DRUG MECHANISM/USE PHARMACOKINETICS SE OTHER
advertisement

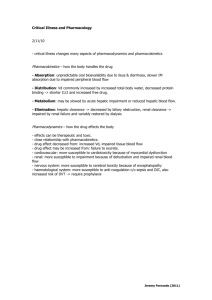
DRUG MECHANISM/USE PHARMACOKINETICS Block COX1 and 2 to inhibit PG synthesis 1. ANALGESIA-PGE2 and PGI2 sensitize nerves to pain 2. ANTIPYRESIS-LPS, TNFa, and IL-1 induce COX2 in the hypothalamus to make PGE2, which raises the set point for temp 3. ANTIINFLAMMATORY-PGs contribute to vasodilation and pain/tenderness (need higher doses to tx inflamm) 4. ANTITHROMBOSIS – block COX1 dependent thromboxane synthesis 5. CLOSURE OF DA-indomethacin or ALPROSTADIL to keep it open 6. TOCOLYSIS-delay onset of labor by blocking PGE2 synthesis. DINOPROSTONE=PGE2 vag suppository for 2nd trimester abortion ASPIRIN IRREVERSIBLY INHIBITS PLATELET Oral, binds COX1 for the life of the platelet albumin(can displace warfarin) Lipid soluble weak acid – crosses membranes T1/2=15 min but salicylate also active 90%reabsorbed Kinetics become 0 order at high doses, longer T1/2 SALICYLATES METHYLSALICYLATE =bengay SALSALATE=fewer GI and no platelets, no fever DIFUNISAL=no antifever, no auditory, less GI and platelets NSAIDS SE OTHER GI – bleeding d/t increased H and pepsin and decreased HCO3 and mucus RENAL-decreased renal blood flow REYES-hepatic and brain damage in kids with influenza or varicella with aspirin and other salicylates URIC ACID SECRETION-decreased at low and increased at high CLOSE DA HYPERSENSITIVITY – to aspirin but not acetaminophen OVERDOSE – Tinnitus Vomiting Hyperventilation – resp alkalosis Uncoupler – hyperthermia Hypoglycemia Metabolic acidosis Then resp acidosis Compared to aspirin, salicylate: Lower GI Less hypersensitivity NO platelet TX of OD: Tx sx with fluids, tepid water Do blood analysis Charcoal and sorbitol IV INFUSION OF NaHCO3 to alkanalize urin Hemodialysis is above 1mg ACETIC ACID DERIVATIVES INDOMETHACIN Potent inhibitor of COX1 1. Close DA 2. Tocolysis 3. Acute Gouty Arthritis Worse GI effects than aspirin Short term use only SULINDAC Prodrug converted to active in liver DICLOFENAC Osteoarthritis and RA KETOROLAC Shortterm tx of postop pain PROPIONIC ACID DERIVATIVES IBUPROFEN NAPROXEN = longer t1/2 KETOPROFEN LONG HALF LIVES PIROXICAM OXAPROZIN Pain, fever, dysmenorrhea, and inflammation LOW COX1 ACTIVITY NABUMETONE ETODOLAC MELOXICAM COX2 SELECTIVE Anti-inflamm for RA and osteoA CELECOXIB ROFECOXIB REMOVED VALDECOXIB REMOVED COX2>>>COX1 Similar efficacy to ibu RA, and osteoA Menstrual pain FAP to reduce polyp # SULFONAMIDE NON SULFA SULFONAMIDE Enterohepatic cycling so prolonged action of 16hr Rapid release, Delayed release and ophthalmic forms Parental IV or IM for short term Less GI toxicity than aspirin GI tox=aspirin Worse GI tox GI tox=aspirin Once/day dosing (t1/2=50hr) But take 7-12 to reach steady state COX2>COX1 Worse GI tox Less GI Minimal GI Similar Renal NO platelet CYP2C9 metabolism CYP2d6 inhibitor T1/2=11.2 so once/day DRUG INTERACTIONS by cyp2c9 inhibitors (cimetidine, omeprazole, zarfirlucast, sulfas, ketoconazole) SERIOUS CV EFFECTS Stevens-Johnson syndrome Serious CV effects Arthrotec = diclofenac +misoprostol ACETAMINOPHEN =NOT AN NSAID! Analgesic and antipyretic but diff from aspirin: NO anti-inflamm NO CNS effects No reyes No CV or resp No gastric irritation NO platelets NO uric acid effects Similar pharm to aspirin. Normally glucuronidated or sulfated and excreted by kindey. Small % oxidated to substance that reacts with –SH groups, but at normal doses this reacts with GLUTATHIONE to yield a nontoxic product OVERDOSE >7.5g, death at >20g Hepatotox at 10-15g Glutathione depleted at high doses and IRREVERSIBLY reacts with – SH of proteins Alcohol also depletes glutathione TX: NACETYLCYSTEINE = thiol that provides alt. SH groups but can’t reverse damage done. IV bc its gross RUMACKMATTHEWNOMOG RAM to determine risk. Toxic levels increase t1/2 Vicadin=hydrocodone +acetaminophen STAGE1=0-24hrs-GI and sweat 2=24-48hrs-nothing 3=71-96hrs-more sever stage 1 and maybe coma. LFT and bilirubin elevated. Decreased clotting 4=4d-weeks – survive w/NO damage or die IMMUNOSUPPRESANT: CYTOTOXIC DRUGS METHOTREXATE* Folic acid analong AZATHIOPRINE* LEFLUNOMIDE GOLD COMPOUNDS AURANOFIN = oral AUROTHIOGLUCOSE = IM HYDROXYCHLOROQUINE =antimalarial D-PENICILLAMINE =chelating agent for Cu, Hg, Pb, Zn MYCOPHENOLATE MOFETIL* =specific for T and B cells bc they have no salvage pathway MECHANISM/USE =DMARDS NOT analgesics or antipyretics RA, asthma, crohns, MS, psoriasis Inhibits DHFR (DHFTHF)so blocks purine synthesis No THF blocks dUMPdTMP so no DNA, RNA, or protein SO inhibits cell proliferation Prevents renal transplant rejection RA, IBD, lupus, nephritis, wegeners Blocks DNA and RNA synthesis RA Inhibits Dihydroorotate dehydrogenase to block pyrimidine synthesis Only for nonresponsive Mech unknown. Inhibit macrophages? PHARMACOKINETICS Take several weeks AE Serious and limit duration OTHER Taken up by folate transporter and gets polyglutamated LEUCOVORIN Rescue =N-formylTHF, competes with metho for uptake N5N10methylene THF So bypasses need for DHFR (also helps block thymidylate synthesis with FLOROURACIL) BM tox GI tox DOC for RA Antiinflamm at high doses LUPUS and nonresponsive RA Mech unknown Unresponsive RA, Wilsons, Cystinuria Max effect may take 3-6mo Kidney, heart, and liver transplants Inhibits DE NOVO synthesis of dGMP and hence RNA and DNA Reversible, noncompetitive block of IMP dehydrogenase Prodrug hydrolyzed immediately prodrug6mercaptopurine (=analog of hypoxanthine) Prodrug converted in gut or liver LONG t1/2 d/t CYLCING LIVER TOX! Teratogenic Long t1/2: Blood=26days Tissue=80days Diarrhea Rash Stomatitis Renal tox Thrombocytopenia IRREVERSIBLE RETINAL DAMAGE More toxic than golds Cutaneous lesions BM tox Autoimmune syndromes FEW Some GI LESS BM tox than aza Minial renal tox (so better than CSA) PREG D ALLOPURINOL blocks xanthine oxidase so causes accum. Of azathioprine->tox Cholestyramine (resin) can be used to shorten t1/2 from 2wks to 1 day IM injection can cause gray/blue pigment to skin IMMUNOSUPPRESANT: CORTICOSTEROIDS IMMUNOSUPPRESANT: TNFa and IL-1 TARGETERS ETANERCEPT* INFLIXIMAB* ADALIMUMAB CERTOLIZUMAB GOLIMUMAB ANAKINRA IMMUNOSUPPRESANT: T-CELL TARGETERS CYCLOSPORINE* TACROLIMUS =similar to CSA SIROLIMUS* =blocks IL2 ACTION MECHANISM/USE Switch on synthesis of IKB, inhibit PLA2 MECHANISM/USE PHARMACOKINETICS AE OTHER PHARMACOKINETICS AE OTHER TNFa receptor attached to Fc portion of human IgG Chimeric monoclonal Ab against TNFa SC 2x/week +/- methotrexate Human-human Conjugated to pegol Anti TNFa human Recombinant human IL1 Receptor Antagonist RA if DMARDS don’t work MECHANISM/USE SC every 2 weeks SC every 4 weeks SC every 4 weeks SC ONCE A DAY Immunosuppression: Tb, opportunistic, infections, no vaccines, demyelinating, lymphoma Autoimmunity – can get lupuslike syndrome Ab against drug itself Prevent Renal, Liver, Heart Rejection RA, IBD, MG Binds CP to prevent CALCINEURIN from activating NF-AT (stops Tcell prolif) Hydrophobic Variable absorption High first pass Need to assay blood levels ABATACEPT =inhibits Tcell prolif Also blocks CALCINEURIN but via FKBP25 receptor Binds FKBP12 but does NOT block calcineurin or IL2 production BLOCKS MTOR (a cell cycle kinase) Non responsive RA CTLA4 soluble B7 receptor attached to Fc of IgG Binds B7 20x stronger than IV infusions every 8 wks PHARMACOKINETICS Don’t use with TNFa blockers Infections Neutropenia AE NEPHROTOXICITY (hard to tell from kidney rejection) HTN Hypercholesterol Hirsuitism LITTLE EFFECT ON BM + methotrexate in RA to limit Ab production against infliximab +/+/With MTX OTHER INTERACTIONS -w/drugs that inhibit P450 3A4 =Antifungals, grapefruit -Drugs that induce it=phenobarbitol, carbamazepine, rifampin, st jons wort, nephrotoxics, lovastatin hydrophobic hydrophobic Also CYP3A4 metabolism (see interactions) So give 4hrs after CSA NOT liver. hepatic a thrmosis LITTLE nephrotox (but makes CSA’s worse) High TG and chol HTN Thrombocytopenia Don’t use with TNFa blockers or anakinra Renal transplant with CSA or GCs DACLIZUMAB BASILIXIMAB CD28 does For ACUTE renal rejection Monoclonal Ab against IL2 R IV before surgery Use with CSA and GCs