Leiden, July 4th 2014 Dear (deputy) editors of the BMC Geriatrics
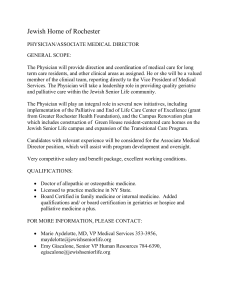
advertisement

Leiden, July 4th 2014 Dear (deputy) editors of the BMC Geriatrics, We would like to thank the editorial staff and the reviewers for their valuable comments on our manuscript. Based on these comments, and your suggestions, we have revised our manuscript ‘Symptoms and treatment when death is expected in dementia patients in long-term care facilities’ (manuscript number 1802990632118536) and have pleasure in resubmitting it to BMC Geriatrics. We believe that the suggested changes have improved the quality of the manuscript. Below we present a point-by-point response to each of the reviewers’ comments. In the revised manuscript all changes have been highlighted. Reviewer: Nathan Davies Questions and answers Q1. Generally well written, however the authors need to correct some phrasing which doesn’t always make sense and some wording throughout the article A1. Thank you for your comment, we have checked and changed several words/sentences to make them clearer: these are highlighted in the revised version of the article. Q2. Introduction The fourth paragraph is a little difficult to read and needs some clarifications for the reader. Line beginning ‘especially the beliefs of health-care…’, I am unsure what the authors are saying here and how it follows from the previous sentence, it needs to be clarified. A2. In the group of patients that lives to the final phase of dementia, the proportion of people dying from cachexia/dehydration is higher compared to patients without dementia (53.2% versus 32.2%; as also reported by Koopmans et al., reference 15). In countries other than the Netherlands, we see a general belief to actively treat these patients with methods for rehydration. We have revised the sentence as follows; ‘Especially the belief among many relatives and health-care workers about an unpleasant death when dehydrated, or the imagined effects of rehydration, may hamper a dignified and evidence-based palliative care.’ Q3. In the final sentence of paragraph four what exactly do the authors mean by ‘more conservative treatment’, could they be more specific? A3. As reported by Houttekier et al. (reference 10), in the Netherlands many people with dementia (92%) die in a long-term care facility and death by cachexia/dehydration is an acceptable scenario. Paragraph four now reads; ‘Differences in treatment during the final phase of patients with dementia have been acknowledged. In many countries (including the USA and some European countries) patients in the terminal phase too often receive aggressive treatments that may be of limited clinical benefit. Especially the belief among many relatives and health-care workers about an unpleasant death when dehydrated, or the imagined effects of rehydration, may hamper a dignified and evidence-based palliative care.’ Methods Q4. Two physicians included patients if they were expected to die within the next 7 days. Was there any attempt to standardize these decisions? Prognosis uncertainty is problematic in dementia so how did they predict this? Did they use standardized criteria? A4. Thank you for this comment. We did not use standardized criteria, but the prediction was agreed upon by a multidisciplinary team comprising the treating physician and the nurses responsible for care of the patient. This is also described in the reference we have added to the revised article by van der Steen et all. (reference 30) The sentence now reads: ‘The expectancy of a patient to die within 7 days is based on an estimation made by the treating physician and nurses caring for the patient, and is often related to the fact that a patient has stopped eating and drinking’. Q5. Translation of the Dutch term ‘stadium’ to ‘stage’ is missing on paragraph eight. A5. As suggested, we have corrected ‘end-stadium dementia’ to ‘end-stage dementia’. Results Q6. What do the authors mean by acute death? Should this be sudden death? A6. Thank you for your comment, this has been corrected to ‘sudden death’. Q7. Cause of death ‘kidney insufficiency’ – should this be renal failure? And what brain injury – this seems a little strange. A7. As suggested, we have corrected ‘kidney insufficiency’ to ‘renal failure’. The brain injury that was mentioned was ‘traumatic brain injury after a fall’. Reviewer: Bettina Husebo Reviewer’s report General impression This is an important manuscript, written by a strong and experienced research group with clinical and scientific knowledge in order to evaluation and treatment of patients with dementia at the end of life. The strength of this study is the prospective follow-up of dying nursing home patients with cognitive impairment. Thank you for your encouraging comments. We hope our responses adequately address your questions and concerns. Questions and answers Abstract Q1. Authors describe that the “expected death within one week” decision was made by the physicians. I would expect that this is a more multidisciplinary process-is it the single doctor who makes this important decision? A1. Thank you for pointing this out (see also point 4 from reviewer Nathan Davies). We did not use standardized criteria but it was indeed a multidisciplinary decision by the treating physician and the nurses caring for the patients on the ward. The sentence now reads; ‘The expectancy of a patient to die within 7 days is based on an estimation made by the treating physician and the nurses caring for the patient, and is often related to the fact that a patient has stopped eating and drinking’. Q2. How were the death diagnoses (dehydration/cachexia) estimated (this is a question for the result, as well)? A2. Elderly care physicians in the Netherlands receive extensive training in elderly care medicine, which includes palliative care. Many people with dementia who are admitted to a long-term care facility stay there until their death. The treating physician is employed by the facility, practices on location, and is in charge of the 24-hour medical care for the patients in the units allocated to the physician. All causes of death were assessed by experienced elderly care physicians who were fully knowledgeable about the patient’s condition in the last phase of life. This part of the discussion now reads: ‘Elderly care physicians in the Netherlands are in charge of the medical care of patients in the long-term care facility. They have received extensive training in elderly care medicine, which includes palliative care. In this study we decided to observe the patients when death was expected within 7 days. The moment of death can be more accurately predicted when the intake of fluid or food has severely diminished; in the present study, the result was that 50% of the patients died within 2 days after the start of the observation. The cause of death was assessed by elderly care physicians who were fully knowledgeable about the patient’s condition in the last phase of life.’ Q3. The manuscript would improve by more details reg. Morphine – mean dosage and application form (this is a question for the result, as well)? A3. Unfortunately, we do not have data on morphine dosage and change in dosage but, in general, in long-term care facilities in the Netherlands we start with a low dose of morphine of 2.5 mg in case of dyspnea and, in case of pain, with 5 mg subcutaneously in total 4 to 6 times per day. In 19 patients participating in the present study, it was not necessary to increase the dosage. In 4 patients, a gradual increase was necessary and, in one patient, there was a substantial increase in dosage on the last day. We have added this information to the revised paper as follows: ‘In 4 patients (16.7%) there was a gradual increase in the dosage of morphine and, in one patient (4.2%), there was a substantial increase in the dosage on the last day. Introduction Q4. This is a well-written introduction and the goals of the study are clearly described. In addition, I would expect a more detailed prescription of expected symptoms in dying patients with dementia at the end of life including dyspnea, death-rattle, restlessness and the need for mouth care. A4. Thank you for your comment. We have added agitation, fear, crying, moaning, choking, gurgling or difficult swallowing because these are some of the symptoms asked about in the observational instruments which were used, and we have also added general palliative care principles, like the need for mouth care and prevention of pressure ulcers, constipation and urinary retention. The sentences now read: ‘The period before death is one in which patients can suffer from pain, dyspnea, agitation, anxiety, fear, crying, moaning, choking, gurgling or difficult swallowing. During this period, mouth care and the prevention of pressure ulcers, constipation and urinary retention are also important.’ Q5. In light of the study content, the reader might expect some reflections regarding different treatment approaches. Further, the reason for the lack of prospective studies should be explained; one would suggest that the point of the dying process is difficult to estimate? A5. The dying process and the moment of dying is difficult to estimate (also reported by Mitchell et al. reference 11); however, in this particular case we chose to study patients with a life expectancy of one week. Although we think that it is always difficult to accurately predict death, the prediction becomes more accurate the closer to the moment of death, perhaps because of the cessation of intake of fluids or food. Our study showed that 50% of the patients died within 2 days after the start of the observation. We have added sentences to clarify this in the discussion, as follows: ‘Elderly care physicians in the Netherlands are in charge of the medical care of patients in the long-term care facility. They have received extensive training in elderly care medicine, which includes palliative care. In this study we decided to observe the patients when death was expected within 7 days. The moment of death can be more accurately predicted when the intake of fluid or food has severely diminished. In the present study, the result was that 50% of the patients died within 2 days after the start of the observation. The cause of death was assessed by the elderly care physicians who were fully knowledgeable about the patient’s condition in the last phase of life.’ Methods Q6. There are some questions in order to the inclusion process of participating institutions: The number of nursing home places/beds could be mentioned as well as the expected death rate. How many patients use to die during one year? Where all the dying patients in this 1- year period of these two institutions or was it an inclusion “by chance”? How many patients were attended to be included and in fact were included. A6. In the article we have now described the inclusion process; ‘During the study period from February 2008 to February 2009 in two Dutch LTCFs a total of 36 patients died on the wards in which the physicians were working. Of these, 12 patients could not be included in the present study because of sudden death (n=5) or because the physician did not have the opportunity to perform the observations (n=7), resulting in 24 participants available for this study.’ Q7. One would expect that some relatives refused participation? A7. All relatives consented to the non-invasive observations by the physician and to the use of coded data for research purposes. Q8. In general, it may be challenging to estimate the “point of no return” or the “last week” – this means the date for inclusion. It is important to describe this procedure even better. Was it the physician alone or a multidisciplinary discussion/insight to estimate the “last week” and how was this decision communicated to the patient (if possible), the family, and other members of the staff? A8. Thank you for mentioning this important point. As also explained in your first question, we did not use standardized criteria but it was indeed a multidisciplinary decision by the treating physician and the nurses on the ward. The sentence now reads: ‘The expectancy of a patient to die within 7 days is based on an estimation made by the treating physician and the nurses caring for the patients, and is often related to the fact that a patient has stopped eating and drinking’. Q9. Related to this, the competence area and working experiences of the physicians would be of interest, because this may be important in light of their ability to assess the symptoms, initiate the treatment, and assess treatment efficacy. I read these paragraphs several times and was slightly confused: Is it the physician who select the patients, estimate “point of no return”, assess pain and symptoms, initiate the treatment, and evaluate the treatment effect”. If so, subjectivity of the results would be rather high and low external validity. Can we expect that a physician evaluates his/her own (pain and symptom management) work objectively in this situation? I hope the research group can elaborate these concerns in a precise and reflected version. A9. Both elderly care physicians had over 7 years of experience in treating patients with dementia who, in the Netherlands, almost always stay in the nursing home until death. The physician coordinates a team of nurses and is in charge of the same ward for a long period of time, during which they become familiar with the patients and their relatives. We understand your concern regarding the objectiveness of the treating physicians. To promote valid and reliable scoring of the observational instruments the physicians received training with an instructional video on the use of two of the observational instruments. We also stated in the discussion that the observations by the treating physician (who is also responsible for the treating decisions) might have been influenced by the study itself and we have added that it would be interesting to repeat the study with independent, objective observers. The new sentence reads: ‘It would be interesting to repeat this study and include independent, objective observers, and also include observations after a change in treatment. At the time of this study, the validated instruments used were the best available. These observational instruments help to structurally assess symptoms in these patients, and can help to observe symptoms and to assess the effect of the treatment received for these symptoms.’ Results Q10. Only 24 patients were included in this study; the “drop-out” rate was high; the statistical strength is questionable in this context. Of these, 11 were observed only one time (is this correct?); 13 individuals were observed more frequently. Regarding the 11 patients: in this end-of-life situation, is it possible to make decisions reg. treatment efficacy by only one observation? This means the assessment of pain and symptom, initiating treatment, and assessment of the treatment efficacy. A10. With this study we intended to observe the frequency and intensity of symptoms in the last days before death. It would be valuable to have more data concerning all patients, on more moments during the day, as well as data before and after a change in treatment. Unfortunately we only collected data in the morning and at the end of the day: moreover, this observational study does not allow to assess treatment efficacy. Q11. Is it possible that patients were included at a rather late time point when 12 died within the first two days? What does it mean regarding the ability to estimate the time of dying? Or is it possible that side-effect by treatment (Morphine) shortened life? A11. As also mentioned in question 8 the exact time of death is difficult to estimate, so indeed half of the patients in this study were included shortly before death. Although the exact amount and dosage of morphine was not known, the physicians reported that in 19 patients (79.1%) that they did not increase the dose of morphine. Only 4 patients received a gradual increase in the dose of morphine and in one patient the dose was substantially increased on the last day. Many patients receive the starting dose of morphine and never have an increase of that dose. They can continue the use of morphine for days or weeks and sometimes even months. We do not see death as a side-effect of this medication at these dosages and there is (as far as we know) no evidence in the literature to support this link. We have added this topic to the discussion as follows: ‘All patients received morphine and, in 19 (79.1%) of these patients, the dosage was not raised. We do not want to imply that the use of morphine in the last days of life with dementia is always necessary, but it is often used to alleviate the burden of pain or dyspnea. In the Netherlands, many patients receive the starting dose of morphine (10-30 mg subcutaneously a day), for a considerable period of time (i.e. days, weeks, sometimes even months). Death is not considered to be a direct side-effect of this medication in these dosages and (as far as we know) there is no published evidence for any association between this treatment and death.’ Q12. It has to be clarified how physicians differed between discomfort and pain, and fear and anxiety. The PAINAD score is rather low. How was observation/rating been conducted: was this observation during care, when the patient was moved/turn over in the bed or in rest? One could suggest that observation of pain in rest tells something else than during care activities or movements? A12. All patients were in bed and in rest when the physician made the observations in the morning or evening. We agree that patients in the terminal phase of life can experience more pain, for instance while they are being turned to receive care, but we did not specifically study that topic. We have added to the Methods section the following sentence: ‘During the observation periods, the patients were in rest.’ Differentiating between ‘fear and anxiety’ and ‘discomfort and pain’ can be difficult, but the DS-DAT is an instrument that measures discomfort and PAINAD is validated to measure pain. At the time of the study these were the best available validated instruments. We have added this to the Discussion as follows; ‘Studying symptoms of dying in patients with dementia is challenging. Although differentiation between pain and, for instance, anxiety or discomfort is difficult, in the present study specific observational instruments were used. The DS-DAT was specifically developed to measure discomfort in advanced dementia, and the PAINAD was developed and validated for the assessment of pain in people with dementia.’ Q13. Is the PAINAD an appropriate instrument to assess pain in dying individuals, and is this instrument validated in order to this situation? By the way, it could be an interesting information how many patients exhibit Cheyne – Stoke respiration at the end-of-life. A13. The PAINAD (Pain Assessment In Advanced Dementia) is an instrument especially developed and validated for the assessment of pain in people with dementia but has not been validated separately for the last days of life. The highest score on the item ‘breathing’ does score noisy labored breathing, long periods of hyperventilation, or Cheyne-Stokes respirations and was scored 8 times. However, because this ‘breathing’ does not differentiate between these separate items, we cannot calculate how many of the 8 times scored were specifically for Cheyne-Stokes respirations. We think that Cheyne-Stokes respirations are often seen in the last days of life and are part of the normal physiological process of dying and this may in fact be a weak point of this instrument. We have added this to the Discussion; ‘The PAINAD has not been validated for use in the last days of life. The item ‘breathing’ in the PAINAD covers 'noisy labored breathing’, ‘long periods of hyperventilation’ or ‘CheyneStokes respirations’. Cheyne-Stokes respirations are often seen in the last days of life and can be part of the normal physiological process of dying. However, because we cannot differentiate between the three symptoms observed under ‘breathing’, we cannot state exactly how many people exhibited Cheyne-Stokes respirations.’ Q14. Cicely Saunders described gurgling/death rattle as the most frequent symptoms at the end-of life. In this study, these symptoms are less frequent observed; can this be explained, for instance low use of hydration? Like the assessment of pain/anxiety, nausea and vomiting may be difficult to evaluate. However, these symptoms are not mentioned in the EOLD-CAD. Suggestions related to this? A14. We also saw gurgling/death rattle, but this was not the most frequent symptom. We find your hypothesis that this may be due to the low use of hydration very interesting, but we cannot answer this properly based on our study data. Q15. Regarding dyspnea: Do authors have a reflection in order potential causes of dyspnea, for instance, pneumonia, lunge oedema, fever, anemia, or anxiety? Could it be possible that different causes estimate different treatment options – others than morphine? A15. Indeed we agree that different causes can lead to different treatment options. However, in this study we do not have the data to differentiate between these other potential causes. Q16. Is it possible to die in peace (90%) with symptoms of discomfort (38%), pain (15%), restlessness (18%), or dyspnea (30%)? One would not expect a 100% symptom and pain relief – but the difference between observed pain/symptoms and the overall evaluation of “calm and peace” by the responsible physician it striking and needs further explanation. A16. The treating physician who observed the patients filled in the Mini Suffering State Examination (MSSE) at the end of the day, and also had to answer questions regarding the whole day with only ‘yes’ or ‘no’ as an option to choose from. The End-of-Life in Dementia scales-Comfort Assessment in Dying (EOLD-CAD) was completed twice a day and was part of the observation. The response options were ‘a lot’, ‘some-what’ and ‘not at all’. In Table 2 we wanted to show whether a symptom was presented, therefore, we combined ‘a lot’ with ‘some what’. ‘A lot’ was scored for discomfort in 10% of the observations, pain in 7.5%, restlessness in 5% and dyspnea in 17.5%. ‘A lot’ was scored in peace in 72.5% and in 17.5% of the cases the physician selected the response option of ‘some-what’. We think this is an explanation for the differences in the interpretation of the percentages. We have now clarified this in Table 2. Q17. There is lack of information in order to the type of the opioid, indication (pain, restlessness, dyspnea), time point of application, application form, and effect of the treatment. In addition, it is rather surprising that the application form (oral, rectal, s.c., i.v/ syringe-driver and the mean dosages of morphine. Other periphery analgesics/week opioids are not mentioned. It is unclear whether the application of morphine is the only treatment option for all symptoms: anxiety, restlessness, gurgling, dyspnea, and pain. A17. Unfortunately, we do not have data on the exact amount of dosage and the application form, as described in question 11. Other analgesics such as paracetamol (acetaminophen) were used in 8 (33.3%) patients but we do not have the exact amount that was prescribed and whether or not PRN medication was actually given when needed. We have revised the sentence in the Methods section as follows: ‘Information about care, medical treatment (including pain, antipsychotic and anti-depressive medication), and treatment decisions in the last 7 days before death were also collected.’ In the Results section we have added: ‘The exact dosages of paracetamol, NSAIDs, anti-depressive and antipsychotic medication, were not available for all patients.’ Q18. The graphs at the end of the manuscript are difficult to understand and need further explanation. A18. We have added an explanation to the graphs. Discussion Q19. Authors suggest that: The low level of burdensome symptoms in all days before death, also in patients dying from dehydration/cachexia, the low rate of aggressive curative treatment and the high rate of palliative treatment with morphine are striking results. These data strengthen the recommendations for a better tailored, less curative aggressive approach to palliative care in dementia.” The use of morphine in general does not guarantee good palliative care. In this study, all patients received morphine. Is it possible that some of them did not really had indication for this treatment? Without a clear indication findings could be interpreted with a ‘one size fits all’ approach to pain and symptom management. A19. Thank you for your question. We wish to avoid the impression that we conclude that all patients should receive morphine in the last days of life. We think that this study can help physicians and researchers to realise that a tailored approach, which is not aimed at life prolongation, is needed in dementia. We did observe symptoms but, overall, the rates of these symptoms were low and morphine was used; however, we think that all symptoms and options to decrease or prevent problems (such as due to urinary retention or pressure ulcers) should feed into a personalised tailored care plan to help the patient and his/her relatives in the process of dying. We have added this to the Conclusion; ‘All symptoms and preventive measures should feed into a personalised tailored care plan to help the patient and the (in)formal caregivers in the process of dying with dementia.’ We do hope that we have adequately addressed all the comments and that our manuscript may now be suitable for publication in BMC Geriatrics. On behalf of all authors, Yours sincerely, Maartje Klapwijk, Researcher and elderly care physician Leiden University Medical Center Department of Public Health and Primary Care P.O. Box 9600 2300 RC Leiden The Netherlands Telephone: +31 71 5268444 e-mail: m.s.klapwijk@lumc.nl