Summary of NICE and Welsh skin MDT standards
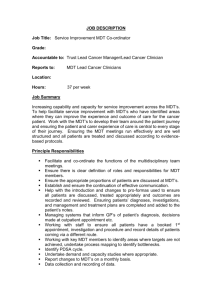
advertisement
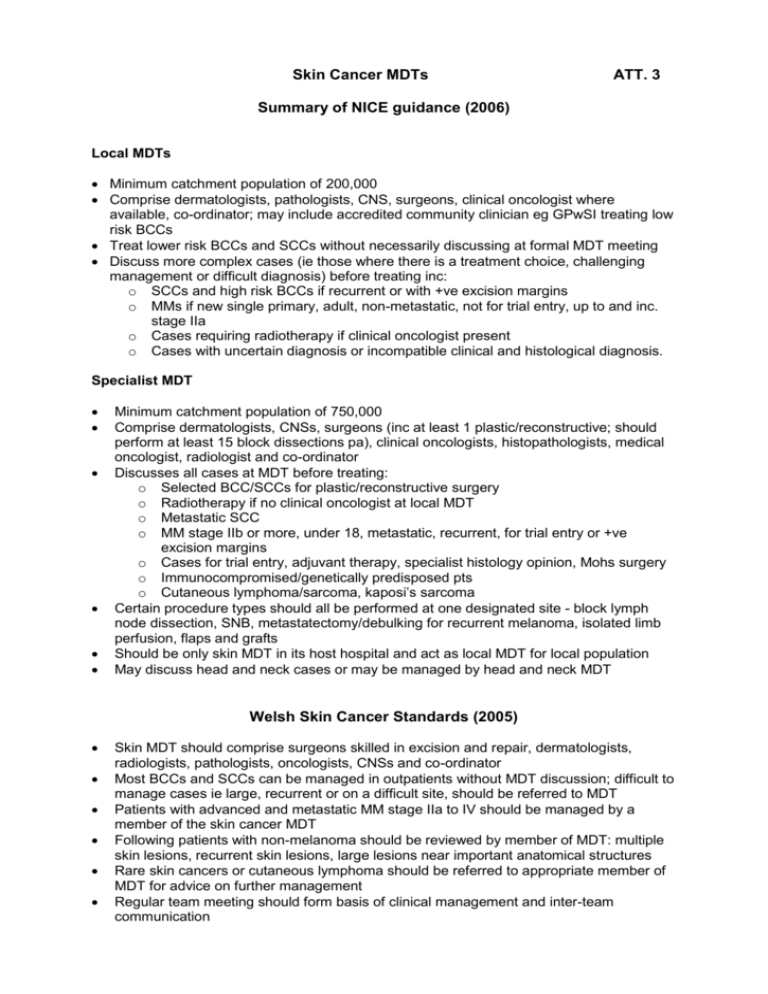
Skin Cancer MDTs ATT. 3 Summary of NICE guidance (2006) Local MDTs Minimum catchment population of 200,000 Comprise dermatologists, pathologists, CNS, surgeons, clinical oncologist where available, co-ordinator; may include accredited community clinician eg GPwSI treating low risk BCCs Treat lower risk BCCs and SCCs without necessarily discussing at formal MDT meeting Discuss more complex cases (ie those where there is a treatment choice, challenging management or difficult diagnosis) before treating inc: o SCCs and high risk BCCs if recurrent or with +ve excision margins o MMs if new single primary, adult, non-metastatic, not for trial entry, up to and inc. stage IIa o Cases requiring radiotherapy if clinical oncologist present o Cases with uncertain diagnosis or incompatible clinical and histological diagnosis. Specialist MDT Minimum catchment population of 750,000 Comprise dermatologists, CNSs, surgeons (inc at least 1 plastic/reconstructive; should perform at least 15 block dissections pa), clinical oncologists, histopathologists, medical oncologist, radiologist and co-ordinator Discusses all cases at MDT before treating: o Selected BCC/SCCs for plastic/reconstructive surgery o Radiotherapy if no clinical oncologist at local MDT o Metastatic SCC o MM stage IIb or more, under 18, metastatic, recurrent, for trial entry or +ve excision margins o Cases for trial entry, adjuvant therapy, specialist histology opinion, Mohs surgery o Immunocompromised/genetically predisposed pts o Cutaneous lymphoma/sarcoma, kaposi’s sarcoma Certain procedure types should all be performed at one designated site - block lymph node dissection, SNB, metastatectomy/debulking for recurrent melanoma, isolated limb perfusion, flaps and grafts Should be only skin MDT in its host hospital and act as local MDT for local population May discuss head and neck cases or may be managed by head and neck MDT Welsh Skin Cancer Standards (2005) Skin MDT should comprise surgeons skilled in excision and repair, dermatologists, radiologists, pathologists, oncologists, CNSs and co-ordinator Most BCCs and SCCs can be managed in outpatients without MDT discussion; difficult to manage cases ie large, recurrent or on a difficult site, should be referred to MDT Patients with advanced and metastatic MM stage IIa to IV should be managed by a member of the skin cancer MDT Following patients with non-melanoma should be reviewed by member of MDT: multiple skin lesions, recurrent skin lesions, large lesions near important anatomical structures Rare skin cancers or cutaneous lymphoma should be referred to appropriate member of MDT for advice on further management Regular team meeting should form basis of clinical management and inter-team communication