scope and organisation of services offered by the North Wales Haematological Cancers MDT. It sets out the agreed standards and processes to which all members of the MDT should work in order to ensure the delivery of high quality patient focused care. The policy has been developed in accordance with national guidelines on the delivery of haematological cancer services, including NICE guidance on Improving Outcomes in Haematological Cancers (2003), the WAG National Standards for Haematological Cancer Services (2005) and JACIE Standards for Haematopoietic Progenitor Cell Collection, Processing and Transplantation (2005). The objectives of this policy are to: Provide a detailed description of the foundations that support the single MDT model adopted in North Wales Describe the operational policy by which MDT members should function Provide an indication to policy makers, commissioners and other stakeholders of how the service is configured and how it functions Establish a framework for the future assessment of the service This policy will be reviewed annually by the North Wales Haematological Cancers MDT and updated as appropriate. 2.0 SCOPE OF THE SERVICE The North Wales Haematological Cancers MDT provides care to a total population of approximately 665,000 (2001 census). The MDT acts as a single team with services based on three sites: Ysbyty Gwynedd, Bangor, part of North West Wales NHS Trust Ysbyty Glan Clwyd, Bodelwyddan, part of Conwy and Denbighshire NHS Trust Ysbyty Maelor, Wrexham, part of North East Wales NHS Trust The MDT manages adults with leukaemia, lymphomas and myeloma. All children presenting with a haematological malignancy are referred to the specialist service at Alder Hey Hospital in Liverpool. The MDT offers treatment up to BCSH level 3 ie up to and including high dose therapy with autologous transplantation. Patients requiring level 4 services (ie allogeneic transplantation) are referred to hospitals outside the North Wales Cancer Network, dependent upon the exact nature of the disease and treatment required. The stem cell harvest service is based at Ysbyty Gwynedd with subsequent re-infusion taking place either at Ysbyty Gwynedd or Ysbyty Glan Clwyd. Wrexham patients are referred to the Christie Hospital in Manchester for stem cell transplantation; the MDT is working towards the repatriation of this work to North Wales in 2007/08. Over the last 3 years the Ysbyty Gwynedd and Ysbyty Glan Clwyd teams have regularly performed over 10 transplants pa (minimum 13, maximum 17) thereby fulfilling JACIE requirements before the repatriation of the Wrexham work. The service is preparing for JACIE accreditation in 2007/08. Final Draft - Haematology Operational Policy June 2007 4 Radiotherapy is provided at the North Wales Cancer Treatment Centre at Ysbyty Glan Clwyd. In addition, Wrexham lymphoma patients requiring therapeutic radiotherapy are referred to the Christie Hospital in Manchester and all patients requiring total body irradiation prior to allogeneic transplantation are referred to the hospital undertaking the transplantation. Diagnostic services are available at all three sites. In addition the MDT has access to specialist pathology services via the All Wales Lymphoma Review Panel and the cytogenetics service in Cardiff. Immunophenotyping of Wrexham patients is undertaken at the Royal Liverpool University Hospital. Patients requiring PET-CT scanning are referred in line with the Health Commission Wales service level agreement. 2.1 RESOURCES AVAILABLE AT EACH SITE YSBYTY GWYNEDD Inpatient facilities Day care facilities Support services Medical staff Nursing staff Pharmacy Alaw Ward - an 18 bedded haematology, oncology and palliative care ward; 8 single rooms, of which 6 are ensuite Alaw Day Unit - a dedicated haematology/oncology day case and outpatient unit; 5 beds and 5 chairs for day case treatments Stem-cell harvesting, cryopreservation and storage facilities meeting MHRA and HTA standards. Laboratories on site; on-site CT, MRI, bronchoscopy, ITU and HDU 3 consultant haematologists (inc. 1 part-time); 1 full-time and 2 parttime Staff Grades; 1 Associate Specialist in Oncology for stem cell work 1 specialist nurse in haematology; chemotherapy and haematology trained nurses on Alaw Unit (inc. venous access) On-site pharmacy using open laminar flow system; Trust developing business case for on site aseptic unit. Lead pharmacist for oncology YSBYTY GLAN CLWYD Inpatient facilities Day care facilities Support services Medical staff Nursing staff Pharmacy Enfys Ward - a 20 bedded haematology and oncology ward within the North Wales Cancer Treatment Centre (NWCTC); 8 single rooms with ensuite including 3 with HEPA filtration for stem cell re-infusion. Heulwen Day Care Unit – a dedicated haematology/oncology treatment unit within the NWCTC; 16 chairs/beds for day case treatments All laboratories on site; on-site CT, MRI, bronchoscopy, ITU and HDU 3 consultant haematologists; 1 Staff Grade and 1 ST1 1 haematology nurse practitioner; chemotherapy and haematology trained nurses on Enfys and Heulwen (inc venous access) On-site aseptic unit; dedicated pharmacist for haematology YSBYTY MAELOR Inpatient facilities Day care facilities Support services Medical staff Nursing staff Pharmacy Access to 6 inpatient beds on Mason Ward (medical ward) with scope for more if required; 5 single rooms inc. 2 en-suite Shooting Star Unit - a purpose built, dedicated haematology/oncology day case and outpatient unit; 5 beds and 6 chairs for day treatments All laboratories on site; on-site CT, MRI, bronchoscopy and ITU 2 consultant haematologists; 1 Associate Specialist and 0.5wte Staff Grade 1 haematology nurse specialist; chemotherapy and haematology trained nurses on Mason and Shooting Star (inc. venous access) On-site aseptic unit; dedicated pharmacist for haematology Final Draft - Haematology Operational Policy June 2007 5 3.0 MDT STRUCTURE AND IMPLEMENTATION The North Wales Haematological Cancers MDT recognises that a multi-disciplinary approach is essential to the management of haematological cancer patients. Both policy development and individual patient treatment planning decisions are improved through review, discussion and agreement by experienced clinicians from a range of specialties. 3.1 NORTH WALES MDT MODEL The North Wales Haematological Cancers MDT has adopted a model whereby the service is overseen by a core North Wales MDT with care delivered to patients on three different sites; this ensures access to a high quality local service for the entire North Wales population. The North Wales MDT membership therefore reflects two levels of involvement: 1. Core MDT members – these members are responsible for the overall running of the North Wales haematological cancers service by defining its operational policy 2. Local clinical team members – these members are the local arm of the North Wales MDT and are responsible for local service delivery in line with the overarching MDT operational policy 3.2 CORE MDT MEMBERS The core MDT is representative of each core discipline and each site providing treatment as part of the North Wales Haematological Cancers MDT. Additional members of the clinical teams may be invited to attend core team meetings as required. Name Dr D Edwards Title Location Cover Consultant Haematologist; lead Ysbyty Gwynedd Internal crossclinician cover Dr J R C Seale Consultant Haematologist Ysbyty Gwynedd Dr C F Hoyle Consultant Haematologist; Ysbyty Glan Clwyd deputy lead clinician Dr M J Goodrick Consultant Haematologist Ysbyty Glan Clwyd Dr E Heartin Consultant Haematologist Ysbyty Glan Clwyd Dr D Watson Consultant Haematologist Ysbyty Maelor Dr J Duguid Consultant Haematologist Ysbyty Maelor To be agreed Pathologist To be agreed Dr A Nethersell Consultant Clinical Oncologist Ysbyty Glan Clwyd No cover Dr D J Widdowson Consultant Radiologist Ysbyty Glan Clwyd To be agreed Linda Jones Specialist Nurse in Haematology Ysbyty Gwynedd Internal crosscover Steph Jackson Haematology Nurse Practitioner Ysbyty Glan Clwyd Jayne Samuels Clinical Nurse Specialist, Haem Ysbyty Maelor To be agreed Palliative care specialist To be agreed Nicola Andrews Data lead Ysbyty Glan Clwyd Graeme Mounsey* JACIE Project Manager Ysbyty Gwynedd Damian Heron* Director NWCN Beryl Roberts* Lead Nurse NWCN Caroline Williams* Project lead NWCN Gillian Evans User advisor NWCN/PGLC * where appropriate; Network officers’ role is to facilitate discussion, problem solve, monitor performance and provide commissioning link Final Draft - Haematology Operational Policy June 2007 6 3.3 ROLE OF THE CORE MDT The core MDT meets regularly (as a minimum quarterly). The role of the North Wales Haematological Cancers core MDT is to: Agree an operational policy for the delivery of haematological cancer services across North Wales based on current national guidance and accepted best practice Ensure the operational policy is implemented effectively on all three sites and reviewed and updated annually Agree referral and clinical guidelines for haematological malignancies in North Wales Agree optimum patient pathways for each disease type Ensure service improvement is embedded in local teams and initiate MDT wide initiatives Agree a minimum data set and analyse clinical data capture, performance and outcomes Agree and implement an annual audit programme Address any MDT wide governance or operational issues raised by the local clinical teams Identify core MDT training needs and agree an ongoing educational programme Agree a list of clinical trials and prepare any submissions for clinical trials Prepare any submissions for new drugs Agree an annual work plan Act as the Network advisory group for haematological malignancies, advising on service provision and making recommendations for service development/reconfiguration Full terms of reference are attached as Appendix 1. 3.4 CORE MDT LEAD CLINICIAN The core MDT lead clinician has responsibility for the development and overall running of the North Wales Haematological Cancers MDT, in particular: To agree the membership and role of the core MDT and ensure it meets at least quarterly To ensure the core MDT agrees an operational policy and clinical guidelines for the optimum management of haematological cancer patients based on accepted best practice. To ensure the operational policy is reviewed and updated annually To ensure clinical guidelines and patient pathways are reviewed and updated regularly To ensure that care is delivered on all three sites in line with the agreed operational policy and clinical guidelines To ensure the MDT fulfils its full role as defined in its terms of reference To agree an annual work plan for the core MDT To attend both Trust and Network cancer meetings and provide expert advice on the tumour site as appropriate, including fulfilling the role as the designated Network Board member The lead clinician’s duties are included in his/her job plan. A full job description is attached as Appendix 2. 3.5 LOCAL CLINICAL TEAM MEMBERS The local clinical teams comprise members of each core discipline required to provide treatment as part of the North Wales Haematological Cancers MDT. In addition each has extended members who offer advice to the team as required. Final Draft - Haematology Operational Policy June 2007 7 YSBYTY GWYNEDD Name Title Dr J Seale Consultant Haematologist; lead clinician Dr D Edwards Cons Haematologist; transplant lead Dr H Korn Locum Cons Haematologist (part-time) Dr E Mitchell Staff Grade Haematologist (part-time) Dr S Griffiths Staff Grade Haematologist (part-time) Dr I Tahan Staff Grade Haematologist Dr T Caslin Consultant Histopathologist Dr M Lord Consultant Histopathologist Dr S Andrew Consultant Histopathologist Dr T Nethersall Consultant Clinical Oncologist, NWCTC Dr R Williams Associate Specialist, Oncology (haem) Dr S Wenham Consultant Radiologist Linda Jones Specialist Nurse in Haematology Manon Jones Senior Nurse, Alaw Unit Jackie Jones Ward Sister, Alaw Ward Laura Edge Ward Sister, Alaw Day Unit Elaine Wain Deputy Sister, Alaw Day Unit Dr A Fowell Macmillan Consultant in Palliative Care Tania Seale Haematology Research Nurse Alice Thomas Haematology Research Nurse Mark Hankey Data co-ordinator Plus the following extended team members: Dr S Darcey Consultant Microbiologist M Hughes Pharmacist Telephone 01248 384370 01248 384369 01248 384384 x5227 01248 384369 01248 384369 01248 384369 01248 394719 01248 394719 01248 394719 01745 445157 01248 384150 01248 384690 01248 384008 x5272 01248 384945 01248 384945 01248 384008 01248 384008 01248 384384 x5142 01248 384994 01248 384995 01248 384384 x5191 Cover Internal crosscover Internal crosscover No cover No cover Dr K Edwards Internal crosscover L Roberts Internal crosscover Sec team 01248 384367 01248 384140 YSBYTY GLAN CLWYD Name Title Dr C Hoyle Consultant Haematologist; lead clinician Dr M Goodrick Consultant Haematologist Dr E Heartin Consultant Haematologist Dr M Hassan Staff Grade Haematologist Dr M Atkinson Consultant Histopathologist Dr T Nethersell Consultant Clinical Oncologist Dr Widdowson Consultant Radiologist Dr P Travis Consultant Radiologist Steph Jackson Haematology Nurse Practitioner Gwyneth Davis Clinical Trials Nurse Janine Travis Haematology Trials Nurse Nerys Wilkes Sister, Enfys Ward Dr C Usborne Consultant in Palliative Care Sue Randles MDT co-ordinator Plus the following extended team members: Dr D Edwards Transplant Director, Ysbyty Gwynedd Dr N Looker Consultant Microbiologist Dr P Manion Consultant Microbiologist Dr C Bell Consultant Anaesthetist H Flint Clinical Lead Pharmacist, Haematology C Wood Radiotherapist C Vickering Dietician Final Draft - Haematology Operational Policy June 2007 8 Telephone 01745 534881 01745 536739 01745 534377 01745 534881 01745 534064 01745 445157 01745 534115 01745 534516 01745 445272 01745 445211 01745 445211 01745 445251 01745 445909 01745 445170 01248 384369 01745 534356 01745 534708 01745 534650 01745 535242 01745 445130 01745 445239 Cover Internal crosscover Dr Dalton Dr Azam Internal crosscover/SpR Internal crosscover Yvonne Rose Anne Hughes YSBYTY MAELOR, WREXHAM Name Dr D Watson Dr J Duguid Dr L DeSoysa Dr P Smith Dr R Williams Dr A Burdge Dr K Pradeep Dr A Al-Samarraie Dr M Elias Dr J Klafkowski Jayne Samuels Anne-Marie Humphreys Sr T Vipond Margaret Moore Dr M Makin Sandra Davies Title Consultant Haematologist; lead clinician Consultant Haematologist Associate Specialist, Haematology Staff Grade, Haematology/Oncology Consultant Histopathologist Consultant Histopathologist Consultant Histopathologist Consultant Clinical Oncologist, NWCTC Consultant Radiologist Consultant Radiologist Clinical Nurse Specialist, Haematology Sister, Shooting Star Day Unit Telephone 01978 725100 01978 725866 01978 725081 01978 727603 01978 725610 01978 725079 01978 725611 01745 445158 01978 727800 01978 725493 01978 727130 01978 727603 Ward sister, Mason Ward Clinical Trials Nurse Consultant in Palliative Care MDT co-ordinator/patient tracker 01978 725443 01978 727604 01978 290919 01978 725199 Cover Internal crosscover Internal crosscover No cover Internal crosscover Internal crosscover/Wenna Hammond Macmillan CNS Other cancer co-ordinator Plus the following extended team members: Dr E Liailopoulou* Transplant Director, Christie Hospital 0161 446 8488 Dr C Cefai Consultant Microbiologist 01978 725861 A Ellis-Jones Cancer Services Pharmacist 01978 725959 * NB This will change to Dr David Edwards at Ysbyty Gwynedd with the transfer of Wrexham stem cell work to Bangor – date to be agreed. In addition the MDT has access as required to the following specialities on each site: dietetics, orthopaedic surgery, dermatology, gastroenterology, ENT, interventional radiology, renal medicine, social work, physiotherapy, occupational therapy, psychology and counselling. 3.6 ROLE OF THE LOCAL CLINICAL TEAMS The role of local clinical teams is to: Deliver care in line with the agreed MDT operational policy Review all patients, establish and record a diagnosis and agree a treatment plan Discuss responses to treatment during and at the end of therapy and agree any necessary changes in management Consider all facets of individual patient’s needs including their psychological needs and liaise with primary care, palliative care, elderly services, voluntary organisations as appropriate Identify requirements for staff and facilities for the treatment it offers Ensure adequate information, advice and support is given to patients and carers Ensure GPs are given prompt and full information on patient management and contact details of relevant clinical team members Record the minimum data set for all haematological malignancies Identify members’ training needs and ensure these are met Participate in clinical trials and research Collaborate in MDT audit Lead local service improvement initiatives and participate in MDT wide initiatives Review any local clinical governance issues including untoward incidents ensuring appropriate action is taken Final Draft - Haematology Operational Policy June 2007 9 3.7 LOCAL CLINICAL TEAM LEAD CLINICIAN Each of the three sites where care is delivered has a lead clinician who is also a member of the core MDT. He/she is responsible for ensuring that: The delivery of care at a local level is compliant with the policies, guidelines and protocols adopted by the North Wales MDT The local team at all levels of involvement are familiar and compliant with the policies, guidelines and protocols adopted by the North Wales MDT Local clinical governance issues are addressed Any conflict between local requirements and that of the MDT are raised with the MDT lead and the employing Trust is informed of the need to do so. 4.0 ACCESSING THE SERVICE 4.1 URGENT ‘SUSPECTED CANCER’ GP REFERRALS All patients meeting the criteria set out in the NICE ‘Referral for suspected cancer’ guidelines (www.nice.org.uk) should be referred to the appropriate local clinical haematological cancers team without delay, as set out in each Trust’s Directory of Cancer Services. This Directory is available on each Trust intranet site and is circulated to local GP practices. All referrals are reviewed by a consultant and if deemed to be appropriate, the patient will be seen within a maximum of 10 working days. If the referral is inappropriate, an alternative course of action is offered eg a routine appointment. 4.2 OTHER REFERRALS Many patients with haematological malignancies, in particular lymphomas, are referred initially to other specialty teams. As soon as a haematological malignancy is diagnosed, a copy of the pathology report should be sent to the local haematological cancers team; in addition any significantly abnormal electrophoresis result should be copied by the biochemistry laboratory to the haematology department to follow-up. 4.3 EMERGENCY ACCESS TO CLINICAL TEAM All patients and their GPs should be given details of how to access members of the local clinical team in an emergency. North Wales telephone triage standards are currently being developed and will be implemented by each team. 4.4 WAITING TIMES All patients diagnosed with a haematological malignancy will, where appropriate, start definitive treatment within national waiting times targets. In reality treatment usually begins much earlier than this in line with clinical need. Final Draft - Haematology Operational Policy June 2007 10 5.0 TREATMENT PLANNING DECISIONS All patients with haematological cancers should be managed by a member of the North Wales Haematological Cancers MDT. Any patient with a haematological malignancy initially presenting to another speciality should be referred to the Haematological Cancers MDT without delay. All patients should be reviewed by their local clinical team and multi-disciplinary treatment planning decisions made in line with agreed MDT clinical guidelines and protocols through daily ward rounds and weekly clinical meetings held on each site. 5.1 5.2 5.3 5.4 YSBYTY GWYNEDD All patients are reviewed on daily consultant-led ward rounds. A clinical team meeting is held every Monday to review all new and relapsed cancer patients; treatment decisions are recorded and a register of attendance kept. This meeting is attended by all members of the core local clinical team (see section 3.5); the histopathologists attend fortnightly. A clinical meeting is held every Wednesday morning where nursing and medical staff discuss current clinical problems. YSBYTY GLAN CLWYD All patients are reviewed on daily consultant-led ward rounds. A meeting is held every Monday afternoon to discuss clinic patients requiring diagnostic input or management decisions. This is attended by the consultant haematologists and haematology nurse practitioner. A pathology meeting is held every Tuesday with the haematologists and histopathologist. A clinical team meeting is held every Friday to discuss all new cancer patients; a list of patients to be discussed is sent out in advance of the meeting, based on new diagnoses made in clinics or via emergency admissions and any additional cases highlighted by histology. The meeting is recorded with minutes circulated to all members of the team; a register of attendance is kept. This meeting is attended by all members of the core local clinical team (see section 3.5) with the exception of the histopathologist, palliative care consultant and ward sister. YSBYTY MAELOR All patients are reviewed on daily consultant-led ward rounds. A clinical team meeting is held every Monday morning to review all patients to be treated that week with the medical team, day unit nursing team, pharmacist and co-ordinator/tracker. A radiology meeting is held on the first and third Friday of each month to review old and new patients; the medical team, radiologists, CNS, day unit nursing staff attend this meeting. Discussions are held with the histopathologist, oncologist and palliative care team on individual cases as required. JOINT/COMPLEX MEETINGS Stem cell meetings are held at Ysbyty Gwynedd on the first Friday of every month to review all stem cell transplant patients. The team from Ysbyty Glan Clwyd attend every other month. The Wrexham team will join this meeting, via video-conferencing if necessary, when their stem cell transplantation work is repatriated to North Wales. Where individual complex cases arise, the North Wales Haematology Cancers MDT is available via email, telephone, video-conferencing or the case may be added to the agenda of an existing meeting eg the Blood Club or MDT meeting. Alternatively, members of the MDT may contact nationally recognised experts for advice prior to the local clinical team meeting in order to ensure the delivery of best possible clinical care. Final Draft - Haematology Operational Policy June 2007 11 6.0 ACCESS TO OTHER SERVICES 6.1 PSYCHOLOGICAL SUPPORT Psychological support is offered by the clinical nurse specialists/nurse practitioners in the local clinical teams who also provide patients with details of any local support groups. Where specialist support is required patients from Ysbyty Glan Clwyd and Ysbyty Wrexham can be referred to the psychology support team based at Ysbyty Glan Clwyd. Patients at Ysbyty Gwynedd can access specialist courses in stress reduction (Mindfulness). The teams can also access their local psychiatric liaison services if required. 6.2 FERTILITY SERVICES The MDT supports patients who wish to access fertility services prior to treatment. It is the agreed policy of the MDT that male patients should be referred to St Mary’s in Manchester and female patients should be referred to the specialist gynaecology service at the Liverpool Women’s Hospital. Ysbyty Gwynedd currently provides a sperm storage service but this is under review following the introduction of more stringent legislation in this area and it is likely Bangor patients will soon be referred to St Mary’s in Manchester in line with MDT policy. 6.3 OTHER SUPPORT SERVICES The MDT has access to dieticians, physiotherapists, OTs and benefits advisors at each site. 6.4 PALLIATIVE CARE The transition from active treatment to palliative care is handled sensitively in accordance with the patient’s individual needs and wishes. Local clinical teams have access to specialist palliative care where appropriate via the individuals listed in section 3.5 above. Each local clinical team follows its Trust’s agreed end of life pathway. 7.0 PATIENT PATHWAYS The North Wales Haematological Cancers MDT has agreed to adopt the All Wales patient pathways for haematological cancers where they exist. The lymphoma pathway has been agreed; work is ongoing to develop All Wales pathways for CLL and AML. For disease types where there is no All Wales pathway, the MDT will work to develop a local agreed pathway. Final Draft - Haematology Operational Policy June 2007 12 8.0 CLINICAL GUIDELINES AND POLICIES All patients should be treated according to agreed clinical guidelines or as part of a formal clinical trial where possible. It is acknowledged that therapy may be adapted in individual patients to take account of other co-morbidities. The North Wales Haematological Cancers MDT has agreed the following clinical guidelines: The British Committee for Standardisation in Haematology (BCSH) Guidelines– see www.bcshguidelines.com The North West Region Haematology Guidelines – see www.nwhaems.co.uk The Myeloma Forum Guidelines – see www.myeloma.org.uk The CLL Forum Guidelines– see www.cllforum.com All treatment should also be conducted in accordance with the following Network wide policies: The North Wales Cancer Network Cytotoxic Chemotherapy Policy 2006 Chemotherapy protocols for each agreed regimen; these will be collated in the next Network Formulary The North Wales triage guidelines (when agreed) In addition local clinical teams should deliver care in line with local Trust policies on: chemotherapy administration (including intrathecal chemotherapy) infection prevention and control the use of all medical devices management of side effects, anaphylactic shock etc risk management and incident reporting These policies and protocols are available on individual Trust intranet sites. 9.0 RISK MANAGEMENT All risk management issues and clinical incidents should be addressed by the relevant local clinical team in line with their Trust policy on risk management and incident reporting. Any necessary action should be taken by the local clinical team and the lessons learnt shared with the core MDT. Any risk management issue involving the whole MDT should be raised with the core MDT by the Trust identifying the issue and dealt with according to their local policy. 10.0 COMMUNICATION 10.1 COMMUNICATION BETWEEN TEAM MEMBERS There is regular communication between on site team members via daily ward rounds and weekly clinical meetings. Where treatment planning decisions are required between these events, telephone and email communication should be used. Members of the North Wales Haematological Cancers MDT meet regularly at quarterly MDT meetings, audit and educational meetings. In addition there is regular telephone and email communication between all members of the MDT. Final Draft - Haematology Operational Policy June 2007 13 10.2 COMMUNICATION BETWEEN MDT AND PATIENT/CARER All patients and carers should be given details of how to contact members of the local clinical team when they are given their diagnosis; this may be the contact details of the consultant and/or the clinical nurse specialist. Patients should be encouraged to bring a family member or friend with them to any consultation where important news is likely to be given. Such consultations should be held in a private room with a nurse present where possible who can then offer further support to the patient. All treatment options should be explained to patients who are then given adequate time to consider their options and make a decision. 10.3 COMMUNICATION SKILLS TRAINING Communication skills training is available to all members of the MDT involved in direct patient care. All members of the MDT who are likely to give bad news should be encouraged to attend such training. 10.4 PATIENT WRITTEN INFORMATION Written patient information should be offered to all patients by their consultant, clinical nurse specialist, trials nurse and/or day case senior nurses; senior nurses should also ensure such information is available in ward and outpatient areas. The North Wales wide patient information folder should be given to all new patients with local information and national leaflets added as appropriate to the individual patient. This information will include leaflets from BACUP, LRF and Macmillan, clinical trials information sheets and local information on MDT arrangements and support groups. Written information should be available in both English and Welsh. 10.5 COMMUNICATION WITH GPs Following a diagnosis of haematological malignancy, the consultant should write to the patient’s GP informing them of the diagnosis and outline treatment plan. 11.0 DATA COLLECTION AND INFORMATION The Cancer Network Information System Cymru (CaNISC) does not yet have an agreed minimum data set for haematological malignancies. However all sites within the MDT enter basic demographic and clinical data on haematological malignancies onto CaNISC and will complete the haematological dataset when agreed. Each hospital submits Patient Episode Database for Wales data based on clinical coding information. Final Draft - Haematology Operational Policy June 2007 14 12.0 AUDIT The MDT participates in all Wales clinical audits as specified by CSCG All Wales Haematological Cancer Steering Group. In addition, the MDT audit group agrees an annual audit plan of two or three network wide audits per year including audits of practice against agreed clinical guidelines. The MDT is currently undertaking an audit of new DLBCL diagnoses and will then agree its audit plan for the forthcoming year. 13.0 CLINICAL TRIALS The MDT will review the national list of clinical trials once available and agree which trials it will take part in. All eligible patients should be given the opportunity to enter an agreed clinical trial. At present this does not occur at Wrexham due to a lack of resources. This issue will be taken forward by the MDT. 14.0 NEW DRUGS The North Wales Cancer Network is setting up a network wide drugs and therapeutics committee to consider the adoption of new drugs as they appear. The MDT will work with this committee on all new haematological drugs. 15.0 ONGOING EDUCATION The Blood Club meets three or four times per year for a programme of education. The Blood Club includes Merseyside services. In addition members of the MDT regularly attend North West Haematologists meetings and the British Society for Haematology, European Society for Haematology and American Society for Haematology annual meetings as well as meetings of the Myeloma Forum, CLL Forum, ALL Forum, BNLI and British Blood Transfusion Society. Both the core MDT and local clinical teams will review their training needs and agree an educational/training programme as appropriate. 16.0 SERVICE IMPROVEMENT Service improvement should be discussed at MDT meetings and be embedded within each local service. User involvement should be encouraged in all service improvement initiatives. Final Draft - Haematology Operational Policy June 2007 15 17.0 AGREEMENT TO OPERATIONAL POLICY Signature ………………………………………………….. Date ……………………………………….. Dr David Edwards Lead Clinician, North Wales Haematological Haematological Malignancies, Ysbyty Gwynedd Cancers MDT and Lead Clinician, Signature ………………………………………………….. Date ……………………………………….. Dr Christine Hoyle Deputy Lead Clinician, North Wales Haematological Cancers MDT and Lead Clinician, Haematological Malignancies, Ysbyty Glan Clwyd Signature ………………………………………………….. Date ……………………………………….. Dr David Watson Lead Clinician, Haematological Malignancies, Ysbyty Maelor Final Draft - Haematology Operational Policy June 2007 16 Appendix 1 North Wales Haematological Cancers Core Multi Disciplinary Team Membership and Terms of Reference 1. Purpose The core MDT is responsible for the overall running of the North Wales haematological cancers service. It aims to achieve the best possible outcomes for patients by ensuring access to a uniformly high quality of care across North Wales. It does this by defining and monitoring the operational policy by which all clinicians providing haematological cancer services in North Wales should operate; this operational policy is based on best clinical practice and national guidance. The core MDT is also the main source of clinical advice to the North Wales Cancer Network Management Board on all matters relating to haematology. 2. Membership The membership of the core MDT includes representatives from each site providing treatment as part of the North Wales Haematological Cancers MDT: o Ysbyty Gwynedd, Bangor, part of North West Wales NHS Trust o Ysbyty Glan Clwyd, Bodelwyddan, part of Conwy and Denbighshire NHS Trust o Ysbyty Maelor, Wrexham, part of North East Wales NHS Trust The membership includes representatives of all disciplines involved in the provision of haematology services, and named deputies, in line with Improving Outcomes in Haematological Cancers (NICE, 2003): o Haematologists o Pathologists o Oncologists o Radiologists o Clinical Nurse Specialists o Palliative care specialists o Data co-ordinators In addition the Network Director, Project Lead and User advisor may be invited as required. The Chair must ensure there is adequate representation from each site and each staff group at the MDT meeting to ensure their full involvement. 3. Chair and Deputy Chair The Chair and Deputy Chair roles are each for a maximum of five years’ duration. The Chair and Deputy Chair will be nominated by members of the MDT. If there are two or more people nominated, there will be a vote to decide who is elected. The Chair and Deputy Chair will both be agreed by the North Wales Cancer Network Board. The Chair and Deputy Chair will not be from the same Trust. 4. Administrative support Administrative support will be provided. Final Draft - Haematology Operational Policy June 2007 17 5. Frequency of meetings Meetings will be held at least quarterly. 6. Terms of reference Service planning To act as the Network advisory group for haematological malignancies, advising on service provision and making recommendations for service improvement/development/reconfiguration To advise the Network on the implications of national policy issues as they arise To agree an operational policy for the delivery of haematological cancer services across North Wales based on current national guidance and accepted best clinical practice. To review and update this policy annually To agree referral and clinical guidelines for haematological malignancies. To review and update these guidelines annually and audit their implementation To agree the optimum patient pathways for each disease type and audit implementation Service improvement and redesign To ensure service improvement is embedded within each local team and initiate MDT wide improvements as appropriate To ensure users are involved in the planning and redesign of services Service quality monitoring To ensure clinical services are delivered in accordance with required national standards i.e. JACIE, WAG cancer standards and NICE Improving Outcomes Guidance. To ensure that the MDT operational policy is implemented effectively on all three sites To ensure adequate facilities and staff exist on each site to allow full implementation of this policy To ensure adequate processes are in place on each site to allow full multi-disciplinary involvement in treatment decisions for individual patients. Where necessary to ensure mechanisms are in place for the North Wales MDT to advise on complex individual cases To agree a minimum data set for haematological malignancies and ensure it is collected on all three sites; to analyse performance and outcome data and take necessary actions To agree and implement an annual audit programme and review the results of these audits To ensure services meet national performance targets and quality standards To address any MDT wide clinical governance concerns raised by local clinical teams Workforce development To identify core MDT members’ training needs To agree an annual educational programme Research and development To agree a list of clinical trials, prepare submissions for new trials and ensure all eligible patients are offered the opportunity of entering a clinical trial as appropriate To work with the Network Drugs and Therapeutics group to agree the implementation of new drugs, preparing all necessary submissions Annual work plan To agree an annual work plan for the MDT Final Draft - Haematology Operational Policy June 2007 18 Appendix 2 North Wales Haematological Cancers Core Multi Disciplinary Team Lead Clinician Job Description 1. JOB TITLE: Lead Clinician, North Wales Haematological Cancers Core MDT 2. ACCOUNTABLE TO: Employing Trust 3. OVERALL RESPONSIBILITY: To be responsible for the development and overall running of the North Wales Haematological Cancers MDT To ensure that a high quality service is delivered to patients under the care of the MDT To establish and maintain appropriate links with all three Trusts involved in the MDT and with colleagues in the North Wales Cancer Network, primary care and the All Wales Haematological Cancers Group To be responsible for providing professional advice within and outside the North Wales Cancer Network on the tumour site and the MDT’s services 4. KEY WORKING RELATIONSHIPS: Members of the core multi-disciplinary team Cancer and Haematology Clinical Directors of the three Trusts involved in the MDT Medical Directors of the three Trusts involved in the MDT Cancer and Haematology Directorate Managers of the three Trusts involved in the MDT Director, North Wales Cancer Network Lead Nurse, North Wales Cancer Network Project Co-ordinator, North Wales Cancer Network 5. SPECIFIC DUTIES: 1. To set up the North Wales Haematological Cancers Multi-Disciplinary Team in line with NICE guidance and supported by the North Wales Cancer Network 2. To agree the membership and role of the core multi-disciplinary team 3. To ensure that the core multi-disciplinary team meets at least quarterly with an agreed core membership, records of attendance, and appropriate records of issues discussed. 4. To ensure that clinical services are delivered in accordance with required national standards i.e. JACIE, WAG cancer standards and NICE Improving Outcomes Guidance. Final Draft - Haematology Operational Policy June 2007 19 5. To agree an MDT operational policy for the delivery of haematological cancer services across North Wales based on current national guidance and accepted best clinical practice. To ensure this policy is reviewed and updated annually. 6. To ensure that clinical services are delivered in accordance with the MDT operational policy 7. To agree with all relevant parties optimum patient pathways, referral guidelines and clinical guidelines for each disease type and ensure these guidelines are reviewed and updated annually. 8. To agree an annual audit programme and ensure its outcomes are reviewed. 9. To agree a minimum data set for haematological malignancies and ensure mechanisms are in place to collect and review this data 10. To agree a list of recognised clinical trials and ensure consistent mechanisms are in place to assess all cancer patients for eligibility into clinical trials. 11. To ensure the MDT and local clinical teams review service improvement opportunities and embed them within clinical operational practice wherever possible. 12. To identify appropriate training needs of all members of the multi-disciplinary team, and agree at regular intervals how to meet these needs. 13. To work with other members of the MDT to ensure patient and carer views of the service are taken into account when planning and delivering services. 14. To ensure any MDT wide clinical governance issues raised by local clinical teams are addressed by the core MDT 15. To agree an annual work programme for the MDT 16. To advise the North Wales Cancer Network Board on issues likely to affect the strategic development of haematological cancer services. 6. TENURE: The post is tenable for a period of up to five years from the date of acceptance. Signed Signed …………………………………………………. …………………………………………… Date: …………………………………………... Date: …………………………………….. Final Draft - Haematology Operational Policy June 2007 20