Positive-Airway
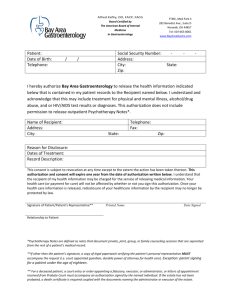
advertisement

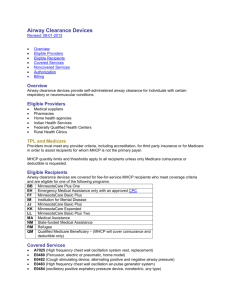
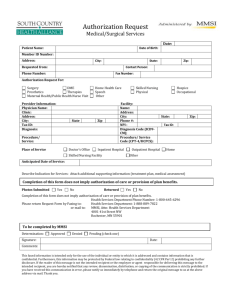
Positive Airway Pressure for Treatment of Obstructive Sleep Apnea Revised: 04-19-2013 Overview Eligible Providers TPL and Medicare Eligible Recipients Covered Services Recipient Compliance Noncovered Services Authorization Billing Overview Continuous Positive Airway Pressure (CPAP) and Bi-level Positive Airway Pressure (Bi-PAP) devices are used for treatment of obstructive sleep apnea. Eligible Providers The following providers may provide positive airway pressure (PAP) devices and related supplies: Medical suppliers Pharmacies Home health agencies Indian Health Services Federally Qualified Health Centers Rural Health Clinics TPL and Medicare Providers must meet any provider criteria, including accreditation, for third party insurance or for Medicare in order to assist recipients for whom MHCP is not the primary payer. MHCP quantity limits and thresholds apply to all recipients unless only Medicare co-insurance or deductible is requested. Eligible Recipients PAP devices and related supplies are covered for eligible recipients with a diagnosis of obstructive sleep apnea made by a physician with experience diagnosing and treating sleep apnea, using a sleep study or other appropriate diagnostic tool. Covered Services Codes: E0470 – E0472, E0601, A4604, A7027-A7039, A7044-A7046 The provider may dispense a CPAP device for the first 3 months’ rental based on a physician’s order that includes a diagnosis of obstructive sleep apnea. During the 6th to 12th week, the supplier must verify that the recipient is complying with the ordered therapy. If the recipient has not achieved compliance by the 12th week, but has made consistent progress toward compliance, MHCP will continue to cover the CPAP device for an additional 8 weeks. If the recipient has not achieved compliance after the additional 8 weeks, the rental should end and the equipment should be taken back. MHCP will pay for the rental of a Bi-PAP device without backup rate for the first 3 months rental based on a physician’s order that includes a diagnosis of obstructive sleep apnea when there has been a failed trial of CPAP. During the 6th to 12th week, the supplier must verify that the recipient is complying with the ordered therapy. If the recipient has not achieved compliance by the 12th week, but has made consistent progress toward compliance, MHCP will continue to cover the BiPAP device for an additional 8 weeks. If the recipient has not achieved compliance after the additional 8 weeks, the rental should end and the equipment should be taken back. MHCP will pay for the purchase of a CPAP or Bi-PAP device with authorization if the recipient has a third party insurance that requires purchase rather than rental. Recipient Compliance To accomplish an accurate and valid verification of compliance it must be clear that the recipient is using the equipment. MHCP does not specify the method that must be used to verify compliance. Possible methods could be: Call the treating provider to verify the recipient is using the equipment and symptoms have stabilized or improved. If the CPAP or Bi-PAP machine has a time meter, make a visit to the recipient’s home to read the meter, or call the recipient to have the recipient read and report the meter count. Keep documentation of the compliance verification in the recipients file. Recommended documentation: Date of verification Method of verification Reading of the time meter from the machine Speaking with the treating provider Name of the treating provider Name of the person within your organization that performed the verification. If the recipient is not using the equipment, the rental should end and the equipment should be taken back MHCP will pay for the rental of a Bi-PAP device with backup rate for recipients with obstructive sleep apnea and coexisting breathing disorders. Both diagnoses must be on the claim. For recipients without obstructive sleep apnea, refer to Respiratory Assist Device policy. Payment is limited to 13 months rental. Before dispensing masks or other supplies, providers must verify with the recipient that the CPAP/BiPAP device is still in use, and that replacement of the supply is necessary because the existing supply is damaged or otherwise worn out. Refer to the Benefits Code Guide and the Medical Supply Coverage Guide (PDF) for coverage information and limits on supplies not specified here. Included with initial dispensing: Compressor CPAP valve (if separate from mask) Disconnection alarm (if needed) Filters Fuses Instruction manual Manometer Separately billable at initial dispensing: Head gear Mask Tubing Humidification device Noncovered Services Carrying case is a non-covered convenience item and is not medically necessary A positive airway pressure device is not covered after the 3rd month unless the supplier has verified patient compliance as described above. Authorization Authorization is required for all purchases of positive airway pressure devices. Authorization is required for maintenance service agreements for E0470-E0472. Maintenance service agreements are not available for E0601. Authorization may be approved for PAP supplies in excess of MHCP limits when necessary. Authorization will not be approved due to willful or careless destruction of supplies by a recipient unless there is documentation that the destruction was due to the physical or mental impairment of the recipient. Submit authorization request and required documentation to the authorization medical review agent. Submit authorization request for maintenance service agreements using the appropriate HCPCS code and the modifier MS via MN–ITS or the MHCP Authorization Request (DHS-4695). Submit authorization request for purchase using the appropriate HCPCS code and the modifier NU via MN–ITS or the MHCP Authorization Request (DHS-4695). Include documentation of the TPL determination. Billing Positive Airway Pressure devices are capped rental only unless a primary payer requires purchase. Use X12 Batch or MN–ITS 837P Professional electronic claim Report the ordering provider in the Other Provider Types section of the MN–ITS Interactive claim If the recipient has Medicare, MHCP will pay the deductible / co-insurance on any units for which Medicare made payment. Any units for which Medicare denies payment must meet MHCP quantity and coverage limits. Bill the first 3 months using modifier RR and modifiers KH, KI and / or KJ as appropriate. When billing for rental after the first 3 months, use modifiers RR, modifiers KH, KI and / or KJ as appropriate and modifier KX if documentation in the file supports that the supplier has verified recipient compliance with treatment. Do not use modifier KX if the supplier has not verified compliance, or if the supplier has information that the recipient is not compliant with treatment except as described above. MHCP will deny claims for rental past the first 3 months, unless the RR and KX modifiers are present to indicate recipient compliance with treatment. Shipping/delivery costs are included in the MHCP maximum allowable payment and may not be separately billed to MHCP or the recipient. PAP devices are expected to serve the recipient for at least 5 years. If a device is stolen or damaged beyond repair, a replacement device may be covered. Submit a claim with an attachment (PDF) explaining why a replacement is required.