Molecular-workshop
advertisement

Cellular Genomics
Cellular Genomics is a technology platform that uses known DNA sequence
information to design products that can detect genetic changes associated with
disease. This platform is especially useful for the detection of cancer since
cancer does not occur without genetic change. Some examples of the genetic
changes associated with cancer include chromosome aneuploidy, chromosome
translocations/rearrangements, deletions, or amplifications. Aneuploidy - a
condition where the number of chromosomes in a cell differs from the normal
diploid number (two copies of each chromosome, 46 total) by loss or duplication
of chromosomes.
Translocation - a condition where part of a chromosome is detached by
breakage and then becomes attached to some other chromosome.
Deletion - a condition where a sequence of DNA along a chromosome is
removed and the regions on either side become joined together.
Amplification - - refers to the production of additional copies of a chromosomal
sequence, which may then be present on the same or a different chromosome.
Norma l
Deletion
Mutation
Rearrangement
Replication
Amplification
FISH
Fluorescence in situ hybridization (FISH) is a type of hybridization in which a
DNA "probe" is labeled with fluorescent molecules so that it can be seen with a
microscope. The word "in situ" means that the hybridization occurs "in place", in
this case, within the nucleus of specimen cells that have been fixed to a
microscope slide.
To conduct a FISH analysis, one warms fixed cells mounted on a microscope
slide to unwind their chromosomal DNA and allow access of the DNA probe.
After adding the probe, the specimen cells are then cooled to allow the DNA
probe to hybridise with its complementary target DNA. Once hybridised, the
fluorescent molecules on the probe will show precisely where their target DNA
lies along a chromosome. Depending upon the design of the probe DNA, one
can detect many types of genetic changes.
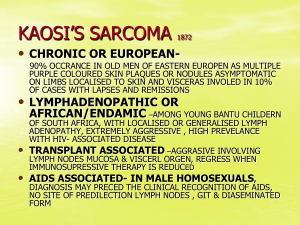
What is Ewing's sarcoma / PNET ?
Ewing's sarcoma is a cancer. The cancer can start in bone or in soft tissues. The
most common sites for Ewing's sarcoma are the pelvis, the thigh, and the trunk of
the body. The peak ages are between 10 and 20, but younger children and older
adults can also get Ewing's sarcoma. We do not know exactly what kind of cell
gives rise to Ewing's sarcoma. It has some features that resemble the early cells
that would normally develop into part of the nervous system. Ewing's sarcoma
has unknown aetiology.
The most common early signs of Ewing's sarcoma are pain and swelling. Like
other sarcomas, Ewing's sarcoma can spread to other parts of the body. Even
when the tumour is detected at a very small size, there may be evidence of
microscopic spread.
For this reason, Ewing's sarcoma always requires treatment to the whole body.
This treatment includes chemotherapy. Chemotherapy is intended to destroy the
tumour cells which have spread to the rest of the body and to shrink the main
mass of tumour cells. Successful treatment also requires another form of
treatment to the main mass of tumour. This can be surgery, radiation therapy, or
a combination of the two.
What are the symptoms of Ewing's sarcoma ?
Symptoms of Ewing's sarcoma vary from person to person and depending on the
location and size of the cancer. The most common symptoms are pain and
swelling or tenderness in the affected area. Pain may become very intense when
the tumour is located near important nerves, like in the sacrum, pelvis or spine.
Swelling is often seen, especially when the log bones of the arms or legs are
affected.
Sometimes the tumour can interfere with movement and can weaken the bones,
occasionally leading to a fracture. Other symptoms of cancer may include
tiredness, fever, weight loss, and anaemia. None of these symptoms is a sure
sign of cancer; if you suspect you have a health problem consult your doctor.
Is primitive neuroectodermal tumour (PNET) different
to Ewing's sarcoma ?
Peripheral primitive neuroectodermal tumours (PNET, or more correctly pPNET)
start in bone or soft tissues. Like Ewing's sarcoma (ES) they are composed of
small-blue-round cells.
They differ from ES in that they show more developed features of cells
associated with the nervous system.
Genetic analyses show that both pPNET and ES share a unique genetic
alteration, an exchange of material between chromosomes 11 and 22. Also, ES
and pPNET have a similar response to chemotherapy. Based on these and other
similarities Ewing's sarcoma and pPNET are regarded as closely related
members of the same family of tumours.
Treatment for pPNET is the same as that for Ewing's sarcoma.
Note: brain tumours are also frequently referred to as primitive neuroectodermal
tumours (PNET). These are very different to pPNET of bone; they do not share
the same 11;22 translocation and require different treatments.
Is Ewing's sarcoma a childhood or an adult disease ?
Approximately half of all people with Ewing's sarcoma of bone are under 15
years of age at diagnosis. However, it is also common in young adults. The peak
ages are between 10 and 20. It is less common before the age of 5 and after the
age of 30. Sometimes young adults may be treated by a "paediatric" oncologist
because of the doctor's experience with treating this type of cancer.
The figure above shows the age distribution for over 900 people with Ewing's
sarcoma of bone registered with clinical trial groups in Germany and the UK.
t(11;22)(q24;q12) EWS-FLI1 Translocation in Ewing's Sarcoma
The t(11;22)(q24;q12) translocation is present in over 90% of Ewing's sarcoma
cases. The resulting EWS-FLI1 fusion gene has been demonstrated to have
oncogenic potential. Many alternative forms of the translocation exist,
corresponding to variations in the locations of the EWS and FLI1 breakpoints.
The most common form, "Type 1", accounts for approximately 60% of cases and
consists of the first seven exons of EWS joined to exons 6-9 of FLI1.
"Type 2", accounts for approximately 25% of cases and also includes FLI1 exon
5. The type of translocation has been related to prognosis.
Primitive Neuroectodermal Tumor (PNET)/Ewing’s Sarcoma t(11;22) FISH
Probe
Each nucleus from neoplastic PNET/Ewing’s sarcoma cells contain a single
normal allele with characteristic red-yellow-green signal. A translocation involving
the EWSR1 gene on chromosome 22q21 results in the breakapart of the normal
allele, resulting in single red and single green signals (highlighted by arrows).
Normal cells contain 2 normal alleles with characteristic red-yellow-green signals.
What is it?
Rearrangements involving the EWSR gene on chromosome 22 {i.e. t(11;22)} are
unique to, and define PNET/Ewing’s sarcoma. Confirmation of this diagnosis can
now be made with high sensitivity and specificity via the t(11;22) FISH assay,
which is a dual color, breakapart translocation probe.
Soft tissue tumors: Synovial sarcoma
Synovial sarcoma is a rare soft tissue sarcoma with features of epithelial
differentiation. In contrast with its name, synovial sarcoma is not associated with
synovial joints. It tends to arise in younger patients with a mean age of
approximately 30 years.
Problem: Synovial sarcoma is a high-grade tumor but typically is associated with
a history of a long-standing nodule, sometimes present for years, which has
increased rapidly in size over a few months. Therefore, it is sometimes
overlooked. The tumor spreads along fascial planes and, thus, can be much
more widespread than apparent on initial evaluation.
Frequency:
Synovial sarcoma is rare, representing approximately 5-10% of all soft
tissue sarcomas.
Approximately 800 new cases occur in the United States per year.
Females are more commonly affected than males.
Etiology: Synovial sarcoma is characterized by a specific chromosomal
translocation t(X;18)(p11;q11) that is observed in more than 90% of cases. This
defect appears to be the underlying cause of the tumor, although how the
resulting fusion protein leads to transformation is poorly understood.
Pathophysiology: The t(X;18)(p11;q11) translocation fuses the SYT gene from
chromosome 18 to either of 2 homologous genes at Xp11, either SSX1 or SSX2.
The fusion proteins SYT-SSX1 and SYT-SSX2 are believed to function as
aberrant transcriptional regulators, resulting in either activation of
protooncogenes or inhibition of tumor suppressor genes. The downstream
targets of these fusion proteins that lead to transformation have not been
identified.
A correlation appears to exist between the histologic subtype of the tumor and
either of the 2 fusion proteins. Biphasic tumors, containing both epithelial and
spindle cell components, express the SYT-SSX1 transcript while monophasic
tumors with only a spindle cell component may express either transcript.
Clinical: Synovial sarcoma usually presents within the first 3 decades of life and
generally is associated with a history of a small nodule that has increased rapidly
in size. The mass often is painful and is located deep. Most commonly, it is
situated around the knee, but it also can appear in the hands and feet
Caption: Picture 1. Lateral radiograph depicts a synovial sarcoma of the dorsum of
the hand. A small nodule, present for 5 years, rapidly enlarged to the present size
over 2 months.
Picture Type: X-RAY
Caption: Picture 2. T1-weighted MRI depicts a synovial sarcoma of the dorsum of
the hand. The tumor has low signal on T1 weighting
Picture Type: MRI
Caption: Picture 3. T2-weighted MRI depicts a synovial sarcoma of the dorsum of
the hand. The tumor has a heterogeneous signal on T2 weighting indicative of a
variable growth pattern.
Picture Type: MRI
Synovial Sarcoma t(x;18) FISH Probe
Each nucleus from neoplastic synovial sarcoma cells contain a single normal
allele with characteristic red-yellow-green signal. A translocation involving the
SYT gene on chromosome 18q11.2 results in the breakapart of the normal allele,
resulting in single red and single green signals (highlighted by arrows). Normal
cells contain 2 normal alleles with characteristics red-yellow-green signals.
What is it?
Rearrangements involving the SYT gene on chromosome 18 {i.e. t(x;18)} are
unique to, and ultimately define synovial sarcoma. Confirmation of this diagnosis
can now be made with high sensitivity and specificity via the t(x;18) FISH assay,
which is a dual colour, breakapart translocation probe.
Clinical contexts in which it is useful:
Synovial sarcomas (SS) account for roughly 5 per cent of soft tissue sarcomas
and often arise in the limbs of young adults, although they can occur at any site
and over a broad age range. The histological diagnosis of SS can often be
challenging, as these tumors may resemble other sarcomas such as malignant
peripheral nerve sheath tumor and Ewing’s sarcoma. Moreover,
immunohistochemistry studies may be suboptimal in definitively establishing a
diagnosis, as the markers used (CD99, bcl-2) are not entirely specific and a
significant subset of SS has been shown to demonstrate no or focal
immunoreactivity for these markers. This problem is further exacerbated in the
limited material present in core needle biopsies.
The
identification of
a unique chromosomal translocations {i.e.
t(X;18)(p11.2;q11.2)} in more than 90% of SS cases has lead to the employment
of new genetic approaches that permit the rapid confirmation of the diagnosis.
The t(X;18)(p11.2;q11.2) involves the SYT gene on chromosome 18 and one of
several SSX genes (SSX1, SSX2 or SSX4) located on chromosome X and can
be readily detected by interphase fluorescent in situ hybridization (FISH). Dual
color, breakapart FISH assays provide a highly specific and sensitive method for
identifying chromosome 18 rearrangements {i.e. t(11;22)(q24;q12)} and have
been optimized for use on paraffin-embedded tissues. Unlike other genetic
approaches that often require a sufficient amount of material, FISH assays can
be performed on small biopsy sections. Moreover, interphase FISH assays
provide direct correlation of FISH results with histologic and immunophenotypic
features.
Follicular Lymphoma t 14:18
LSI BCL2 Dual Color, Break Apart Rearrangement Probe
Gallery of cell nuclei in a case of follicular lymphoma showing overlapping yellow
signals indicating presence of fusion of red (18q21) and green (14q32) signals
characteristic of a t(14;18)(q32;q21) translocation
H&E stained section of follicular lymphoma with vague nodular
architecture
Probe map for analysis of follicular lymphoma
Probe Image
Normal cell hybridization using the LSI BCL2 (18q21) Dual Color, Break Apart
Rearrangement Probe.
Abnormal cell hybridization using the LSI BCL2 (18q21) Dual Color, Break Apart
Rearrangement Probe.
• FOLLICULAR LYMPHOMAS TYPICALLY EXPRESS THE ANTI-APOPTOTIC
PROTEIN, BCL-2, AS A RESULT OF A t(14;18)(q32;q21) TRANSLOCATION
INVOLVING THE BCL-2 GENE ON CHROMOSOME 18 AND THE IMMUNOGLOBULIN
HEAVY CHAIN GENE ON CHROMOSOME 14.
• FLUORESCENCE IN SITU HYBRIDIZATION (FISH) ANALYSIS PROVIDES A
HIGHLY SENSITIVE (>93%) AND SPECIFIC (>95%) METHODOLOGY THAT IS
SUPERIOR TO PCR-BASED TECHNIQUES PERFORMED OUT OF PARAFFIN
SECTIONS FOR THE DETECTION OF THE t(14;18)(q32;q21) TRANSLOCATION
THAT IS THE SIGNATURE OF FOLLICULAR LYMPHOMA.
Breast Cancer
HER-2 DNA Probe Kit is designed to detect amplification of the HER-2/neu gene
via fluorescence in situ hybridization (FISH) in human breast cancer tissue
specimens.
Results currently used as prognostic factors in stage II, node-positive
breast cancer patients.
further indicated as an aid to predict disease-free and overall survival
patients with stage II node-positive breast cancer treated with adjuvant
cyclophosphamide, doxorubicin and 5-fluorouracil (CAF) chemotherapy.
FDA approved for selection of patients for whom Herceptin® therapy is
being considered.
HER-2/neu, also known as c-erbB2 or HER-2, is a gene that has been shown to
play a key role in the regulation of cell growth. The gene codes for a 185 kd
transmembrane cell surface receptor that is a member of the tyrosine kinase
family. HER-2 has been shown to be amplified in human breast, ovarian and
other cancers.
DNA Probe Description
The HER-2 DNA Probe Kit consists of two labeled DNA probes.
The HER-2 probe that spans the entire HER-2 gene is labeled in
SpectrumOrangeTM.
The CEP 17 probe is labeled in SpectrumGreen TM and hybridizes to the
alpha satellite DNA located at the centromere of chromosome 17
(17p11.1-q11.1).
Inclusion of the CEP 17 probe allows for the relative copy number of the
HER-2 gene to be determined.
Results of Hybridization
Results on enumeration of 20 interphase nuclei from tumor cells per target are
reported as the ratio of average HER-2/neu copy number to that of CEP 17.
specimens with amplification showed a LSI HER-2/neu and CEP 17 signal
ratio of ≥ 2.0;
normal specimens showed a ratio of less than 2.0.
Map not to scale
PathVysion HER-2 DNA Probe Kit hybridized to breast tissue
showing multiple copies of the HER-2 gene as represented by
multiple orange signals. The ratio of orange to green probe signals is
greater than 2.0 indicating HER-2 amplification.
Two green signals indicate the presence of two copies of chromosome 17.
Two orange signals indicate the presence of two copies of HER-2 genes in the
same nucleus. The ratio of HER-2 to CEP 17 is 1.0, which is non-amplified.
Three green signals indicate the presence of three copies of chromosome 17.
Approximately 13 orange signals indicate the presence of 13 copies of HER-2
genes in the same nucleus.
The ratio of HER-2 to CEP 17 is approximately 4,which is amplified.
Aneusomy in breast cancer has been well documented and is considered an
early event in breast carcinoma.
96% of malignant tumors showed aneusomy of one or more of
chromosome 1, 8,11, or 17,
no aneusomy in benign tumors.
The Breast Aneusomy Probe Set was designed as a research tool to help study
aneusomies and patterns of aneusomy that can provide important information as
it pertains to prognosis, progression, recurrence, and metastasis. This probe set
has been optimized for use in cytology specimens.
Results of Hybridization
This probe set is provided for those researchers interested in assessing
chromosome
copy
number
of
chromosome
1,
chromosome
8,
chromosome 11, and chromosome 17.
In a normal diploid cell two gold signals, two red signals, two green
signals, and two aqua signals should be observed (Figure 1).
In a normal diploid cell, two copies of each signal should be observed
(Figure 1). They include those for LSI 1 (two gold signals), CEP 8 (two red
signals), CEP 11 (two green signals), and CEP 17 (two aqua signals).
DNA Probe Description
The LSI 1 probe is an approximately 470 kb clone contig positioned at
1p12. The probe is direct labeled in SpectrumGoldTM.
The CEP 8 alpha satellite DNA probe hybridizes to the centromere region
of chromosome 8. The probe is direct labeled with SpectrumRed TM.
The CEP 11 alpha satellite DNA probe hybridizes to the centromere
region
of
chromosome
SpectrumGreenTM.
11.
The
probe
is
direct
labeled
with
The CEP 17 alpha satellite DNA probe hybridizes to the centromere
region
of
chromosome
17.
The
SpectrumAquaTM.
Breast Aneusomy Multi-Color Probe Set
probe
is
direct
labeled
with
Breast Aneusomy Multi-Color Probe Set
Normal results observed in an interphase cell obtained from a Fine Needle Aspirate
sample after the Breast Aneusomy probe hybridization. Each probe signal: LSI ® 1
(gold), CEP® 8 (red), CEP 11 (green), and CEP 17 (aqua) is present in 2 copies.
Aneusomic interphase cell obtained from a fine needle aspirate sample showing 3
copies of LSI 1(gold), 3 copies of CEP 8 (red), 3 copies of CEP 11 (green), and 4
copies of CEP 17 (aqua) after Breast Aneusomy probe hybridization.
BLADDER CANCER
The UroVysionTM Bladder Cancer Kit (UroVysion Kit) is designed to detect
aneuploidy for chromosomes 3, 7, 17 and loss of the 9p21 locus via
fluorescence in situ hybridization (FISH) in urine specimens from subjects
with transitional cell carcinoma of the bladder.
Results from the UroVysion Kit are intended for use as a noninvasive
method for monitoring for tumor recurrence in conjunction with cystoscopy
in patients previously diagnosed with bladder cancer.
DNA Probe Description
The UroVysion Bladder Cancer Kit probes are directly labeled with fluorophores.
The UroVysionTM Bladder Cancer Kit (UroVysion Kit) consists of three alphasatellite
repeat
sequence
probes;
CEP®
3
SpectrumRedTM,
CEP
7
SpectrumGreenTM and CEP 17 SpectrumAqua that hybridize to the centromere
regions of chromosomes 3, 7 and 17, respectively. In addition, a unique
sequence probe, LSI® p16 (9p21) SpectrumGold, is included that hybridizes to
the p16 gene at 9p21.
Results of Hybridization
Determination of results is conducted by enumeration of CEP 3, 7 and 17, and
LSI p16 (9p21) signals through microscopic examination of the nucleus.
Hybridization is viewed using a fluorescence microscope equipped with
appropriate excitation and emission filters allowing visualization of the red, green,
aqua and gold fluorescent signals. Samples hybridized with the UroVysion
Bladder Cancer Kit will exhibit signals indicative of the copy number of
chromosomes 3, 7 and 17 and of the p16 gene.
Normal result - interphase cell obtained from a bladder specimen
Each probe signal; CEP 3 (red), CEP 7 (green), CEP 17 (aqua) and LSI
9p21 (gold) is present in two copies.
Aneusomic interphase cell - bladder specimen.
two copies of chromosome 3 (red), four copies of chromosome 7 (green),
five copies of chromosome 17 (aqua) and one copy of region 9p21 (gold).