HELP_Health-Care-Homes-Help_Data-Entry
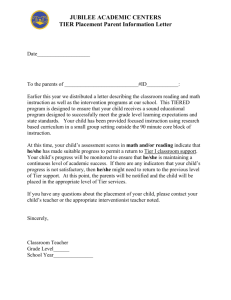
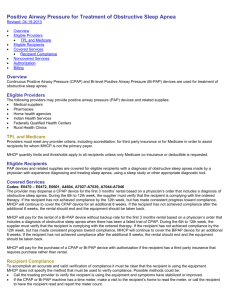
advertisement

Health Care Homes Help — Data Entry Results Screen Tier e Results Overview Aggregated Diagnostic Groups (ADG) Complexity Level Modifier Expanded Diagnostic Cluster (EDC) Language Mental Illness MHCP Found MTMS (Medication Therapy Management Services) NPI P4P (Pay-for-performance) Resource Utilization Band (RUB) Tier Level <br> Overview The HCH Data Entry Results is a guide for the health care home team at your clinic. Review every recipient’s/patient’s preliminary tier assignment to confirm that the patient complexity was accurately assessed. Aggregated Diagnostic Groups (ADG) ADGs are groups of ICD diagnosis codes that are homogenous with respect to clinical criteria and expected need for healthcare services. The ADG categories reflect the entire spectrum of care, with certain ADGs indicating preventive care, while others assigned when specialty care is more likely. Recipients/Patients with only one diagnosis over a time period are assigned only one ADG, while a recipient/patient with multiple diagnoses can be assigned to one or more ADGs. To be included in HCH Tiers 1-4, a patient must be included in at least one ADG group that indicates that their condition is chronic, severe, and requires a care team to coordinate services in order to attain or maintain the recipient’s/patient’s stability or to reach their optimal goals. Time-limited ADGs (ADG 3 and ADG 4) do not meet HCH Tier eligibility criteria. ADGs are generated by the MHCP risk adjustment software, the ACG System.,. Complexity Level Modifier The Health Care Home modifier defined by MHCP as indicating the Tier level. One Complexity Level Modifier is required when billing the S0280 or S0281 procedure code. See the Tier Level description for more information. Expanded Diagnostic Cluster (EDC) EDC’s are broad groupings of diagnosis codes that remove differences in coding behavior between practitioners. ICD codes within an EDC share similar clinical characteristics and evoke similar types of diagnostic and therapeutic responses. The main criterion used for the ICD-to-EDC assignment is diagnostic similarity. EDC groups are generated by mapping ICD codes that refer to the same disease or condition to a single EDC. EDCs that are associated with the same organ system are rolled up into condition groups that are summed and mapped to a HCH tier level. EDC condition groups that do not indicate a need for sustained care coordination do not meet HCH tier eligibility criteria. These include: ADM (administrative). GSU (general surgery), GSI (general signs and symptoms), NEW (neonatal), and REC (reconstructive) classes. EDCs are generated by the MHCP risk adjustment software, the ACG® System. Refer to the EDC Code and Description list for a complete description. Language Indicator field for provider use. Mark 'Y' if recipient/patient needs to communicate about their health care in a non-English primary language. This means that the recipient’s/patient’s English skill levels are not sufficient to discuss and create complicated care plans, complex care choices and options, etc. This also includes those recipient’s/patients who are hearing impaired and require a sign language interpreter. Please consider whether the language barrier is significant enough to prevent a discussion with a recipient’s/patient’s care team for care coordination services for patients with severe chronic conditions. If so, the U3 modifier should be used when billing the S0280 or S0281 procedure code. This extra designation for non-English speaking recipients/patients is in addition to any billing that is done for interpreter services for interpretation. This designation is for the extra work of care coordination. Mental Illness A “Y” indicates the recipient’s/patient’s conditions indicate a “Serious and Persistent Mental Illness”. These “Serious and Persistent Mental Illness” are defined in Minnesota Statute 245.462, subdivision 20. The health care home team should review the recipient’s/patient’s record to confirm whether the diagnosis is associated with some level of functional impairment resulting in a more intense need for care coordination. If so and the patient is a MHCP recipient, the U4 modifier should be used when billing the S0280 or S0281 procedure code. This designation is in addition to the condition count for the condition group associated with the mental health diagnoses. ‘U4’ means that a diagnosis of schizophrenia, bipolar disorder, major depression or borderline personality disorder was entered for this recipient/patient. The U4 modifier may also be used when the caregiver of a dependent recipient has these diagnoses. If so and the patient is not a MHCP recipient, contact the payer for more billing information. MHCP Found A “Y” value indicates the recipient’s major program is eligible for health care home services. MTMS (Medication Therapy Management Services) A “Y” means that the recipient/patient is potentially eligible for the MHCP MTMS program, based on the number of chronic diagnoses that had been entered. If the patient is a MHCP recipient, see the MHCP Provider Manual – Medication Therapy Management Services chapter for additional eligibility requirements. If the patient is not a MHCP recipient, contact the payer for potential eligibility on a similar program. NPI NPIs are the standard unique health identifier to use in submitting and processing health care claims and other transactions. P4P (Pay-for-performance) MHCP fee-for-service (FFS) recipients of the Medical Assistance (MA), General Assistance Medical Care (GAMC) and MinnesotaCare programs are eligible for the MHCP Pay-for-Performance program if the provider renders optimal chronic disease care and the patient meets the following criteria: 1. Be 18-75 years of age 2. Have a diagnosis in one or both of the following categories: Diabetes Cardiovascular disease <br> A "C" means that cardiovascular diagnoses covered by the MHCP Pay-for-Performance program were entered for the recipient/patient. A "D" means that diabetes diagnoses covered by the MHCP Pay-for-Performance program were entered for the recipient/patient. A “B” means that the diagnoses covered under both Pay-for-Performance programs were entered for the recipient/patient. If the patient is a MHCP recipient, MHCP fee-for-service (FFS0 providers who render optimal chronic disease care to their qualifying MHCP FFS recipients are eligible for $250 results awards twice in 12 months. See MHCP Industry Initiatives – Pay-for-performance for additional eligibility requirements. If the patient is not a MHCP recipient, contact the payer for potential eligibility on a similar program. Resource Utilization Band (RUB) RUBs are groups of ACGs that have similar resource use. RUBs can be used as an indicator of severity/co-morbidity. 0 = no or only invalid diagnoses, 1 = healthy health care users, 2 = low morbidity, 3 = moderate morbidity, 4 = high morbidity, 5 = very high morbidity. RUBs are generated by the MHCP risk adjustment software, the ACG System. Tier Level The preliminary Health Care Home tier level calculated by the Tier e-Tool based on the diagnoses and medications entered for the recipient/patient. The accuracy of the Tier e-Tool tier assignment depends on a complete list of ICD codes being submitted for each recipient/patient. The chronic disease diagnoses are grouped in condition groups based on organ system. The Tier e-Tool generates a count of chronic condition groups for each recipient/patient. The Tier e-tool converts the count of chronic condition groups into a preliminary HCH tier using the table shown below. Number of Condition Groups 0 1–3 4–6 7–9 10 or more HCH Tier Complexity Tier Level 0 1 2 3 4 None U1 TF U2 TG