Total contact casting for diabetic foot ulcers
advertisement

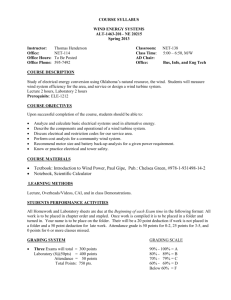
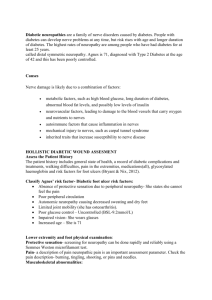
Title: Total contact casting for neuropathic foot ulcers and Acute Charcot’s arthropathy in diabetes – evidence based care pathway Author: Dr V Baskar, on behalf of the Wolverhampton Diabetes Foot Group Date: Jan 2013 Version: Draft pending agreement with Orthopedic and Vascular teams Review date: Jan 2015 Approval needed from: Diabetes LIT Dissemination: Diabetes foot group Archived: Wolverhampton Diabetes Centre Website as part of Foot guidance TCC’s for Diabetic Foot Ulcers – Care pathway Page 1 of 9 Summary Continued mechanical trauma is a key factor responsible for the failure of healing of chronic neuropathic foot ulcers Pressure offloading reliably reduces plantar pressure and has been shown to increase healing rates and shorten healing times Total Contact Casts are believed to be the gold standard method with better and faster healing rates compared to other removable off-loading devices - 89-95% ulcers healed at 12 weeks with 20-25d reduction in healing times o TCC’s superiority is related to poor compliance with removable devices The majority of studies excluded ulcers that were clinically infected or those patients with significant peripheral vascular disease Where TCC’s are used in closely monitored settings, iatrogenic contact ulcerations are seen in very small proportion of patients - reversible minor complication in 1 in 20 casts and permanent sequel from casts in 1 in 400 TCC’s results in considerable reduction in the size of the limb and need mandatory removal and reapplication at the end of the first week o For the management of underlying ulcer and monitoring for iatrogenic ulcers, TCC’s will also need reapplying at 2-3weekly intervals thereafter The time and resource constraints from repeated reapplications of TCC’s is hugely outweighed by costs and morbidity of managing a non-healing ulcer Limited studies have successfully used TCC’s with ulcer windows to circumvent logistical difficulties without concern of ulcer herniation through such windows Recent studies have also attempted to make Removable offloading devices ‘instantly irremovable’ using single layer of fiberglass cast and have shown equivalent healing to TCC’s and at lower costs although these findings need replication in larger studies TCC’s are also the gold standard treatment for Acute Charcot’s foot o Casting is however needed for longer periods and will also need mandatory removal and reapplication at weekly intervals TCC’s for Diabetic Foot Ulcers – Care pathway Page 2 of 9 TCC in Diabetic neuropathic plantar ulcers and Acute Charcot Non healing (>3months) neuropathic plantar ulcers despite optimal footwear or Acute Charcot arthropathy Clinically significant Infection or Peripheral vascular disease* (* Absent both pulses in ulcerated feet or Claudication <200yds or ABPI<0.7 or Evidence of ischemia) YES Eradicate infection Consider vascular assessment/referral No infection & No PVD Consider offloading with casts Compliance to offloading device likely Removable cast walkers (RCW) Compliance to offloading device doubtful Total Contact Casts (TCC) Liaise with plaster room Instant TCC (Fiberglass cast over RCW) TCC with ulcer window Conventional TCC Selected cases where ulcer can be made nonweight bearing End of 1st week & at least & 2 weekly thereafter Removal Reapplication Mandatorily at end of 1st week At least 2-3weekly thereafter (weekly if Acute Charcot) Ongoing f/up In WDC At least 2 weekly until ulcer healed Poor response at 12 weeks (longer for Acute Charcot) Consider alternative options TCC’s for Diabetic Foot Ulcers – Care pathway Page 3 of 9 Governance issues The application of Total Contact Casts must be a Consultant level decision The management plan on the choice of cast method, duration of treatment and monitoring frequency have to be documented in the notes/Letters drive and copied to the Plaster team In selected cases where ulcers can be safely made non-weight bearing, casts with ulcer windows can be considered but with clear documentation as above All requests for TCC’s for patients with diabetes must involve the Specialist Chiropody service in the Diabetes Centre and such details prospectively maintained in a Cast register to allow secure audit trail Any iatrogenic complications while on contact casts has to be reported as a clinical incident and such incidents to be maintained in the Risk Register in WDC and to be shared in the Foot group meeting periodically Patient information leaflets are to be issued following application of TCC’s TCC’s for Diabetic Foot Ulcers – Care pathway Page 4 of 9 Total contact casting for diabetic foot ulcers – evidence based care pathway One of the key factors responsible for the failure of chronic ulcers to heal is continued mechanical trauma to the bed of the healing wound, often occurring during normal activities of daily living and encouraged by the insensate foot. The regenerating wound bed can be protected by a variety of pressure offloading methods including casting, bracing, footwear and surgical offloading. 1. Do Contact casts work? Pressure relief: Contact casts have been shown to reduce plantar pressure by 32-69% (1). This study was however done in healthy non-deformed and non-ulcerated feet in individuals without diabetes. In another study involving 25 patients with diabetes and foot ulcers, removable and non-removable casts were found to reduce pressure in the forefoot to a similar extent (2). Efficacy: As with many other areas of diabetic foot, the quality of available research in this topic is poor and high quality multi-centre RCT showing efficacy of contact casting is lacking. There have however been a few single centre RCT’s involving small patient samples that have shown higher and quicker healing rates of plantar ulcers with total contact casts (TCC) compared to other modalities of offloading (3-6). The proportion of ulcers healed at 12weeks was 89-95%, 52-79% and 30-50% with TCC, Removable Cast Walkers (RCW) and therapeutic shoes respectively. Median time to healing of ulcers was also significantly less with TCC (33-41 days with TCC, 50-58d with RCW and 6165days with therapeutic shoes). The location of the ulcer and presence of deformity has impact on the effectiveness of TCC with forefoot ulcers healing significantly faster than non-forefoot ulcers (10) and midfoot deformities (commonly observed in Charcot) having the longest healing times (11-12). In general, the inferior results of removable offloading devices are believed to be related to poor compliance to non-weight bearing. Ulcer patients have been shown to take an average of 72% of their daily steps unprotected when TCC’s for Diabetic Foot Ulcers – Care pathway Page 5 of 9 given a removable device to offload (7). Attempts to render removable cast walkers instantly non-removable using easier techniques (e.g. single layer of fiberglass cast over RCW) have been shown to have similar results to conventional total contact casts at much lower time and costs involved (8-9). Histological studies: A small study comparing histology of diabetic foot ulcers in patients with and without total contact casts found a significantly more reparative histological pattern (with neo-capillaries and fibroblasts) in the TCC group compared to the inflammatory pattern observed in the conventional non-TCC group (13). This lends further proof at cellular level that pressure relief leads to a favourable healing environment. 2. What are the risks associated with TCC? Time and resource constraints: The application and repeated replacements of casting devices has been an expensive and time-consuming task with additional impact from need for optimal training to the technicians. The cost of managing non-healing diabetic foot ulcers (£300 per month) and its most feared consequence of limb loss (£10000 prior to any rehabilitation cost), however, is considerable, and most studies have concluded the cost effectiveness of total contact casts done in the optimal setting, especially where instant TCC methods are chosen (4, 9, 14). Iatrogenic ulcerations: Ulcerations occurring while within the cast due to pressure or friction from cast material is a risk that can be minimized with careful casting techniques. In a large retrospective review of 398 casts in 70 individuals (92% with diabetes), one minor complication was observed in every twenty TCC’s and 30% of patients suffered one complication during the course of their treatment (15). All new ulcers except one healed with simple modalities within 3 weeks and one patient ended up requiring toe amputation (permanent sequelae from cast of 1 in 400). Ulcer recurrence post casting: One study estimated a 20% reulceration rate following TCC largely related to lack of compliance to treatment program although little mention TCC’s for Diabetic Foot Ulcers – Care pathway Page 6 of 9 was made on specialist footwear use post healing of ulcerations (16). Several studies have confirmed the preventative value of specialist footwear for reulcerations (17-18). Monitoring issues: There is genuine concern that non-removable casting of the foot would render it inaccessible for monitoring for new ulcers and of progress of existing ulcers. In addition, there is considerable reduction in the swelling and the size of foot following plaster casts that would make them too big and at risk of friction and contact ulcers especially after the first week of their application. Good practice would suggest the mandatory need for removal and reapplication of casts after the first week with subsequent reapplications guided by clinical progress but at the very least at 2-3 weekly intervals. Where contact casts have been done in centers with such robust onward monitoring, the incidence of iatrogenic problems from TCC has been incredibly low (15). Casts with ulcer windows: Others have studied TCC’s with windows over ulcers that can be safely made non-weight bearing, as alternatives, and found comparable healing rates to non-removable TCC (19). This comes with the additional logistical advantages of not having to remove and reapply casts many times and allows on-going monitoring of the wound. While there is a theoretical risk of ulcer herniation through the window, where such patients are closely monitored, this risk is believed to be very small. Instant TCC’s, however, has the potential to be the most effective and the safest way of offloading needing very little additional training. 3. Challenging limbs Most studies of TCC have excluded patients with significant infection, osteomyelitis or peripheral vascular disease (especially where ABPI is <0.5). One study placed 98 subjects with vascular insufficiency and/or mildly infected limbs in TCC and showed encouraging results with successful outcomes in all situations except neuroischemic heel ulcers with infection although the best outcomes were for those subjects without vascular disease or infection (20). In another study involving immunosuppressed post transplant patients with diabetes, TCC was found to be as safe and efficacious but with longer healing times compared to immunocompetent comparators (21). Until these findings are TCC’s for Diabetic Foot Ulcers – Care pathway Page 7 of 9 replicated in other good quality studies, TCC should remain contraindicated in patients with significant peripheral vascular disease. 4. Acute Charcot foot and TCC Immobilization is the cornerstone treatment for Acute Charcot and TCC’s are again believed to be the gold standard treatment for patients with this condition. The general principles and efficacy of TCC in Charcot is similar to what is described for neuropathic ulcers. In addition, given the higher possibility of progression and ulceration in Acute Charcot, these patients will need mandatory removal and reapplication of TCC’s at weekly intervals. The length of time the limb needs to be casted can vary from few weeks to several months and is best judged by clinical, radiological and dermal thermometric signs. Also, ulcers following Charcot commonly need longer times in casts to heal (11, 12). Conclusion Despite the lack of large multi-centered RCT’s to strengthen the role of TCC, currently available studies do support their efficacy and safety in treatment of diabetic foot ulcers. However, despite the well-documented gold standard status of TCC for the healing of diabetic foot ulcers, a recent survey found less than 2% of specialists surveyed to be this modality for the majority of their patients with DFU (22). The logistics and the perceived costs may have been important factors in its under use although the instant TCC concept offers genuine hope. The instant TCC technique can be achieved with a lot less training and will allow the treatment modality to be used far more widespread than traditional TCC and at much lower costs and time although its results need replicating in other centers. TCC’s for Diabetic Foot Ulcers – Care pathway Page 8 of 9 References 1. Wertsch et al, J rehab res devpt 1995; 32: 205-9 2. Lavery et al, Diabetes Care 1996; 19: 818-21 3. Mueller et al, Diabetes Care 1989; 12: 384-388 4. Armstrong et al, Diabetes Care 2001; 24: 1019-22 5. Armstrong et al, Diabetes Care 2005; 28: 551-54 6. Caravaggi et al, Diabetes Care 2007: 30: 2577-78 7. Armstrong et al, Diabetes Care 2003; 26: 2595 –97 8. Piaggesi et al, Diabetes Care 2007; 30: 586-90 9. Katz et al, Diabetes Care 2005; 28: 555-59 10. Walker et al, Arch Physical Medical Rehabilitation 1987; 68: 217-21 11. Edmonds M, Drugs 2006; 66: 913-29 12. Sinacore et al, Foot and Ankle Intl 1998; 19: 613-18 13. Piaggesi et al, Diabetes Care 2003; 26: 3123-28 14. Shearer et al, The Diabetic Foot 2003; 6: 30-37 15. Guyton et al, Foot and Ankle Intl 2005; 26: 903-7 16. Helm et al, Archives Physical Medical rehab 1991; 72: 967-70 17. Uccilli et al, Diabetes Care 1995; 18: 1376-78 18. Busch et al, Diabetic Medicine 2003; 20: 665-69 19. Ha Van et al, Diabetes Care 2003; 26: 2848-52 20. Nabuurs-Franssen et al, Diabetes Care 2005; 28: 243-247 21. Sinacore DR. Archive Physical Medicine Rehab 1999; 80: 935-40 22. Wu et al, Diabetes Care 2008; 31: 2118-19 TCC’s for Diabetic Foot Ulcers – Care pathway Page 9 of 9