CNS Infections Faculty Copy - Page 1 VIROLOGY CASE
advertisement

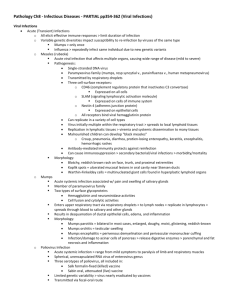
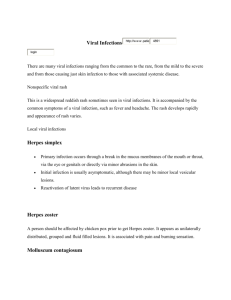
CNS Infections Faculty Copy - Page 1 VIROLOGY CASE-BASED SMALL GROUP DISCUSSION SESSION 31 CNS INFECTIONS MONDAY, APRIL 23, 2001 10:30AM – 12:30PM Reading Assignment: Sherris Medical Microbiology, Chapters 35, 37, 39, 40 CNS Infections Faculty Copy - Page 2 CASE HISTORY 1 The patient was a 3 month-old male who presented in August with a fever of 39.2C, extreme irritability and vomiting. His fontanelles were normal and his neck was supple. The rest of his examination was unremarkable. A lumbar puncture was done and CSF revealed a WBC count of 75/mm3 with 72% neutrophils, 8% lymphocytes, and 20% monocytes; the glucose level was 60 mg/dl and the protein level was 22 mg/dl (both normal). A Gram stain was negative for bacteria. CSF samples were sent for viral cultures. Intravenous ceftriaxone was begun empirically for presumed bacterial meningitis. Blood, urine, and CSF bacterial cultures were negative and ceftriaxone was discontinued on the second day. He was discharged on the third hospital day as his symptoms were improved. After discharge, his CSF viral culture became positive for an enterovirus. BACKGROUND Viruses of the enterovirus group (coxsackievirus, echovirus, and poliovirus) characteristically cause this type of illness during late summer and early fall. These are single-stranded RNA viruses known as picornaviruses. This patient's viral culture was positive for coxsackievirus. Many types of enteroviruses can cause aseptic meningitis. The incidence is highest in children less than 1 year old, such as this patient. Myocarditis, pericarditis, and pleurodynia are associated with group B coxsackievirus. Polioviruses characteristically cause paralysis (usually asymmetric), but wild type poliovirus has fortunately been eradicated from the Americans. (rare cases of vaccineassociated polio have led to a change to use of IPV prior to OPV in routine childhood immunization schedules). Herpangina (vesicular oral ulcers) and hand-foot-and-mouth disease are classically caused by group A coxsackieviruses. A variety of coxsackieviruses and echoviruses have been associated with benign viral exanthems, mimicking measles or rubella. STUDY QUESTIONS 1. What isolation should the patient be put in? Patients should be put in enteric isolation. Enteroviruses are transmitted mostly by the fecal-oral route, but some serotypes may be spread by respiratory secretions or fomites. 2. What is known about the pathogenesis of the infection? Differences in pathogenesis for the enteroviruses mainly result from differences in tissue tropism and cytolytic capacity of the virus. The upper respiratory tract, the oropharynx, and the intestinal tract are the portals of entry for the enteroviruses. The virions are impervious to stomach acid, proteases, and bile. The virus initiates replication in the mucosa and lymphoid tissue of the tonsils and pharynx and later infects lymphoid cells of Peyer's patches underlying the intestinal CNS Infections Faculty Copy - Page 3 mucosa. Primary viremia spreads the virus to receptor-bearing target tissues, where a second phase of viral replication may occur, resulting in symptoms and a secondary viremia. Virus shedding from the oropharynx can be detected for a short time before symptoms begin, whereas virus production and shedding from the intestine may last for 30 days or longer, even in the presence of a humoral immune response. Coxsackieviruses and echoviruses recognize receptors expressed on many cell types and tissues and cause a broad repertoire of disease. These and other enteroviruses recognize receptors on cells of the central nervous system, heart, lung, pancreas, and other tissues. Most enteroviruses are cytolytic, replicating rapidly and causing direct damage to the target cell. Antibody is the major protective immune response to the enteroviruses. Secretory antibody can prevent the initial establishment of infection in the oropharynx and gastrointestinal tract, and serum antibody prevents viremic spread to the target tissue and therefore disease. Serum antibody is generally observed 7 to 10 days after infection. Figure 1. Pathogenesis of enteroviruses. The target tissue infected by the enterovirus determines the predominant disease caused by the virus. CNS Infections Faculty Copy - Page 4 3. How is the viral infection detected? The finding of >5 white blood cells/mm 3 of CSF is abnormal and is indicative of meningitis. The patient was treated for bacterial meningitis because of the predominance of neutrophils in the CSF. Early in the course of viral meningitis (the first 24 to 48 h), neutrophils can be predominant. However, mononuclear cells are predominant later in the disease. The normal CSF glucose level also argues against bacterial meningitis. Finally, a positive CSF viral culture confirms the diagnosis of viral meningitis. 4. Why was there a neutrophil predominance on the LP? Neutrophil is a common finding in early viral meningitis, but as indicated above, mononuclear cells predominate later in the disease. 5. What is the appropriate treatment for this viral infection? The management of patients with enteroviral infections includes supportive care. Infection control measures are recommended for patients and their families to interrupt transmission of virus to others who may be susceptible. These include handwashing. This is of particular importance in day-care centers, where agents that are spread by the fecal-oral route are of particular concern. A new drug that inhibits the uncoating of picornavirus particles is being evaluated in clinical trials. Pleconaril binds reversibly to a hydrophobic pocket in the outer coat protein (VPI) of picornaviruses. Binding in this site prevents uncoating of the virion RNA following attachment and penetration of the cell membrane. Inhibiting this step prevents replication of the RNA and production of progeny virions. The compound has undergone extensive in vitro sensitivity testing against over 215 clinical isolates of enterovirus strains known to cause serious human disease; over 90% of the 100 known rhinovirus serotypes at a concentration of 1 ug/ml. Pleconaril was protective in several mortality studies conducted in weanling, suckling and adult mice infected with several different strains of coxsackievirus. Clinical Studies Pleconaril has been studied in over 700 human adult and pediatric volunteers and patients in 17 completed clinical studies to date, as well as in six ongoing placebo controlled trials of the clinical trials conducted to date, pleconaril has been very well tolerated, with an aggregate side effect profile similar to placebo. Phase I Pleconaril exhibits dose-dependent linear pharmacokinetics resulting in plasma levels at pharmacodynamic steady state that are in excess of levels required to inhibit viral replication of rhinoviruses and enteroviruses. Pediatric pharmacokinetics are similar to that of adults, requiring no dosage adjustment for children. Neonatal pharmacokinetic studies are currently underway. CNS Infections Faculty Copy - Page 5 Viral Meningitis In a placebo controlled adult enteroviral meningitis study, pleconaril treatment resulted in a statistically significant shortening of disease duration (54% reduction, 11 vs. 5 days; p = 0.0005) the primary endpoint of the study. Elements of the primary endpoint included clinically important symptoms of viral meningitis such as a reduction in severe incapacitating headache, which usually leads to hospitalization. Pleconaril was statistically superior to placebo in the secondary endpoints of the time to complete absence of headache (50% reduction, 14 vs. 7 days; p = 0.014), duration of analgesic use (50% reduction, 12 vs. 6 days; p = trends favoring pleconaril were also observed in other secondary endpoints, including a reduction in the time to return to work and a reduction in the time return to full levels of leisure activity. Viral Respiratory Infections Pleconaril demonstrated pronounced and clinically significant reductions in respiratory and systemic symptoms resulting from the intranasal administration of a safety-tested strain of coxsackievirus A-21 in health volunteers when compared to placebo. Clinical studies are currently underway in vial respiratory disease in odds media prone children, patients with asthma, and otherwise normal subjects. Pharmaceutics Pleconaril is supplied as a cherry-peppermint flavored oral liquid containing pleconaril at a concentration of 40 milligrams per milliliter in medium chain triglycerides (Miglyol 810) 2 % surfactants (Tween 80 and Arlacel) as well as 0.15% saccharin. This formulation is palatable when taken by children and adults. A tablet dosage form has been developed for the adult market. 6. Would this infection be likely to occur in February? No. Enterovirus meningitis outbreaks generally occur in the late summer and early fall. CNS Infections Faculty Copy - Page 6 CASE HISTORY 2 A 4 year old girl developed drowsiness, listlessness, abdominal pain, anorexia, sore throat, nasal congestion, drooling, and pain on the left side of the neck for 2 days. The following day, she developed fever to 104oF and behavioral changes. She had hallucinations, difficulty standing, insomnia, and refused to drink liquids. Other vital signs included pulse 210 and respiratory rate 32. WBC count was 20,800/mm3. Her initial diagnosis was possible drug ingestion. Urine toxicology screen was negative. A head CT scan was normal. She then developed a seizure and bradycardia, requiring cardiopulmonary resuscitation. She was transferred to an ICU with diagnosis of sepsis, encephalitis, or drug ingestion. Ceftriaxone and acyclovir were started. She developed coma and an EEG showed generalized sharp and slow wave discharges. Nine days after the onset of symptoms, she died. During the hospitalization, family members reported that approximately three weeks prior to the onset of symptoms, a bat had been found in the childs bedroom. The child had no obvious bite wounds and told her family that she had not been bitten by the bat. The family did not seek medical advice at that time and buried the bat in their backyard. The childs autopsy showed severe cerebral edema and brain herniation. Intracytoplasmic inclusions were present in the brain and spinal cord. Brain tissue and a nuchal skin biopsy sample taken one day prior to death were positive for rabies antigen by direct fluorescent antibody testing. The health department exhumed the bat. Nucleotide sequence analysis of sample generated by RT-PCR from the bat and the patient were identical. This is a true case which occurred in the state of Washington. Another interesting case involving a kitten in a pet store is in the optional reading. BACKGROUND Rabies virus is a negative strand RNA virus. Rabies is generally transmitted by a bite from an infected animal (bat, skunk, fox, dog or cat). Inhalation of heavily contaminated material, such as bat droppings, can also cause infection. Rabies virus first replicates in striated muscle tissue at the site of inoculation. It then enters the peripheral nervous system at the neuromuscular junctions and spreads up the nerves to the central nervous system, where it replicates exclusively within the gray matter. It then passes centrifugally along autonomic nerves to reach other tissues, including the salivary glands, adrenal medulla, kidneys, and lungs. Passage into the salivary glands in animals facilitates further transmission of the disease by infected saliva. CNS Infections Faculty Copy - Page 7 1. Should the patient have been in isolation? What was done for exposed contacts? The patient should have been in strict isolation to prevent transmission of rabies virus in her secretions (especially saliva) from infecting health care workers. All health care workers that came into contact with this patient were given post-exposure prophylaxis. (See answer to question #4). 2. What is the incubation period for rabies? The incubation period ranges from 10 days to a year, depending on the amount of virus introduced, the amount of tissue involved, the host immune mechanisms, and the distance the virus must travel from the site of inoculation of the central nervous system. Thus, the incubation period is generally shorter with face wounds than with leg wounds. Immunization early in the incubation period frequently aborts the infection. 3. Why is it difficult to diagnose this infection? What clinical symptom did this patient have which is classic for rabies (but is not always present)? Refusal of liquids with apparent fear of water (agoraphobia) is a classically described symptom of rabies. Laboratory diagnosis of rabies in animals or deceased patients is accomplished by indirect or direct demonstration of virus in brain tissue or scalp biopsy. Viral antigen can be demonstrated rapidly by immunofluorescence procedures. Intracerebral inoculation of infected brain tissue or secretions into suckling mice results in death in 3 to 10 days. Histologic examination of their brain tissue shows Negri bodies; both Negri bodies and rhabdovirus particles may be demonstrated by electron microscopy. Specific antibodies to rabies virus can be detected in serum, but generally only late in the disease. In many areas of the world, the dog is the most important vector of the rabies virus to humans. Other important sources of disease are the wolf in eastern Europe, the mongoose in Africa, the fox in western Europe, and the bat in Latin America and the United States. 4. If the family had reported finding the bat in the patients room immediately to the physician or health department, what treatment would the patient have received? The patient would have received rabies prophylaxis. Once symptoms appear, vaccine and immune globulin are ineffective. Postexposure prophylaxis requires careful evaluation and judgment. Every year more than one million Americans are bitten by animals, and in each instance a decision must be made whether to initiate postexposure rabies prophylaxis. In this decision the physician must consider (1) whether the individual came into physical contact with saliva or another substance likely to contain rabies virus; (2) whether there was significant wounding or abrasion; (3) whether rabies is known or suspected in the animal species and area associated with the exposure; (4) whether the bite was provoked or unprovoked (i.e., the circumstances surrounding the exposure); and (5) whether the animal is available for laboratory examination. Any wild animal or ill, unvaccinated, or stray domestic animal involved in a possible rabies exposure, such as an unprovoked bite, should be captured and killed. The head should be sent immediately to an appropriate laboratory, CNS Infections Faculty Copy - Page 8 usually at the state health department, for search for rabies antigen by immunofluorescence. If examination of the brain by this technique is negative for rabies virus, it can be assumed that the saliva contains no virus and that the exposed person requires no treatment. If the test is positive, the patient should be given postexposure prophylaxis. It should be noted that rodents and rabbits are not important vectors of rabies virus. The incubation period of rabies in dogs is short. Therefore, the animal can be observed and if it remains healthy for 10 days, it can be considered non-rabid. Postexposure prophylaxis is based on immediate, thorough washing of the wound with soap and water; passive immunization with hyperimmune globulin, of which at least half the dose should be instilled around the wound site; and active immunization with antirabies vaccine. With human diploid vaccine, five doses given on days 1,3, 7, 14 and 28 are recommended. Physicians should always seek the advice of the local health department when the question of rabies prophylaxis arises. 5. Who should routinely receive rabies virus vaccine? Currently, the prevention of rabies is divided into preexposure and postexposure prophylaxis. Preexposure prophylaxis is recommended for individuals at high risk of contact with rabies virus, such as veterinarians, spelunkers, laboratory workers, and animal handlers. The vaccine currently used in the United States for preexposure prophylaxis employs an attenuated rabies virus grown in human diploid cell culture and inactivated with β-propiolactone. Preexposure prophylaxis consists of two subcutaneous injections of vaccine given 1 month apart, followed by a booster dose several months later. Prevention is the mainstay of controlling human rabies. Intensive supportive care has resulted in two or three long-term survivals; despite the best modern medical care, however, the mortality still exceeds 90%. In addition, because of the infrequency of the disease, many cases die without definitive diagnosis. Human hyperimmune antirabies globulin, interferon and vaccine do not alter the diseases once symptoms have developed. CASE HISTORY 3 A 35 year old white female presented to the Emergency Room in January with fever and a left focal seizure. She had been previously healthy, but developed fever and malaise one day before the seizure CNS Infections Faculty Copy - Page 9 episode. In the Emergency Room, she was disoriented with a temperature of 39o C. Physical examination was otherwise unremarkable. A CT scan of the head showed a focal area of low attenuation in the right temporal region, but without brain shift, LP revealed 100 WBC with 100% lymphocytes, 100 RBC, protein 100, glucose 60 (protein , glucose normal) CSF gram stain and culture were negative. Acyclovir was initiated for presumed herpes encephalitis. CSF was sent for PCR for HSV1 and HSV2 and was positive for HSV1. Viral culture of CSF was negative. BACKGROUND Herpes Simplex Virus Type 1. (Enveloped, double-stranded DNA-virus). STUDY QUESTIONS 1. Should the patient be isolated? No. HSV encephalitis is sporadic, not epidemic, and not contagious. 2. Was this likely an acute or recurrent infection? Does HSV-2 cause encephalitis? Encephalitis may rarely result from HSV-1 infection. Herpes encephalitis accounts for up to 10% of all cases of viral encephalitis in the United States. Most cases occur in adults with high levels of anti-HSV-1 antibody, suggesting reactivation of latent virus in the trigeminal nerve root ganglion and extension of productive (lytic) infection into the temporoparietal area of the brain. Primary HSV infection with neurotropic spread of the virus from peripheral sites up the olfactory bulb into the brain may also result in parenchymal brain infection. HSV-2 can also cause encephalitis in neonates, as a primary infection acquired from the mother. 3. What clinical findings suggest herpes encephalitis as the diagnosis? Classically, the disease affects one temporal lobe, leading to focal neurologic signs and cerebral edema. If untreated, mortality is 70%. Clinically, the disease can resemble brain abscess, tumor, or intracerebral hemorrhage. In neonates, the infection is less often focal. 4. Why was PCR used to detect this viral infection instead of serology or virus isolation? Rapid diagnosis is very important and there are encouraging results suggesting that HSV can be detected in cerebrospinal fluid by the polymerase chain reaction (PCR), although the virus is rarely, if ever, cultured from this site. Brain biopsy with culture of the virus from brain tissue has previously been the gold-standard method of diagnosis. 5. What is the mechanism of action of acyclovir? Intravenous acyclovir is effective in inhibiting viral replication. Acyclovir (ACV) is a nucleoside analogue of guanosine. ACV has selective action against those herpesviruses that encode a Thymidine Kinase (TK). The viral Thymidine Kinase activated the drug by phosphorylation, and host cell enzymes complete the process to the triphosphate form. No CNS Infections Faculty Copy - Page 10 initial phosphorylation occurs in uninfected cells, and thus there is no active drug to inhibit cellular DNA synthesis or to cause toxicity. Activation of acyclovir (acycloguanosine) in herpes simplex viral infected cells. Acyclovir is converted to acycloguanosine monophosphate (acyclovir GMP) by the herpes-specific viral thymidine kinase and then to acyclovir GTP by cellular kinases. In herpesvirus infected cells, ACV triphosphate competes with guanosine triphosphate and causes termination of the growing viral DNA chain because there is no 3'-hydroxyl group on the ACV molecule to allow chain elongation. The selectivity and minimal toxicity of ACV is also due to its 100-fold greater utilization by the viral DNA polymerase than by cellular DNA polymerase. Mutations in either the herpesvirus TK or polymerase can generate ACV resistant strains. These resistant strains are less virulent but can still cause disease in immunocompromised patients. Activity of ACV against herpesviruses directly correlates with the capacity of the virus to produce TK. The order of TK induction and ACV sensitivity is: HSV-1 and >VZV>>EBV>>>CMV CNS Infections Faculty Copy - Page 11 CASE HISTORY 4 A 16 year-old white male presented to the ER in August with fever and unresponsiveness. He was reportedly well until two days prior to admission, when he developed low grade fever and lethargy. He gradually became more somnolent. The patient lived in a rural area, and had been playing football frequently in a field next to an old tire dump. In the ER, he was responsive only to deep pain. There were no focal neurologic defects and no other abnormalities on physical examination except for numerous mosquito bites. A CT scan of the head showed no abnormalities. LP showed 400 WBC, 90% lymphocytes, O RBC; protein 40, glucose 60 (both normal) CSF gram stain and culture were negative. EEG showed diffuse slow wave activity, nonfocal. Acute and convalescent viral titers to La Cross virus were negative and 1:640, respectively. After 3 days, the patient became responsive and completely recovered 7 days after onset of illness. BACKGROUND La Cross virus is a negative strand RNA virus with a segmented genome. La Cross virus is a member of the California encephalitis virus group of viruses in the Bunyaviridae family. The virus is a transmitted by the bite of an infected mosquito (Aedes triseriatus). This mosquito vector is common in suburban and rural areas. STUDY QUESTIONS 1. Should this patient be isolated? No. He is not infectious. However, at presentation you would not know the diagnosis, would consider enterovirus as a possible cause, and would therefore place the patient in enteric isolation. 2. What is known about the pathogenesis of the infection? Infection of the human by a biting, infected arthropod is followed by viremia, which is apparently amplified by extensive virus replication in the reticuloendothelial system and vascular endothelium. After replication, the virus becomes localized in various target organs, depending on its tropism, and illness results. The viruses produce cell necrosis with resultant inflammation which leads to fever in nearly all infections. If the major viral tropism is for the central nervous system (CNS), virus reaching this site by crossing the blood-brain barrier or along neural pathways can cause meningeal inflammation (aseptic meningitis) or neuronal dysfunction (encephalitis). The CNS pathology consists of meningeal and perivascular mononuclear cell infiltrates, degeneration of neurons with neuronophagia, and occasionally destruction of the supporting structure of neurons. 3. Describe how the viral infection was detected? Prior to the serology, what key laboratory findings pointed to a viral encephalitis? Specific diagnosis is usually accomplished by serologic techniques using acute and convalescent sera. The arboviruses may be isolated in various culture systems (but not in CNS Infections Faculty Copy - Page 12 most hospital laboratories); for most agents, however, isolation is by intracerebral inoculation of newborn mice, which often results in encephalitis and death. The viruses may be found in the blood (viremia) from a few days before onset of symptoms through the first 1 to 2 days of illness; attempts at isolation from the blood are generally useful only when viremia is prolonged, as in dengue, Colorado tick fever, and some of the hemorrhagic fevers. Virus is not present in the stool and is rarely found in the throat; viral recovery from cerebrospinal fluid is also unusual. Virus can be isolated readily from affected tissue during the acute phase of illness, but this approach is seldom practical in diagnosis. Various diagnostic serologic tests have been used including hemagglutination inhibition, complement fixation, virus neutralization methods, and enzyme immunoassay. Early rapid presumptive diagnosis can sometimes by made by the detection of IgM-specific antibodies that often appear within a few days of onset and persist 1 to 2 months, but these tests are not generally commercially available. The presence of 90% lymphocytes in the LP is consistent with a viral encephalitis 4. What is the appropriate treatment for this infection? Supportive care only. No specific treatment is available. 5. Are there any long term consequences associated with this viral infection? No. Recovery is generally complete with lasting immunity. However, patients with eastern equine encephalitis may have poorer outcome with long-term neurologic sequelae. CNS Infections Faculty Copy - Page 13 SLIDES FOR VIROLOGY CNS INFECTIONS CASE 3 Slides 1 and 2 CT scans of a patient with Herpes encephalitis. Slide 1 is at day 3 of illness, and slide 2 is at day 10 of illness. Note the progression of severe hemorrhagic infarction throughout the brain. This patient was treated with acyclovir but had significant neurologic sequelae. Slides 3 and 4 MR scans of the neonate with Herpes encephalitis caused by Herpes Simplex Virus Type 2. Slide 3 is at day 2 of illness and slide 4 is at day 9 of illness. Note that hemorrhagic infarction is most severe in frontal and temporal lobes. This baby was treated with acyclovir but died at day 30. CNS Infections Faculty Copy - Page 14 OPTIONAL ARTICLES FOR CASE STUDIES 1. Management of central nervous system infections during an epidemic of enteroviral aseptic meningitis. (1980), Jonathan I. Singer, M.D., Phillip R. Maur, M.D., John P. Riley, M.D., and Pamela Burger Smith, B.S., Pediatrics, Vol 96, No. 3 part 2:559-563. 2. Mass Treatment of Humans Exposed to Rabies-New Hampshire, 1994, (1994), MMWR Vol. 44 No. 26:484-486. 3. Case Records of the Massachusetts General Hospital: Case 21 - 1998. NEJM 339: 105112. 4. Review Article: Viral Encephalitis, (1990), Richard J. Whitley, M.D., New England Journal of Medicine, Vol 323, No 4:242-250. 5. Arbovirus Disease-United States, 1993, (1994), MMWR, Vol No 21:385-387. 6. Human Rabaies - California, Georgia, Minnesota, New York and Wisconsin, 2000. MMWR, Vol No 49: 1111-1115. *****