Lancet Respiratory Medicine Paper
advertisement

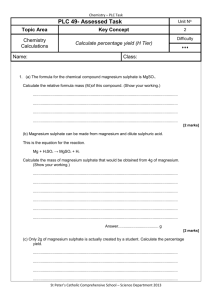
The 3Mg Trial: Randomised controlled trial of intravenous or nebulised magnesium sulphate or standard therapy for severe acute asthma Steve Goodacre PhD1, Judith Cohen PhD1, Mike Bradburn MSc1, Alasdair Gray MD2, Jonathan Benger MD3, Timothy Coats MD4 on behalf of the 3Mg Research Team 1 School of Health and Related Research (ScHARR), University of Sheffield, 2Emergency Department, Royal Infirmary of Edinburgh, 3Faculty of Health and Life Sciences, University of the West of England, Bristol, 4Emergency Department, Leicester Royal Infirmary Corresponding author Steve Goodacre, Professor of Emergency Medicine University of Sheffield, Regent Court, 30 Regent Street, Sheffield, S1 4DA Email: s.goodacre@sheffield.ac.uk Tel: +44 114 222 0842 This is the accepted version of an article that has been published in the Lancet Respiratory Medicine: http://www.thelancet.com/journals/lanres/article/PIIS2213-2600(13)70070-5/fulltext Registration: http://www.controlled-trials.com/ISRCTN04417063 Lancet protocol 08PRT/503: http://www.thelancet.com/protocol-reviews/08PRT-503 1 Abstract Background: Previous studies suggest that intravenous (IV) or nebulised magnesium sulphate may improve respiratory function in acute asthma. We aimed to determine whether IV or nebulised magnesium sulphate improve symptoms of breathlessness and reduce the need for hospital admission in adults with severe acute asthma. Methods: In a double-blind placebo-controlled trial undertaken in the emergency departments of 34 hospitals we randomised 1109 adults with severe acute asthma to receive either IV magnesium sulphate (2g over 20 minutes) or nebulised magnesium sulphate (3 x 500mg over one hour) alongside standard therapy including salbutamol, or standard therapy alone. Consented participants were allocated to numbered treatment packs using a telephone or internet randomisation system. A simple randomisation sequence was used in 20 hospitals participating at the outset, but switched to blocked randomisation, stratified by hospital, for subsequent hospitals. Each treatment pack contained an IV infusion and three nebuliser solutions, either of which could be active treatment or placebo. The primary outcome measures were the proportion of patients admitted to hospital (either after emergency department treatment or at any time over the subsequent seven days) and breathlessness measured on a 100mm visual analogue scale (VAS) over two hours after initiation of treatment. Participants were analysed in the groups to which they were allocated, regardless of whether they actually received or completed the allocated treatment. Recruitment continued towards a target of 1200 participants until funding expired and the trial closed. ISRCTN04417063 Findings: Hospital admission was recorded for 1084 patients (394 IV magnesium sulphate, 332 nebulised magnesium sulphate, 358 placebo, mean age 36.1 years, 763/1084 (70%) female) and VAS breathlessness for 976. IV magnesium sulphate was associated with an odds ratio of 0.73 (95% confidence interval 0.51 to 1.04, p=0.083) for hospital admission, an improvement in VAS breathlessness that was 2.6mm (-1.6 to 6.8mm, p=0.231) greater than 2 placebo, and an improvement in percentage predicted peak expiratory flow rate (PEFR) that was 0.4% (-2.3 to 3.0%, p=0.786) less than placebo. Nebulised magnesium sulphate was associated with an odds ratio of 0.96 (0.65 to 1.40, p=0.819) for hospital admission, an improvement in VAS breathlessness that was 2.6mm (-1.8mm to 7.0mm, p=0.253) less than placebo, and an improvement in percentage predicted PEFR that was 0.6% (-2.1 to 3.4%, p=0.652) less than placebo. Interpretation: These findings suggest that there is no role for nebulised magnesium sulphate in the management of severe acute asthma in adults and at best only a limited role for IV magnesium sulphate. Funding: National Institute for Health Research Health Technology Assessment Programme (HTA06/01/02) 3 Background Acute asthma is responsible for around 60,000 hospital admissions per year in England1. Current guidelines2,3 advise a stepwise approach to the management of exacerbations. Initially all patients should receive oxygen, nebulised 2-agonists, nebulised anticholinergic agent and corticosteroids. However, bronchodilators act within minutes whereas corticosteroids require hours to take effect. This suggests a potential role for magnesium sulphate as an additional treatment option in the therapeutic gap between nebulised bronchodilators and corticosteroids. Magnesium sulphate has been evaluated in both the intravenous (IV) and nebulised form. The nebulised route offers the potential advantage of a quick onset of action and lower incidence of side effects. Its disadvantages include a lower dose of drug delivered and the patient requiring some respiratory effort to maximise its effectiveness. The IV route provides direct access to the venous system, allowing the delivery of high drug concentrations. The disadvantages include the requirement for intravenous access and the drug being administered by infusion over 20 minutes. Several systematic reviews and meta-analyses have evaluated the role of IV or nebulised magnesium sulphate in acute asthma4-10. The most recent10 showed that IV treatment appeared to be effective in children but was unable to draw clear conclusions about treatment in adults. Both IV treatment (10 trials, 955 adults) and nebulised treatment (7 trials, 430 adults) were associated with weak evidence of improved respiratory function compared to control. No trials directly compared IV to nebulised magnesium sulphate. The standardised mean difference (SMD) for IV treatment was 0.25 (95% CI -0.01 to 0.51, p=0.06) and for nebulised treatment was 0.17 (95% CI -0.02 to 0.36, p=0.09). Meta-analysis showed that IV treatment was associated with weak evidence of an effect on hospital admission (relative risk (RR) 0.68, 95% CI 0.46 to 1.02, p=0.06) while nebulised treatment 4 was associated with no significant effect (RR 0.87, 95% CI 0.70 to 1.08, p=0.22). One further trial of IV magnesium sulphate in adults11 has since been published. Inclusion of this trial in the meta-analysis12 resulted in the effect upon respiratory function being slightly larger and statistically significant (SMD=0.35, 95% CI 0.06 to 0.64, p=0.02) but the effect on hospital admission remained non-significant (RR=0.85, 95% CI 0.68 to 1.06, p=0.14). It is not clear whether changes in measures of respiratory function are associated with important changes in patient management or a clinically meaningful improvement in symptoms. Uncertainty in the evidence is reflected in treatment recommendations. Current guidelines in the United Kingdom2 and the United States3 suggest that IV magnesium sulphate should be considered in adults with life-threatening features or severe acute asthma that has not responded to inhaled bronchodilator therapy. No recommendations are made regarding nebulised magnesium sulphate. We measured the effectiveness of IV and nebulised magnesium sulphate in adults with severe acute asthma. We specifically aimed to determine whether IV or nebulised magnesium sulphate, used alongside standard treatment including salbutamol, reduces the proportion of patients requiring hospital admission at initial presentation or during the following seven days, and whether IV or nebulised magnesium sulphate improves patient assessment of breathlessness over two hours after initiation of treatment. Methods Study design and patients We undertook a multi-centre, double blind, placebo controlled, three-arm, randomised trial in 34 emergency departments in the United Kingdom. The trial protocol has been published13. Adults (age>16) attending the emergency department with severe acute asthma were eligible for recruitment (i.e. acute asthma with either PEFR < 50% of best or predicted, respiratory rate > 25/min, heart rate > 110/min, or inability to complete sentences in one 5 breath). We excluded patients who had life threatening features (oxygen saturation < 92%, silent chest, cyanosis, poor respiratory effort, bradycardia, arrhythmia, hypotension, exhaustion, coma or confusion), those with a contraindication to either nebulised or intravenous magnesium sulphate (pregnancy, hepatic or renal failure, heart block or known hypermagnesaemia), those unable to provide written or verbal consent, and previous participants in the 3Mg trial. We amended the protocol during the trial to also exclude those who had received magnesium sulphate in the 24 hours prior to recruitment. Written or verbal consent was sought from all participants. Those initially providing verbal consent were asked for written consent as soon as their condition permitted. Randomisation and masking Consented participants were randomised through a telephone or internet randomisation system managed by the Sheffield Clinical Trials Research Unit (CTRU). After being entered into the trial participants were allocated to numbered treatment packs kept in the emergency department. A simple randomisation sequence was used in the 20 hospitals participating at the outset, but switched to blocked randomisation (block sizes of four or six), stratified by hospital, for subsequent hospitals to safeguard against new centres recruiting too few in any trial arm. Each treatment pack contained an IV infusion and three nebuliser solutions, either of which could be active treatment or placebo. Participants, hospital staff and research staff were blinded to the allocated treatment. Interventions and concurrent treatments The three treatment arms were as follows: 1. IV magnesium sulphate, 8 mmol (2g) in 100ml normal saline given over 20 minutes, and three 7.5ml vials of 0.9% saline nebulised at 20 minutes intervals 2. IV normal saline, 100ml given over 20 minutes, and three 7.5ml vials of 2 mmol (500mg) magnesium sulphate nebulised at 20 minutes intervals 6 3. IV normal saline, 100ml given over 20 minutes, and three 7.5ml vials of 0.9% saline nebulised at 20 minutes intervals Standard therapy was provided in accordance with guidelines2 from the British Thoracic Society (BTS) and Scottish Intercollegiate Guidelines Network (SIGN) and consisted of oxygen, nebulised salbutamol (5mg), nebulised ipratropium (500mcg) and oral prednisolone administered during recruitment, followed by up to 5mg salbutamol added to each trial nebuliser. Other treatments were given at the discretion of the clinician. Patients were managed in the emergency department and data collected until two hours after randomisation. At this point, if not already undertaken, a final disposition decision was made (hospital admission or discharge) and initial data collection completed. Outcome measures Two primary outcomes were specified: 1. The health service primary outcome was the proportion of patients admitted to hospital, either after emergency department treatment or at any time over the subsequent seven days. 2. The patient-centred primary outcome was the patient’s visual analogue scale (VAS) for breathlessness over two hours after initiation of treatment. VAS breathlessness has been used to measure breathlessness during exercise14 and has been shown to correlate with respiratory function and symptomatic change in cohorts with acute asthma15,16. Secondary outcomes included mortality, adverse events, use of ventilation or respiratory support, length of hospital stay, admission to a high dependency unit (HDU) or intensive care unit (ICU), change in PEFR and physiological variables (oxygen saturation, heart rate, respiratory rate, blood pressure) over two hours, quality of life at baseline and one month, 7 number of unscheduled health care contacts over the subsequent month, and satisfaction with care. Adverse events and side effects occurring during emergency department treatment were routinely recorded on the Case Report Form by the treating clinician. Key events (cardiac arrest, respiratory arrest, emergency intubation, non-invasive ventilation, pneumothorax and arrhythmia) and common side effects (flushing, nausea, vomiting and hypotension (systolic <100mmHg)) were specifically sought and recorded. Other events were recorded on a general adverse event reporting form. Patient notes were reviewed by a research nurse who recorded any side effects identified during treatment or adverse events occurring up to 30 days after treatment. Adverse events were identified and reported according to Good Clinical Practice (GCP) guidance. Sample size We planned to recruit 1200 participants divided equally between the three trial arms to provide the following statistical power: 1. Assuming that 80% of patients with severe acute asthma are admitted after emergency department management and hospital admission is recorded for all participants, the study would have 90% power to detect a 10% absolute reduction in the proportion admitted (i.e. to 70%) for any pair of treatment groups compared (twosided alpha=0.05). 2. Assuming that 80% of participants have their VAS measured then the study would have 90% power to detect a 8mm difference in a 100mm VAS at two hours after treatment initiation (two-sided alpha=0.05). Previous data have established that the standard deviation on a 100mm VAS is 30mm, and that 22mm represents a minimum clinically significant difference15. Statistical analysis 8 Participants were analysed in the groups to which they were allocated, regardless of whether they actually received or completed the allocated treatment. Logistic regression was used for analysis of admission rates. For length of stay, means (medians) were compared using censored Normal (log-Normal) regression to account for interval censoring in discharged patients (for whom no time of discharge was recorded) and also admissions which were ongoing at 30 days. Number of days on ICU/HDU were compared using Mann-Whitney U test. Analysis of covariance was used for all other outcomes. The primary analysis was adjusted for hospital and is presented for observed data (complete case); further analyses using different imputation strategies were used as confirmatory analyses. A secondary explanatory analysis was undertaken limited to those who completed the treatment as per protocol. We used Simes’s (1986) method17, which is a modification of the Bonferroni method but has better power, to adjust for multiplicity arising from having two primary outcomes. The two pre-planned comparisons between the three groups were (1) active treatment (IV or nebulised) versus placebo and (2) IV versus nebulised magnesium sulphate. We also present comparisons of IV magnesium sulphate versus placebo and nebulised magnesium sulphate versus placebo for completeness. We undertook three preplanned subgroup analyses stratified by age (above or below 50 years), baseline PEFR (above or below median) and whether the patient had received treatment with salbutamol before the trial treatments. An independent Data Monitoring Committee (DMC) reviewed trial data at regular intervals and reported recommendations to the Trial Steering Committee in accordance with the DMC charter. The Trial was approved by the Scotland A Research Ethics Committee. The trial sponsor was Sheffield Teaching Hospitals NHS Foundation Trust. Role of the funding source The study funders had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. 9 The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. Results Patients were recruited from 34 hospitals between 30/7/2008 and 30/6/2012. Recruitment was slower than anticipated and ended when the trial funding expired. The flow of patients through the trial is shown in figure 1. Of the 1109 patients recruited, 25 withdrew without commencing trial medication, were recruited in error (protocol violations) or could not be allocated to a treatment pack, so 1084 were included in the analysis. Table 1 shows the baseline characteristics of the recruited patients. Age and sex characteristics were balanced across the groups, but there were more white ethnicity patients in the IV magnesium group and more patients who had never smoked in the nebulised magnesium group. Supplemental tables 1 and 2 show the trial and concurrent medications received by the three patient groups. There was a high degree of adherence to the trial protocol: the mean total dose of nebulised solution was 21.3ml, with 85% receiving the full dose of 22.5ml, while the mean total dose of IV infusion was 97.1ml with 89% receiving the full IV infusion. The results of primary outcome analysis are shown in table 2 (admission to hospital) and table 3 (VAS breathlessness). The odds ratios for admission to hospital were 0.84 (95% CI 0.61 to 1.15, p=0.276) for active treatment versus placebo, 0.76 (0.53 to 1.10, p=0.146) for IV versus nebuliser, 0.73 (0.51 to 1.04, p=0.083) for IV versus placebo, and 0.96 (0.65 to1.40, p=0.819) for nebuliser versus placebo. The mean differences in improvement in VAS were 0.0mm (95% CI -1.9 to 1.9mm, p=0.999) for active treatment versus placebo, 5.1mm (0.8 to 9.4mm, p=0.019) for IV versus nebuliser, 2.6mm (-1.6 to 6.8mm, p=0.231) for IV versus placebo, and -2.6mm (-7.0 to 1.8mm, p=0.253) for nebuliser versus placebo (a positive value indicates a greater improvement than the comparator). Further analyses were run with plausible imputations for the 108 (10%) patients with no 2-hour change in VAS recorded; these had no material impact on the findings. 10 Table 4 shows the analysis of PEFR as a percentage of predicted PEFR. The mean differences in improvement in % predicted PEFR were -0.5% (95% CI -2.9 to 1.9%, p=0.676) for active treatment versus placebo, 0.3% (-2.4 to 3.0%, p=0.841) for IV versus nebuliser, 0.4% (-3.0 to 2.3%, p=0.786) for IV versus placebo, and -0.6% (-3.4 to 2.1%), p=0.652) for nebuliser versus placebo (a positive value indicates a greater improvement than the comparator). There were no significant differences in any comparisons of physiological measures. Full details of physiological measures and oxygen flow rates are provided in supplemental tables 3 to 8. Table 5 shows analysis of length of stay, admission to the ICU or HDU, and use of respiratory support. There was no significant difference between the three groups in these outcomes. Figure 2 shows the proportion of patients in hospital by treatment group as a function of time from hospital admission. Any small difference between the groups had disappeared by 24 hours. Table 6 shows adverse events and side effects. The odds ratios for suffering any side effect were 1.68 (95% CI 1.11 to 2.52, p=0.014) for active treatment versus placebo, 1.00 (0.66 to 1.52, p=0.988) for IV versus nebuliser, 1.68 (1.07 to 2.63, p=0.025) for IV versus placebo, and 1.67 (1.05 to 2.66, p=0.031) for nebuliser versus placebo. Table 7 shows the medications prescribed to patients discharged after emergency department treatment. Most patients received prednisolone and a few received additional inhalers. There were no significant findings on pre-planned subgroup analysis. In particular, the odds ratio for hospital admission with IV treatment versus placebo was 0.76 (95% CI 0.45 to 1.30) in patients presenting with more severe asthma (defined as PEFR<=50% of predicted) and 0.67 (95% CI 0.42 to 1.06) in those presenting with less severe asthma. 11 Discussion The 3Mg trial is the largest trial of magnesium sulphate ever undertaken in acute asthma, the first powered on the basis of detecting a meaningful difference in admission to hospital and the only trial to directly compare IV to nebulised treatment. We were unable to demonstrate a clinically worthwhile benefit from either IV or nebulised magnesium sulphate compared to placebo. There was some evidence of IV magnesium sulphate having an effect upon hospital admission and the confidence interval for this estimate includes the possibility of both a worthwhile effect and no effect, but any effect on breathlessness was smaller than the minimum clinically significant difference14. There was no suggestion of an effect from nebulised magnesium sulphate in either primary outcome. Meta-analysis of previous trials suggested evidence of benefit from both IV and nebulised magnesium sulphate10. This contrasts with our findings of no benefit from nebulised treatment and weak evidence of benefit from IV treatment. There are a number of potential reasons for this inconsistency. Meta-analysis of previous trials may be subject to publication bias if positive trials are preferentially submitted and accepted for publication. Some previous trials may have been limited by inadequate allocation concealment or blinding that inflated estimates of treatment effects. All three arms of the 3Mg trial received treatment with nebulised β-agonists which may have limited the potential for magnesium sulphate to provide additional bronchodilatation, whereas it was not always clear that all patients received optimal standard treatment in previous trials. In this respect it is worth noting that patients in the control arm showed marked improvements in peak expiratory flow rate and VAS breathlessness, and few required respiratory support, indicating a good response to standard treatment alone. One potential explanation that can probably be discounted is that the trial treatment was inadequate, in terms of the planned dosage and actual amount of drug given. The protocol specified dosages of IV and nebulised magnesium sulphate that were at the top end of 12 dosages used in previous trials. Data presented in the supplemental tables show high adherence to the trial protocols with most patients receiving the full dose of the relevant drugs. Pragmatic trials carry a risk that trial treatment will be delivered in a suboptimal manner, but we found no evidence of this in the 3Mg trial. Our findings for nebulised magnesium sulphate contrast with those of the MAGNETIC trial which showed an improvement in asthma severity score at 60 minutes post-treatment with nebulised magnesium sulphate compared to placebo in acute severe pediatric asthma18. Previous meta-analysis10 suggested that IV magnesium sulphate is more effective in children than adults. The findings of 3Mg and MAGNETIC suggest that the same is true of nebulised magnesium sulphate. The 3Mg trial had strengths and limitations that need to be considered when interpreting the findings. The trial terminated when funding expired and recruited 1084 patients against a target of 1200. Despite this shortfall, it still had 84% power to detect a 10% difference in admission rate for nebulised treatment versus placebo and 87% power for IV treatment versus placebo based on the original sample size projections. Furthermore, VAS breathlessness was recorded for 90% of the study population, as opposed to the anticipated 80% in the power calculation, so there was no loss of power to detect a difference in this outcome. 3Mg is therefore the largest trial of IV or nebulised magnesium sulphate in acute asthma and the only trial powered to detect clinically important differences in admission rate. 3Mg designed as a pragmatic trial to determine the effectiveness of using magnesium sulphate alongside other treatments as part of routine emergency department practice. The study population was pragmatically defined using information routinely available to emergency department staff. This means that the findings are generalisable to typical patients attending hospital with acute asthma, but also means that the study population could have included some patients with other diagnoses. We evaluated magnesium sulphate 13 alongside standard treatment rather than comparing it to elements of standard treatment. This may have reduced the potential for magnesium sulphate to make a difference, but withholding standard treatment would have been unethical. We selected primary outcomes that measured the effect of treatment upon symptoms (VAS breathlessness) and management (hospital admission). We also measured physiological parameters and PEFR as secondary outcomes. It is possible that other measures, such as forced expiratory volume in one second (FEV1) might have been more sensitive to changes in respiratory function, but these are not routinely measured in the emergency department, and would not provide evidence of clinical effectiveness. Demonstrating clinical effectiveness involves showing a meaningful improvement in patient symptoms or management, not just a change in respiratory parameters. Finally, we deliberately excluded patients with life-threatening asthma and were unable to power the study to detect differences in serious adverse outcomes (including death), so we are unable to determine whether magnesium sulphate may have an effect upon serious adverse outcomes in life-threatening asthma. The findings of this trial suggest that there is no role for nebulised magnesium sulphate in the management of severe acute asthma in adults and at best a limited role for IV magnesium sulphate. Patients receiving standard treatment showed marked improvements in breathlessness and PEFR, and few required respiratory support. Although most were admitted to hospital, we found no evidence that nebulised magnesium sulphate reduced the admission rate and only weak evidence of an effect from IV magnesium sulphate. The low rate of side effects and adverse events (other than those related to the underlying illness) suggests a low risk of harm from IV administration but the corresponding evidence of benefit is modest and uncertain. Further clinical trials of magnesium sulphate in adults with acute asthma are unlikely to be worthwhile. If IV treatment has an effect upon admission rate or adverse events that was not detected by 3Mg then it would need a much larger trial to detect such an effect. The logistic 14 barriers to undertaking clinical trials in patients with a medical emergency would seem to prevent a larger trial being feasible at an acceptable cost. Research in context Systematic review A 2007 systematic review, updated in 2009, identified eleven trials of IV magnesium sulphate in 1018 adults and seven trials of nebulised magnesium sulphate in 430 adults with acute asthma. Meta-analysis suggested that both IV and nebulised treatment had potentially worthwhile effects on respiratory function (standardised mean difference for IV treatment=0.35, 95% CI 0.06 to 0.064, p=0.02; standardised mean difference for nebulised treatment=0.17 (95% CI -0.02 to 0.36, p=0.09) and showed non-significant trends towards reduced admission to hospital (relative risk for IV treatment=0.85, 95% CI 0.68 to 1.06, p=0.14; relative risk for nebulised treatment=0.87, 95% CI 0.70 to 1.08, p=0.22). Interpretation Our large pragmatic study failed to provide convincing evidence that IV or nebulised magnesium sulphate produce clinically worthwhile benefits in adults with severe acute asthma. Although magnesium sulphate is a safe treatment with few significant side effects, current data do not support a role in the standard treatment of adults with severe acute asthma. Conflicts of interest None to declare Sources of funding The 3Mg Trial was funded by the National Institute for Health Research Health Technology Assessment Programme (reference 06/02/01). The views and opinions expressed are those of the authors and do not necessarily reflect those of the Department of Health. 15 Contributors Membership of the 3Mg Research Team is outlined in the linked online appendix. The coapplicants designed the trial. The Project Management Group and Local Investigators undertook the trial with independent oversight from the Trial Steering Committee and Data Monitoring Committee. Steve Goodacre wrote the first draft of this paper. Mike Bradburn undertook the statistical analysis. Steve Goodacre, Mike Bradburn, Judith Cohen, Alasdair Gray, Tim Coats and Jonathan Benger contributed to redrafting of the paper and approved the final draft. The 3Mg Research Team Writing Group: Steve Goodacre, Judith Cohen, Mike Bradburn, John Stevens (University of Sheffield), Alasdair Gray (Royal Infirmary of Edinburgh), Jonathan Benger (University of the West of England), Tim Coats (University of Leicester); Project Management Group: Steve Goodacre (Chief Investigator), Judith Cohen (Trial Manager), Mike Bradburn, Chin Maguire, Yvonne Meades (University of Sheffield), Alasdair Gray, Moyra Masson (Royal Infirmary of Edinburgh), Jonathan Benger (University of the West of England), Tim Coats (University of Leicester); Trial Steering Committee: Andrew Greening (Independent Chair, Western General Hospital, Edinburgh), Magdy Sakr (Independent, University Hospitals of Coventry and Warwickshire), Roseanne McNamee (Independent, University of Manchester), Jenny Negus (Independent, Patient Representative), Steve Goodacre, Alasdair Gray, Judith Cohen; Data Monitoring and Ethics Committee: Sandra Eldridge (Chair, Queen Mary University of London), Mark Elliott (St James University Hospital, Leeds), Steve Crane (York Hospital); Co-applicants: Steve Goodacre, Jon Nicholl, Mike Campbell, Julie Ratcliffe (University of Sheffield), Alasdair Gray (Royal Infirmary of Edinburgh), Jonathan Benger (University of the West of England), Tim Coats (University of Leicester), Stephen Holgate (University of Southampton), Peter Jackson (Sheffield Teaching Hospitals NHS Foundation Trust); Local Investigators: Abdul Jalil (Doncaster Royal Infirmary), Alasdair Corfield (Royal 16 Alexandra Hospital, Paisley), Alasdair Gray (Royal Infirmary of Edinburgh), Alastair Stevenson (Ayr Hospital), Angus Cooper (Aberdeen Royal Infirmary), Ann Marie Morris (University Hospital of North Staffordshire), Colin Dewar (Fife, Queen Margaret Hospital and Victoria Hospital), Crawford McGuffie (Crosshouse Hospital), David Robinson (Bradford Royal Infirmary), Barbara Madigan (Royal United Hospital Bath ), Frank Coffey (Queen’s Medical Centre , Nottingham), Gary Kitching (York Hospital), Gavin Lloyd (Royal Devon & Exeter Hospital), Iain Lennon (Derbyshire Royal Infirmary), Jason Smith (Derriford Hospital, Plymouth), John Keaney (Hairmyres Hospital), Jonathan Benger (Bristol Royal Infirmary), Julian Humphrey (Barnsley Hospital), Khurram Iftikhar (Southend University Hospital), Matt Shepherd (Pinderfields Hospital), Matthew Pereira (Addenbrooke's Hospital,- Cambridge), Mehmood Chaudhry (University Hospital Coventry), Nathan Spencer (Kettering General Hospital), Patrick Dissmann (James Cook University Hospital, Middlesbrough), Samuel McBride (Lancaster Royal Infirmary), Simon Chapman (Bristol Frenchay Hospital), Steve Goodacre (Northern General Hospital, Sheffield), Suzanne Brady (Rotherham General Hospital), Taj Hassan (Leeds Teaching Hospitals), Tim Coats (Leicester Royal Infirmary), Tim Harris (The Royal London Hospital), Tristan Dyer (Northampton General Hospital), William Townend (Hull Royal Infirmary). Acknowledgements We thank Katie Biggs, Timothy Chater, Joseph Clark, Christopher Ellis, Amanda Loban, Kathryn MacKellar, Diana Papaioannou and Martina Santarelli for their help with trial administration, monitoring and co-ordination, and data management. References 1. The NHS Information Centre for Health and Social Care. Hospital Episode Statistics (HES) Online. http://www.hesonline.org.uk Accessed 3/12/2012. 17 2. British Thoracic Society/Scottish Guidelines Intercollegiate Network. British guideline on the management of asthma, revised edition 2007. 3. National Asthma Education and Prevention Program Expert Panel Report #3: Guidelines for the Diagnosis and Management of Asthma. US Department of Health and Human Services National Institutes of Health National Heart, Lung, and Blood Institute, 2007. 4. Rowe BH, Bretzlaff JA, Bourdon C, Bota GW, Camargo CA Jr. Magnesium sulfate for treating exacerbations of acute asthma in the emergency department. Cochrane Database Syst Rev 2000;(2):CD001490. 5. Alter HJ, Koepsell TD, Hilty WM. Intravenous magnesium as an adjuvant in acute bronchospasm: a meta-analysis. Ann Emerg Med 2000;36:191-7. 6. Rodrigo G, Rodrigo C, Burschtin O. Efficacy of magnesium sulfate in acute adult asthma: a meta-analysis of randomized trials. Am J Emerg Med 2000;18:216-21. 7. Cheuk DK, Chau TC, Lee SL. A meta-analysis on intravenous magnesium sulphate for treating acute asthma. Arch Dis Child. 2005;90:74-7. 8. Blitz M, Blitz S, Beasely R, Diner BM, Hughes R, Knopp JA, Rowe BH. Inhaled magnesium sulfate in the treatment of acute asthma. Cochrane Database Syst Rev. 2005;19;(4): CD003898. 9. Villeneuve EJ, Zed PJ. Nebulized magnesium sulfate in the management of acute exacerbations of asthma. Ann Pharmacother. 2006;40:1118-24. 10. Mohammed S, Goodacre S. Intravenous and nebulised magnesium sulphate for acute asthma: systematic review and meta-analysis. Emerg Med J 2007, 24;823-830. 11. Singh AK, Gaur S & Kumar R. A randomised controlled trial of intravenous magnesium sulphate as an adjunct to standard therapy in acute severe asthma. Iran J Allergy Asthma Imunol 2008;7:221-229. 12. Cohen J, Goodacre S. Magnesium sulphate meta-analysis update February 2009, unpublished. http://www.shef.ac.uk/polopoly_fs/1.44176!/file/Mg-meta-analysisupdated-Feb-2009.pdf - accessed 4/12/2012. 18 13. Protocol 08PRT/503: The 3Mg trial: randomised controlled trial of intravenous or nebulised magnesium sulphate or standard therapy for acute severe asthma (ISRCTN04417063). Lancet 2008, http://www.thelancet.com/protocolreviews/08PRT-503 14. Wilson RC, Jones PW. Comparison of the visual analogue scale and Borg scale for measurement of dyspnoea during exercise. Clin Sci 1989;76:277-282. 15. Karras DJ, Sammon ME, Terregino CA, Lopez BL, Griswold SK & Arnold GK. Clinically meaningful changes in quantitative measures of asthma severity. Acad Emerg Med 2000;7:327-334. 16. Gupta D, Aggarwal AN, Sublamaxi MV, Jindal SK. Assessing severity of asthma: spirometric correlates with visual analogue scale (VAS). Indian J Chest Dis Allied Sci 2000;42:95-100. 17. Simes RJ. An improved Bonferroni procedure for multiple tests of significance. Biometrika 1986;73, 751-4. 18. Powell C, Kolamunnage-Dona R, Lowe J, Boland A, Petrou S, Doull I, Hood K, Williamson P on behalf of the MAGNETIC study group.MAGNESIUM TRIAL IN CHILDREN MAGNETIC: A Randomised, Placebo Controlled Trial of Nebulised Magnesium Sulphate in Acute Severe Asthma in Children. Lancet Respiratory Medicine 2013 19 Figure 1: CONSORT flow chart Assessed for eligibility (n=2783) Enrolment Excluded (n= 1674) Ineligible (n=847) - Life threatening asthma (n=466) - Contraindicated (n=73) - Received magnesium in previous 24 hours (n=19) - Previous participant (n=319) Declined to participate (n=200) Administrative reasons (ED too busy, staff not trained no treatment pack available; n=306) Unable to give consent (n=31) Other reasons (n=201) Not recorded (n=89) Randomised (n=1109) Allocation Allocated to nebulised magnesium sulphate (n=339) Received intervention (n=333) Did not receive intervention (n=6) Withdrew consent prior to treatment (n=2) Treatment pack not available (n=4) Allocated to IV magnesium sulphate (n=406) Received allocated intervention (n= 396) Did not receive intervention (n=10) Withdrew consent prior to treatment (n=7) Treatment pack not available (n=2) Self-discharged prior to treatment (n=1) Allocated to placebo (n=364) Received allocated intervention (n=358) Did not receive intervention (n=6) Withdrew consent prior to treatment (n=2) Treatment pack not available (n=3) Self-discharged prior to treatment (n=1) Follow-Up Completed follow-up in ED (n=332) 30-day questionnaire completed (n=152) Completed follow-up in ED (n=393) 30-day questionnaire completed (n=186) Completed follow-up in ED (n=357) 30-day questionnaire completed (n=162) Analysis Analysed (n=332) Excluded from analysis (n=7) Treatment not started (n=6) Ineligible patient, prisoner (n=1) Analysed (n=394) Excluded from analysis (n=12) Treatment not started (n=10) Ineligible patient, previous participant (n=2) 20 Previous participant (n=2) Analysed (n=358) Excluded from analysis (n=6) Treatment not started (n=6) Figure 2: Length of stay following initial attendance Length of stay following initial attendance 1.00 0.75 0.50 0.25 0.00 0 4 8 12 24 Placebo 48 Time to discharge (hours) Nebulised Mg 21 72 96 IV Mg Table 1: Baseline demographics and characteristics Nebulised magnesium sulphate (N=332) IV magnesium sulphate (N=394) Placebo (N=358) Total (N=1084) 36.5 (14.8) 35.0 (23, 47) 16, 85 35.6 (13.1) 34.0 (25, 44) 16, 84 36.4 (14.1) 34.5 (24, 47) 16, 88 36.1 (14.0) 34.0 (24, 46) 16, 88 Gender Male Female 100 (30%) 232 (70%) 115 (29%) 279 (71%) 106 (30%) 252 (70%) 321 (30%) 763 (70%) Ethnicity White Mixed Asian or Asian British Black or Black British Other Not stated Missing 286 (86%) 2 (1%) 14 (4%) 2 (1%) 2 (1%) 22 (7%) 4 (1%) 369 (94%) 1 (<1%) 8 (2%) 5 (1%) 0 8 (2%) 3 (1%) 319 (89%) 5 (1%) 16 (4%) 4 (1%) 0 11 (3%) 3 (1%) 974 (90%) 8 (1%) 38 (4%) 11 (1%) 2 (<1%) 41 (4%) 10 (1%) Smoking status Never Current Previous Missing 151 (45%) 98 (30%) 72 (22%) 11 (3%) 156 (40%) 138 (35%) 95 (24%) 5 (1%) 143 (40%) 127 (35%) 81 (23%) 7 (2%) 450 (42%) 363 (33%) 248 (23%) 23 (2%) 324 430.0 (118.8) 425.0 (350, 500) 100, 700 29 (9%) 389 431.8 (116.9) 435.0 (350, 500) 140, 800 42 (11%) 346 435.0 (110.8) 425.0 (350, 500) 150, 790 27 (8%) 1059 432.3 (115.4) 425.0 (350, 500) 100, 800 98 (9%) 69 (21%) 66 (17%) 68 (19%) 203 (19%) Age Mean (s.d.) Median (i.q.r.) Min-max Predicted PEFR n Mean (s.d.) Median (i.q.r.) Min-max Other previous serious lung disease Other serious illness 22 Table 2: Admission to hospital at presentation or within seven days Status at four hours Admitted Discharged Dead Unknown Subsequent hospital admission within seven days Subsequent hospital admission following discharge at initial attendance Admitted to hospital at any time within seven days Nebulised magnesium sulphate (N=332) IV magnesium sulphate (N=394) Placebo (N=358) Total (N=1084) 254 (77%) 77 (23%) 0 1 (<1%) 279 (71%) 114 (29%) 0 1 (<1%) 278 (78%) 80 (22%) 0 0 811 (75%) 271 (25%) 0 2 (<1%) 15 (5%) 10 (3%) 7 (2%) 32 (3%) 6 (2%) 5 (1%) 3 (1%) 14 (1%) 261 (79%) 285 (72%) 281 (78%) 827 (76%) Comparisons Active v placebo IV v nebuliser IV v placebo Nebuliser v placebo Odds ratio (95% CI) 0.84 (0.61,1.15) 0.76 (0.53,1.10) 0.73 (0.51,1.04) 0.96 (0.65,1.40) 23 p-value 0.276 0.146 0.083 0.819 Table 3: Change in VAS breathlessness from baseline to two hours Nebulised magnesium IV magnesium Placebo (N=332) (N=394) (N=358) VAS at baseline No. of obs. 326 386 349 Mean (s.d.) 61.6 (23.3) 61.9 (22.8) 63.1 (23.5) Change in VAS at 1 hour No. of obs. Mean (s.d.) 314 -18.4 (22.8) 372 -24.2 (24.4) Overall (N=1084) 1061 62.2 (23.2) 344 -21.5 (24.7) 1030 -21.5 (24.1) Change in VAS at 2 hours No. of obs. 296 357 323 Mean (s.d.) -28.2 (27.4) -34.3 (27.7) -31.3 (29.4) Comparisons Mean difference (95% CI) Active v placebo 0.0 (-1.9,1.9) IV v nebuliser -5.1 (-9.4,-0.8) IV v placebo -2.6 (-6.8,1.6) Nebuliser v placebo 2.6 (-1.8,7.0) 976 -31.5 (28.2) p-value 0.999 0.019 0.231 0.253 24 Table 4: Change in PEFR (% of predicted) from baseline to two hours Nebulised magnesium (N=332) %PEFR at baseline No. of obs. Mean (s.d.) IV magnesium (N=394) 308 50.0 (19.6) Placebo (N=358) Overall (N=1084) 375 54.3 (20.2) 327 50.5 (19.1) 1010 51.7 (19.7) 282 349 304 935 9.9 (15.0) 11.4 (15.7) 10.2 (14.7) 10.6 (15.2) Change in %PEFR at 2 hours No. of obs. 270 Mean (s.d.) 13.4 (18.0) 337 14.4 (17.4) 291 14.4 (16.3) 898 14.1 (17.2) Change in %PEFR at 1 hour No. of obs. Mean (s.d.) Comparisons Active v placebo IV v nebuliser IV v placebo Nebuliser v placebo Mean difference -0.5 (-2.9,1.9) 0.3 (-2.4,3.0) -0.4 (-3.0,2.3) -0.6 (-3.4,2.1) 25 p-value 0.676 0.841 0.786 0.652 Table 5: Analysis of length of stay and use of ICU, HDU and ventilation Length of stay (hours) n Mean (s.d.) Median (i.q.r.) Min-max Days on ICU No (%) with any stay Mean (s.d.) Median (i.q.r.) Days on HDU No (%) with any stay Mean (s.d.) Median (i.q.r.) Required ventilation Non-invasive Emergency intubation Nebulised magnesium sulphate IV magnesium sulphate Placebo Total (N=332) (N=394) (N=358) (N=1084) 329 63.2 (79.7) 35.1 (5, 88) 3, 623 388 57.0 (75.1) 31.5 (4, 78) 4, 723 353 63.3 (84.3) 36.4 (5, 87) 1, 694 1070 61.0 (79.6) 34.1 (4, 84) 1, 723 9 (3%) 3.3 (4.8) 2.0 (1, 4) 11 (3%) 3.1 (5.0) 2.0 (0, 4) 5 (1%) 2.9 (3.9) 2.0 (0, 4) 22 (7%) 3.3 (4.8) 2.0 (1, 4) 23 (6%) 3.1 (5.0) 2.0 (0, 4) 3 (1%) 2 (1%) 2 (1%) 6 (2%) 2 (1%) 4 (1%) 26 P-values Active v placebo IV v nebuliser 0.659 0.432 0.379 0.230 25 (2%) 3.1 (4.6) 2.0 (0, 4) 0.161 0.947 0.159 0.941 20 (6%) 2.9 (3.9) 2.0 (0, 4) 65 (6%) 3.1 (4.6) 2.0 (0, 4) 0.690 0.661 0.715 0.630 4 (1%) 3 (1%) 1 (<1%) 13 (1%) 7 (1%) 7 (1%) 0.936 0.458 Table 6: Adverse events and side effects Adverse events Any adverse event Arrhythmia Cardiac arrest Death Intubation Non-invasive ventilation Other asthma related Other non-asthma related Side effects Any side effect Flushing Hypotension Nausea Vomiting Other Comparisons* Active v placebo IV v nebuliser IV v placebo Nebuliser v placebo Nebulised magnesium sulphate (N=332) IV magnesium sulphate (N=394) Placebo (N=358) Overall (N=1084) 41 (12.3%) 0 0 1 (0.3%) 2 (0.6%) 2 (0.6%) 26 (7.8%) 53 (13.5%) 1 (0.3%) 1 (0.3%) 1 (0.3%) 4 (1.0%) 2 (0.5%) 26 (6.6%) 36 (10.1%) 1 (0.3%) 0 0 1 (0.3%) 3 (0.8%) 22 (6.1%) 130 (12.0%) 2 (0.2%) 1 (0.1%) 2 (0.2%) 7 (0.6%) 7 (0.6%) 74 (6.8%) 14 (4.2%) 20 (5.1%) 12 (3.4%) 46 (4.2%) (N=332) (N=394) (N=358) (N=1084) 52 (15.7%) 3 (0.9%) 31 (9.3%) 5 (1.5%) 6 (1.8%) 12 (3.6%) 61 (15.5%) 7 (1.8%) 31 (7.8%) 14 (3.5%) 6 (1.5%) 15 (3.8%) 36 (10.1%) 2 (0.6%) 22 (6.1%) 7 (2.0%) 3 (0.8%) 5 (1.4%) 149 (13.7%) 12 (1.1%) 84 (7.7%) 26 (2.4%) 15 (1.4%) 32 (2.9%) Odds ratio (95% CI) 1.68 (1.11,2.52) 1.00 (0.66,1.52) 1.68 (1.07,2.63) 1.67 (1.05, 2.66) p-value 0.014 0.988 0.025 0.031 n.b. Numbers refer to patients experiencing an event of each type. Total number of events will not equal the sum of individual events if a patient experiences multiple side effects. * comparison is any side effect (yes/no) 27 Table 7: Medications given at discharge Discharged at 4 hours Any medication Prednisolone Salbutamol Seretide Beclometasone Pulmicort Ipratropium Salmetarol Combivent Other Nebulised magnesium sulphate (N=332) 77 IV magnesium sulphate (N=394) 114 Placebo (N=358) 80 Overall (N=1084) 271 64 (83%) 62 (81%) 21 (27%) 3 (4%) 1 (1%) 3 (4%) 1 (1%) 0 1 (1%) 0 98 (86%) 93 (82%) 44 (39%) 4 (4%) 4 (4%) 3 (3%) 1 (1%) 1 (1%) 0 2 (2%) 64 (80%) 63 (79%) 27 (34%) 2 (3%) 3 (4%) 0 0 0 0 0 226 (83%) 218 (80%) 92 (34%) 9 (3%) 8 (3%) 6 (2%) 2 (1%) 1 (<1%) 1 (<1%) 2 (1%) 28