Case Study 1: Sickle cell patient complains about shortness of breath
advertisement
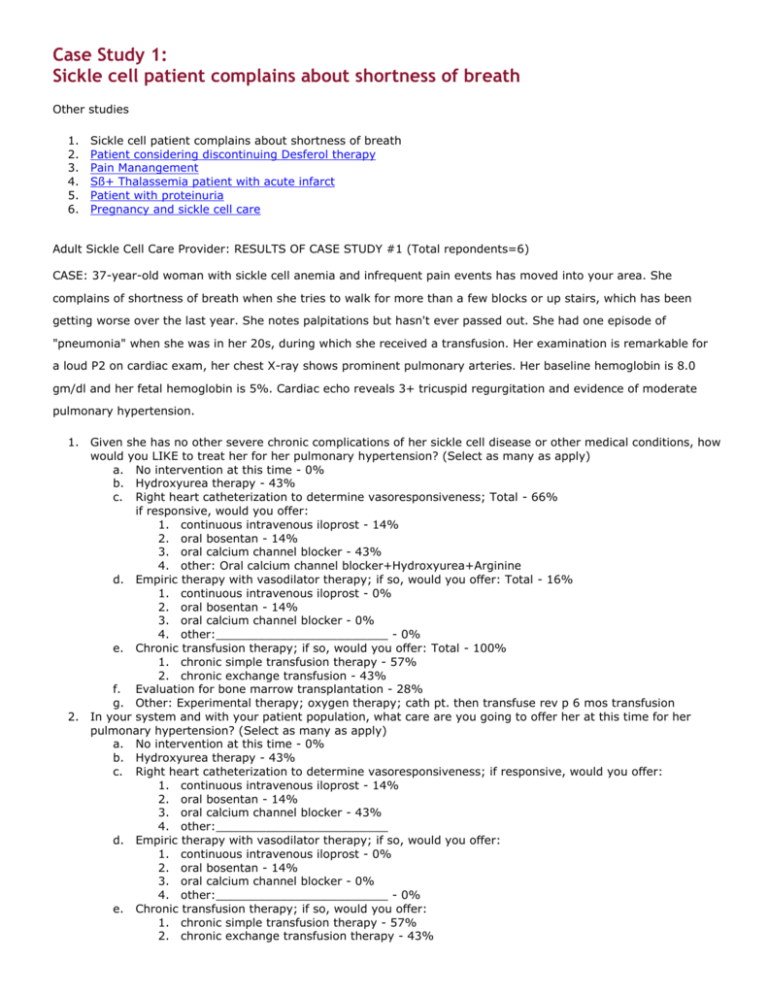
Case Study 1: Sickle cell patient complains about shortness of breath Other studies 1. 2. 3. 4. 5. 6. Sickle cell patient complains about shortness of breath Patient considering discontinuing Desferol therapy Pain Manangement Sß+ Thalassemia patient with acute infarct Patient with proteinuria Pregnancy and sickle cell care Adult Sickle Cell Care Provider: RESULTS OF CASE STUDY #1 (Total repondents=6) CASE: 37-year-old woman with sickle cell anemia and infrequent pain events has moved into your area. She complains of shortness of breath when she tries to walk for more than a few blocks or up stairs, which has been getting worse over the last year. She notes palpitations but hasn't ever passed out. She had one episode of "pneumonia" when she was in her 20s, during which she received a transfusion. Her examination is remarkable for a loud P2 on cardiac exam, her chest X-ray shows prominent pulmonary arteries. Her baseline hemoglobin is 8.0 gm/dl and her fetal hemoglobin is 5%. Cardiac echo reveals 3+ tricuspid regurgitation and evidence of moderate pulmonary hypertension. 1. Given she has no other severe chronic complications of her sickle cell disease or other medical conditions, how would you LIKE to treat her for her pulmonary hypertension? (Select as many as apply) a. No intervention at this time - 0% b. Hydroxyurea therapy - 43% c. Right heart catheterization to determine vasoresponsiveness; Total - 66% if responsive, would you offer: 1. continuous intravenous iloprost - 14% 2. oral bosentan - 14% 3. oral calcium channel blocker - 43% 4. other: Oral calcium channel blocker+Hydroxyurea+Arginine d. Empiric therapy with vasodilator therapy; if so, would you offer: Total - 16% 1. continuous intravenous iloprost - 0% 2. oral bosentan - 14% 3. oral calcium channel blocker - 0% 4. other:________________________ - 0% e. Chronic transfusion therapy; if so, would you offer: Total - 100% 1. chronic simple transfusion therapy - 57% 2. chronic exchange transfusion - 43% f. Evaluation for bone marrow transplantation - 28% g. Other: Experimental therapy; oxygen therapy; cath pt. then transfuse rev p 6 mos transfusion 2. In your system and with your patient population, what care are you going to offer her at this time for her pulmonary hypertension? (Select as many as apply) a. No intervention at this time - 0% b. Hydroxyurea therapy - 43% c. Right heart catheterization to determine vasoresponsiveness; if responsive, would you offer: 1. continuous intravenous iloprost - 14% 2. oral bosentan - 14% 3. oral calcium channel blocker - 43% 4. other:________________________ d. Empiric therapy with vasodilator therapy; if so, would you offer: 1. continuous intravenous iloprost - 0% 2. oral bosentan - 14% 3. oral calcium channel blocker - 0% 4. other:________________________ - 0% e. Chronic transfusion therapy; if so, would you offer: 1. chronic simple transfusion therapy - 57% 2. chronic exchange transfusion therapy - 43% f. g. Evaluation for bone marrow transplantation - 28% Other:same as above Other Comments: Patient classified as NYHA functional class II. Lack of cardiology support to determine vasoresponsiveness is virtually absent here at this time. If pt. were NYHA II or IV would not give vasodilators without heart cath. Hydroxyurea has no proven benefit but practically may delay progression of disease. If patient does not demonstrate vasoresponsiveness would consider bosentan. I think these are excellent questions. We should pool all our patients; design protocol and prospectively study. With a hgb of 8.0 when was her last transfusion, and had she had a recent infection? Would repeat echo for pul artery pressure to determine if some reversal of high PA pressure. Discussion/Summary The case presented represents a common medical problem facing adults with sickle cell disease. Chronic lung disease, with subsequent pulmonary hypertension in many cases, may develop in up to 40% of sickle cell disease patients. The presence of pulmonary hypertension in these patients is associated with shortened survival. To date, there has been no careful study of interventions that may reduce the morbidity and mortality of this complication or when to introduce them. Recent reviews acknowledge the increased recognition of this problem, provide interesting hypotheses as to the underlying pathophysiology and propose possible therapeutic interventions, but reports of successful intervention are limited to small case series. Those of us responding to this case would all offer some sort of intervention, and often more than one approach. All would at least provide chronic transfusion therapy. This is likely based on successful use of transfusion to suppress other complications of sickle cell disease and anecdotal success for patients with pulmonary hypertension. Interestingly, aside abstracts presented at the national sickle cell meetings, there are no published data to suggest transfusion impacts significantly on the pulmonary process. Many believe it to be effective therapy, and it is discussed in reviews as an indication for chronic transfusion, but it would be helpful to at least pool observational data to demonstrate a benefit. Bone marrow transplant evaluation was considered by some practitioners, and raises the issue of indications & inclusion criteria for BMT studies, which may be different for adult than pediatric patients. The use of continuous-infusion vasodilator therapy has been reported to be successful in improving hemodynamic abnormalities in small series of patients with sickle cell disease. Most practitioners responding to this case would first do a right heart catheterization to establish responsiveness, but some would proceed directly to empiric therapy. Intravenous vasodilator therapy appears to be tolerated in most of the cases reported, though the numbers treated are small. I couldn't find any published reports of the use of oral calcium channel blockers for this purpose or bosentan in sickle cell disease. Another area ripe for study. The use of hydroxyurea to treat chronic sickle cell lung disease is an option considered by some practitioners. While there are data reporting regeneration of the spleen on hydroxyurea therapy, implying reversal of or at least recovery from chronic injury, the benefit of hydroxyurea in chronic sickle lung disease is unstudied. Again, even observational data of improvement in pulmonary hypertension while on hydrea would be a step in the right direction, though formal study is needed to answer the question of benefit. In summary, the practitioners who responded all would offer some kind of intervention for symptomatic, moderately severe pulmonary hypertension in their sickle cell disease patients. Only one respondent felt that there was a significant limitation of access, at least in general, to the care they'd like to provide. However, only a few care providers participated in this discussion and others may have significant limitations in their care system. The real need in this area is careful study of these and other interventions that may impact on this complication. It will fall to adult care providers to move this forward, since it is a complication that affects adults much more frequently than children. Below is a limited bibliography of relatively recent publications. 1. Adedji MO, Caspedes J, Allen K, Subramony C, Hughson MD. Pulmonary thrombotic arteriopathy in patients with sickle cell disease. Arch Pathol Lab Med 2001 Nov;125(11):1436-41. 2. Castro O, Hogue M, Brown B. Pulmonary hypertension in sickle cell disease: Cardiac catheterization results and survival. Blood first edition paper, prepublished online October 3, 2002. 3. Hague AK, Gokhale S, Rampy BA, Adegboyega P, Duarte A, Saldana M. Pulmonary hypertension in sickle cell hemoglobinopathy: a clinicopathologic study of 20 cases. Hum Pathol 2002 Oct;33(10):1037-43. 4. Kaur K, Brown B, Lombardo F. Prostacyclin for secondary pulmonary hypertension. Letter to the Editor. Annals of Int Med 2000 18;132(2). 5. Knight J, Murphy T, Browning I. The lung in sickle cell disease. Pediatric Pulmonology 1999 28:205-216. 6. Minter K, Gladwin M. Pulmonanry complications of sickle cell anemia: A need for increased recognition, treatment, and research. Am J Repir Crit Care Med 2001;164:2016-2019. Thank you for participating. Please let us know if you would be interested in pooling patient information or even organizing to facilitate prospective studies in this area. Kathy Hassell Back to Top For additional information please contact: Colorado Sickle Cell Center If you are experiencing problems using this website contact Webmaster