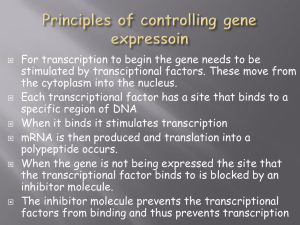
Introduction to Cardiology Transcription
advertisement

Introduction to Cardiology Transcription by Linda C. Campbell, CMT, AHDI-F The Cardiology Transcription Unit The SUM Program Cardiology Transcription Unit, 2nd edition, was developed to meet the growing demand for quality training in medical transcription. Providing four hours of authentic physician dictation, the unit is designed to simulate on-the-job training within an educational framework by presenting a variety of cardiology reports with variable dictating styles and regional and foreign accents. The reports have been carefully selected in terms of vocabulary density and subject matter, professionally edited to delete confidential information, and sequenced in a graduated easy-to-complex fashion for maximum learning and confidence building. They represent numerous standard and specialized medical and surgical conditions from the vast field of cardiology. Sixty-four medical and surgical cardiology reports are offered in this unit. Dictations 1-12 introduce the student to cardiology dictation through history and physicals and admission notes. Dictations 13-16 are emergency department reports. Dictations 20-28 are state-of-the-art diagnostic procedures, including electrophysiciologic studies and cardiac catheterization, arteriography, and ventriculography. Dictations 29-42 are acute-care discharge summaries, while dictations 43-64 are cardiac operative reports. Accompanying each dictation is an accurate transcript with explanatory footnotes supplied where indicated. Special features of this introduction include informative articles on the art and science of cardiology from the perspective of both physician and practitioner. Cardiology Words and Phrases Quick-Reference List (with nearly 900 entries) is included in the ancillary material to the Cardiology Transcription Unit, 2nd edition. References Students should proceed in an orderly and systematic fashion to master cardiology terminology and various dictating styles. The first step is to obtain the appropriate reference materials and learn to use them properly. Dictionaries are essential to accurate medical transcription. A standard English dictionary is paramount, and an unabridged dictionary offers spellings and plurals not readily found elsewhere. Basic recommended medical references include the latest editions of Dorland’s Medical Dictionary; Stedman’s Medical Dictionary; Vera Pyle’s Current Medical Terminology; Cardiovascular/Thoracic Words and Phrases. Other useful references include John H. Dirckx’s H & P: A Nonphysician’s Guide to the Medical History and Physical Examination, 3rd edition; Human Diseases, 2nd edition; Laboratory Tests and Diagnostic Procedures in Medicine; and HPI’s The Medical Transcription Workbook, 3rd edition. Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com The Reports Acute-care hospital dictation consists chiefly of the “basic four” reports: History and Physical Examination, Consultation, Operative Report, and Discharge Summary. Additionally, the Cardiology Transcription Unit contains several emergency room notes and state-of-the-art diagnostic procedures. The History and Physical Examination (H&P). Shortly before or after a patient is admitted to the hospital, the physician obtains the patient’s history and conducts a physical examination. These findings are then dictated by category and usually include the patient’s chief complaint (presenting problem); history of present illness (events leading to the patient’s hospitalization); past medical history (medical and surgical problems from childhood to present, medications, allergies); family history (the medical condition of parents and other family members); social history (the patient’s occupation, lifestyle, habits); review of systems (the medical condition of the patient’s major organs); and the physical examination. The physical examination details the physician’s findings on examination of the patient. The following subheadings are usually dictated: general appearance, vital signs, skin, HEENT (head, eyes, ears, nose, and throat), chest, breasts, heart, lungs, abdomen, back, extremities, genitalia or pelvic, rectal, neurologic, and occasionally a mental status exam. The physician completes the H&P dictation with the admitting diagnosis. A brief description of proposed treatment (treatment plan) may be dictated as well. A complete discussion of the history and physical examination can be found in H&P: A Nonphysician’s Guide to the Medical History and Physical. The Consultation. A cardiologist or cardiac surgeon may be asked to consult on another physician’s patient in order to render an opinion regarding the treatment and diagnosis of a cardiac condition. The Consultation Report usually contains a brief history of the patient’s illness, the physical findings, pertinent laboratory work, a working diagnosis, and a suggested course of treatment. The Operative Report. When a surgical procedure is performed, a detailed, documented report of the operation is required. The Operative Report usually includes the date of operation; the duration of anesthesia and operating times (frequently gleaned from written records); the names of the operating surgeon and assistants; the preoperative and postoperative diagnoses; the title of the operation performed; the type of anesthesia used; specimens sent to the pathology laboratory; indications for surgery; the operative findings; and a detailed description of the operation itself, including suture materials used to close the incision, estimated blood loss, complications encountered, condition of the patient at the end of the procedure, and if applicable, the tourniquet time, blood and/or fluid replacement, drains placed, and medications administered. Some surgeons dictate a postoperative plan. The Discharge Summary. By the time the patient is ready for discharge from an acute-care facility, a variety of treatment modalities will have been carried out. The Discharge Summary is the medical document that summarizes the patient’s course in the hospital, and it is usually dictated just before or after the patient is discharged from the hospital. Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com The Discharge Summary contains the following information: admission and discharge diagnoses, procedures or operations performed (if any), a brief review of the patient’s history and the physician’s findings on physical examination, a report of laboratory work performed and pertinent findings, the patient’s hospital course (including treatment modalities), discharge medications, and the discharge plan (often referred to as disposition.) Transcription Technique The first step. Before you begin transcribing, ascertain that your equipment is in proper working order. Assemble your reference books, gather your papers and supplies together, and isolate yourself from frequent interruptions. It is important to read the introductory articles in this book and to review the table of contents to gain an understanding of the types of reports you will be encountering. Briefly leaf through the transcripts so you will know how to set up the various formats. Building a foundation. The reports in the Cardiology Transcription Unit are sequenced so that your terminology foundation builds as you advance to the next report. Plan to transcribe each report more than once, until you become thoroughly familiar with its terminology and competent in its transcription. While you are learning, you may elect to double-space your transcripts to facilitate proofreading and error identification. Your draft copy should then be transcribed into a final error-free copy. Your ultimate goal is to produce a first-time final copy without the use of a draft copy. The standard of quality you are striving for is that which you will produce in your future employment as a medical transcriptionist—a neat, accurate, and complete report that may be placed in the patient’s medical chart as a permanent record of healthcare. Keep in mind that the transcription of medical reports (medical or technical writing) differs in technique from the production of essays and manuscripts (formal writing). The latter requires strict adherence to prescribed format, style, and syntax, and often the writer generates several draft copies before arriving at a finished polished document. Medical reports, in contrast, contain many abbreviations, brief forms, shortcuts, and word coinages that are an integral part of the language of medicine. In the workplace, a first-time final copy of a medical report is expected, and it is simply not feasible or necessary for the productionoriented medical transcriptionist working in a fast-paced environment to attempt to convert a medical document into a piece of formal writing or a polished essay. Occasionally you may encounter a dictation that seems too challenging for you at the moment. If you find yourself becoming too frustrated or discouraged after an honest attempt at transcribing a particular report, skip it for the time being and return to it later. However, be careful not to resort to this practice too often, lest you defeat the purpose of programmed learning. Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com Pace yourself. First, listen to each report, making note of words you don’t know and look them up. Then, transcribe each report carefully, stopping as often as necessary to look up new and unfamiliar words for spelling and meaning. If you fail to locate a word in your reference materials, it could be that the word in question has an initial letter other than the sound you hear. For instance, the phonetic pronunciation of v sounds very much like that of f or b, the letter m may sound like n, and so on. Some letters share the same sound. The z sound you hear may actually be an x (xiphoid) and the k might be ch (ischemic). Medical terms that contain silent letters (tachyarrhythmia) also present a challenge. As you gain experience utilizing available resources, you will become familiar with the techniques of determining sound-alikes and efficient in locating the appropriate terms. You may find that you are unable to understand a word the first time you encounter it, or you may not be able to find it in your references. When this is the case, leave a blank (or blanks) and continue with the transcription. The dictator may use the word in question a second time, enabling you to determine the appropriate term, or context clues may eventually help you decipher the term. The medical transcriptionist on the job encounters difficult terms as well. When presented with a questionable word or finding, the practitioner has several options, depending on the work environment and the employer’s procedures: (1) Seek another transcriptionist’s opinion. (2) Refer to the patient’s chart or electronic medical record, if available. (3) Send the report to a supervisor, mentor, or QA specialist. (4) Contact the dictating physician to ask what was dictated. (5) Leave a blank in the report and flag it to for verification. While you may not have access to these remedies as a student, you may want to confer with your instructor, acquire a mentor (the Association for Healthcare Documentation Integrity has a mentoring program for students), or consult with your classmates. When you have finished a report, go back and listen to the dictation again while proofreading your transcript. Check the correctness of your transcript and attempt to fill in any blanks you left earlier. Transcriptionists often find they can decipher a difficult word after listening to it again at a later time. Do not consult the transcript keys until you have completed a report to the best of your ability, using all available references. Comparing your transcripts with the transcript keys at the end of the transcription process will enable you to verify the accuracy of your work. Follow the above procedures for each dictation in turn. Footnotes The cardiology transcript keys have been prepared with the highest degree of accuracy. Because this is an advanced dictation unit, it is assumed that users will now be able to recognize certain types of edits that may have had footnotes in The SUM Program Beginning Medical Transcription Unit; thus, not every edit will have an explanatory footnote. Users should also be able to recognize when minor differences between their transcripts and the transcript keys are acceptable variations. When a dictation error occurs repeatedly within a report, it is usually footnoted only the first time it occurs. The addition of headings for consistency in format and expansion of abbreviations on first use will be footnoted only once in each report. Reports requiring little or no editing have no footnotes. Punctuation and grammatical editing changes are not generally footnoted; specific guidelines for these are addressed below. Footnotes are utilized Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com to indicate medical dictation errors and to note editorial changes. Generally speaking, ESL dictators may need more editing for grammar and syntax than dictators whose native language is English. In the transcripts, we have edited ESL dictators where we felt it appropriate, usually without footnotes to explain obvious edits for grammar and syntax. Transcription Guidelines Format and style. A variety of medical report formats and styles exist nationwide. The transcripts in this unit demonstrate several different acceptable formats but by no means all of them. In general, we have followed the ASTM standard for medical report formats as illustrated in The Book of Style for Medical Transcription. The physician’s dictating style may determine the appropriate format, or a particular medical facility may mandate certain format standards. Thus, various report formats may vary from dictator to dictator, report to report, and setting to setting. We acknowledge that many stylistic factors determine proper editing, punctuation, and grammar, that our way is not the only way, and that respected reference materials vary and may even contradict one another and themselves. Additionally, the employer of the transcriptionist may mandate specific rules of style, grammar, and format, and in that case the transcriptionist should follow the employer’s requirements. As a general stylistic reference, we recommend The Book of Style for Medical Transcription. In addition, we offer the following specific recommendations. Editing. The medical transcripts in this unit contain only minor editing changes. While the experienced medical transcriptionist, with a firm grasp of medical language and terminology and familiarity with the dictating physician’s preferences, may edit more extensively, we advise that the student transcribe the dictation verbatim (as dictated), making changes only to correct obvious dictation errors and to comply with standard style and usage guidelines. In many circumstances several editing options are available, and the student’s transcripts will likely vary in style from the transcript keys provided, although there should be no variations in medical content. Syntax or sentence structure. Where warranted, the transcriptionist may add conjunctions (and, or, but), prepositions (of, to, with), articles (a, an, the), pronouns (it, she, her, he, him), and verbs (including helping verbs) to complete a sentence. Such editing may be considered superfluous in a strict verbatim environment, and the MT should avoid altering the dictator’s style. It should also be noted that in certain parts of a report (the physical exam for example) may be defined by clipped sentences, phrases, and single words. Dictated: No tenderness present over chest. Transcribed: No tenderness is present over the chest. Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com Paragraphing. Transcribe paragraphs as dictated unless paragraphing would alter medical meaning or continuity. Paragraphing may be added where appropriate to break up long reports, to delineate headings, and to separate the findings from the procedure. Tense. As a rule, the history portion of a History and Physical, Consultation, Discharge Summary, and Operative Report is generally dictated in past tense. However, it is possible to correctly use every tense within a single paragraph. Some physicians dictate in the present tense, some in the past, and some switch back and forth. While some dictators expect the transcriptionist to change the report to past tense, other dictators insist that the report be transcribed as dictated. When the dictator’s preference is not known, the transcriptionist may transcribe as dictated. Editing tense is tricky, and the transcriptionist should be very certain that an edit is needed before making one. Headings. The transcriptionist may add headings and subheadings as appropriate. If a physician dictates the singular form Diagnosis when more than one diagnosis is provided, the transcriptionist may transcribe either Diagnosis or Diagnoses. The transcriptionist should be alert for important headings that are not dictated but are a vital part of the report. These include the Final or Discharge Diagnosis in a Discharge Summary; the Diagnosis or Impression in a History and Physical and a Consultation; and the Preoperative and Postoperative Diagnoses and Title of Operation in an Operative Report. If any of these are not dictated, the transcriptionist should supply them as appropriate or flag the report to the attention of the dictator. Report Format. There are many acceptable formats for the set-up of medical and surgical reports. In addition, there are alternative acceptable forms for the same sentence, depending on whether the format calls for a narrative such as might be contained in a discharge summary, subheadings such as in a consult or office note, or main headings as in the physical examination portion of an H&P. The following examples represent just a few of such variations in format. Dictated: Extremities unremarkable. Transcribed: The extremities are unremarkable. (Narrative paragraph format.) Transcribed: Extremities: Unremarkable. (Narrative paragraph format with subheadings.) Transcribed: EXTREMITIES: Unremarkable. (Formal Physical Examination with separate paragraphs for each subheading.) Transcribed: EXTREMITIES: The extremities are unremarkable. (Formal Physical Examination with separate paragraphs for each subheading.) Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com Lists and Diagnoses. Diagnoses, for which numbers may or may not be dictated, are generally transcribed in these transcript keys in a numbered vertical format. Medications may be transcribed as a vertical list or in a horizontal narrative style. On the job, facility specifications would dictate how lists should be transcribed, including any special formatting for diagnoses, such as those that follow the New York Heart Classification (NYHC) for heart disease. In the transcript keys, we follow the format outlined in “The Value of Using the Entire New York Heart Association’s Classification of Heart and Vascular Disease,” by J. Willishurst, M.D., MACP of Emory University, Atlanta, Georgia, USA (Clin. Cardiol. 29, 415–417 [2006]), as follows: 1. Heart Disease Etiology: Rheumatic heart disease (mitral stenosis) Anatomy: Slight right ventricular hypertrophy Left atrial enlargement Mitral valve calcification Physiology: Mitral valve stenosis Congestive heart failure Atrial fibrillation (apical rate 160 beats/min) Pulmonary hypertension Functional: Class 3 Objective Assessment: C 2. Cancer left breast (operated June 2003) 3. Essential hypertension (controlled with therapy) 4. Anxiety Physicians often dictate only the functional class, in which case, it would probably simply follow on the same line with the diagnosis. If you encounter something like this unexpectedly in the workplace, you should stop and ask for instructions, however, rather than assuming there is only one way to handle such a situation. Abbreviations, Brief Forms, Medical Slang, and Symbols Abbreviations are frequently dictated in medical reports and are an integral part of the language of medicine. Many professional transcriptionists readily utilize abbreviations when dictated, and in some instances, the translation of abbreviations may cause confusion rather than achieve clarity. For example, VDRL is readily recognized as a laboratory test for syphilis but would be obscured if translated Venereal Disease Research Laboratory. Many professional medical transcriptionists prefer to spell out all abbreviations and brief forms when dictated. Their rationale is that abbreviations obscure the clarity of the medical report and make it imprecise. On the other hand, many other professional transcriptionists readily utilize abbreviations when dictated. Except for the abbreviations specified below that need not be translated, HPI has, in all of its dictation units, expanded most abbreviations on first use within a report to ensure that the students were actually hearing the abbreviations correctly. One consonant can often sound like another—p, b, t, and d are often confused with each other, as are p and v, b and v, m and n, s and f, even n with the word and (&). Unless required to expand abbreviations, students may not Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com realize they’re transcribing the wrong letters. Furthermore, requiring students to expand abbreviations ensures that they will be able to do so if required to on the job. Abbreviations for laboratory tests (CBC, PT, TSH), electrodiagnostic tests (EMG, EKG, EEG), imaging procedures (CT, MRI, PET, SPECT, etc.), and metric units of measure are rarely expanded and sometimes appear even in diagnoses. Other common abbreviations, easily recognized by anyone with a medical background (and some lay persons) may not need to be expanded as well (for example, abbreviations like HEENT, CBC, CPR, AIDS, HIV). Of course, “easily recognized” can be said to be in the eye of the beholder, so if in doubt, ask for specific guidance from your instructor or, on the job, your supervisor or QA department. The ISMP Error-Prone Abbreviations List. See the ISMP Website (http://www.ismp.org/) or The Book of Style for Medical Transcription, 3rd edition, for a complete listing of the ISMP (Institute of Safe Medical Practices) list of error-prone abbreviations. In practice, the list has been controversial. The Joint Commission, the organization that accredits hospitals, nursing homes, and other healthcare facilities, recognizes the value of the ISMP list; however, it has chosen to incorporate only a few of the abbreviations on its official “Do Not Use” list. The abbreviations on the “Do Not Use” list are as follows: U write out unit IU write out International Units q.d. (upper and lowercase, with and without periods) translate as daily q.o.d. (upper and lowercase, with and without periods) translate as every other day MS translate appropriately as morphine sulfate or magnesium sulfate MSO4 translate appropriately as morphine sulfate or magnesium sulfate MgSO4 translate appropriately as morphine sulfate or magnesium sulfate The Joint Commission list also requires adding a leading zero to doses of less than 1 (0.5) and omitting a trailing zero from whole unit doses (50 IU) because in both cases the decimal point can be missed. Additional abbreviations for possible consideration on the JC’s official “Do Not Use” list include abbreviated drug names, apothecary units, cc which should be written as mL, and the symbol for micrograms, which can be abbreviated mcg. In these transcript keys, we have generally followed the ISMP list, rather than the Joint Commission’s official “Do Not Use” list because it is the ISMP list that is in the The Book of Style for Medical Transcription and most easily accessible by the users of this program. However, it should also be noted that the Joint Commission is emphatic that it is not the transcriptionist’s responsibility to edit error-prone abbreviations. The primary responsibility for compliance rests with the author of the documentation. “Author,” in this context, includes a person who dictates documentation to be transcribed. We would consider it inappropriate for a transcriptionist to interpret or speculate on the intended meaning of any dictation that is not clear. If a “do not use” term is used in the dictation and the dictation is Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com clear, that term should be transcribed as spoken; not translated or edited into its presumed meaning. If the dictation is not clear, then there must be a mechanism by which the originator can clarify it. Joint Commission Patient Safety Goals, New, 1/07 As with most style issues, the employer or client will no doubt have specific requirements regarding the use of error-prone abbreviations, may even have adopted its own list, and will have policies regarding whether the transcriptionist should edit error-prone abbreviations. Brief forms and slang. Brief forms can be confused with medical slang. Brief forms are shortened forms of legitimate words that can be documented in a reputable dictionary. A good rule to remember is, “When in doubt, spell it out.” A slang term is either not listed in reputable references or if listed is designated slang. Slang terms are often taken from the middle or ends of medical terms rather than the beginning. Avoid the use of slang terms and phrases except when essential to the report, when editing would result in excessive wordiness or restructuring, or when their meaning cannot be determined with certainty. Brief Form exam (examination) lab (laboratory) Slang nitro (nitroglycerin) lytes (electrolytes) crit (hematocrit) alk phos (alkaline phosphatase) Abbreviation Guidelines for the Cardiology Transcription Unit When dictated, abbreviations may be transcribed in the body of a report and at the beginning of a sentence, if their meaning is clearly understood. ST depression was noted on EKG. If the dictator abbreviates the title of a major heading within a report, the transcriptionist should translate the abbreviation. Dictated: CV: Transcribed: CARDIOVASCULAR: The first time an uncommon abbreviation is used within a report, the transcriptionist should translate it and put the abbreviation within parentheses following the translation. In instances where translation of the abbreviation may confuse rather than clarify, the abbreviation should be retained. Dictated: An AAA was discovered on echocardiography. Transcribed: An abdominal aortic aneurysm (AAA) was discovered on echocardiography. Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com Dictated: The AICD was set in the DDD mode. Transcribed: The automatic implantable cardioverter defibrillator (AICD) was set in the DDD mode. EKG leads. Subscripts are not used for the V1 through V6 leads because special characters do not transmit well electronically. The standard limb leads are identified by Roman numerals. V1 through V6 leads I, II, and III aVF, aVL, aVR Heart sounds. Similarly, subscripts are not used for the heart sounds S1 through S4 and A2 and P2. ST segments and T waves. The frequently dictated expression ST-T wave changes has become so ubiquitous that its use is widely accepted. A fuller statement would be “ST-segment and T-wave changes,” to avoid the implication that what is meant is “ST-wave and T-wave changes.” Most dictators probably say “or” in the negative statement, “No ST or T-wave changes are noted,” or its many variations. Again, inserting segment after ST would make the statement clearer, but it is not required. If “ST-segment and T-wave changes” is transcribed, the hyphens should be used because ST-segment and T-wave consistute compound adjectives. The phrase “ST-T segment deviation,” which is found in some word books, is simply wrong. There is an ST segment (the part of the ECG tracing extending from the S wave to the T wave) and there is a T wave, but one cannot speak of an ST-T segment, much less an ST-T segment deviation. Symbols. The symbol x may be used to represent the word times (bleeding x3 days). It is also used to represent by in measurements (3 x 5 cm). The percent symbol (%) should be used with numerals; in a range, the symbol should be repeated with each value (10% to 20%). The degree symbol º does not transmit well electronically, so it is recommended that degrees be spelled out in medical reports. If the temperature scale (Fahrenheit, Celsius, centigrade) is also dictated, write it out as well, changing centigrade to the preferred metric scale, Celsius. In medical reports where the degree symbol is used, the abbreviation F is used for Fahrenheit and C for Celsius and centigrade. Do not insert a space after the degree symbol or a period after the abbreviation for the scale. 37ºC 98.6ºF 37 degrees Celsius 98.6 degrees Fahrenheit Numbers Avoid beginning a sentence with a numeral. Either write out the number or alter the beginning of the sentence. Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com Dictated: 2 mL of Xylocaine was given. Transcribed: Two milliliters of Xylocaine was given. Xylocaine 2 mL was given. Then 2 mL of Xylocaine was given. Dictated: 45-year-old black male Transcribed: A 45-year-old black male or This is a 45-year-old black male or This 45-year-old black male (if verb follows) Dictated: 5-FU therapy was given. Transcribed: Therapy with 5-FU was given. The transcriptionist should enumerate a long list of diagnoses, whether or not numbers are dictated. When the dictator numbers the diagnoses, retain the numbers unless there is only one diagnosis. Do not add an apostrophe when pluralizing multi-digit numbers; do add an apostrophe when making single-digit numbers plural. 100s 4 x 4’s Suture sizes may or may not be dictated with a number sign. As a general rule, transcribe as dictated. However, when the suture size is a whole number, the number sign may be added for clarity. 00 or 2-0 or #2-0 Dexon suture #1 Tevdek suture Units of Measure It is customary to abbreviate metric measurements in medical reports. Abbreviations for metric measurements contain no periods and are in the same form for both singular and plural usage. For example, cm is the abbreviation for both centimeter and centimeters. Standard English units of measure contain so few letters that they are usually spelled out. mg (milligrams) mmHg (millimeters of mercury) inch foot Metric measurements in this transcription unit follow the recommendations of the SI system (Système International d’Unités); for example, cm (centimeters), mL (milliliters), and g (gram). Fractions should be converted to decimals when they are used with metric units of measure, and decimals should be converted to fractions when they are used with standard units of measure. 0.25 cm 1/4 inch 3.5 mL Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com Note: English fractions may be spelled out or transcribed as numbers, depending on style preferences; quarter-inch Penrose drain or 1/4-inch Penrose drain are both acceptable. Metric numbers less than one should be preceded with a zero and a decimal point (0.5) to avoid the decimal being lost and the number interpreted as a whole number rather than a fraction, whether or not the zero was dictated. If the physician dictates a whole number with a decimal point and a zero, retain the zero and the decimal if the value refers to a laboratory test result or dimensions or volume in surgery and pathology. If the value refers to a drug dose, do not place a decimal and a zero after the whole number. 0.5 mm in diameter 3 cm in length but 3 inches In a series of metric measurements, do not repeat the unit of measure unless it is different for the different values or its absence would confuse the reader. Dictated: 3.3 cm x 1 x 4 Transcribed: 3.3 x 1 x 4 cm But: 2.5 mm x 2 cm Use a singular form of a verb with units of measure. Approximately 10 mL of fluid was aspirated from the pleural cavity. Word Forms Alternative spellings. Some words have more than one acceptable spelling, and the preferred spelling may vary from reference to reference. anulus (not annulus) PR interval, P-R interval transected, transsected long-standing, longstanding Combined forms. Physicians frequently dictate combined forms. It is acceptable to use either the combined form or the standard (often hyphenated) form when it is uncertain which is dictated. femoral-popliteal or femoropopliteal inferior-lateral or inferolateral tracheal-bronchial or tracheobronchial Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com Plurals. Generally, medical words derived from Latin or Greek are pluralized according to guidelines in the recommended references. However, some physicians prefer to pluralize Latin terms in the same way that English words are pluralized. Transcribe as dictated unless incorrect. fistulas or fistulae lumens or lumina cannulas or cannulae Punctuation Standard punctuation is followed in these transcripts. Where the physician dictates punctuation marks, you should transcribe as dictated, unless the punctuation is incorrect or results in an error in meaning. Punctuation marks may be added or changed to clarify meaning and assist in reading. Comma. There are two schools of thought on comma usage. The traditional approach requires frequent use of commas for clarity. Contemporary usage avoids heavy use of commas in order to simplify and unclutter the written language. Although either style is acceptable, contemporary usage (demonstrated in these transcripts) is more compatible with medical and technical writing. No matter which style you use, strive for consistency in punctuation within each report that you transcribe. Hyphen. The trend in contemporary usage is to avoid the use of hyphens when they are not required for clarity. The use of hyphens with metric abbreviations is discouraged by the S.I. Committee and is no longer recommended by The Book of Style for Medical Transcription, 3rd edition. QT interval or Q-T interval 1 mm ST segment depression 3 cm incision The prefix post is not generally hyphenated. When used as an adjective before a noun, post is connected to the root word without a hyphen. When it functions as a preposition (meaning after), it stands alone. The postoperative assessment was negative. The patient is status post myocardial infarction. When like or most appears as a suffix, it is attached to the root word without a hyphen, unless the root word is multisyllabic or failure to hyphenate would affect clarity. swanlike uppermost seizure-like lateral-most The use of hyphens with mid varies. The prefix mid may stand alone as an adjective (mid and left chest) or combine with a root word without a hyphen (midchest, midlateral). Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com A hyphen is not needed to connect a single letter and noun combination, such as J point and T wave; however, a hyphen is used to join a single letter and noun when they function as a compound adjective (ST-segment depression and T-wave changes). Compound designations of Americans identified by ethnicity, race, or nationality are no longer hyphenated, either as nouns or adjectives. Japanese American male Mexican American female Colon/Capitalization. Capitalize the first word following a colon in a heading or subheading. HEART: The heart sounds are strong on auscultation. Possessive Eponyms The use of the apostrophe plus s (’s) to form a possessive eponym is optional. The reports in this unit were transcribed verbatim, and the ’s was used only when the physician dictated the possessive form. Starling mechanism or Starling’s mechanism Wenckebach phenomenon or Wenckebach’s phenomenon Eponymic adjectives in Cardiology Words and Phrases: A Quick-Reference Guide are presented without the possessive form, for simplicity. Summing It Up This versatile training unit was developed to meet the needs of all transcription students. Whether your method is by self-study or formal instruction, whether you are a novice or an experienced generalist with a desire to assess your competency, we recognize your worthwhile goals and encourage you in your endeavors. Cardiology, The SUM Program Advanced Medical Transcription Unit, 2nd ed. Health Professions Institute www.hpisum.com