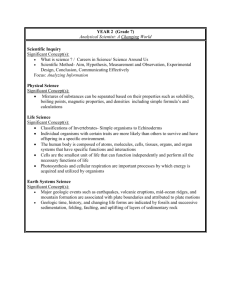
Information for the ward regarding KPC carbepenemase producers
advertisement

Information for Wards regarding KPC carbepenemase producers What are they : These are bacteria (usually E.coli or Klebsiella pneumoniae) which are normally found in the GI tract. In colonized patients the bacteria have acquired a set of genes that make them resistant to multiple antibiotics. The most concerning is resistance to the carbepenems (meropenem, ertapenem etc) which we use for serious gram –ve infections as organisms are almost always sensitive to these antibiotics. They are resistant to all penicillins and combination penicillins (coamoxiclav/ tazocin). They are usually sensitive to tigecycline and gentamicin and may also be sensitive to ciprofloxacin. There are rare cases where these organisms have become resistant to almost all antibiotics currently in use. Where have the come from : KPC strains are known to be a problem in the US, India, China and elsewhere. These organisms are slowly becoming endemic in the North West region over the past 2 years but are rare in the rest of the UK. It is not known how they entered the hospital environment originally. Patients in Stepping Hill will have acquired the organism while admitted to one of the other hospitals in the region. So far we have not had any new cases acquired at this hospital. Infection Prevention : These organisms will be part of the bacterial flora colonising the patients GI tract. They can also colonise the urinary tract, especially in patients with catheters or abnormalities of the urinary tract. These bacteria do not survive well in the environment. PPE when attending to the patient is important. Care should be taken when handling urine/ faeces or equipment contaminated by these bodily fluids. Standard cleaning of the patient environment and contaminated equipment is sufficient as these organisms do not survive long in the external setting. The patient should be isolated and ideally have their own toilet/showering facilities. Cross infection is most likely to be due to contamination of the hands of staff or relatives. Staff or relatives can carry the bacteria to other patients who then become colonized, if handwashing is poor. Good hand hygiene and use of PPE are therefore critical in stopping the spread of these organisms. Alcohol gel is active against these organisms. At present we don’t know if patients become decolonised over time. We treat them as colonised for their whole admission and any future admissions. Patients carrying this organism are one of our highest priorities for isolation, the other being active C.difficile disease. Patients are screened by rectal swabs. At present we only screen if a patient has been in prolonged contact with another colonized patient. Disease : Most patients are colonised but have no symptoms. Some patients will present with urinary tract infections, which will be difficult to treat as the organism is usually resistant to oral options and the majority of iv options. The organism can also be a problem if patients have intra-abdominal sepsis or require abdominal surgery. Intravascular line sepsis has also occurred with these organisms. The other vulnerable group of patients are the immunosuppressed. In all these cases antibiotic choice will be severely limited and sub-optimal. These organisms can also colonise wounds and ulcers but should not be a problem with intact skin. Important points : This is a new emerging problem so infection control is vital. So far we have had NO in-hospital spread at Stepping Hill Hospital. However these organisms can become endemic and spread throughout a hospital, as has happened in other parts of the region. It is vitally important therefore to adhere to use of PPE and good cleaning of all contaminated equipment. The organism is easily removed from surfaces and does not survive well in the external environment. It is staff and relatives who are the main risk for transferring these organisms to other patients, mainly on their hands. Alcohol gel is adequate for unsoiled handwashing. Treatment options are severely limited and sub-optimal for any patient who develops infection with these organisms. Therefore our best defence is PREVENTION of cross-infection. We have no idea if patients ever become decolonised and there is no straightforward way to attempt decolonization. Patients are therefore considered to be colonized for the whole of their current admission and any future admissions. Further Information For further information please contact either the Microbiology Department (xt.4491) or the Infection Prevention Team (xt.4669) Alternatively the authors of this information sheet can be contacted by email : Dr. D Scarr (Microbiology ST2) : dominic.scarr@stockport.nhs.uk Dr. S. Maxwell (Consultant Microbiologist) : sarah.maxwell@stockport.nhs.uk Dr. Moira Taylor (Consultant Microbiologist) : moira.taylor@stockport.nhs.uk