Outline - Transplant Hepatology Fellowship Program MOT/UHN
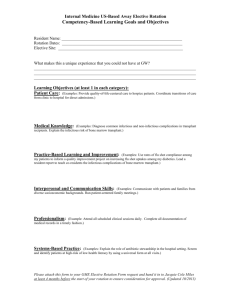
advertisement

TRANSPLANT HEPATOLOGY FELLOWSHIP PROGRAM Multiorgan Transplant Program (MOT), University Health Network/Toronto General Hospital, University of Toronto, Toronto, Canada Contact: Dr. Eberhard L. Renner, M.D., FRCPC, Professor of Medicine, Director GI Transplantation, NCSB 11C-1238 attn. Ms. Kimberley Burke, Administrative Coordinator, phone (416) 340-5221 or E-mail Kimberly.Burke@uhn.on.ca Transplant Hepatology Fellowship Program ER 2/12/2016 SUMMARY Introduction There is increasing demand for physicians experienced in treating patients pre-, peri- and post-liver-transplantation. Expertise in Transplant Hepatology requires training beyond what is typically offered in a Gastroenterology/Hepatology fellowship. The Liver Transplant Program at the Multiorgan Transplant Program (MOT)/University Health Network (UHN) offers this additional training in a Transplant Hepatology Fellowship. Goals of the Program: to provide training in all aspects of (academic) liver transplantation to enable the successful candidate to become an independent (academic) Transplant Hepatologist. Setting: The liver transplant program at UHN performs annually approx. 150 liver transplants (of which approx. 50 are live donor transplants) and follows more than 1’200 liver transplant recipients long-term. It is run by 6 full time staff surgeons and 5 full time staff hepatologists. There are 3-5 transplant hepatology fellowship positions (staff/fellow ratio of >1:1). Clinical services include inpatient (ward, intermediate and intensive care units) and outpatient activities (assessment, pre- and post-transplant Clinics, day care unit). In addition to patient management conferences, the program offers weekly a number of formal teaching events and ample opportunity to participate in ongoing clinical/lab-based research. Profile of Applicants: Interest in liver transplantation in an academic setting Medical license (in Canada or country of origin) Subspecialty training in Gastroenterology/Hepatology completed (in Canada or country of origin) Willingness to participate in in-hospital night-time on-call schedule for Multiorgan Transplant ward (approx. 4 nights per month). Start date: Jan 1st or Jul 1st. Duration: Two years (one year possible for selected candidates, depending on previous training and references; candidates seeking a two year training opportunity will be given preference) Stipend: Approx. CAD 60’000 a year. Application: Interested physicians should send a short cover letter stating the reason for applying, an updated CV (including list of publications) and three letters of support to: Eberhard L. Renner, M.D., FRCP(C) Professor of Medicine Director GI Transplantation University of Toronto Toronto General Hospital/NCSB 11C-1238 585 University Ave. Toronto, ON Canada M5G 2N2 Phone: (416) 340-5221 E-mail: Eberhard.Renner@uhn.on.ca 2/19 Transplant Hepatology Fellowship Program ER 2/12/2016 TABLE OF CONTENTS Introduction p. 4 Setting p. 4 Goals of the Program p. 4 General Learning Objectives p. 4 Profile of Applicants p. 5 Number of Fellowship Positions p. 5 Start date p. 5 Duration p. 5 Stipend p. 5 Application Process p. 5 Overall Structure of Program p. 6 Rotation Scheme P. 6 Mentoring p. 6 Evaluation of Fellows p. 7 Evaluation of Fellowship Program p. 7 Members of Education Committee p. 7 APPENDIX I: Specific Learning Objectives p. 8 APPENDIX II: Schedule of Main Activities within Rotations p.11 APPENDIX III: Questionnaire for Periodic Evaluation of Program by Fellows p.15 APPENDIX IV: Evaluation for Transplant Hepatology Fellows p.18 APPENDIX V: Template for Advertisement p.19 3/19 Transplant Hepatology Fellowship Program ER 2/12/2016 FELLOWSHIP PROGRAM IN TRANSPLANT HEPATOLOGY – Liver Transplant Program, MOT, UHN/University of Toronto Introduction There is increasing demand for physicians experienced in treating patients pre-, peri- and post-liver-transplantation. Expertise in Transplant Hepatology requires training beyond what is typically offered in a Gastroenterology/Hepatology fellowship. In the US, the American Board of Internal Medicine has recently accredited a subspecialty policy for Transplant Hepatology. The Liver Transplant Program at the Multiorgan Transplant Program (MOT)/University Health Network (UHN) offers a Fellowship Program in Transplant Hepatology that is open to qualified national and international candidates. Setting: The liver transplant program at UHN performs annually approx. 150 liver transplants (of which approx. 50 are live donor transplants) and follows more than 1’200 liver transplant recipients long-term. It is uniquely embedded with other solid organ transplant programs (heart, lung, kidney, pancreas, small bowel) in an interdisciplinary organizational structure, the Multiorgan Transplant Program (MOT). The liver transplant program is run by 6 full time staff surgeons and 5 full time staff hepatologists. The clinical activity of all staff hepatologists focuses strictly on transplantation. There are 3-5 transplant hepatology fellowship positions, leading to a staff/fellow ratio of >1:1. Clinical services include inpatient (ward, intermediate care and intensive care unit) and outpatient activities (assessment, pre- and post-transplant Clinics, day care unit). In addition to patient management conferences such as weekly listing and live donor meetings, there are several regular teaching events including weekly MOT rounds and liver transplant seminars, as well as monthly clinical and research rounds, quality assurance rounds, liver pathology rounds, hepatobiliay rounds and journal club. There is ample opportunity to participate in ongoing clinical and/or lab-based research activities supervised/mentored by one of the staff hepatologists and/or surgeons. Goals of the Program: to provide training in all aspects of liver transplantation to enable the successful candidate to become an independent Transplant Hepatologist to further individual talents in research and/or education thereby providing the best possible basis for an academic carrier in Transplant Hepatology General Learning Objectives (for Specific Learning Objective see APPENDIX I) The successful candidate will be able to judge indications and contraindications of and to appropriately select patients for liver transplantation manage pre-transplant conditions/complications of chronic liver disease including portal hypertensive GI bleeding, portal hypertensive fluid retention, SBP and hepato-renal syndrome, hepatic encephalopathy, hepatic pruritus, hepatocellular carcinoma and other hepatobiliary malignancies, porto-pulmonary hypertension 4/19 Transplant Hepatology Fellowship Program ER 2/12/2016 and hepato-pulmonary syndrome, malnutrition and obesity in the liver transplant candidate, as well as underlying liver diseases such as chronic hepatitis B/C virus infection and metabolic liver disorders in the cirrhotic awaiting a transplant contribute to the interdisciplinary management of patients with fulminant hepatic failure apply the criteria for selection and allocation of donor organs (including live donor assessment) contribute to the interdisciplinary perioperative management of deceased and live donor liver transplant recipients (and live liver donors) manage medical issues of liver transplant recipients, including immunosuppression, acute and chronic rejection, infectious complications, metabolic consequences such as diabetes, dyslipidemia, hypertension and weight gain, renal dysfunction, as well as disease recurrence in the graft deal with ethical issues involved in deceased and live donor liver transplantation Profile of Applicants: Interest in an academic carrier as a Transplant Hepatologist Medical license (in Canada or country of origin) Subspecialty training in Gastroenterology/Hepatology completed (in Canada or country of origin) Willingness to participate in in-hospital night-time on-call schedule for Multiorgan Transplant ward (approx. 4 nights per month). Ideally, offer for an (academic) position to return to after completion of fellowship Number of Fellowship Positions: 3 –5 Start date Yearly, July 1 or January 1. Duration: Two years (one year possible for selected candidates, depending on previous training and references; candidates seeking a two year training opportunity will be given preference) Stipend: CAD 60’000 a year Application Process: Interested physicians should send a short cover letter stating the reason for applying, an updated CV (including list of publications) and three letters of support to Eberhard L. Renner, M.D., FRCP(C) Professor of Medicine Director GI Transplantation University of Toronto 5/19 Transplant Hepatology Fellowship Program ER 2/12/2016 Toronto General Hospital NCSB 11C-1238 585 University Ave. Toronto, ON Canada M5G 2N2 Phone: (416) 340-5221 E-mail: Eberhard.Renner@uhn.on.ca Applications must be received the latest one year prior to the planned start date. An education committee comprised of all staff transplant hepatologists will screen the applications, may ask for additional references and/or invite promising candidates for an interview (by phone if an interview in person is felt not to be feasible) and will decide on acceptance. Applicants will be notified about the decision the latest 6 months prior to the planned start date. Overall Structure of Program: Year one: o clinical focus with rotation through in-patient ward (including approx. 1/7 inhospital night-time on-calls) and outpatient Clinics o active participation in teaching events (presentations at internal seminars, rounds, case discussions etc.) o own clinical research project (or lab-based research depending on interest and previous training). Year two: o research focus with own clinical research project (or lab-based research project depending on interest and previous training) o rotation through in-patient ward (including approx. 1/7 in-hospital night-time on-calls) and outpatient Clinics o active participation in teaching events (presentations at internal seminars, rounds, case discussions etc.) Rotation Scheme (for detailed description of main activities see APPENDIX II): Monthly rotation through inpatient service, outpatient service and research/elective block. A detailed rotation schedule will be defined for each fellow by the program director at least 3 months in advance. Mentoring: Fellows will be mentored by a) the Program Director and b) the staff physician supervising their research project(s). The Program Director will conduct an entrance interview with all fellows during which specific training interests and carrier plan is discussed and each fellow’s personal goals for the fellowship are fixed in writing. This and regular evaluations (see below) assure that the goals of both, program and trainee are met. 6/19 Transplant Hepatology Fellowship Program ER 2/12/2016 Evaluation: Fellows: o Fellows will be evaluated by the supervising staff at 3 and 6 months after the start of the fellowship, and every 6 months thereafter. o The program director will compile these evaluations and discuss the compiled evaluation in person with the fellow. o Based on an entrance interview (cf. above) at the start of the fellowship, and the evaluation-discussions, fellow and program director will agree and fix in writing the aims for the individual fellow for the next time period. o At the end of the fellowship, fellows who at least meet expectations as an independent consultant in their final evaluation by the supervising staff (cf. APPENDIX IV) will get a certificate by the MOT/UHN acknowledging successful completion of the fellowship. Fellowship Program: o Structured evaluation of program (teaching events and teaching staff) by fellows using questionnaire (see APPENDIX III) every 6 months o Eliciting oral feedback from fellows during evaluation discussions (cf. above) and exit interview to be conducted by the Program Director with each fellow at the end of the fellowship. o Statistics on publication record of fellows during fellowship and carrier path thereafter o At least quarterly meetings of Education Committee to detect problems and improve/solve them Members of Education Committee: Dr. Gary Levy Dr. Les Lilly Dr. Eberhard Renner (acting director of fellowship program) Dr. Nazia Selzner Dr. George Therapondos 7/19 Transplant Hepatology Fellowship Program ER 2/12/2016 APPENDIX I Specific Learning Objectives Clinical Skills Takes history, does physical and arrives at appropriate differential diagnosis in pre-, peri- and post-liver transplant patients. Orders laboratory, radiological and other diagnostic procedures including liver biopsy in a medically appropriate and cost-effective way; demonstrates knowledge in the interpretation of these investigations. Arrives at an acceptable plan of management, demonstrating knowledge in the non-operative and operative treatment of the disease process. Manages patients in the ambulatory setting, demonstrating knowledge of common office techniques and procedures. Manages the patient throughout the entire in-hospital course, demonstrating knowledge of common office techniques and procedures. Provides a plan for patient discharge and follow-up. Cognitive Knowledge Knows the principles of organ allocation and the ethical issues involved Knows the principles of liver preservation, including mechanisms of preservation and reperfusion injury Knows indications and contraindications of liver transplantation Knows immunology and pathology of rejection, and the mechanisms of action of immunosuppressive drugs Knows the epidemiology, clinical presentation, diagnosis and therapy of transplant-related postoperative complications including infections, tumors, immunosuppression-related complications and recurrence of underlying diseases in the graft. Knows the ethical questions and positions relevant to liver transplantation. Technical Skills Adds to experience with liver biopsy Adds to experience with paracentesis Adds to experience in upper GI endoscopy including treatment of portal hypertensive varices Adds to experience in diagnostic lower GI endoscopy Communicator Obtains and synthesizes the relevant history from patients, their families and the community Demonstrates an appreciation of the unique relationship between transplant patients and their families and be able to deal effectively and compassionately with patients and family members by establishing therapeutic relationships. Demonstrates an appreciation of the psychological needs of transplant patients. 8/19 Transplant Hepatology Fellowship Program ER 2/12/2016 Listens effectively Demonstrates effective communication skills including oral presentations at rounds and conferences. Writes or dictates timely meaningful notes and reports on all patients Can summarize a patient’s condition concisely Presents consults verbally in an understandable way Communicates effectively and empathetically with his/her patients and their families. Can conduct a family meeting effectively. Can and does discuss treatment plans with the charge nurse on the team. Communicates treatment plans to all members of the team so that they understand. Demonstrates skill in working with others who present significant communication challenges such as ethno-cultural background different from the physician’s own, anger or confusion Collaborator Consults effectively with other physicians and health care professionals. Contributes effectively to other interdisciplinary team activities. Uses the team approach in the management of complex patients effectively. Demonstrates respects for ancillary staff Participates in discharge planning rounds Manager Utilizes resources effectively to balance patient care, personal learning needs, and outside activities. Does notes and dictations appropriately and in a timely fashion. Comes to morning rounds, clinics, teaching sessions and academic events on schedule/time. Books tests and procedures appropriately and efficiently. Multitasks appropriately and effectively, prioritizes tasks appropriately and understands the principles of effective delegation. Delegates responsibilities appropriately and/or accepts delegated tasks appropriately. Understands population-based approaches to health care services and their implication for medical practice and preordination to access. Maintains and demonstrates an up to date personal log of procedures. Health Advocate Identifies the important determinants of health affecting patients. Demonstrates an understanding of injury prevention. Recognizes and responds to those issues where advocacy is appropriate. Contributes to health-maintenance advocacy for patients, including such areas as smoking, alcohol and recreational drug use. 9/19 Transplant Hepatology Fellowship Program ER 2/12/2016 Understands the importance of organ donation and the strategies that can improve the opportunity for a patient and their family to donate. Scholar Develops, implements and monitors a personal continuing education strategy. Critically appraises sources of medical information. Facilitates learning of patients, house staff / students and other health care professionals through formal and informal teaching opportunities. Presents at rounds at a level relevant to year of training. Attends and participate in academic activities including Seminar, Rounds, Conferences and Journal Club. Contributes to development of new knowledge to foster the academic growth of the specialty of transplantation by participating in scholarly work. Professional Delivers the highest quality care with integrity, honesty and compassion. Exhibits appropriate personal and interpersonal professional behaviours. Has an ethical relationship with colleagues, patients, and relatives. Demonstrates sensitivity to age, gender, culture and ethnicity in dealing with patients and their families. Has a complete knowledge of the principles of biomedical ethics and medical jurisprudence. Has knowledge and understanding of the professional legal and ethical codes to which all physicians are bound. Recognizes and respects his/her own limitations of professional competence. Recognizes the importance of maintenance of competence and evaluation of outcomes. Understands the legal issues related to informed consent, confidentiality, and refusal of treatment. Has the ability to recognize, analyze and know how to deal with unprofessional behaviours in clinical practice, taking into account hospital, university and provincial regulations. Dresses appropriately and cleanly, arrives in time. Displays teamwork and respect for all members of the health care team. Answers pages and responds in a timely fashion. Maintains patient privacy and dignity and acts with personal integrity. 10/19 Transplant Hepatology Fellowship Program ER 2/12/2016 APPENDIX II Main Activities within Rotations 1. Inpatient Rotation (duration usually one month): o “Runs” the in-patient ward (incl. ACU) in (1-2 weekly) rotation with the surgical fellows (and, in some months, a rotating GI resident). Work starts at 0700 with the morning rounds and ends after sign-out rounds in the late afternoon. The responsibility for the ward is with the fellow on service for the week. If this is a surgical fellow/rotating GI resident, the transplant hepatology fellow participates in the morning/sign-out rounds and assists with the ward work during the day (this includes covering the ward during times the surgical fellow is in the OR). o works on research project o participates in educational events (cf. Table 1, bold print) Table 1: Daily Schedule of Activities during Inpatient Rotation: Morning Monday Tuesday 0700~1600 0700~1600 ward rounds/ inpatient care ward rounds/ inpatient care Wednesday 0700~0900 ward rounds 0800-0900 MOT rounds 0900~1600 ward rounds/ inpatient care Thursday Friday 0700- 0800 Liver TPL Seminar 07000900 ward rounds 0800~1600 ward rounds/ inpatient care 0900-1000 Listing meeting Saturday (if 1. call) Sunday (if 1. call) 0700approx. 1200 0700approx. 1200 ward rounds/ inpatient care ward rounds/ inpatient care ~1600 sign-out rounds ~1600 sign-out rounds 1000~1600 inpatient care Afternoon ~1600 sign-out rounds ~ 1600 sign-out rounds 1830- … HB rounds (monthly) 1830- … ~1600 sign-out rounds ~ 1500 sign-out rounds 1600-1700 Clinical/ Research/ QA Rounds ~1600 sign-out rounds JC (monthly) 11/19 Transplant Hepatology Fellowship Program ER 2/12/2016 2. Outpatient Rotation (duration usually one month): o participates in Assessment Clinic (Tuesday afternoon), Pre-transplant Clinic (Wednesday afternoon) and post-transplant Clinics (Monday morning, Wednesday morning, Thursday morning) o works on research project o participates in educational events (cf. Table 2, bold print) Table 2: Daily Schedule of Activities during Outpatient Rotation: Morning Monday Tuesday Wednesday Thursday 0800-0900 Liver Path Rounds 0800-0900 Live Donor Meeting 0800-0900 MOT Rounds 0900-1200 Interventions (with LL) 0900-1200 Post-OLT Clinic (with ER) 0700- 0800 Liver TPL Seminar 0900-1300 Post-OLT Clinic (with LL) 0900-1200 Post-OLT Clinic (with GT) Friday 0900-1000 Listing meeting 0800-1200 Endoscopy (with LL) and/or intervention (with TG) Afternoon 1200-1600 Assessment Clinic (with LL, ER, GT) 1830- … HB rounds (monthly 1300-1600 PreOLT Clinic (with LL, ER, GT) 1600-1700 Clinical/ Research/ QA Rounds 1830- … JC (monthly) 3. Research Rotation (duration typically one month): o works on research project o participates in educational events (cf. Table 3, bold print) o provided progress in assigned research project is deemed satisfactory, this rotation may also be used for an elective; electives are chosen and individually arranged after discussion with the program director in areas related to liver transplantation such as to hepatopathology or transplant ID; discussions must start at least 3 months in advance. 12/19 Transplant Hepatology Fellowship Program ER 2/12/2016 Table 3: Daily Schedule of Activities during Research Rotation: Monday Morning Tuesday 0800-0900 Liver Path rounds Wednesday Thursday 0800-0900 MOT Rounds 0700- 0800 Liver TPL Seminar Friday Afternoon 1600-1700 Clinical/ Research/ QA Rounds 1830- … HB rounds (monthly 1830- … JC (monthly) Other Activities Independent of the above rotations, fellows will take approx. 1/7 in-house night calls for MOT participate in other rounds/conferences/teaching activities, as time permits work by themselves through the most recent Transplant Hepatology CAQ Review Course electronically available (http://www.amedcoesystems.com/presentations/aasld/index.html) develop/lead the research project that is assigned to them by the program director in consultation with the staff hepatologists (one of whom will serve as mentor); aim: at least one presentation at an international meeting and at least one publication per year. Holidays, Meeting Attendance and Sick Leave Fellows are allowed to take 20 working days a year as holidays (missed on-call nights must be compensated prior or after); the start/end date of any holiday break or other foreseeable absence (meetings) from the service has to be coordinated with/approved by the program director 6 months in advance. Meeting attendance: Fellows are encouraged to submit abstracts on their research projects to the pertinent international (AASLD, ATC, ILTS) and/or national (CASL, CTS) meetings. The program will (at least partially) support the attendance of one meeting per year for each fellow, provided the work of the fellow has been accepted 13/19 Transplant Hepatology Fellowship Program ER 2/12/2016 for presentation. The fellow must seek pre-approval of expenses (travel, hotel and meeting registration) with the program director at least 3 months in advance. In order re-imbursement of pre-approved expenses can proceed, the fellow must supply the program director with originals of receipts (including boarding passes, hotel, meeting registration). Fellows with sick leaves exceeding a total of 30 working days during a calendar year will automatically fail that fellowship year; this can be appealed with the Educational Committee (attn. program director), provided it was attributable to exceptional circumstances such as a serious illness or accident and the fellow’s overall performance, as determined by the majority of evaluations for that year exceeds expectations. 14/19 Transplant Hepatology Fellowship Program ER 2/12/2016 APPENDIX III Questionnaire for Periodic Evaluation of Program by Fellows 1. During the past period of rotation, my training expectations were please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 2. During the past period of rotation, the balance between clinical duties, research and teaching was overall please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 3. During the past period of rotation, I experienced the clinical duties assigned to me as please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 4. During the past period of rotation, I experienced the formal and bedside teaching as please, specify …………………………………………………………….. 15/19 Transplant Hepatology Fellowship Program ER 2/12/2016 …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 5. During the past period of rotation, I experienced the time/effort required for preparing presentations at seminars and rounds etc. as please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 6. During the past period of rotation, I experienced the time/opportunity for developing/pursuing my research projects as please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 7. During the past period of rotation, I experienced the overall atmosphere within the team/program as please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 8. During the past period of rotation, I experienced the interaction of staff physicians/surgeons and allied health cares professionals with me as 16/19 Transplant Hepatology Fellowship Program ER 2/12/2016 please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 9. During the past period of rotation, I felt that my efforts of reaching my training goals were overall please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. please, specify …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. 10. During the last period of rotation, I recognized the following as additional weakness of the fellowship program …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. and have the following suggestion for improvement …………………………………………………………….. …………………………………………………………….. …………………………………………………………….. THANK YOU FOR YOUR FEEDBACK! 17/19 Transplant Hepatology Fellowship Program ER 2/12/2016 APPENDIX IV: Evaluation of Transplant Hepatology Fellows CanMEDs Roles (Listed overleaf) Unsatis -factory Needs to improve Meets expectations Exceeds expectations Outstanding Not applicable Basic science knowledge 1, 6 Critical evaluation of scientific papers 1, 6 7 1 2, 3, 7 6 All CRITERIA A. FUNDAMENTAL SKILLS Clinical knowledge & skills 1 Research protocol execution 6 Quality of written & oral reporting Skilled use of equipment 2, 6 B. EMERGENCY CARE Performance under emergency conditions C. PROFESSIONAL ATTITUDE Ethical standards (eg, recognizes & addresses moral and ethical issues) Equity issues (eg, sensitive to gender, culture, etc) Physician-Patient relationship 7 2, 7 Team relationship 2, 3, 7 Sense of responsibility 4, 5, 7 Self-assessment ability 7 Self-directed learning 1, 6, 7 D. RESEARCH & LABORATORY SKILLS Grant writing ability 4, 6 Technical Skills (research design, data gathering, etc) 6, 7 Ability to address ethical issues in research 6 E. SCHOLARLY ACTIVITY Publication (preparation, abstracts submitted, publication) 1, 6 Quality of presentations 1, 6 Participation / Attendance in Grand Rounds 6, 7 Ability to function as an independent researcher F. TEACHING PERFORMANCE 3, 4, 5, 6 G. OVERALL COMPETENCE Ability to function as an independent consultant H. CERTIFICATE: Should a certificate be issued for this trainee upon completion? Yes No 18/19 Transplant Hepatology Fellowship Program ER 2/12/2016 APPENDIX V: Template for Advertisement TRANSPLANT HEPATOLOGY FELLOWSHIP Multiorgan Transplant Program, University Health Network/Toronto General Hospital, University of Toronto, Toronto, Canada We invite applications for x Transplant Hepatology Fellowship positions starting Jan 1/July 1, 200x. With annually approx. 150 liver transplants (of which approx. 50 are live donor transplants) and its unique organization within an interdisciplinary Multiorgan Transplant Program, our Liver Transplant Program not only offers training in all clinical aspects of transplant hepatology, but also ample opportunity for clinical and/or lab-based research. Goals of the Program: to provide training in all aspects of (academic) liver transplantation to enable the successful candidate to become an independent (academic) Transplant Hepatologist. Profile of Applicants: Interest in liver transplantation in an academic setting Medical license (in Canada or country of origin) Subspecialty training in Gastroenterology/Hepatology completed (in Canada or country of origin) Willingness to participate in in-hospital night-time on-call schedule for Multiorgan Transplant ward (approx. 4 nights per month). Start date: Jan 1/July 1, 200x. Duration: Two years (one year possible for selected candidates, depending on previous training and references; candidates seeking a two year training opportunity will be given preference) Stipend: Approx. CAD 60’000 a year. Application: Interested physicians should send a short cover letter stating the reason for applying, an updated CV (including list of publications) and three letters of support to: Education Committee attn.: Eberhard L. Renner, M.D., FRCP(C) Professor of Medicine Director GI Transplantation University of Toronto Toronto General Hospital NCSB 11C-1238 585 University Ave. Toronto, ON Canada M5G 2N2 Phone: (416) 340-5221 E-mail: Eberhard.Renner@uhn.on.ca Applications must be received by x. The Education Committee may invite promising candidates for an interview and will decide on acceptance. Applicants will be notified by x. 19/19