Why does inflammation cause anemia
advertisement

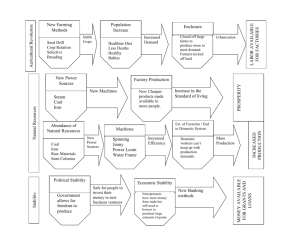
Why does inflammation cause anemia? The bone marrow is the epicenter of red blood cell (RBC) production. In order to create proper RBCs many co-factors are required which include Folate and Vitamin B12. Iron is also required as every RBC contains four iron atoms. The function of the iron atoms is to bind oxygen for pick up from the lungs and delivery to the tissues. The kidneys also play a role in anemia. The kidneys sense oxygen levels and produce a hormone called erythropoietin upon low oxygen levels. Erythropoietin stimulates RBC production in the bone marrow. Patients with Chronic Kidney Disease (CKD) may receive synthetic erythropoietin called erythropoietin stimulating agents (ESAs) like Procrit, Epogen, or Aranesp. However, if the body's storage of iron is low, then effective RBC production from the bone marrow will be limited. The majority of the body's iron storage is found within the RBCs. The average life span of the RBCs is 120 days. Upon death of the RBCs, the iron is recycled by the spleen and macrophages. The macrophages engulf the iron and are stored by the iron-storage protein called ferritin. Furthermore, within the blood stream, iron called be transported by proteins called transferrin. A majority of the body's iron content is recycled. On a blood test, there are three common tests that are analyzed for evaluation for anemia. These are Iron, TIBC, and Ferritin. TIBC stands for Total Iron Binding Capacity and is an indirect measurement of the transferrin protein. During an inflammatory process certain inflammatory chemicals called cytokines can inhibit the normal process of iron release and absorption leading to anemia. Theses cytokines are: Interleukin-1 (IL-1), IL-6, IL-10, TNF-alpha, and Interferon gamma. Let's take the example of a bacterial infection. Bacteria contain a complex sugar structure called lipopolysaccharide (LPS). LPS can stimulate cytokine release of IL-6 from white blood cells called monocytes. Both IL-6 and LPS in turn stimulate the release of a liver protein called hepcidin. Hepcidin's effects are to decrease intestinal absorption of iron from the duodenum and to inhibit iron release from the macrophages. (see cartoons) If iron is not released from the macrophages then it cannot be utilized by the bone marrow for RBC production. Moreover, there are several other ways the immune system can worsen anemia: 1) Interferon gamma, TNF-alpha, and IL-1 all can inhibit the kidney's production of erythropoietin. 2) TNF-alpha can enhance the capacity of macrophages to engulf RBCs and incorporate their iron content. 3) Hepcidin and Interferon gamma can inhibit the macrophage's capacity to release iron. 4) Interferon gamma can enhance iron absorption by macrophages. 5) IL-1, IL-6, and IL-10 can increase the ferritin content in macrophages allowing for more storage capacity. 6) Finally, IL-10 can enhance the release of iron from transferrin to the macrophages. Thus, inflammation causes increased macrophage storage of iron and inhibits its release. Inflammation also inhibits intestinal absorption of iron and decreases the kidney's production of erythropoietin. High ferritin levels on a blood test can signify an inflammatory process. Whereas a low ferritin level reflects possible iron depletion. In order to further assess this, a Transferrin Saturation (T- Sat) needs to be calculated. This is done by taking iron level and dividing it by the TIBC level from the blood test and multiplying by 100. A ferritin below 100 and a T-sat below 16-21% signifies iron deficiency. In dialysis patients the criteria is different. A T-sat of less than 21% and a ferritin less than 500 relates iron deficiency. CKD patients do not commonly absorb oral iron effectively (probably due to hepcidin's effects). Thus, IV iron is commonly given. Without a sufficient amount of iron storage, ESAs like Epogen, Procrit, and Aranesp will not be as effective. Why does the body make such an effort to conceal iron storage during an inflammatory process. Probably this is due to the fact that certain bacteria also use iron for their own growth. And thus, during a bacterial infection in the blood or pneumonia, it is probably not wise to receive IV iron. Weiss, G, Goodnough, L: Anemia of Chronic Disease. NEJM; 350 (10); March, 10, 2005